Abstract
Purpose
The objective of this study is to describe the authors’ results with intrastromal corneal ring segments (Intacs) and a new variation of lamellar keratoplasty, termed intralamellar keratoplasty (ILK), for the treatment of keratoconus (KCN) and post–laser-assisted in situ keratomileusis (LASIK) ectasia.
Methods
A retrospective review of contact lens–intolerant KCN and post-LASIK ectasia cases that had surgery with either Intacs or ILK was performed. The end points were mean uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), spherical equivalent (SE), manifest and topographic cylinder, and restoration of contact lens tolerance.
Results
Intacs were implanted in 13 keratoconic or post-LASIK ectasia eyes of 11 subjects. Mean UCVA improved by 1 line (range, −5 to +8); mean BCVA improved by 1 line (range, −1 to +4). Mean manifest SE was essentially unchanged. Mean manifest cylinder was reduced by 2.77 diopters (D), mean topographic cylinder was decreased by 2.29 D, and 12 of 13 eyes were successfully able to wear contact lenses. Four eyes with advanced KCN underwent ILK. Mean UCVA improved by 1 line (range, 0 to 12); mean BCVA improved by 4 lines (range, 1 to 10). Mean SE was lessened by 1.13 D. Mean manifest cylinder was reduced by 1.82 D and mean topographic cylinder by 1.14 D. Half the subjects were successfully fit with contact lenses.
Conclusion
Both Intacs and ILK improved mean UCVA, BCVA, and manifest and topographic astigmatism. In most cases, good contact lens fit was achieved with visual rehabilitation to levels that obviated penetrating keratoplasty.
INTRODUCTION
Keratoconus (KCN) is a noninflammatory ectatic condition in which the cornea assumes a conical shape due to weakness, thinning, and anterior protrusion of the corneal surface.1–3 A similar clinical entity, post–laser-assisted in situ keratomileusis (LASIK) ectasia, is sometimes seen in patients following LASIK procedure who have subsequent progressive corneal thinning and bulging, with topography similar to KCN.
The refractive error caused by the ectatic cornea is initially managed with either spectacles or contact lenses. When ectasia progresses to the point where contact lenses no longer provide useful vision, then surgical intervention may be considered. Penetrating keratoplasty is the most commonly performed surgical procedure for ectatic corneas, but is associated with complications including graft rejection,4 induced astigmatism, complications of intraocular surgery such as glaucoma, cataract formation, retinal detachment, cystoid macular edema, endophthalmitis, and expulsive hemorrhage. To avoid these complications, new methods such as lamellar keratoplasty (LKP) 5,6 and intrastromal corneal ring segments (Intacs; Micro-Thin Prescription Inserts; Addition Technologies, Fremont, California) have evolved. LKP has the advantages of being extraocular and reversible if tissue complications occur. Another advantage includes the ability to replace only selected areas of diseased corneal tissue with healthy donor tissue. LKP results, however, may be limited by vision-reducing graft-host interface problems and the technical nature of the surgical procedure.7 Intacs, which were initially used to correct low myopia,8,9 have been shown to improve vision in both KCN2,3,10–12 and post-LASIK ectasia.13–17
The objective of this study is to report the results with Intacs and our variation of the LKP procedure, Intralamellar keratoplasty (ILK), in the treatment of both KCN and post-LASIK ectasia.
METHODS
A retrospective review of the authors’ KCN and post-LASIK ectasia cases, which underwent surgery between June 2002 and October 2005, was performed. All subjects had clear central corneas, had clinical evidence of progression of the disease, and were contact lens–intolerant. KCN and post-LASIK ectasia were diagnosed by slit-lamp signs and videokeratography. Intacs surgery was performed in KCN or post-LASIK ectasia patients who had mild inferior oval sagging cones. The ILK procedure was performed in patients with severe central ectatic cones.
SURGICAL TECHNIQUE
Intacs
An informed consent was obtained prior to surgery. In the early cases, the data accumulation was in conformity with all federal and state laws and specifically Health Insurance Portability and Accountability Act (HIPAA) guidelines. In the cases performed after 2004, the informed consent followed the guidelines of the Humanitarian Device Exemption protocol for the use of Intacs in KCN and the data accumulation was supervised by the Human Rights and Protections Program/IRB at the University of California, San Diego. The surgery was performed under topical anesthesia, proparacaine 0.5%, and all procedures were performed by the same surgeon (D.S.). The first two cases were performed with standard Intacs procedure using asymmetric-sized Intacs segments (0.3 5 mm superiorly and 0.25 mm inferiorly).
Standard Intacs Procedure
The geometric center of the cornea was marked with a blunt Sinskey hook. A pre-inked marker was centered on the cornea to provide a visual guide for the placement of the incision at the steep corneal meridian, at a 7-mm optical zone. Corneal pachymetry (PachetteTM; DGH Technology, Exton, Pennsylvania) was performed over the site of the peripheral incision, and a 15° diamond knife was used to make a 1.2-mm incision at a depth of 67% of the pachymetry reading overlying the corneal incision mark. A modified Suarez spreader was used to begin a lamellar corneal dissection. Specially designed dissecting instruments (Addition Technology, Fremont, California) were inserted into the incision to create curved peripheral corneal tunnels. The intrastromal tunnels were prepared using clockwise and counterclockwise dissecting instruments. Each of the Intacs was manually rotated into the tunnel until the desired position was reached. The incision was closed using a single 10-0 nylon suture. The surgical eye then received topical prednisolone acetate 1%, topical tobramycin, and a clear shield.
Intacs With Femtosecond Laser
In the subsequent 11 cases, the femtosecond laser (Intralase Corp, Irvine, California) was used to create the channels. The same-sized Intacs segments (0.35 mm) were implanted. The following laser settings were used: channel depth was two thirds the corneal thickness, entry incision length was 1.2 mm, entry incision width was 5 μm, channel size inner diameter was 6.8 mm, and the outer diameter was 7.4 to 7.6 mm. The entry wound was opened with a blunt Sinskey hook. Each of the Intacs was then manually rotated into the tunnel until the desired position was reached. The incision was closed using a single 10-0 nylon suture. The surgical eye then received topical prednisolone acetate 1%, topical tobramycin, and a clear shield.
INTRALAMELLAR KERATOPLASTY
An informed consent was obtained for lamellar corneal transplantation surgery. The data accumulation was in conformity with all federal and state laws and specifically HIPAA guidelines. The donor stromal lenticule was created using the Intralase. Human globes were acquired from the San Diego Eye Bank (San Diego, California). A spiral pattern method was used, with 2.1 μJ spiral energy and 3.1 μJ side-cut energy. The laser parameters were set to cut the first lamellar interface at a depth of 400 μm posterior to the epithelial surface. The diameter of the lamellar cut was 9 mm. A side cut was then performed creating a tapered edge to the lenticule. Then, a second superficial lamellar cut was made at a depth of 150 μm posterior to the epithelial surface. This produced a 250-μm donor corneal lamellar disc.
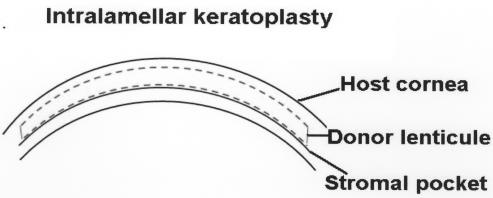
Next, a stromal pocket was formed in the host cornea at a depth of 250 μm using the Intralase. The diameter of the pocket was 9.5 mm, with a 3.0-mm exit incision at the 12 o’clock position (Figure 1).
FIGURE 1.
Diagram illustrating the intralamellar pocket created by femtosecond laser (Intralase) in the host cornea and a sketch of the stromal pocket cut.
The patient was then taken to the operating room where after standard preparation with povidone-iodine 10% solution and placement of a sterile drape, a lid speculum was inserted to hold the eyelids apart. The donor lamellar lenticule was removed using simple manual dissection. The host corneal pocket was prepared by opening the superior incision with a Sinskey hook and opening the stromal pocket with a Martinez spatula. The donor lamellar lenticule was folded and inserted into the recipient stromal pocket through the anterior incision (Figure 2). The donor lenticule was centered and smoothed with a cyclodialysis spatula. The wound was closed with a single 10-0 nylon suture.
FIGURE 2.
Cross section of the cornea showing the donor lenticule inside the host corneal pocket for the intralamellar keratoplasty procedure.
Follow-Up
The patients were seen for surgical follow-up at day 1, week 1, month 1, month 3, and month 6. For this retrospective analysis, results at 3 months and 6 months postoperatively were reviewed and analyzed. Uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), manifest refraction, topography, contact lens tolerance, and incidence of major complications were assessed at these visits.
Visual Acuity
Visual acuity was measured using the Snellen chart at 20 feet and transformed into logarithm of the minimum angle of resolution (logMAR) for further statistical analysis as recommended by Holladay.18 Visual acuity data are expressed as logMAR ± standard deviation (SD; Snellen value).
Refractive Outcome
The refractive outcome was assessed with a phoropter manifest refraction using standard refraction techniques. The sphere, cylinder, axis of the cylinder, and the spherical equivalent (SE) of the refraction were tabulated.
Corneal Topography
Corneal topography was assessed using the Orbscan (Bausch & Lomb, Rochester, New York). The simulated keratometry values (K1 and K2) and astigmatism were tabulated.
Contact Lens Tolerance
Contact lenses were fit by an optometrist skilled in fitting KCN eyes. The optometrist determined the appropriate type of contact lens and measured the best-corrected vision with the lens.
Complications
The patient’s charts were reviewed for any incidence of major complications, including infections, interface scarring or haze, lamellar graft rejection, Intacs segment extrusion, Intacs channel haze, and lamellar channel deposits.
Statistical Analysis
Statistical analysis with Statistica software version 5.0 was used to calculate the basic descriptive statistics including the mean and standard deviation. In the analysis of the Intacs group, statistical significance (P < .05) was reported based on the nonparametric Wilcoxon test. In the ILK group, statistical significance was not assessed owing to the small sample size.
RESULTS
INTACS GROUP
Patient Population
Thirteen eyes of 11 patients were treated with Intacs. Eight of the eyes from seven patients had post-LASIK ectasia, whereas five of the eyes from four patients had KCN. Seven of the patients were male and four were female. The mean age of these patients was 46.8 ± 11.47 years (range, 28 to 67). The eyes in this group had mild inferior cones with the mean UCVA, BCVA, SE, and manifest and topographic cylinder as shown in Table 1.
TABLE 1.
MEAN PREOPERATIVE DATA IN INTACS GROUP
| PARAMETERS | MEAN | ±SD |
|---|---|---|
| Age | 46.8 | 11.47 |
| UCVA* | 1.1 (20/250) | 0.42 |
| BCVA* | 0.3 (20/40) | 0.19 |
| Mean SE (D) | −2.66 | 3.68 |
| Mean manifest cylinder (D) | 4.67 | 1.33 |
| Mean topographic cylinder (D) | 5.48 | 2.33 |
BCVA = best corrected visual acuity; D = diopters; Intacs = intrastromal corneal ring segment; SD = standard deviation; SE = spherical equivalent; UCVA = uncorrected visual acuity.
In logMAR values (Snellen acuity).
Visual Acuity
The mean preoperative UCVA improved from 1.10 ± 0.42 (20/250) to 0.88 ± 0.52 (20/150) 3 months after the procedure (P = .06), and to 1.0 ± 0.44 (20/200) at 6 months (P = .22). One eye lost 5 lines of UCVA, eight maintained the preoperative UCVA, and four gained 1 to 8 lines of UCVA at 6 months follow-up. There was a mean gain of 1 line UCVA from preoperative to the last follow-up at 6 months.
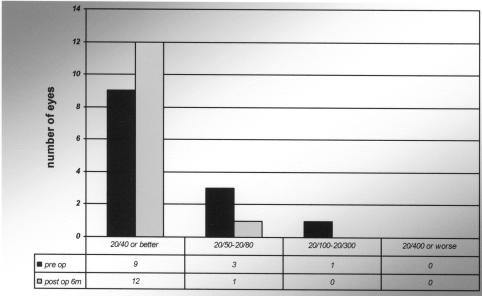
The mean BCVA improved from 0.30 ± 0.19 (20/40) to 0.20 ± 0.16 (20/32) at 3 months (P = .32) and to 0.20 ± 0.14 (20/32) at 6 months postoperatively (P = .12). Four eyes lost 1 to 2 lines of BCVA, one maintained the preoperative BCVA, and eight gained 1 to 4 lines of BCVA at 6 months (Figure 3). There was a mean gain of 1 line BCVA from preoperative to the last follow-up at 6 months.
FIGURE 3.
Intrastromal corneal ring segments group. Comparison between preoperative best-corrected visual acuity (BCVA) and postoperative BCVA at 6 months
Refractive Outcome
The mean manifest SE remained essentially unchanged from a preoperative value of −2.66 diopters (D) to −2.36 D at 3 months and −2.61 D at 6 months postoperatively (P = .55, P =.58, respectively).
The mean manifest refractive cylinder decreased from 4.67 D preoperatively to 2.0 D at 3 months postoperatively (P = .003) and to 1.90 D at 6 months postoperatively (a reduction of 2.77 D from preoperative to 6 months postoperative; P = .003) (Table 2).
TABLE 2.
COMPARISON BETWEEN MEAN PREOPERATIVE AND 6 MONTHS POSTOPERATIVE DATA IN INTACS GROUP
| PREOPERATIVE | POSTOPERATIVE 6 MO | |||
|---|---|---|---|---|
| PARAMETERS | MEAN | ± SD | MEAN | ±SD |
| UCVA* | 1.1 (20/250) | 0.42 | 1.0 (20/200) | 0.44 |
| BCVA* | 0.30 (20/40) | 0.19 | 0.20 (20/32) | 0.14 |
| Mean SE (D) | −2.66 | 3.68 | −2.61 | 3.23 |
| Mean manifest cylinder (D) | 4.67 | 1.33 | 1.90 | 1.50 |
| Mean topographic cylinder (D) | 5.48 | 2.33 | 3.19 | 2.0 |
BCVA = best corrected visual acuity; D = diopters; Intacs = intrastromal corneal ring segments; SD = standard deviation; SE = spherical equivalent; UCVA = uncorrected visual acuity.
In logMAR values (Snellen acuity).
Topography
The mean topographic astigmatism decreased from 5.48 D preoperatively, to 3.44 D at 3 months (P = .055), and 3.19 D at 6 months postoperatively (a reduction of 2.29 D at 6 months postoperatively; P = .01) (Table 2).
Contact Lens Tolerance
Eleven of the 13 eyes (84.6%) were contact lens tolerant at 3 months. At 6 months after Intacs implantation, 12 of 13 (92.3%) were successfully fit with contact lenses. Of these 12 eyes, seven (58%) had soft toric lenses, two (17%) had rigid gas permeable lenses, and the remaining three (25%) had hybrid contact lenses.
Complications
There were no major complications seen in this series of patients.
ILK GROUP
Patient Population
Four eyes of four patients were treated with ILK. Three of the patients were male and one was female. The mean age of these patients was 39 ± 12.5 years (range, 28 to 52). Eyes in this group had severe central cones with mean UCVA, BCVA, SE, and manifest and topographic cylinder as shown in Table 3.
TABLE 3.
MEAN PREOPERATIVE DATA IN INTRALAMELLAR KERATOPLASTY GROUP
| PARAMETERS | MEAN | ±SD |
|---|---|---|
| Age | 39 | 12.5 |
| UCVA* | 1.3 (20/400) | 0.47 |
| BCVA* | 0.88 (20/150) | 0.34 |
| Mean SE (D) | −10.38 | 5.39 |
| Mean manifest cylinder (D) | 3.5 | 4.17 |
| Mean topographic cylinder (D) | 6.35 | 1.89 |
BCVA = best corrected visual acuity; D = diopters; SD = standard deviation; SE = spherical equivalent; UCVA = uncorrected visual acuity.
In logMAR values (Snellen acuity).
Visual Acuity
The mean UCVA improved from a preoperative value of 1.3 ± 0.47 (20/400) to 1.0 ± 0.29 (20/200) at 3 months and to 1.1 ± 0.15 (20/250) at 6 months postoperatively. No eye lost lines of UCVA, three maintained the preoperative UCVA, and one eye gained 5 lines of UCVA after 6 months. There was a mean gain of 1 line of UCVA between preoperative to 6 months.
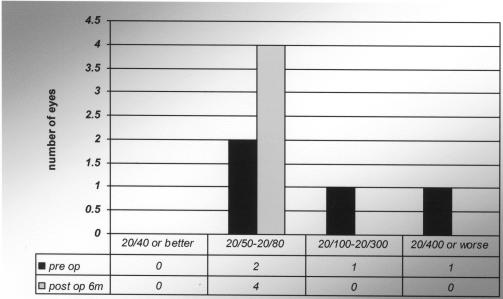
The mean BCVA also improved from 0.88 ± 0.34 (20/150) preoperatively, to 0.40 ± 0.09 (20/50) at 3 months and to 0.48 ± 0.06 (20/60) at 6 months postoperatively. All eyes gained between 1 and 8 lines of BCVA at 6 months (Figure 4). There was a mean gain of 4 lines of BCVA from preoperative to 6 months.
FIGURE 4.
Intralamellar keratoplasty group. Comparison between preoperative best-corrected visual acuity (BCVA) and postoperative BCVA at 6 months
Refractive Outcome
The mean manifest SE was improved from −10.38 D preoperatively, to −8.82 D at 3 months, and −9.25 D at 6 months postoperatively (a reduction of 1.13 D at 6 months postoperatively). The mean manifest refractive cylinder decreased from 3.5 D preoperatively, to 2.25 D at 3 months, and 1.68 D at 6 months postoperatively (a reduction by 1.82 D, 6 months postoperatively) (Table 4).
TABLE 4.
COMPARISON BETWEEN MEAN PREOPERATIVE AND 6 MONTHS POSTOPERATIVE DATA IN INTRALAMELLAR KERATOPLASTY GROUP
| PREOPERATIVE | POSTOPERATIVE 6 MO | |||
|---|---|---|---|---|
| PARAMETER | MEAN | ± SD | MEAN | ± SD |
| UCVA* | 1.3 (20/400) | 0.47 | 1.10 (20/250) | 0.15 |
| BCVA* | 0.88 (20/150) | 0.34 | 0.48 (20/60) | 0.06 |
| Mean SE (D) | −10.38 | 5.39 | −9.25 | 5.12 |
| Mean manifest cylinder (D) | 3.5 | 4.17 | 1.68 | 2.89 |
| Mean topographic cylinder (D) | 6.35 | 1.89 | 5.21 | 2.52 |
BCVA = best corrected visual acuity; D = diopters; SD = standard deviation; SE = spherical equivalent; UCVA = uncorrected visual acuity.
In logMAR values (Snellen acuity).
Topography
The mean topographic astigmatism was relatively unchanged from the preoperative value of 6.35 D to 6.23 D at 3 months, but was improved to 5.21 D at 6 months (a reduction of 1.14 D, 6 months postoperatively) (Table 4).
Contact Lens Tolerance
Two of the four eyes were able to wear contact lenses after the ILK procedure.
Complications
There were no major complications seen in this series of patients.
DISCUSSION
Surgical techniques are evolving for the treatment of KCN and post-LASIK ectasia. Intacs2,19–21 and new LKP procedures5,6,22,23 are developing to decrease the corneal ectasia and provide visual rehabilitation with spectacles or contact lenses.
This study involved keratoconic and post-LASIK ectasia eyes that underwent same-thickness, double-segment Intacs placement. The UCVA in 12 of the 13 cases (92%) were either stable or improved from preoperative values to 6 months. Four (30.7%) eyes gained lines of improvement in UCVA, and eight (61.5%) eyes achieved similar improvements in BCVA at 6 months. These findings were similar to the results reported by other investigators using two symmetric-sized segments,15 asymmetric-sized segments,10 and only one segment.17 Although the SE in the patients in this series decreased minimally at 3 months and remained essentially unchanged at 6 months follow-up, a significant reduction was found in manifest and topographic cylinder, 2.75 D and 2.29 D, respectively, similar to work reported by Colin and associates2 and Kanellopoulos and colleagues.19 The reduction of the astigmatic component of the refraction in the patients allowed 12 of the 13 eyes (93%) to be fit with contact lenses at 6 months postoperatively, with all patients achieving a BCVA > 20/40. Furthermore, seven (58%) of these 12 contact lens–tolerant eyes were able to wear soft toric lenses, three (25%) had hybrid contact lenses, and only two (17%) needed rigid gas permeable lenses. These results reflect the function of Intacs as a biomechanical-tectonic procedure, facilitating contact lens fit.1,24
The preliminary results of our LKP variation, termed ILK, are also described. At 6 months follow-up, no eye lost lines of UCVA. Notably, a mean gain of 4 lines of BCVA was documented, as well as an improvement in SE and manifest and topographic cylinder. Postoperatively, contact lenses could be fit in two of the four patients who were intolerant prior to surgery. One of the contact lens–intolerant patients was comfortable with his UCVA, and the last patient was mildly retarded and therefore unable to wear a contact lens. No major complications were detected in this procedure.
In conclusion, in the series of patients reported here, both Intacs and ILK appear to be safe and effective surgical procedures for the treatment of ectatic and KCN eyes with clear central corneas. In both groups, the mean UCVA, BCVA, refractive cylinder, and keratometric readings were all improved. The majority of patients were visually rehabilitated with contact lenses or spectacles, obviating the need for penetrating keratoplasty.
Nonetheless, Intacs and ILK are new approaches to the treatment of corneal ectatic disorders. Conclusions from our experience are limited by the small number of cases and by the retrospective nature of this study. Ultimately, larger case series and longer follow-up are needed to draw definitive conclusions regarding the efficacy of these procedures in the management of KCN and post-LASIK ectasia.
PEER DISCUSSION
DR JAY H. KRACHMER
The authors present two different methods for treating specific situations in which there is thinning and protrusion of a clear cornea. One clinical presentation occurs when a patient with advanced keratoconus is unable to wear contact lenses. In my experience, patients with advanced keratoconus usually also have scarring requiring penetrating keratoplasty. Occasionally the cornea is clear enough to allow for another surgical approach. In this study, Intacs where placed in five eyes and a new surgical procedure, Intralamellar Keratoplasty, was performed in four eyes. The other clinical situation is a complication of LASIK refractive surgery in which progressive thinning and protrusion of the operated cornea occurs. Intacs were placed in eight eyes with that complication. Intralamellar keratoplasty was not used for post-LASIK corneal ectasia.
In general, uncorrected visual acuities and best corrected visual acuities improved as compared to preoperatively. In my practice, patients who had penetrating keratoplasty for keratoconus and wear contact lenses have better visual acuity than reported in this study. The advantages, however, of these procedures over an intraocular procedure with the potential of rejection, are obvious.
The issue of contact lens intolerance and the ability to wear contact lenses is not a simple one. In this study, nearly all patients who were preoperatively intolerant to contact lenses could wear them after surgery. Studies in which contact lens wear is measured before and after procedures need to take into account the motivation and skills of the contact lens fitter and follow-up period for each patient. Some contact lens fitters give up far earlier than others. They might have less skill and experience fitting difficult cases such as those in this study. Other contact lens fitters with a great deal of experience and motivation are extremely reluctant to accept defeat. Their patients might wear multiple lenses on one eye with multiple eye drops and variable wearing times and are considered successful. Were contact lens fitters with these characteristics involved in the preoperative period? It is impressive that such a high percentage were tolerant of contact lenses. Could the same fitter have been successful preoperatively?
The authors recognize that this was a retrospective study with only a six-month follow-up period. After one or two years, will the patients still be able to wear contact lenses? Will there be any deterioration of uncorrected and/or best-corrected visual acuities? Will there be interface scarring in those patients that underwent Intralamellar Keratoplasty? Will there be irregular astigmatism requiring the use of contact lenses? Will there be extrusion of Intacs?
Another weakness of the study, also recognized by the authors, is the small number of cases. Of course, small numbers are appropriate with new procedures.
In this study, the authors have presented alternative methods for correcting vision in specific clinical settings of corneal thinning and protrusion. I applaud their quest for innovative methods for helping such patients.
DR JAMES P. MCCULLEY
I would like you to comment on the possible future of corneal incision surgery and whether you think lasers are going to almost totally replace blades.
DR DOUGLAS D. KOCH
You really have two groups of patients, post-LASIK ectasias and keratoconus. Did you feel that there was any difference between these groups despite the small number of patients? What ring dimensions did you use in this study? How did you determine where you placed them?
DR RICHARD C. TROUTMAN
What did the topography show pre- and post-operatively as this might tell us whether the astigmatism was controlled, and also whether the corneal myopia, which is the biggest aspect of keratoconus in the post-operative correction of vision, was controlled.
DR DAVID J. SCHANZLIN
Certainly the issue of contact lens intolerance is a variable that needs to be controlled. In this study it was controlled in that all cases referred to me were sent to our expert in keratoconus fitting. She performed the pre-op fittings and post-operative fittings. I should note that during this same period of time, there were 70 patients referred in with keratoconus or post-LASIK ectasia who were specifically referred for these procedures yet we only ended up with 17. We were able to fit lenses in well over two-thirds of those patients.
What will be the long-term follow-up? With the Intacs you see a very stable result between three months and six months after surgery. With topography you see the red bulge decreases in size, and you get flattening and more regularity of the astigmatism, but you do not eliminate it. So you can get them into a soft toric contact lens frequently but sometimes it still takes a Rigid Gas Permeable lens, although it fits better post-operatively.
We have not seen interface scarring that at six months, though that is a concern with any lamellar procedure. Here you have two interfaces that could become opaque. What limits the visual acuity in these cases is that you are adding a thick piece of tissue and you have left Bowman Membrane intact, so you are causing posterior curvature changes of the cornea and this is what’s limiting us currently on the 20/60 level. We have not seen extrusion of Intacs but that is a concern, especially if the Intacs are replaced in a shallow fashion. If you keep them at a two-thirds depth, which is not been a problem given the entire worldwide experience with Intacs.
Concerning the future of lasers versus blades in keratoconus, certainly studies are underway using the Intralase to make our penetrating grafts with top hat type of incisions. If you are referring to using Intralase for LASIK cases versus blades, that’s a different question. In my opinion it will occur as well.
Dr. Koch asked about the two different groups of patients. The severe keratoconus are the ones we have approached with the intra-lamellar keratoplasty technique and the milder keratoconus are the ones we’ve been able to treat with Intacs. And you can make that assessment based on the topography ahead of time.
Dr. Troutman’s comments about the topography and the need to talk to the patients ahead of time that these procedures will not eliminate their need for contact lenses. We cannot guarantee that you will be stable over time, although we are gathering data that at least the Intacs do appear stable. When we look at the topography, the bulge is decreased in size, and it begs the question, if we can get a stable topography with a smaller bulge that can be encompassed within a PRK treatment, can we ultimately shave off the irregular part of the cornea, and ultimately have a total rehabilitation of some of these patients? We are not there yet, but that is certainly a direction that this research may take us.
REFERENCES
- 1.Ucakhan OO, Kanpolat A, Ozdemir O. Contact lens fitting for keratoconus after Intacs placement. Eye Contact Lens. 2006 Mar;32:75–77. doi: 10.1097/01.icl.0000174749.96423.ca. [DOI] [PubMed] [Google Scholar]
- 2.Colin J, Cochener B, Savary CB, et al. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 3.Colin J, Savary CB, Malet G, et al. Intacs inserts for treating keratoconus: one year results. Ophthalmology. 2001;108:1409–1414. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 4.Thompson RW, Jr, Price MO, Bowers PJ, et al. Long term graft survival after penetrating keratoplasty. Ophthalmology. 2003;110:1396–1402. doi: 10.1016/S0161-6420(03)00463-9. [DOI] [PubMed] [Google Scholar]
- 5.Alio JL, Shah S, Barraquer C, et al. New techniques in lamellar keratoplasty. Curr Opin Ophthalmol. 2002;13:224–229. doi: 10.1097/00055735-200208000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Shimazaki J, Shimmura S, Ishioka M, et al. Randomized clinical trial of deep lamellar keratoplasty vs penetrating keratoplasty. Am J Ophthalmol. 2002;134:159–165. doi: 10.1016/s0002-9394(02)01523-4. [DOI] [PubMed] [Google Scholar]
- 7.Soong HK, Katz DG, Farjo AA, et al. Central lamellar keratoplasty for optical indications. Cornea. 1999;18:249–256. doi: 10.1097/00003226-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Nose W, Neeves RA, Burris TE, et al. Intrastromal corneal ring: 12-month sighted myopic eyes. J Refract Surg. 1996;12:20–28. doi: 10.3928/1081-597X-19960101-08. [DOI] [PubMed] [Google Scholar]
- 9.Schanzlin DJ, Asbell PA, Burris TE, et al. The intrastromal corneal ring segments: phase II results for the correction of myopia. Ophthalmology. 1997;104:1067–1078. doi: 10.1016/s0161-6420(97)30183-3. [DOI] [PubMed] [Google Scholar]
- 10.Boxer Wachler BS, Christie JP, Chandra NS, et al. Intacs for keratoconus. Ophthalmology. 2003;110:1031–1040. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 11.Siganos CS, Kymionis GD, Kartakis N, et al. Management of keratoconus with Intacs. Am J Ophthalmol. 2003;35:64–70. doi: 10.1016/s0002-9394(02)01824-x. [DOI] [PubMed] [Google Scholar]
- 12.Levinger S, Pokroy R. Keratoconus managed with Intacs: one-year results. Arch Ophthalmol. 2005;123:1308–1314. doi: 10.1001/archopht.123.10.1308. [DOI] [PubMed] [Google Scholar]
- 13.Siganos CS, Kimiyonis GD, Astyrakakis N, et al. Management of corneal ectasia after laser in situ keratomileusis with INTACS. J Refract Surg. 2002;18:43–46. doi: 10.3928/1081-597X-20020101-06. [DOI] [PubMed] [Google Scholar]
- 14.Alio J, Salem T, Artola A. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1568–1574. doi: 10.1016/s0886-3350(01)01275-5. [DOI] [PubMed] [Google Scholar]
- 15.Kymionis GD, Siganos CS, Kounis G, et al. Management of post-LASIK corneal ectasia with Intacs inserts. Arch Ophthalmol. 2003;121:322–326. doi: 10.1001/archopht.121.3.322. [DOI] [PubMed] [Google Scholar]
- 16.Lovisolo CF, Flemming JF. Intracorneal ring segments for iatrogenic keratectasia after laser in situ keratomileusis or photorefractive keratectomy. J Refract Surg. 2002;18:535–541. doi: 10.3928/1081-597X-20020901-08. [DOI] [PubMed] [Google Scholar]
- 17.Pokroy R, Levinger S, Hirsh A. Single Intacs segment for post-LASIK keratectasia. J Cataract Refract Surg. 2004;30:1685–1695. doi: 10.1016/j.jcrs.2004.02.050. [DOI] [PubMed] [Google Scholar]
- 18.Holladay JT. Visual acuity measurements. J Cataract Refract Surg. 2004;30:287–290. doi: 10.1016/j.jcrs.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: efficacy and complications. Cornea. 2006;25:29–33. doi: 10.1097/01.ico.0000167883.63266.60. [DOI] [PubMed] [Google Scholar]
- 20.Levinger S, Pokroy R. Keratoconus managed with Intacs: one-year results. Arch Ophthalmol. 2005;123:1308–1314. doi: 10.1001/archopht.123.10.1308. [DOI] [PubMed] [Google Scholar]
- 21.Sharma M, Boxer Wachler B. Comparison of single-segment and double-segment Intacs for keratoconus and post-LASIK ectasia. Am J Ophthalmol. 2006;141:891–895. doi: 10.1016/j.ajo.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 22.Bilgihan K, Ozdek SC, Sari A, et al. Microkeratome-assisted lamellar keratoplasty for keratoconus: stromal sandwich. J Cataract Refract Surg. 2003;29:1267–1272. doi: 10.1016/s0886-3350(02)02055-2. [DOI] [PubMed] [Google Scholar]
- 23.Panda A, Bageshwar LM, Ray M, et al. Deep lamellar keratoplasty vs penetrating keratoplasty for corneal lesions. Cornea. 1999;18:172–175. doi: 10.1097/00003226-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Nepomuceno RL, Boxer Wachler BS, Weissman BA. Feasibility of contact lens fitting on keratoconus patients with INTACS inserts. Cont Lens Ant Eye. 2003;26:175–180. doi: 10.1016/S1367-0484(03)00049-3. [DOI] [PubMed] [Google Scholar]