Abstract
Diabetes mellitus is an important predisposing factor for tuberculosis. The aim of this study was to investigate the mechanism underlying this association using a murine model. Mice with streptozotocin-induced diabetes mellitus were prone to Mycobacterium tuberculosis infection, as indicated by increased numbers of live bacteria in lung, liver and spleen. In diabetic mice, the levels of IL-12 and IFN-γ in the lung, liver and spleen were lower than those in control animals on day 14 postinfection, while the opposite was true for IL-4 levels in the lung and liver. The expression pattern of inducible nitric oxide synthase (iNOS), in the two mice types was as for IL-12 and IFN-γ. In addition, peritoneal exudate cells obtained from diabetic mice produced lower amounts of IL-12 and NO than those from control mice, when stimulated in vitro with M. bovis BCG. Spleen cells from diabetic mice infected with M. tuberculosis produced a significantly lower amount of IFN-γ upon restimulation with purified protein derivatives (PPD) than those from infected nondiabetic mice. Interestingly, addition of high glucose levels (33 mM) to the cultures of PPD-restimulated spleen cells reduced the synthesis of IFN-γ only in diabetic mice, and not in nondiabetic mice. Finally, control of blood glucose levels by insulin therapy resulted in improvement of the impaired host protection and Th1-related cytokine synthesis. Our results suggest that the reduced production of Th1-related cytokines and NO account for the hampered host defense against M. tuberculosis infection under diabetic conditions.
Keywords: diabetes mellitus, Mycobacterium tuberculosis, IL-12, IFN-γ, nitric oxide
Introduction
Diabetes mellitus is one of the most important risk factors for worsening tuberculosis [1]. The frequency of diabetes in tuberculosis patients is reported to be about 10–15%, and the prevalence of this infectious disease is 2–5 times higher in diabetic patients than in nondiabetic controls [2]. In spite of such clinical observations, the mechanism for the increased susceptibility of patients with diabetes mellitus to tuberculosis remains to be fully understood. Many investigators have focused on the functional roles of neutrophils, such as their migration to the inflammatory tissues and phagocytosis and killing against bacteria, because the infectious diseases caused by extracellular bacteria are highly prevalent under diabetic conditions. All these neutrophilic functions are well documented to be strongly impaired in these patients [3–5]. In an earlier study, Saiki and coworkers proposed an excellent animal model to approach this issue [6]. Diabetic mice established by administering streptozotocin were highly prone to Mycobacterium tuberculosis infection with an attenuated delayed-type hypersensitivity response to mycobacterial antigens. However, to date this interesting study has not been followed-up.
Host defense against M. tuberculosis infection is largely mediated by cellular immune responses [7]. Type-1 helper T (Th1) cells play a central role in the host defense by inducing the production of interferon (IFN)-γ, which potentiates the nitric oxide (NO)-dependent killing activity of macrophages [8]. Interleukin (IL)-12 is an essential cytokine for the development of Th1 cells from naïve Th cells [9]. Recently, CD8+ T cells were found to contribute to the host resistance against this bacterial pathogen. These cells function by generating IFN-γ and destroying the infected cells [10–12]. IL-12 is also a prerequisite cytokine for acquisition of these properties by CD8+ T cells [13]. The essential roles of IFN-γ and IL-12 have been proved using mice with a targeted disruption of the genes for these cytokines. Both IFN-γ–/– and IL-12–/– mice are highly prone to infection with M. tuberculosis [14–17]. In addition, the discovery of patients with genetic dysfunction of the IFN-γ receptor (R), IL-12Rβ1, and IL-12 has clarified the role of Th1-related cytokines in host resistance to infection in humans. These patients undergo repeated infection by intracellular pathogens, including acid-fast bacilli [18]. On the other hand, no clear role for Th2 cytokines has been reported in the host immune responses to this infection [7,19].
In clinical investigations by Tsukaguchi et al. [20,21], Th1 responses, as indicated by the production of IFN-γ and IL-12, were demonstrated to be attenuated in tuberculosis patients with diabetes mellitus, when compared to nondiabetic cases. Such reduced Th1 responses correlated well with the progression of the diabetic condition. On this background, we addressed in the present study the mechanism of increased susceptibility to M. tuberculosis infection in diabetes using a mouse model of diabetes mellitus that was established by administration of streptozotocin, a pancreatic islet β-cell toxin. In these mice, host resistance against M. tuberculosis infection was diminished, and this impaired host defense was associated with reduced production of Th1-related cytokines, including IL-12 and IFN-γ, and NO and impaired development of Th1 cells.
Materials and methods
Mice
Female ICR mice were purchased from CLEA Japan (Tokyo, Japan) and used at 6–18 weeks of age. All experimental protocols described in the present study were approved by the Ethics Review Committee for Animal Experimentation of our university (University of the Ryukyus, Okinawa, Japan).
Culture medium and reagents
RPMI1640 medium was obtained from Nippro (Osaka, Japan), fetal calf serum (FCS) from Cansera (Rexdale, Ontario, Canada) and streptozotocin (STZ) from Sigma Chemical Co. (St. Louis, MO, USA). M. bovis BCG (Tokyo strain) and purified protein derivatives (PPD) were purchased from Nihon BCG Co. (Tokyo).
Induction of diabetes mellitus
Diabetic mice were established by intraperitoneal injection of 150 mg/kg STZ dissolved in 5 µm sodium citrate buffer (pH 4·5) after one night starvation. Control mice received injections of equivalent volumes of sodium citrate buffer. Fasting blood glucose levels in diabetic mice were elevated to more than 33·3 m m on day 14 post-treatment, and this condition continued for more than 5 weeks, while fasting glucose levels were kept at less than 11·1 m m in control mice during the observation period. Some diabetic mice received daily subcutaneous injections of human recombinant insulin (Novo Nordisk, Tokyo, Japan) at 0·5–2 unit/mouse from the second day after STZ treatment, which resulted in improved blood glucose levels mostly less than 22·2 m m.
Infection with microorganisms
M. tuberculosis H37Rv strain (ATCC25618) from the same frozen stock was grown in Middlebrook 7H9 medium (Difco, Detroit, MI) containing 0·05% Tween-80 to mid-log phase. The bacteria were suspended in 100-µl normal saline after washing three times with normal saline containing 0·05% Tween-80. Mice were infected with an intravenous inoculum of M. tuberculosis (1–3 × 105 CFU) 3–5 weeks after administration of STZ or control vehicle.
Enumeration of viable M. tuberculosis
Mice were sacrificed on day 12 after infection, and spleen, lung and liver were dissected out carefully and then separately homogenized in 10 ml of distilled water by teasing with a stainless mesh at room temperature. The homogenates, appropriately diluted with distilled water, were inoculated at 100 µl on nutrient Middlebrook 7H11 agar (Difco) plates and cultured for 2–3 weeks, followed by counting the number of colonies.
Preparation of organ homogenates
Mice were sacrificed before and on 7, 14 and 35 days after infection, and spleen, lung and liver were separately homogenized in 2 ml of phosphate-buffered saline (PBS) for spleen and lung or 5 ml for liver by teasing with a stainless mesh. The homogenates were centrifuged, filtered through a 0·22-µm filter (Millipore Corp., Bedford, MA, USA) and kept at − 70°C before measurement for cytokine concentrations.
Extraction of RNA and real time RT-PCR
Total cellular RNA was extracted from the lung, liver and spleen of diabetic and nondiabetic mice on days 7 and 14 after infection with M. tuberculosis using ISOGEN (Wako, Osaka), followed by reverse transcription [22]. The levels of inducible NO synthase (iNOS) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA in the cDNA were quantified by real-time PCR on a LightCycler (Roche Diagnostic Systems). Hot start PCR was performed in 20 µl containing 50 m m Tris-HCL (pH 8·3), 4 m m MgCl2, 500 µg/ml bovine serum albumin (BSA), 200 µm dNTPs, 0·125 U/µl Taq, 0·175 µm Taqstart Abs, 0·25 µm primers, and 2 µl of cDNA template and monitored in real time with the fluorescent DNA binding dye SYBR green (Roche Diagnostic Systems). The following primer pairs were used: 5′-AGG TAC TCA GCG TGC TCC AC-3′ (sense) and 5′-GCA CCG AAG ATA TCT TCA TG-3′ (antisense) for iNOS, and 5′-CTC ATG ACC ACA GTC CAT GC-3′ (sense) and 5′-CAC ATT GGG GGT AGG AAC AC-3′ (antisense) for GAPDH. Standard curves for iNOS and GAPDH were generated after 2-fold dilutions of positive samples. The mRNA level for each sample was normalized by dividing the calculated value by the GAPDH value.
Preparation and culture of peritoneal exudate cells
Diabetic or nondiabetic mice were injected intraperitoneally with 5 × 106 CFU of M. bovis BCG, and peritoneal exudate cells (PEC) were harvested 3 days later by three cycles of injection of 5 ml of cold RPMI1640 supplemented with 10% FCS. The obtained cells were washed three times in RPMI1640 culture medium. In a flow cytometric analysis, PEC from three diabetic and control mice contained 34·6 ± 8·6 and 47·1 ± 6·5% T cells (P = 0·115) [fluorescein isothiocyanate (FITC)-anti-CD3 mAb (145–2C11: PharMingen, San Diego, CA, USA)], 28·1 ± 11·1 and 18·0 ± 13·5% B cells (P = 0·372) [PE-anti-B220 mAb (RA3–6B2: PharMingen)], 34·6 ± 8·6 and 47·1 ± 6·5% natural killer (NK) cells (P = 0·44) [antiasialo GM1 Ab (Wako)] and 23·4 ± 3·1 and 32·5 ± 6·1% macrophages (P = 0·081) [FITC-CD11b mAb (M1/70: PharMingen) and PE-anti-MHC class II mAb (M5/114·15·2: PharMingen)], respectively. These cells were cultured at 1 × 106/ml with various amounts of M. bovis BCG for 48 h, and the culture supernatants were collected and measured for the concentration of IL-12p40 and NO.
In vitro restimulation of spleen cells
Spleen cells were prepared from mice on day 8 after infection with M. tuberculosis and cultured at 2 × 106/ml with various doses of PPD for 48 h in RPMI1640 medium supplemented with 10% FCS. The culture supernatants were collected and assayed for concentrations of IFN-γ and IL-4 by enzyme-linked immunosorbent assay (ELISA).
Measurement of cytokines
The concentrations of IFN-γ, IL-4 and IL-12p40 in organ homogenates and culture supernatants were measured by specific ELISA kits [purchased from Endogen Inc. (Cambridge, MA, USA) for IFN-γ and IL-4 and from BioSource International, Inc. (Camarillo, CA, USA) for IL-12p40]. The detection limits of assays for IFN-γ, IL-4 and IL-12p40 were 15, 5 and 2 pg/ml, respectively.
Assay for NO
To estimate the synthesis of NO by PEC, the amount of nitrite, one of its metabolites, accumulated in the culture was measured as shown by Stuehr & Nathan [23]. Briefly, 100 µl of supernatant was mixed with the same volume of Griess reagent and absorbance was read at 550 nm using an automated microplate reader. Nitrite concentration was calculated from a NaNO2 standard curve.
Statistical analysis
Analysis of data was conducted using Statview II software (Abacus Concept, Inc., Berkeley, CA, USA) on a Macintosh computer. Data were expressed as mean ± standard deviation (SD). Statistical analysis between groups was performed using one-way analysis of variance (anova) test with a posthoc analysis (Fisher PLSD test). (Survival data is not shown in this study.) A P-value less than 0·05 was considered significant.
Results
Increased susceptibility to M. tuberculosis infection in diabetic mice
We first compared the clinical course of M. tuberculosis infection between diabetic and nondiabetic control mice. For this purpose, mice were infected 3 weeks after treatment with STZ or control vehicle, and the number of live bacteria in lung, liver and spleen was counted on days 14 and 35 postinfection. As shown in Table 1, the number of live bacteria on day 14 was significantly higher in the lung, liver and spleen of diabetic mice than that in control mice. Insulin treatment apparently prevented mice from the symptoms including polydypsia, diarrhoea and debility caused by diabetes mellitus (data not shown). The same treatment also improved the bacterial clearance in these organs, although the difference was not statistically significant in the lung and spleen (Table 1). On day 35, we obtained a similar result, although statistical significance was only detected in the lung and liver between diabetic and nondiabetic control mice.
Table 1.
Bacterial loads in diabetic mice.*
| Day 14† | Day 35† | |
|---|---|---|
| Lung | ||
| CNT | 5.10 ± 0.60 | 6.00 ± 0.52 |
| DM | 5.65 ± 0.28§ | 7.52 ± 0.63§ |
| DM/insulin | 5.28 ± 0.26¶ | 6.91 ± 0.39¶ |
| Liver | ||
| CNT | 6.46 ± 0.46 | 5.47 ± 0.56 |
| DM | 7.16 ± 0.26§ | 6.39 ± 0.75§ |
| DM/insulin | 6.43 ± 0.05** | 5.75 ± 0.27¶ |
| Spleen | ||
| CNT | 5.84 ± 0.45 | 4.88 ± 0.51 |
| DM | 6.32 ± 0.24§ | 5.49 ± 0.69‡ |
| DM/insulin | 6.06 ± 0.21¶ | 4.98 ± 0.22¶ |
Diabetic(DM) or Control (CNT) mice were infected with M. tuberculosis and DM mice received treatment with insulin. The number of live colonies in lung, liver and spleen on days 14 and 35 was measured.
Mean ± SD (CFU/organ) of 3 to 7 mice.
Not significant compared with CNT mice.
P < 0.05 compared with CNT mice.
Not significant compared with DM mice.
P < 0·05 compared with DM mice.
Production of Th1-related and Th2 cytokines in diabetic mice
The host defense to M. tuberculosis infection is mediated largely by cellular immunity [7], and Th1-related cytokines, including IL-12 and IFN-γ, play a critical role in the host protective responses [14–17], although the role of Th2 cytokines is not substantiated [7,19]. To investigate the mechanism of the increased susceptibility of diabetic mice to this pathogen, we compared the levels of IL-12, IFN-γ and IL-4 in the lung, liver and spleen on day 14 after M. tuberculosis infection between diabetic and control mice. As shown in Table 2, levels of IL-12 were significantly lower in the lung and spleen and tended to be lower in the liver of diabetic mice than those in control animals. Similarly, IFN-γ levels were significantly reduced in the liver and spleen of diabetic, compared with those in control animals, although the difference was not significant in the lung. Insulin treatment significantly restored the reduced levels of IL-12 in the lung and spleen, but not significantly on the liver of diabetic mice. Similar tendency was observed in the levels of IFN-γ by this treatment, although the difference was not statistically significant. On the other hand, levels of IL-4 were higher in the lung and liver of diabetic than nondiabetic control mice, although the difference was not significant in the lung. Insulin treatment tended to reduce the levels of IL-4 in the lung of diabetic mice. There was no difference observed in the spleen of three mouse groups.
Table 2.
Synthesis of cytokines in diabetic mice.*
| IL-12† | IFN-γ† | IL-4† | |
|---|---|---|---|
| Lung | |||
| CNT | 531 ± 245 | 11008 ± 8141 | 462 ± 62 |
| DM | 201 ± 105§ | 6015 ± 2482‡ | 736 ± 338‡ |
| DM/insulin | 418 ± 166** | 8899 ± 2697¶ | 575 ± 93¶ |
| Liver | |||
| CNT | 1025 ± 476 | 14263 ± 2392 | 997 ± 252 |
| DM | 728 ± 333‡ | 9307 ± 1363§ | 1995 ± 663§ |
| DM/insulin | 1190 ± 345¶ | 11209 ± 1664¶ | 1791 ± 734¶ |
| Spleen | |||
| CNT | 457 ± 222 | 7283 ± 2127 | 568 ± 107 |
| DM | 230 ± 49§ | 5355 ± 520§ | 533 ± 164‡ |
| DM/insulin | 497 ± 124** | 6462 ± 1017¶ | 480 ± 76¶ |
Diabetic(DM) or Control (CNT) mice were infected with M. tuberculosis and DM mice received treatment with insulin. The concentrations of the cytokines in lung, liver and spleen on day 14 were measured.
Mean ± SD (pg/organ) of 5 to 6 mice.
Not significant compared with CNT mice.
P < 0.05 compared with CNT mice.
Not significant compared with DM mice.
P < 0.05 compared with DM mice.
Low expression of iNOS in diabetic mice
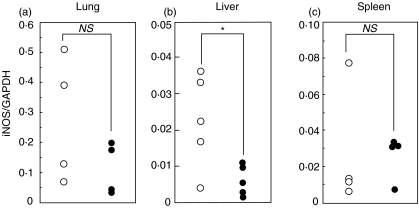
NO is known to act as a major effector molecule to kill M. tuberculosis by IFN-γ-activated macrophages [8,24] and to be essential for the host resistance to this infection [8,24–26]. iNOS, which catalyses the production of NO from l-arginine [27], is required to be expressed for the efficient eradication of this pathogen [26]. Therefore, using real-time RT-PCR, we investigated how iNOS mRNA induced by M. tuberculosis infection was affected by the diabetic condition. As shown in Fig. 1, the relative levels of iNOS expression on day 7 were significantly lower in the liver and tended to be lower in the lung of diabetic than nondiabetic control mice, although such tendency was not observed in the spleen.
Fig. 1.
Effect of diabetic condition on the expression of iNOS mRNA after M. tuberculosis infection. Diabetic and control mice were infected with M. tuberculosis. Total RNA was extracted from (a) lung, (b) liver and (c) spleen on day 7 postinfection, and real-time PCR was conducted to measure the expression of iNOS and GAPDH mRNA. The results are expressed as the relative values to GAPDH. Each symbol represents the result of each mouse. ○ control; • diabetic mice. NS, not significant; *P < 0·05, compared with control mice.
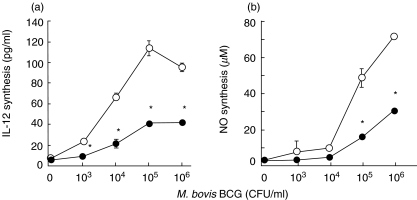
Effect of diabetes on synthesis of IL-12 and NO by PEC
To further define the effect of the diabetic condition on cytokine response, PEC from diabetic and nondiabetic control mice were stimulated in vitro with various doses of M. bovis BCG, and the concentrations of IL-12 in the culture supernatants were measured at 48 h after initiation of the cultures. As shown in Fig. 2, PEC from nondiabetic mice produced this cytokine in a dose-dependent manner, and such production was significantly reduced in diabetic mice. Furthermore, the concentrations of NO measured in the same culture supernatants were significantly lower in diabetic mice than those in controls.
Fig. 2.
Reduced production of (a) IL-12 and (b) NO by PEC in diabetic mice. PEC were prepared from diabetic and control mice on day 3 after intraperitoneal injection of M. bovis BCG. The cells were stimulated in vitro with various doses of M. bovis BCG for 48 h, and the concentrations of IL-12 and NO in the culture supernatants were measured. Each symbol represents the mean ± SD of triplicate cultures. ○ control; • diabetic mice. *P < 0·05, compared with control mice.
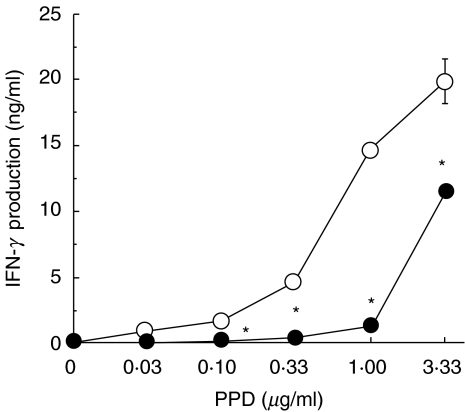
Impaired Th1 cell development in diabetic mice
We further examined the effect of diabetes on the development of Th1 cells caused by M. tuberculosis infection. For this purpose, spleen cells obtained from diabetic and control mice on day 8 postinfection were re-stimulated in vitro with various doses of PPD, and IFN-γ synthesis was compared between the two mouse groups. As shown in Fig. 3, IFN-γ was produced upon PPD re-stimulation in a dose-dependent manner, but not by stimulation with an unrelated protein, tetanus toxoid (data not shown). IFN-γ production was markedly reduced in spleen cells of diabetic mice compared with those from control mice. These results indicated that the development of Th1 cells specific for mycobacterial antigens was attenuated in diabetes mellitus.
Fig. 3.
Effect of diabetes on development of Th1 cells. Diabetic and control mice were infected with M. tuberculosis. Spleen cells were prepared on day 8 and re-stimulated with various doses of PPD for 48 h. The concentrations of IFN-γ in the culture supernatants were measured. Each symbol represents the mean ± SD of triplicate cultures. ○ control; • diabetic mice. *P < 0·05, compared with control mice.
In further experiments, we tested the effect of diabetes on the development of Th2 cells by measuring the synthesis of IL-4 from spleen cells upon re-stimulation with PPD. However, the re-stimulated spleen cells did not produce this cytokine at a detectable level in either diabetic or control mice (data not shown).
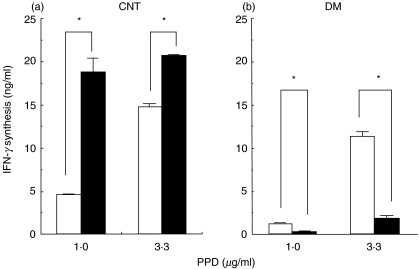
Effect of high glucose levels on in vitro production of IFN-γ by Th1 cells
In the next experiments, we tested whether high glucose concentrations influenced the in vitro synthesis of IFN-γ by PPD-re-stimulated spleen cells from mice infected with M. tuberculosis. As shown in Fig. 4, in diabetic mice, IFN-γ production was significantly less under high glucose conditions than in cultures with normal glucose levels. In sharp contrast, the high glucose cultures led to enhanced production of IFN-γ in nondiabetic mice. On the other hand, high glucose conditions did not have much influence on the synthesis of IL-12 and NO by M. bovis BCG-stimulated PEC between diabetic and control mice (data not shown). These results indicated that the short-term-high glucose exposure differentially affected in vitro IFN-γ production by Th1 cells specific for mycobacterial antigens in diabetic and nondiabetic mice, and suggested that high glucose conditions further exacerbated the impaired production of IFN-γ in diabetic mice.
Fig. 4.
Reduced production of IFN-γ by Th1 cells under high glucose conditions. (a) Control and (b) diabetic mice were infected with M. tuberculosis. Spleen cells were prepared on day 8 and re-stimulated with 1·0 and 3·3 µg/ml of PPD in high (33·3 m m) or normal (11·1 m m) glucose conditions for 48 h. The concentrations of IFN-γ in the culture supernatants were measured. Each bar represents the mean ± SD of triplicate cultures. □ normal; ▪ high glucose condition. CNT, control; DM, diabetic mice. *P < 0·05.
Discussion
The present study in an animal model of diabetes mellitus provides the first direct evidence of reduced expression of Th1-related cytokines and iNOS in response to M. tuberculosis in diabetes mellitus. This reduced expression correlated well with the impaired host resistance to this infection. In an earlier study, Saiki et al. [6] demonstrated that diabetic mice established by administration of STZ exhibited weaker delayed-type hypersensitivity to PPD and were more prone to M. tuberculosis infection than control nondiabetic mice. However, these findings were not followed-up to define the mechanism. Here, we extended these important observations by demonstrating the reduced expression of IL-12, IFN-γ and iNOS and the attenuated Th1 cell development in diabetic mice.
IFN-γ acts as a principle effector cytokine that plays a role in eradicating tubercle bacilli through the induction of a NO-mediated killing mechanism [14,15,24–26]. In some clinical investigations, tuberculosis patients with diabetes mellitus showed lower levels of serum IFN-γ and attenuated synthesis of this cytokine by peripheral blood mononuclear cells (PBMC) than did nondiabetic tuberculosis patients [20,21]. These previous observations raised the possibility that impaired synthesis of IFN-γ may be the mechanism accounting for hampered host resistance to M. tuberculosis infection under diabetic conditions. In the present study, we addressed this possibility using an animal model of diabetes mellitus. As predicted, diabetic mice produced lower amounts of IFN-γ in the liver and spleen after infection with this infectious pathogen than did nondiabetic control mice. In chronic infection like M. tuberculosis, antigen-specific Th1 cells are essential as the major source of IFN-γ production for the host defense [8]. In diabetic mice, the development of Th1 cells, as detected by IFN-γ production by spleen cells re-stimulated with PPD, was strongly inhibited compared with that in nondiabetic mice. Previous investigations found that the STZ-induced diabetic mice were susceptible to infection with Candida albicans, due to reduction and enhancement in the production of Th1 and Th2 cytokines, respectively [28,29]. They concluded that systemic candida infection became severe under the shifted balance of Th1-Th2 cytokine synthesis towards a Th2-dominant condition. Thus, similar mechanisms may underlie the increased susceptibility of diabetic animals to infection with M. tuberculosis and C. albicans, although the significance of Th2 cytokines remains elusive.
IL-12 induces the production of IFN-γ by innate immune lymphocytes and acts as an indispensable cytokine for the development of Th1 cells from naïve Th cells [9]. Quite compatible with this notion, diabetic mice showed reduced synthesis of IL-12 in the lung and spleen after infection with M. tuberculosis. From these results, the insufficient synthesis of IL-12 may be recognized as a principle cause rendering diabetic mice highly susceptible to this infection. Consistent with this, PEC from diabetic mice produced significantly lower amounts of IL-12 than those from control mice upon stimulation with M. bovis BCG. Similar observations were reported in clinical investigations [20,21], where serum levels of IL-12 and its production by PPD-stimulated PBMC were lower in tuberculosis patients with diabetic mellitus than those in nondiabetic tuberculosis patients. In very recent studies, M. tuberculosis was shown to deliver the signals for expression of IL-12 by macrophages and dendritic cells via toll-like receptors [30–32]. Therefore, such a signal delivering mechanism may be hampered under diabetic conditions. Further investigations will be necessary to address this possibility.
The bactericidal mechanism against M. tuberculosis is predominantly mediated by NO in rodents [8,24,25]. Mice with a targeted disruption of the iNOS gene are highly prone to infection with this bacterial pathogen [26]. Here, we demonstrated that expression of iNOS mRNA in the liver was reduced in diabetic mice compared with controls after M. tuberculosis infection and that NO synthesis by BCG-stimulated PEC from diabetic mice was significantly lower than that from control mice. The expression of iNOS by macrophages is critically regulated by IFN-γ[27]. Therefore, the reduced production of this cytokine was considered to cause hampered expression of iNOS under diabetic conditions.
Previously, Hill et al. [33] demonstrated that high glucose conditions depressed the release, but not production, of IL-1 by LPS-stimulated murine macrophages through activation of protein kinase C. Other investigations revealed the hyperglycaemia-induced suppression of iNOS in macrophages and smooth muscle cells [34,35]. These observations suggested that hyperglycaemia was involved in the dysregulation of host inflammatory responses. On this background, we tested the effect of high blood glucose levels on the synthesis of Th1-related cytokines and NO caused by mycobacterial infection. Interestingly, short-term hyperglycaemia resulted in the suppression of IFN-γ by PPD-re-stimulated Th1 cells, only in diabetic mice, whereas such an effect was not observed in nondiabetic control mice. In contrast, the synthesis of IL-12 and NO by BCG-stimulated PEC was not much affected by high glucose conditions in both diabetic and nondiabetic mice (data not shown). Thus, short-term hyperglycaemia may contribute to the aggravated infection with M. tuberculosis through reduction in synthesis of IFN-γ, although the precise mechanism remains to be elucidated.
Th2 cytokines, such as IL-4, interfere with Th1 responses by suppressing the synthesis of Th1-related cytokines and their action on target cells [36]. In some experimental models, Th2 cytokines have been demonstrated to counteract host resistance to several infectious pathogens [37–40]. The altered balance of Th1-Th2 responses towards a Th2-dominant condition is associated with an exacerbated clinical course of infectious diseases [41,42]. These observations raise the possibility that Th2 cytokines may contribute to the impaired host resistance against mycobacterial infection in diabetic conditions. Our results that IL-4 synthesis was higher in the liver of diabetic than nondiabetic mice are consistent with this possibility, although no convincing evidence has been provided to define the role of Th2 cytokines in the host defense to M. tuberculosis [7,19].
Finally, there is a possible involvement of streptozotocin itself, rather than diabetic condition, in the impaired host immune response against M. tuberculosis infection. To address this possibility, we tested the effect of insulin therapy on the host protective response in diabetic mice. This treatment lowered the blood glucose levels in these mice, which was associated with improved bacterial clearance and Th1 cytokine synthesis, although such recovery was partial. In addition, it should be noted that IL-4 synthesis was not suppressed, but rather increased, in diabetic mice after M. tuberculosis infection. These observations may provide evidences arguing against the nonspecific effect caused by this agent, although this possibility can’t be completely excluded.
In conclusion, in the present study, we have provided evidence accounting for the mechanism of attenuated host resistance to M. tuberculosis infection in hosts with diabetes mellitus by demonstrating reduced production of IL-12 and IFN-γ and hampered expression of iNOS in the infected tissues. Further studies are neccesary to determine the molecular mechanism(s) of the low expression of these molecules in diabetic conditions. Such studies should be also helpful for the development of efficient treatment and prevention of tuberculosis complicating patients with diabetic syndromes.
Acknowledgments
This work was supported in part by a Grant-in-aid for Science Research (C) (KAKENHI15591061) from the Ministry of Education, Culture, Sports, Science and Technology and by Grants from the Ministry of Health, Labor and Welfare, Japan.
References
- 1.Kim SJ, Hong YP, Lew WJ, Yang SC, Lee EG. Incidence of pulmonary tuberculosis among diabetics. Tuber Lung Dis. 1995;76:529–33. doi: 10.1016/0962-8479(95)90529-4. [DOI] [PubMed] [Google Scholar]
- 2.Yamagishi F. Medical risk factors of tuberculosis and countermeasures. Kekkaku. 2002;77:799–804. (in Japanese) [PubMed] [Google Scholar]
- 3.Delamaire M, Maugendre D, Moreno M, Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14:29–34. doi: 10.1002/(SICI)1096-9136(199701)14:1<29::AID-DIA300>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Naghibi M, Smith RP, Baltch AL, Gates SA, Wu DH, Hammer MC, Michelsen PB. The effect of diabetes mellitus on chemotactic and bactericidal activity of human polymorphonuclear leukocytes. Diabetes Res Clin Pract. 1987;4:27–35. doi: 10.1016/s0168-8227(87)80030-x. [DOI] [PubMed] [Google Scholar]
- 5.Wilson RM, Tomlinson DR, Reeves WG. Neutrophil sorbitol production impairs oxidative killing in diabetes. Diabet Med. 1987;4:37–40. doi: 10.1111/j.1464-5491.1987.tb00825.x. [DOI] [PubMed] [Google Scholar]
- 6.Saiki O, Negoro S, Tsuyuguchi I, Yamamura Y. Depressed immunological defence mechanisms in mice with experimentally induced diabetes. Infect Immun. 1980;28:127–31. doi: 10.1128/iai.28.1.127-131.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flynn JL, Chan J. Immunology of tuberculosis. Annu Rev Immunol. 2001;19:93–129. doi: 10.1146/annurev.immunol.19.1.93. [DOI] [PubMed] [Google Scholar]
- 8.Chan J, Xing Y, Magliozzo RS, Bloom BR. Killing of virulent Mycobacterium tuberculosis by reactive nitrogen intermediates produced by activated murine macrophages. J Exp Med. 1992;175:1111–22. doi: 10.1084/jem.175.4.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trinchieri G. Interleukin-12: a cytokine at the interface of inflammation and immunity. Adv Immunol. 1998;70:83–243. doi: 10.1016/s0065-2776(08)60387-9. [DOI] [PubMed] [Google Scholar]
- 10.Serbina NV, Flynn JL. Early emergence of CD8+ T cells primed for production of type 1 cytokines in the lungs of Mycobacterium tuberculosis-infected mice. Infect Immun. 1999;67:3980–8. doi: 10.1128/iai.67.8.3980-3988.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Serbina NV, Liu CC, Scanga CA, Flynn JL. CD8+ CTL from lungs of Mycobacterium tuberculosis-infected mice express perforin in vivo and lyse infected macrophages. J Immunol. 2000;165:353–63. doi: 10.4049/jimmunol.165.1.353. [DOI] [PubMed] [Google Scholar]
- 12.Lazarevic V, Flynn J. CD8+ T cells in tuberculosis. Am J Respir Crit Care Med. 2002;166:1116–21. doi: 10.1164/rccm.2204027. [DOI] [PubMed] [Google Scholar]
- 13.Samten B, Wizel B, Shams H, et al. CD40 ligand trimer enhances the response of CD8+ T cells to Mycobacterium tuberculosis. J Immunol. 2003;170:3180–6. doi: 10.4049/jimmunol.170.6.3180. [DOI] [PubMed] [Google Scholar]
- 14.Flynn JL, Chan J, Triebold KJ, Dalton DK, Stewart TA, Bloom BR. An essential role for interferon gamma in resistance to Mycobacterium tuberculosis infection. J Exp Med. 1993;178:2249–54. doi: 10.1084/jem.178.6.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cooper AM, Dalton DK, Stewart TA, Griffin JP, Russell DG, Orme IM. Disseminated tuberculosis in interferon gamma gene-disrupted mice. J Exp Med. 1993;178:2243–7. doi: 10.1084/jem.178.6.2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cooper AM, Magram J, Ferrante J, Orme IM. Interleukin 12 (IL-12) is crucial to the development of protective immunity in mice intravenously infected with mycobacterium tuberculosis. J Exp Med. 1997;186:39–45. doi: 10.1084/jem.186.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kinjo Y, Kawakami K, Uezu K, et al. Contribution of IL-18 to Th1 response and host defense against infection by Mycobacterium tuberculosis: a comparative study with IL-12p40. J Immunol. 2002;169:323–9. doi: 10.4049/jimmunol.169.1.323. [DOI] [PubMed] [Google Scholar]
- 18.Ottenhoff TH, Kumararatne D, Casanova JL. Novel human immunodeficiencies reveal the essential role of type-I cytokines in immunity to intracellular bacteria. Immunol Today. 1998;19:491–4. doi: 10.1016/s0167-5699(98)01321-8. [DOI] [PubMed] [Google Scholar]
- 19.North RJ. Mice incapable of making IL-4 or IL-10 display normal resistance to infection with Mycobacterium tuberculosis. Clin Exp Immunol. 1998;113:55–8. doi: 10.1046/j.1365-2249.1998.00636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsukaguchi K, Okamura H, Ikuno M, et al. The relation between diabetes mellitus and IFN-gamma, IL-12 and IL-10 productions by CD4+ alpha beta T cells and monocytes in patients with pulmonary tuberculosis. Kekkaku. 1997;72:617–22. (in Japanese) [PubMed] [Google Scholar]
- 21.Tsukaguchi K, Okamura H, Matsuzawa K, Tamura M, Miyazaki R, Tamaki S, Kimura H. Longitudinal assessment of IFN-gamma production in patients with pulmonary tuberculosis complicated with diabetes mellitus. Kekkaku. 2002;77:409–13. (in Japanese) [PubMed] [Google Scholar]
- 22.Kawakami K, Tohyama M, Qifeng X, Saito A. Expression of cytokines and inducible nitric oxide synthase mRNA in the lungs of mice infected with Cryptococcus neoformans: effects of interleukin-12. Infect Immun. 1997;65:1307–12. doi: 10.1128/iai.65.4.1307-1312.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuehr DJ, Nathan CF. Nitric oxide: a macrophage product responsible for cytostasis and respiratory inhibition in tumor target cells. J Exp Med. 1989;169:1543–55. doi: 10.1084/jem.169.5.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiloh MU, Nathan CF. Reactive nitrogen intermediates and the pathogenesis of Salmonella and Mycobacteria. Curr Opin Microbiol. 2000;3:35–42. doi: 10.1016/s1369-5274(99)00048-x. [DOI] [PubMed] [Google Scholar]
- 25.Flynn JL, Scanga CA, Tanaka KE, Chan J. Effects of aminoguanidine on latent murine tuberculosis. J Immunol. 1998;160:1796–803. [PubMed] [Google Scholar]
- 26.Ehlers S, Benini J, Held HD, Roeck C, Alber G, Uhlig S. Alphabeta T cell receptor-positive cells and interferon-gamma, but not inducible nitric oxide synthase, are critical for granuloma necrosis in a mouse model of mycobacteria-induced pulmonary immunopathology. J Exp Med. 2001;194:1847–59. doi: 10.1084/jem.194.12.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacMicking J, Xie QW, Nathan C. Nitric oxide and macrophage function. Annu Rev Immunol. 1997;15:323–50. doi: 10.1146/annurev.immunol.15.1.323. [DOI] [PubMed] [Google Scholar]
- 28.Mosci P, Vecchiarelli A, Cenci E, Puliti M, Bistoni F. Low-dose streptozotocin-induced diabetes in mice. I. Course of Candida albicans infection. Cell Immunol. 1993;150:27–35. doi: 10.1006/cimm.1993.1175. [DOI] [PubMed] [Google Scholar]
- 29.Mencacci A, Romani L, Mosci P, Cenci E, Tonnetti L, Vecchiarelli A, Bistoni F. Low-dose streptozotocin-induced diabetes in mice. II. Susceptibility to Candida albicans infection correlates with the induction of a biased Th2-like antifungal response. Cell Immunol. 1993;150:36–44. doi: 10.1006/cimm.1993.1176. [DOI] [PubMed] [Google Scholar]
- 30.Means TK, Jones BW, Schromm AB, et al. Differential effects of a Toll-like receptor antagonist on Mycobacterium tuberculosis-induced macrophage responses. J Immunol. 2001;166:4074–82. doi: 10.4049/jimmunol.166.6.4074. [DOI] [PubMed] [Google Scholar]
- 31.Reiling N, Holscher C, Fehrenbach A, Kroger S, Kirschning CJ, Goyert S, Ehlers S. Cutting edge. Toll-like receptor (TLR) 2- and TLR4-mediated pathogen recognition in resistance to airborne infection with Mycobacterium tuberculosis. J Immunol. 2002;169:3480–4. doi: 10.4049/jimmunol.169.7.3480. [DOI] [PubMed] [Google Scholar]
- 32.Heldwein KA, Fenton MJ. The role of Toll-like receptors in immunity against mycobacterial infection. Microbes Infect. 2002;4:937–44. doi: 10.1016/s1286-4579(02)01611-8. [DOI] [PubMed] [Google Scholar]
- 33.Hill JR, Kwon G, Marshall CA, McDaniel ML. Hyperglycemic levels of glucose inhibit interleukin 1 release from RAW 264.7 murine macrophages by activation of protein kinase C. J Biol Chem. 1998;273:3308–13. doi: 10.1074/jbc.273.6.3308. [DOI] [PubMed] [Google Scholar]
- 34.Tseng CC, Hattori Y, Kasai K, Nakanishi N, Shimoda S. Decreased production of nitric oxide by LPS-treated J774 macrophages in high-glucose medium. Life Sci. 1997;60:99–106. doi: 10.1016/s0024-3205(96)00683-2. [DOI] [PubMed] [Google Scholar]
- 35.Muniyappa R, Srinivas PR, Ram JL, Walsh MF, Sowers JR. Calcium and protein kinase C mediate high-glucose-induced inhibition of inducible nitric oxide synthase in vascular smooth muscle cells. Hypertension. 1998;31:289–95. doi: 10.1161/01.hyp.31.1.289. [DOI] [PubMed] [Google Scholar]
- 36.Mosmann TR, Sad S. The expanding universe of T-cell subsets. Th1, Th2 More Immunol Today. 1996;17:138–46. doi: 10.1016/0167-5699(96)80606-2. [DOI] [PubMed] [Google Scholar]
- 37.Kopf M, Brombacher F, Kohler G, et al. IL-4-deficient Balb/c mice resist infection with Leishmania major. J Exp Med. 1996;184:1127–36. doi: 10.1084/jem.184.3.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Padigel UM, Alexander J, Farrell JP. The role of interleukin-10 in susceptibility of BALB/c mice to infection with Leishmania mexicana and Leishmania amazonensis. J Immunol. 2003;171:3705–10. doi: 10.4049/jimmunol.171.7.3705. [DOI] [PubMed] [Google Scholar]
- 39.Decken K, Kohler G, Palmer-Lehmann K, Wunderlin A, Mattner F, Magram J, Gately MK, Alber G. Interleukin-12 is essential for a protective Th1 response in mice infected with Cryptococcus neoformans. Infect Immun. 1998;66:4994–5000. doi: 10.1128/iai.66.10.4994-5000.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blackstock R, Buchanan KL, Adesina AM, Murphy JW. Differential regulation of immune responses by highly and weakly virulent Cryptococcus neoformans isolates. Infect Immun. 1999;67:3601–9. doi: 10.1128/iai.67.7.3601-3609.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heinzel FP, Sadick MD, Holaday BJ, Coffman RL, Locksley RM. Reciprocal expression of interferon-gamma or interleukin-4 during the resolution or progression of murine leishmaniasis. Evidence for expansion of distinct helper T cell subsets. J Exp Med. 1989;169:59–72. doi: 10.1084/jem.169.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heinzel FP, Ahmed F, Hujer AM, Rerko RM. Immunoregulation of murine leishmaniasis by interleukin-12. Res Immunol. 1995;146:575–81. doi: 10.1016/0923-2494(96)83034-3. [DOI] [PubMed] [Google Scholar]