Abstract
Purpose
To evaluate the effect of refractive error management on resolution of accommodative esotropia, deterioration of accommodative esotropia, and the natural history of hypermetropia in accommodative esotropia.
Methods
Retrospective cohort study and nested case-control study of patients with accommodative esotropia untreated prior to diagnosis by the author. Eligibility criteria included esodeviation of ≥10 prism diopters (PD) on distance and near fixation on initial examination, hypermetropia, distance esodeviation <10 PD with full cycloplegic refraction correction on first follow-up examination, and at least 2 years of follow-up.
Results
The study included 285 patients with mean follow-up of 102 months. After age 7 years, mean annual decrease in hypermetropia was .24 D for patients wearing full cycloplegic refraction and for patients in whom hypermetropia was undercorrected by 1.00 D or more. Age at diagnosis (P < .0001), oblique muscle dysfunction (P < .0001), and abnormal distance-near relationship (P = .007) were associated with deterioration of accommodative esotropia. Of 51 patients with an intermittent abnormal distance-near relationship, 19 (37%) had increased hypermetropia on cycloplegic refraction, and prescription of the increased correction normalized the distance-near relationship.
Conclusions
The possibility that undercorrecting hypermetropia speeds its resolution is not supported by this study. Accommodative esotropia is usually stable, but younger age at diagnosis, oblique muscle dysfunction, and abnormal distance-near relationship are associated with deterioration. Undercorrection of hypermetropia can cause an abnormal distance-near relationship, which in turn can cause deterioration of accommodative esotropia. Aggressive undercorrection of hypermetropia should be pursued carefully, because the risk may outweigh the potential advantages.
HYPOTHESIS
Careful management of refractive error is critical to the treatment outcome of accommodative esotropia. Undercorrection of hypermetropia may result in instability of accommodative esotropia, with eventual deterioration of control in some patients, and undercorrection of hypermetropia may not improve the chance of resolution of accommodative esotropia.
INTRODUCTION
Accommodative esotropia is a convergent deviation of the eyes associated with the accommodative effort necessary to overcome the blurred image caused by hypermetropia.1–4 Accommodative esotropia usually presents in preschool years, and is often intermittent, and the deviation is typically eliminated by controlling the accommodative effort with optical correction of the hypermetropia. Accommodative esotropia has been classified as both refractive, caused by the accommodative effort on distance and near fixation associated with hypermetropia, and nonrefractive, where the eyes are aligned on distance fixation but esotropic on near fixation. Accommodative esotropia is common, accounting for approximately one half of all childhood esotropia.5 At first glance, treatment seems straightforward, and one would expect good results from standard treatment. However, published evidence indicates that accommodative esotropia treatment outcomes are inconsistent and often less than ideal. Amblyopia is common in these cases, many accommodative esotropia patients do not have bifoveal fusion, and strabismus surgery is sometimes necessary after initially successful optical treatment of the esotropia.6–16
The purpose of this study is to determine the influence of refractive error management on the natural history and treatment outcomes of a population of accommodative esotropia patients examined in a faculty pediatric ophthalmology practice. This study is unique in that one physician performed all initial examinations, all treatment, and all follow-up examinations. Characteristics of this patient group were evaluated and compared with those in previously published studies to address several unresolved issues regarding accommodative esotropia.
HISTORICAL BACKGROUND
Frans Cornelius Donders, a Dutch physiologist and physician, first described accommodative esotropia.1 Donders had published an essay in Dutch entitled Ametropie en hare gevolgen (Ametropia and Its Results) and was invited by Sir William Bowman to present his findings to The New Sydenham Society in London. The resulting text, On the Anomalies of Accommodation and Refraction of the Eye,1 not only described his series of 133 patients with accommodative esotropia but contained extensive discussions of accommodation, refractive errors, and the contribution of anisometropia to the development of amblyopia.
Although Donders contributed to many disciplines of human physiology, he is best known for his description of accommodative esotropia. He met with resistance from both physicians and patients and wrote, “If the squint sets in very early in life, wearing spectacles is of course attended with difficulties, and particularly when the patients are of the female sex, they are unwilling to be condemned to wear glasses during their whole life.”1 Today, management of hypermetropia in strabismus patients varies greatly among ophthalmologists, possibly compromising appropriate treatment of accommodative esotropia. Although in the minority, some ophthalmologists have advocated strabismus surgery for fully accommodative esotropia with removal of the hypermetropic correction.17–21 Published rebuttals to this approach have emphasized its long-term consequences.18,22–24
PROBLEMS
The overriding issue in the treatment of accommodative esotropia is the management of hypermetropia. Initial correction of hypermetropia, management of hypermetropic correction when small-angle esotropia persists with correction, undercorrection of hypermetropia, and the use of bifocals can all affect the level of fusional status and incidence of deterioration of accommodative esotropia. A failure to determine the basic deviation in infantile esotropia may cause underdiagnosis of early-onset accommodative esotropia with resultant unnecessary surgery and possible reoperation for secondary surgical exotropia. Undercorrection of hypermetropia without careful attention to alignment will result in poorer treatment outcomes. Variation in the management of hypermetropia in accommodative esotropia, as well as the degree of patient compliance may account for differences in stereoacuity levels, in the incidence of abnormal distance-near relationship, and in the incidence of deterioration of control of the accommodative esotropia with resultant strabismus surgery from one study to another.
This thesis studies the following issues that remain unresolved in the current literature:
Change in hypermetropia in accommodative esotropia and resolution of accommodative esotropia
Traditional teaching suggests that optical correction may be discontinued in the accommodative esotropia patient by the early teenage years3,25–29; however, accommodative esotropia is known to persist through the teenage and adult years.30,31 Hypermetropia typically remains unchanged or increases until 7 years of age2,32–34 and typically decreases after 7 years of age.32–34 Management of hypermetropia varies from decreasing the hypermetropic correction after the patient reaches 6 years of age in an attempt to improve fusional vergence3,25–29 to maintaining the full hypermetropic correction.35 Hypermetropia decreases minimally after age 7 in the typical accommodative esotropia patient.36,37 Whether undercorrection of the hypermetropia may stimulate a more rapid decrease of the hypermetropia is unresolved.38–40
This thesis addresses the issues of the incidence of spontaneous resolution of accommodative esotropia, the natural history of hypermetropia in the accommodative esotropia patient, the effect of undercorrection of hypermetropia on the natural history of hypermetropia, and the patient characteristics that allow undercorrection of hypermetropia.
Early-onset accommodative esotropia
Accommodative esotropia may occur in the first year of life,41–44 sometimes associated with only mild hypermetropia, and may be misdiagnosed as nonaccommodative infantile esotropia. There are conflicting published reports regarding treatment outcomes of early-onset accommodative esotropia compared with outcomes in later-onset accommodative esotropia.42,43 This thesis evaluates and compares stability and quality of stereoacuity in accommodative esotropia with onset in the first year of life to later-onset accommodative esotropia.
Deterioration of accommodative esotropia
Deterioration of optical control of accommodative esotropia requiring strabismus surgery does occur, sometimes after years of good control of the esotropia. Deterioration of accommodative esotropia has been associated with abnormal distance-near relationship and with inferior oblique overaction, but results have differed among studies.7,14,15,34,45 This thesis will examine the incidence of deterioration of accommodative esotropia, the effect of an abnormal distance-near relationship and the effect of oblique muscle dysfunction on the stability of control of accommodative esotropia, and the association between increasing hypermetropia and the apparent development of an abnormal distance-near relationship.
QUESTIONS
This thesis addresses the following:
Regarding the change in hypermetropia in accommodative esotropia and resolution of accommodative esotropia
Does accommodative esotropia typically resolve? Does hypermetropia decrease significantly in accommodative esotropia, and can undercorrection of hypermetropia result in a greater decrease of the hypermetropia?
Regarding early-onset accommodative esotropia
Do patients with early-onset accommodative esotropia have poorer treatment outcomes than patients with later-onset accommodative esotropia?
Regarding deterioration of accommodative esotropia
Does incomitance related to oblique muscle dysfunction contribute to deterioration of accommodative esotropia? Does abnormal distance-near relationship contribute to deterioration of accommodative esotropia? Is apparent abnormal distance-near relationship associated with undercorrection of hypermetropia?
METHODS
The protocol for this study was submitted to the author’s institutional review board, which determined that the protocol was exempt from further review because of the retrospective nature of the study. Data collection and analysis conformed to guidelines of the Health Insurance Portabililty and Accountability Act.
DEFINITIONS
Terminology and inclusion criteria vary among studies of accommodative esotropia. The terminology presented here helps clearly define the patient population for easier comparison to prior studies. Other investigators may use different terminology, and this language will be discussed when it is pertinent. But, in general, the terms used for this study are as follows:
Basic deviation
Deviation measured when fusional and accommodative vergences are suspended. Basic deviation is measured by prism and alternate cover testing with full cycloplegic optical correction and with the patient fixing on a distance target. In accommodative esotropia, basic deviation can be reliably measured only after the patient has consistently worn the full hypermetropic correction determined by cycloplegic refraction.46
Abnormal distance-near relationship
Esodeviation on prism and alternate cover testing on near fixation is at least 10 prism diopters (PD) greater than the esodeviation on prism and alternate cover testing on distance fixation with full cycloplegic correction in place. Abnormal distance-near relationship was considered consistent if present on a majority of examinations during follow-up. In some studies in the ophthalmic literature, an abnormal distance-near relationship has been considered clinical evidence of a high accommodative convergence to accommodation (AC/A) relationship.6,7,14,45
Fully accommodative esotropia
Orthophoria on distance and near fixation with full cycloplegic correction on the first follow-up examination after initiation of optical treatment. In fully accommodative esotropia, there is no basic deviation, and the distance-near relationship is normal.
Amblyopia
At least 2 lines difference in linear Snellen or Snellen equivalent visual acuity with best correction. On fixation preference testing in nonverbal children, the child’s failure to maintain fixation with one eye was used as evidence of amblyopia.
Bifoveal Fusion (sensory)
50 seconds of arc or better Titmus stereoacuity (Stereo Optical, Chicago, Illinois). This level of stereoacuity has been used to indicate “bifixation” in existing literature.9
Early-onset accommodative esotropia
Accommodative esotropia diagnosed at 12 months of age or younger. This definition has been used in the existing literature.42,43
Deterioration of accommodative esotropia
Increase in the horizontal basic deviation requiring strabismus surgery.
Resolution of accommodative esotropia
No esodeviation is present without correction, or the amount of esodeviation is not significantly different with and without correction, allowing optical correction to be discontinued.
INCLUSION CRITERIA
Records were reviewed from the author’s pediatric ophthalmology faculty practice to find patients who met the following criteria:
Initial examination performed by the author between 1982 and 2000.
Esodeviation of 10 PD or greater on distance and near fixation at initial examination.
Hypermetropia of any amount.
Distance deviation of less than 10 PD with spectacles containing full cycloplegic refraction at the first follow-up examination.
No previous optical, medical, or surgical treatment for strabismus.
A minimum of 2 years of follow-up and treatment, all performed by the author.
TESTING METHODS
The following diagnostic tests were used at initial examination and follow-up.
Visual acuity
Determined with linear Snellen optotypes at 6 m. In younger children, visual acuity was measured with linear Allen figures, and in nonverbal children, fixation preference was evaluated on distance and near fixation.
Esodeviation
Cover-uncover testing was used to distinguish constant from intermittent esotropia, and the deviation was quantified with prism and alternate cover testing with the patient fixing at 6 m and at 33 cm on an accommodative target. In several patients who presented in infancy, the esodeviation initially was measured only on near fixation, but all patients were measured on distance fixation on follow-up examinations.
Incomitance
Esodeviation in diagnostic positions of gaze was measured with prism and alternate cover testing with correction. V pattern of 15 PD or greater and A pattern of 10 PD or greater were considered significant.
Oblique dysfunction
Oblique muscle overaction was graded on a +1 to +4 scale. Any hypertropia in lateral gaze was measured by prism and alternate cover test.
Hypermetropia
Cycloplegic refraction by retinoscopy was typically done 30 to 40 minutes following instillation of 1% cyclopentolate eyedrops. In some patients with darkly pigmented irides or in whom cycloplegia did not appear adequate following the use of cyclopentolate, refraction was done following instillation of 1% atropine ointment for 3 days prior to the examination.
Alignment on follow-up examination
The basic deviation was determined by prism and alternate cover testing, and alternate cover testing was done with fixation at 33 cm to determine the distance-near relationship.
TREATMENT
Initial Treatment
In all cases, the esodeviation was initially treated with spectacles containing the full cycloplegic refraction. Patients were reexamined after 4 to 6 weeks of spectacle wear. If any esodeviation was present with spectacle correction on the first follow-up examination, the cycloplegic refraction was repeated, and if increased hypermetropia was uncovered, the increased correction was placed in the spectacles.
Undercorrection of Hypermetropia
If the patient was orthophoric on distance and near fixation on the initial follow-up examination or on subsequent examinations, the spectacle correction was not changed, even if cycloplegic refraction showed increased hypermetropia. Thus in some patients the hypermetropia was undercorrected from an early stage in the treatment of the accommodative esotropia. In other patients, if possible, the hypermetropia was undercorrected beginning at about 5 to 6 years of age. The hypermetropia was undercorrected as long as alignment was maintained with the decreased correction. However, the hypermetropia was not aggressively undercorrected to produce more than a small-angle esophoria on distance or near fixation with correction.
DATA COLLECTED
The following data were collected:
Age at initial examination and at most recent examination
Age at onset of esotropia by history
Amount of esotropia in prism diopters without correction on distance and near fixation at the initial examination
Amount of esotropia with and without correction on the first follow-up examination
Any difference in distance and near esotropia with correction on any examination during follow-up
Refractive error on initial and most recent examinations
Incidence of amblyopia on initial examination, on most recent examination, and at any time during follow-up
Quality of sensory fusion on most recent examination as determined by Titmus stereoacuity
Incidence of oblique muscle dysfunction and/or incomitance
Incidence of strabismus surgery
CHANGE IN HYPERMETROPIA AND RESOLUTION OF ACCOMMODATIVE ESOTROPIA
This retrospective cohort study included a subgroup of patients who had refractive error measured within 6 months of their seventh birthday. Total change in spherical equivalent was determined from initial examination to the examination near the seventh birthday. Patients were further divided into three groups:
Group 1: Patients wearing full cycloplegic refraction at the last examination
Group 2: Patients in whom the hypermetropia was undercorrected by less than 1.00 diopter (D)
Group 3: Patients in whom the hypermetropia was undercorrected by 1.00 D or more
The change in spherical equivalent from the examination near the seventh birthday to the most recent examination was calculated as change in diopters per year. The decrease in hypermetropia in diopters per year from age 7 until the most recent examination was calculated for each group, and the number of patients in each group with resolution of the accommodative esotropia was determined. Changes in hypermetropia were compared among the three groups to determine if undercorrection of hypermetropia contributed to a greater incidence of resolution of accommodative esotropia and to a greater decrease in hypermetropia.
EARLY-ONSET ACCOMMODATIVE ESOTROPIA
Patients in whom esotropia was found on examination at less than or equal to 12 months of age were included in a retrospective cohort study. Incidence of high-grade stereopsis and incidence of strabismus surgery were determined for this patient group and compared to the incidence among patients in whom diagnosis of accommodative esotropia was made after 2 years of age.
DETERIORATION OF ACCOMMODATIVE ESOTROPIA
Patients were identified in whom strabismus surgery was performed after initially successful alignment with spectacles, and possible factors contributing to deterioration were examined in a nested case-control study. Patients with abnormal distance-near relationship on any examination during follow-up were identified, and incidence of bifocal wear was determined. If the distance-near relationship was abnormal on a specific examination for a given patient, change in refractive error was determined for that particular examination to evaluate the effect of undercorrected hypermetropia on the distance-near relationship. The effect of the abnormal distance-near relationship on the level of stereopsis and on the incidence of strabismus surgery was evaluated.
RESULTS
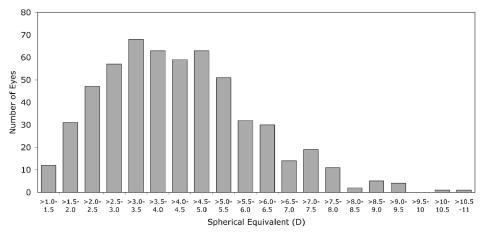
Two hundred eighty-five patients met the inclusion criteria, 156 (55%) female and 129 (45%) male. Sixty-four patients (22%) had a sibling with accommodative esotropia. Mean age at diagnosis was 41 months (range, 3 to 144 months), and mean age at last examination was 143 months (range, 31 to 271 months) for a mean follow-up of 102 months (range, 24 to 227 months). Mean hypermetropic spherical equivalent on presentation was 4.33 ± 1.71 D. Figure 1 shows the distribution of spherical equivalent at initial examination. Table 1 shows esodeviation measurements at initial examination, first follow-up examination, and last examination.
FIGURE 1.
Distribution of spherical equivalent on initial examination (285 patients, 570 eyes). D = diopter.
TABLE 1.
PRIMARY POSITION ESODEVIATION (285 PATIENTS)*
| DISTANCE FIXATION | NEAR FIXATION | |||
|---|---|---|---|---|
| EXAMINATION | MEAN ± SD | RANGE | MEAN ± SD | RANGE |
| Initial examination, without correction | 19 ± 8 | 10 – 55 | 21 ± 8 | 10 – 50 |
| Follow-up examination, with correction | 1.6 ± 2.5 | 0 – 8 | 4.4 ± 5.4 | 0 – 30 |
| Last examination, with correction | 1.0 ± 2.5 | 0 – 16 | 3.0 ± 4.3 | 0 – 20 |
SD = standard deviation.
All measurements in prism diopters.
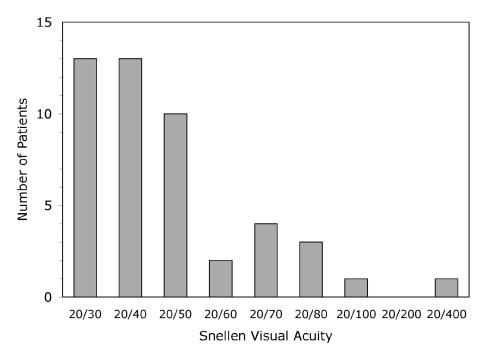
Amblyopia was a common diagnosis in this patient population. Amblyopia often resolved with treatment, but if persistent, visual acuity in the amblyopic eye at last examination was usually mildly decreased (Figure 2). Ninety-seven of the 285 patients (34%) were treated for amblyopia at some time during their follow-up. Sixty-six of the 285 patients (23%) had amblyopia on the first follow-up examination, and 47 of the 285 patients (16%) had amblyopia on their last examination.
FIGURE 2.
Level of amblyopia on most recent examination (47 patients).
Titmus stereoacuity testing was done on the most recent examination in 258 of the 285 patients, and of these, 112 (43%) had 50 seconds of arc or better stereoacuity.
Oblique dysfunction was uncommon but was frequently associated with deterioration. Twenty-four patients (8.4%) had inferior oblique overaction during their follow-up, and 17 patients had inferior oblique muscle surgery. Five patients (1.8%) had superior oblique overaction, and four of these had surgery for A-pattern and superior oblique overaction.
CHANGE IN HYPERMETROPIA AND SPONTANEOUS RESOLUTION OF ACCOMMODATIVE ESOTROPIA
Intentional undercorrection of hypermetropia was most likely to be achieved in patients with orthophoria on distance and near fixation at the first follow-up examination as well as at the last examination and was least likely to be achieved in patients with abnormal distance-near relationship (Table 2).
TABLE 2.
FACTORS POSSIBLY INFLUENCING ABILITY TO UNDERCORRECT HYPERMETROPIA
| FACTOR | GROUP1* | GROUP2† | GROUP 3‡ | PROBABILITY§ |
|---|---|---|---|---|
| Bifoveal fusion¶ | 25/58 (43%) | 35/81 (43%) | 26/45 (58%) | P = .16 |
| Orthophoria on first follow-up exam | 21/63 (33%) | 32/85 (38%) | 30/45 (67%) | P < .001 |
| Orthophoria on last exam | 16/63 (25%) | 40/85 (47%) | 25/45 (56%) | P < .001 |
| Deterioration of horizontal deviation requiring strabismus surgery | 15/63 (24%) | 10/85 (12%) | 7/45 (16%) | P = .19 |
| Abnormal distance-near relationship# | 27/63 (43%) | 16/85 (19%) | 1/45 ( 2.2%) | P < .0001 |
| Oblique dysfunction | 11/63 (17%) | 8/85 ( 9.4%) | 5/45 (11%) | P = .27 |
Full cycloplegic refraction.
Hypermetropia undercorrected less than 1.00 diopter.
Hypermetropia undercorrected by 1.00 diopter or more.
Chi-square test for trend.
50 seconds of arc or better Titmus stereoacuity.
Near esodeviation greater than distance esodeviation by 10 prism diopters or more on majority of examinations.
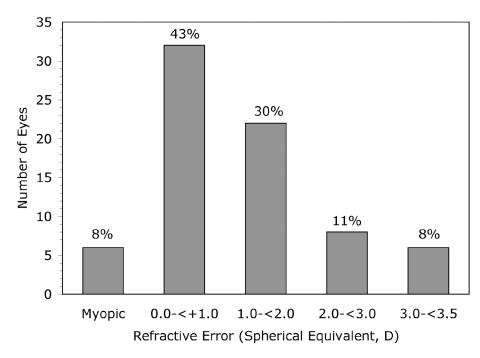
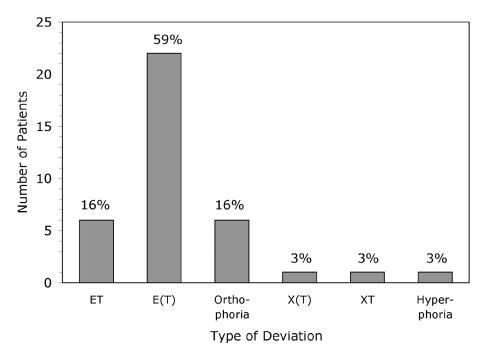
Accommodative esotropia did not typically resolve. Hypermetropic correction was discontinued for patients with enduring adequate alignment in 37 of the 285 patients (13%) at a mean age of 11.6 years (range, 7 to 17). On their last examination, 11 of those patients were wearing glasses or contact lenses for myopia, astigmatism, anisometropia, or a combination of the three, and many had some residual hypermetropia (Figure 3). Residual deviations without correction in patients with resolution of accommodative esotropia are shown in Figure 4. For the 37 patients with resolution of accommodative esotropia, mean hypermetropia on initial examination was 3.18 D compared with 4.50 D for the group without resolution of accommodative esotropia (P<.0001, t test). If only patients 12 years of age or older at last examination were included, 28 (20%) of 138 patients no longer required a hypermetropic correction to maintain adequate alignment. Kaplan-Meier survival analysis predicts hypermetropic correction would be discontinued in 30% of the patient population 15 years after initiation of treatment.
FIGURE 3.
Spherical equivalent on last examination in patients with resolution of accommodative esotropia (74 eyes). D = diopter.
FIGURE 4.
Residual deviation without correction in patients with resolution of accommodative esotropia (37 patients). All deviations measured < 10 prism diopters. ET = constant esotropia; E(T) = intermittent esotropia; X(T) = intermittent exotropia; XT = constant exotropia.
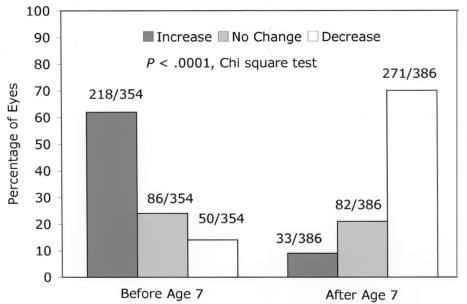
The majority of patients had an increase in hypermetropia from initial examination to age 7 years and a decrease in hypermetropia from age 7 to the last examination (P < .0001; chi-square test; Figure 5). In patients diagnosed before 6 years of age and refracted within 6 months of their seventh birthday, mean hypermetropic spherical equivalent increased from 4.28 D at initial examination to 4.93 D at age 7 years, a rate of .15 D per year. In patients refracted within 6 months of their seventh birthday, mean hypermetropic spherical equivalent decreased from 4.88 D at age 7 to 3.85 D on last examination, a mean annual decrease of .17 D.
FIGURE 5.
Change in hypermetropia (spherical equivalent) before and after age 7 years. A difference of ≤.25 D was considered no change.
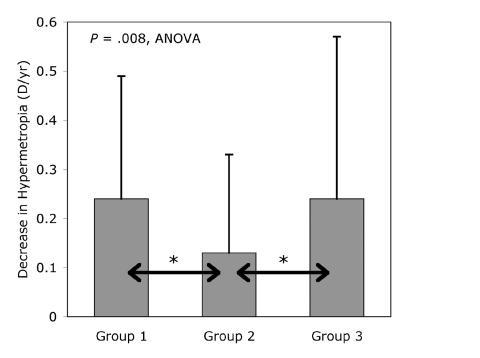
Undercorrection of hypermetropia did not cause a greater rate of decrease of the hypermetropia. Of the 193 patients with determination of refractive error within 6 months of their seventh birthday, 63 were wearing full cycloplegic refraction at their last examination (Group 1). In 85 patients, the hypermetropia was undercorrected by less than 1.00 D (Group 2), and in 45 patients, the hypermetropia was undercorrected by 1.00 D or more (Group 3). In Group 2, the undercorrection was started at a mean age of 6.4 years, and the mean duration of the undercorrection was 6.6 years. In Group 3, the undercorrection was started at a mean age of 5.0 years, and the mean duration of the undercorrection was 7.7 years. Mean annual decrease of hypermetropia in each group is shown in Figure 6. The mean annual decrease in hypermetropia in Group 2 was significantly smaller than in Groups 1 and 3 (P = .008; one-way analysis of variance).
FIGURE 6.
Decrease in hypermetropia after age 7 years, diopters (D)/year. Group 1: Patients wearing full cycloplegic refraction. Group 2: Patients with hypermetropia undercorrected by < 1.00 diopter. Group 3: Patients with hypermetropia undercorrected by ≥ 1.00 diopter. Error bars denote one standard deviation.
Children in whom hypermetropia was undercorrected did not have a higher incidence of resolution of accommodative esotropia than those who wore full cycloplegic refraction. One hundred eleven patients who had refractions within 6 months of their seventh birthday were older than 12 years on their last examination, and 26 (23%) of those no longer required hypermetropic correction. Hypermetropic correction was discontinued in 12 (29%) of 41 patients in Group 1, 10 of 47 (21%) in Group 2, and four of 23 (17%) in Group 3. There was no significant trend among groups of decreasing proportions outgrowing accommodative esotropia with increasing amounts of undercorrection (P = .25; chi-square test for trend).
Thirty-one of the 37 patients with resolution of accommodative esotropia were refracted within 6 months of their seventh birthday. The mean decrease of hypermetropia in this group was .37 D per year compared with .16 D per year for the group without resolution of accommodative esotropia (P = .001; t test).
Seventy-three patients had determination of refractive error within 6 months of their 12th birthday and also on their last examination. Mean follow-up after age 12 in this group was 45 months, and mean decrease in hypermetropia was .16 D per year.
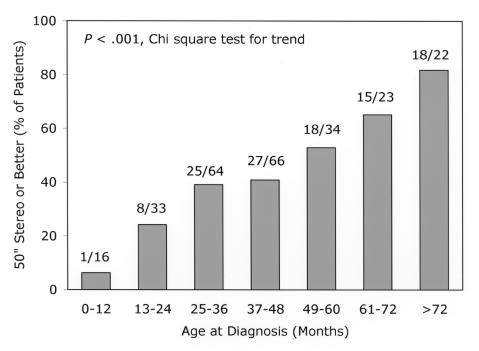
EARLY-ONSET ACCOMMODATIVE ESOTROPIA
Level of stereoacuity at last examination was related to age at diagnosis of accommodative esotropia (Figure 7). Twenty-one patients were 12 months of age or younger at the time of their initial examination, and 224 patients were older than 2 years at the time of initial examination. Distance deviation, near deviation, and spherical equivalent at the time of initial examination, as well as length of follow-up, were similar in the two groups (Table 3). Mean time from onset of esotropia by history to diagnosis of accommodative esotropia in the early-onset group was 3.1 months. Deterioration of accommodative esotropia requiring strabismus surgery and oblique muscle dysfunction were more common in the early-onset group, and amblyopia was more common in the later-onset group (Table 4). Mean duration from diagnosis of accommodative esotropia to strabismus surgery was 38 months in the early-onset group (range, 14 to 84 months).
FIGURE 7.
Incidence of bifoveal fusion (50 seconds of arc or better Titmus stereoacuity) by age at diagnosis (258 patients).
TABLE 3.
COMPARISON OF EARLY AND LATER-ONSET ACCOMMODATIVE ESOTROPIA PATIENTS
| EARLY ONSET (N = 21)* | LATER ONSET (N = 224)† | PROBABILITY‡ | |||
|---|---|---|---|---|---|
| VARIABLE | MEAN ± SD | RANGE | MEAN ± SD | RANGE | |
| Age at diagnosis, months | 9 ± 2 | 3 – 12 | 48 ± 20 | 25 – 144 | P < .0001 |
| Distance deviation, initial exam, PD | 21 ± 9 | 10 – 35 | 19 ± 8 | 10 – 55 | P = .38 |
| Near deviation, initial exam, PD | 23 ± 8 | 10 – 40 | 21 ± 8 | 10 – 50 | P = .32 |
| Spherical equivalent, initial exam, D | 4.70 ± 2.11 | 1.75 – 8.62 | 4.29 ± 1.64 | 1.12 – 11.00 | P = .40 |
| Follow-up, months | 126 ± 71 | 24 – 227 | 100 ± 45 | 24 – 219 | P = .12 |
D = diopters; PD = prism diopters; SD = standard deviation.
Diagnosed at or before 12 months of age.
Diagnosed after 24 months of age.
t test.
TABLE 4.
COMPARISON OF EARLY- AND LATER-ONSET ACCOMMODATIVE ESOTROPIA PATIENTS
| VARIABLE | EARLY ONSET* | LATER ONSET† | PROBABILITY‡ |
|---|---|---|---|
| E(T) on presentation | 12/21 (57%) | 87/224 (39%) | P = .16 |
| Aligned on first follow-up examination§ | 13/21 (62%) | 95/224 (42%) | P = .14 |
| Anisometropia on initial examination¶ | 3/21 (14%) | 64/224 (29%) | P = .25 |
| Amblyopia | 2/21 ( 9.5%) | 76/224 (34%) | P = .04 |
| Oblique muscle dysfunction | 8/21 (38%) | 16/224 ( 7.1%) | P < .0001 |
| Strabismus surgery | 9/21 (43%) | 22/224 ( 9.8%) | P < .0001 |
| Abnormal D-N relationship# | 5/21 (24%) | 48/224 ( 21%) | P = .80 |
D-N = distance-near; E(T) = intermittent esotropia.
Diagnosis at or before 12 months of age.
Diagnosis after 24 months of age.
Chi-square test.
Orthophoria on distance and near fixation with correction.
1.00 diopter or greater difference in spherical equivalent or cylindrical correction.
Near esodeviation greater than distance esodeviation by 10 prism diopters or more on majority of examinations.
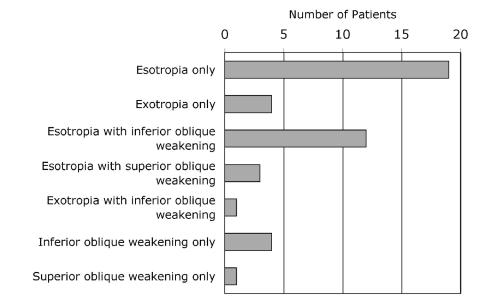
DETERIORATION OF CONTROL OF ACCOMMODATIVE ESOTROPIA
Younger age at diagnosis, oblique muscle dysfunction, and abnormal distance-near relationship were associated with deterioration of control of accommodative esotropia, and deterioration was less likely to occur in patients with fully accommodative esotropia (Table 5). Forty-four patients (15%) had strabismus surgery during their follow-up. The mean time from initial optical treatment to surgery was 38 months. Of these 44 patients, 21 had oblique muscle dysfunction. Figure 8 shows the type of surgery performed. Five patients had oblique muscle surgery for incomitance related to oblique dysfunction but did not have primary position misalignment requiring horizontal rectus muscle surgery, so the incidence of deterioration of primary position alignment was 39 of the total 285 patients (14%). Kaplan-Meier survival analysis predicts a 19% incidence of deterioration requiring strabismus surgery at 18 years after initiation of optical treatment. None of the five patients who had oblique muscle surgery required horizontal rectus muscle surgery later.
TABLE 5.
FACTORS ASSOCIATED WITH DETERIORATION OF CONTROL OF ESODEVIATION REQUIRING STRABISMUS SURGERY
| DETERIORATION (N = 39) | NO DETERIORATION (N = 246) | ||
|---|---|---|---|
| FACTOR | MEAN ± SD | MEAN ± SD | PROBABILITY* |
| Age at diagnosis, months | 25 ± 14 | 43 ± 22 | P < .0001 |
| Spherical equivalent at diagnosis, D | 3.95 ± 1.77 | 4.39 ± 1.69 | P = .15 |
| ET at diagnosis, PD | 21 ± 9 | 19 ± 8 | P = .40 |
| Incidence | Incidence | Probability† | |
| Constant ET at diagnosis | 28 (72%) | 145 (59%) | P = .18 |
| Fully accommodative ET‡ | 11 (28%) | 117 (48%) | P = .04 |
| Amblyopia during follow-up | 19 (49%) | 78 (32%) | P = .06 |
| Abnormal distance-near relationship§ | 16 (41%) | 49 (20%) | P = .007 |
| Oblique dysfunction and/or incomitance | 17 (44%) | 12 (4.9%) | P < .0001 |
D = diopters; ET = esotropia; PD = prism diopters; SD = standard deviation.
t test.
Chi-square test.
Orthophoria on distance and near fixation with correction on first follow-up examination.
Near esodeviation greater than distance esodeviation by 10 PD or more on majority of examinations.
FIGURE 8.
Types of strabismus surgery (44 patients).
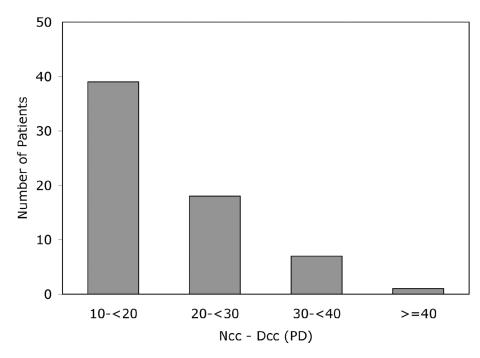
One hundred sixteen of the 285 patients (41%) had an abnormal distance-near relationship on at least one examination during follow-up. In 65 (23%) of the 285 patients, the abnormal distance-near relationship was consistent. The difference between distance and near esotropia in these 65 patients is shown in Figure 9.
FIGURE 9.
Difference between distance and near esodeviation in patients with consistent abnormal distance-near relationship, measured in prism diopters with optical correction (65 patients). Dcc = distance deviation with correction; Ncc = near deviation with correction; PD = prism diopters.
Of the 51 patients with an abnormal distance-near relationship on at least one examination but not consistently present, 19 (37%) had increased hypermetropia on cycloplegic refraction, and new spectacles with the increased correction normalized the distance-near relationship. Mean increase of spherical equivalent in the preferred eye was .92 D (range, .50 to 1.62), and mean difference between the distance and near esodeviation was 12 PD. None of these 51 patients wore bifocals at any time.
Patients with a consistently abnormal distance-near relationship were younger at diagnosis and had less hypermetropia than the rest of the study population. Deterioration of accommodative esotropia was more common and high-grade stereoacuity was less likely in this group (Table 6). Twenty-six of the 65 patients (40%) with a consistently abnormal distance-near relationship wore bifocals during their follow-up, and in 16 patients the bifocals had been discontinued at the time of the last examination. Table 7 compares patients with a consistently abnormal distance-near relationship who wore bifocals to those with a consistently abnormal distance-near relationship who did not wear bifocals.
TABLE 6.
INFLUENCE OF ABNORMAL DISTANCE-NEAR (D-N) RELATIONSHIP
| VARIABLE | ABNORMAL D-N* | NORMAL D-N | PROBABILITY |
|---|---|---|---|
| Mean age at diagnosis, months (±SD) | 34 ± 14 | 43 ± 24 | P = .0004† |
| Mean spherical equivalent, D (±SD) | 3.57 ± 1.39 | 4.55 ± 1.72 | P < .0001† |
| Bifoveal‡ | 18/62 (29%) | 94/196 (48%) | P = .01§ |
| Amblyopia | 26/65 (40%) | 71/220 (32%) | P = .31§ |
| Deterioration of accommodative ET | 16/65 (25%) | 23/220 (10%) | P = .007§ |
| Resolution of accommodative ET | 10/65 (15%) | 27/220 (12%) | P = .66§ |
D = diopters; ET = esotropia; SD = standard deviation.
Near esodeviation greater than distance esodeviation by 10 prism diopters or more on majority of examinations.
t-test.
50 seconds of arc or better stereoacuity.
Chi-square test.
TABLE 7.
BIFOCALS COMPARED TO NO BIFOCALS IN PATIENTS WITH ABNORMAL DISTANCE-NEAR RELATIONSHIP*
| VARIABLE | BIFOCALS | NO BIFOCALS | PROBABILITY |
|---|---|---|---|
| Mean age at last examination, months (±SD) | 148 ± 59 | 157 ± 41 | P = .50† |
| Mean amount abnormal D-N relationship, PD (±SD)* | 23 ± 7 | 16 ± 4 | P < .0001† |
| Bifoveal‡ | 8/25 (32%) | 10/37 (27%) | P = .89§ |
| Amblyopia | 8/26 (31%) | 18/39 (46%) | P = .33§ |
| Hypermetropic correction discontinued | 6/26 (23%) | 4/39 (10%) | P = .29§ |
| Strabismus surgery | 8/26 (31%) | 11/39 (28%) | P = .82§ |
D-N = distance-near; PD = prism diopters; SD = standard deviation.
Near esodeviation greater than distance esodeviation by 10 PD or more.
t test.
50 seconds of arc or better Titmus stereoacuity.
Chi-square test.
DISCUSSION
The major error in managing childhood esotropia is inadequate control of accommodation, which can confuse the diagnosis and lead to incorrect treatment.47 Comparison of accommodative esotropia studies is difficult because definitions and inclusion criteria vary among studies, and inclusion criteria are not always clearly defined. Authors often do not clearly explain how they manage hypermetropia regarding initial spectacle prescription or undercorrection of hypermetropia during follow-up. It is often unclear whether full cycloplegic refraction is prescribed as initial treatment and whether cycloplegic refraction is repeated when residual esotropia or distance-near disparity is present. Failure to fully correct the hypermetropia in these situations leads to greater rates of distance-near disparity as well as to greater rates of deterioration. In treating accommodative esotropia properly, the physician must always be aware of the basic deviation. Preferred practice pattern guidelines suggest spectacle prescription for hypermetropia of ≥ +1.50 D when associated with esotropia and also stress the need for a subsequent cycloplegic refraction when esotropia is not controlled with current spectacles.48 Comparison of cyclopentolate and atropine use for initial cycloplegic refractions showed failure of cyclopentolate to uncover the full amount of hypermetropia, especially in children with hypermetropia of more than +2.00 D.49 This emphasizes the importance of a follow-up cycloplegic refraction once spectacles have been prescribed, and esotropia should not be considered nonaccommodative until this follow-up cycloplegic refraction has been done.
In approximately two thirds of patients, hypermetropia can be gradually undercorrected, possibly improving fusional vergence. But how aggressively should the hypermetropia be undercorrected? Approaches may vary from maintaining orthophoria with correction to allowing intermittent esotropia with correction. More aggressive undercorrection of hypermetropia may lead to a lower incidence of high-grade stereoacuity and a higher incidence of deterioration.
Amblyopia in this patient population was common, responded well to treatment, and when present on the last examination, was usually mild. These findings are consistent with findings in the existing literature.8,16
Even though the incidence of sensory bifoveal fusion was higher in this study than that previously reported,9 the majority of accommodative esotropia patients did not have high-grade stereoacuity. Bifoveal fusion was very rare in children diagnosed with accommodative esotropia in the first year of life.
In this study, 50 seconds of arc or better Titmus stereoacuity was used to indicate sensory bifoveal fusion. It is well known that monocular clues allow recognition of some Titmus circles up to 140 to 200 seconds of arc (circles 4 and 3).50–52 Fawcett and Birch53 compared results of stereoacuity testing with Titmus, Randot circles (Stereo Optical, Chicago, Illinois), and the Randot Preschool Stereoacuity Test (Stereo Optical). They found agreement among the tests in patients with better than 100 seconds of arc stereoacuity. The authors stated, “The examiner can have confidence in stereoacuity scores of 160 seconds of arc or better. However, caution is suggested when interpreting stereoacuity scores >160 seconds of arc because it is within this range that monocular form cues may invalidate test results….”53 In this study, no assumptions were made based on lower-grade stereoacuity. The studies of stereoacuity testing mentioned here would support using 50 seconds of arc or better stereoacuity to imply sensory bifoveal fusion.
Even though oblique muscle dysfunction was not prevalent in this study, it was associated with deterioration of control of accommodative esotropia, and the majority of patients requiring oblique surgery also needed horizontal rectus muscle surgery. Wilson and Parks54 found a higher incidence of inferior oblique overaction in 150 patients with accommodative esotropia. One third of their accommodative esotropia patients required strabismus surgery, but unlike the current study, inferior oblique overaction was not associated with a higher incidence of deterioration of optical control of the esotropia. Raab7 found a 17% overall incidence of inferior oblique overaction in his series of 193 accommodative esotropia patients. He also found that inferior oblique overaction was associated with deterioration of control of the esotropia. Miller and Guyton55 reported that A or V patterns frequently occurred in patients with esotropia following surgery for intermittent exotropia and proposed that A and V patterns develop as a result of loss of fusion. In this series, of the 21 patients who required oblique muscle surgery, 17 developed oblique dysfunction with A or V patterns after initiation of optical treatment. Most of these patients had some esodeviation with optical correction, and only one was bifoveal.
CHANGE IN REFRACTIVE ERROR AND SPONTANEOUS RESOLUTION OF ACCOMMODATIVE ESOTROPIA
Accommodative esotropia did not resolve in the majority of patients studied. Swan30 described persistence of accommodative esotropia into adulthood, and Raab and Spierer31 found that esotropia “subsided” in 24.4% of their accommodative esotropia patients. Kaplan-Meier survival analysis of this study population predicts a 30% resolution at 15 years follow-up.
Raab36 found an annual decrease of .18 D of hypermetropia in accommodative esotropia patients after age 7 years, and Repka and coworkers37 found an annual decrease of .11 D of hypermetropia. The .17 D per year decrease in hypermetropia in this study confirms the very modest decrease of hypermetropia that occurs in accommodative esotropia after age 7 years. In this study, it is interesting that the gradual decrease in hypermetropia continues through the teenage years at about the same rate as the decrease between ages 7 and 12 years. Even so, most patients continue to have significant hypermetropia into adulthood.
Patients in this study who wore full cycloplegic refraction were as likely to have resolution of accommodative esotropia as patients who wore spectacles with the hypermetropia undercorrected. Decrease of hypermetropia was no less in patients who wore full cycloplegic correction than in patients who wore an undercorrected hypermetropic correction. Flitcroft and coworkers found an annual decrease of only .005 D of hypermetropia in accommodative esotropia patients who wore full cycloplegic refraction, and they suggested that treatment with full cycloplegic refraction may interfere with emmetropization (Flitcroft DI, Investigative Ophthalmology and Visual Science, 1998, Abstract). Studies of the natural history of hypermetropia in preschool children have led to conflicting conclusions, with one study suggesting a trend toward impeded emmetropization by spectacle correction,56 another showing no difference in emmetropization between children with and without hypermetropic correction,57 and another suggesting that hypermetropia behaves differently in strabismic children than in nonstrabismic children.58 All of these studies reported refractive error changes in preschool children, and most subjects were nonstrabismic, so it is difficult to apply the findings to older children with accommodative esotropia. In studying the effect of overcorrecting minus lens therapy for intermittent exotropia, Kushner found no greater decrease in hypermetropia in patients treated with overminus spectacles than in those hypermetropic patients not treated with overminus spectacles.59
Lambert and coworkers40 have suggested that aggressive undercorrection of the hypermetropia may eliminate the need for optical correction to control the accommodative esotropia. They considered a child successfully weaned from glasses if the child was “orthotropic” on distance and near correction without optical correction. In their series, 70% of patients had less than 3.00 D of hypermetropia on presentation, and patients successfully weaned from spectacles had a mean spherical equivalent of only 2.40 D at presentation. The actual decrease of hypermetropia was not evaluated, and the investigators suggested improved fusional vergence as the main reason glasses could be discontinued.
It is evident from these previous studies that the natural history of hypermetropia in accommodative esotropia is not clear, and that there is no consensus on the effect of spectacle correction on the course of hypermetropia in accommodative esotropia. In the patient population for this study, hypermetropia usually increased from initial examination to age 7 years, but only by a mean .65 D (.15 D per year). This may represent a true increase in hypermetropia, but the change may also be influenced by more hypermetropia being uncovered on subsequent cycloplegic refractions after a child wore glasses. In a moderate to high hypermetrope, an apparent .65 D increase in refractive error would not be unusual just from the relaxation of ciliary muscle tone.
Prior studies generally agree that hypermetropia decreases after age 7 but, on average, by only a small amount. The average child in this study presented with hypermetropia of 4.28 D, which increased to 4.93 D by age 7. With a mean annual decrease of .17 D of hypermetropia after age 7, this child would be almost 11 years old before hypermetropia had again reached 4.28 D. It is not likely this average child would experience enough further decrease of the hypermetropia to allow resolution of accommodative esotropia.
Resolution of accommodative esotropia in this study most often occurred in children who started with a lesser degree of hypermetropia than the typical accommodative esotropia patient, and in whom the hypermetropia decreased at a faster rate than the average for the entire population. Patients with resolution of accommodative esotropia often had some residual hypermetropia, suggesting that resolution of accommodative esotropia is due to a combination of some decrease of the hypermetropia and improved fusional vergence. In patients with good alignment without optical correction but with some residual hypermetropia, it is possible that accommodative esotropia will reoccur in adulthood when increased accommodative effort may be necessary to overcome the hypermetropia. Because most patients with resolution of accommodative esotropia in the present study still had a small-angle esophoria or intermittent esotropia, reoccurrence of accommodative esotropia in adulthood appears to be a strong possibility. Shippman and coworkers60 reported 11 adults in whom accommodative esotropia reoccurred between 20 and 65 years of age. Six of these patients had hypermetropia of less than 2.00 D. Thus not only do a small percentage of patients experience resolution of accommodative esotropia as young teenagers, some of these patients are likely to develop accommodative esotropia again as adults.
The results of this study indicate that undercorrecting the hypermetropia in accommodative esotropia does not cause the hypermetropia to decrease faster and eventually resolve. It is possible that the undercorrected patients were not undercorrected aggressively enough to produce a faster decrease of hypermetropia. Whether a patient can be undercorrected and the amount of the undercorrection are determined by the control of esotropia. Greater undercorrection of hypermetropia can cause less stability of optical control, resulting in a greater incidence of strabismus surgery and a lower incidence of bifoveal fusion. Aggressive undercorrection of hypermetropia may improve fusional vergence, but there is no evidence that this will cause a more rapid decrease of the hypermetropia. Patients with fully accommodative esotropia had the most stable alignment and the best stereoacuity during follow-up, and this group could most effectively be optically undercorrected. In many children there is no choice. Full cycloplegic refraction is required to maintain adequate alignment and to achieve the best possible binocular vision result.
This is the only study, to the author’s knowledge, that examines the outcome of refractive error in children with accommodative esotropia with fully corrected hypermetropia compared to those with undercorrected hypermetropia. These results indicate that undercorrection of hypermetropia does not cause faster decrease of hypermetropia. The most important factor predicting resolution of accommodative esotropia is the amount of hypermetropia at the time of diagnosis.
EARLY-ONSET ACCOMMODATIVE ESOTROPIA
Early-onset accommodative esotropia is associated with poor stereoacuity and a high rate of deterioration. Pollard41 first described early-onset accommodative esotropia, presenting two patients with onset before 6 months of age, one at 4.5 months, the other at 5 months. Hypermetropia was 4.50 D in one patient and 3.50 D in the other, and the esotropia was controlled with spectacles in both patients. Baker and Parks42 studied 21 patients with early-onset accommodative esotropia. Of their reported patients, 48% had deterioration of optical control of the esotropia and required strabismus surgery, and all but one patient continued to require a hypermetropic correction. Dickey and Scott15 described 13 patients with a history of esotropia onset in the first year of life followed for at least 10 years, but they did not report the age at which spectacles were prescribed. Ten of their 13 patients (77%) eventually had deterioration of control of accommodative esotropia and required strabismus surgery. Coats and coworkers43 reported a series of 17 patients diagnosed with accommodative esotropia in the first year of life and compared them with a control group with onset after 2 years of age. Eighteen percent of the early-onset group had strabismus surgery vs 4% of the control group, but the difference was not statistically significant. The authors concluded that the early-onset group did not have worse outcomes than the later-onset control group. Their mean follow-up was a relatively short 34 months for the early-onset group, compared with 88 months in the Baker series and 126 months in this study. In this study population, strabismus surgery was done a mean of 38 months after optical treatment was initiated, and in four of nine patients who required surgery, the strabismus surgery was done more than 34 months after optical treatment was started. Thus longer follow-up in the Coats series might have resulted in a higher rate of deterioration of the accommodative esotropia. Coats and coworkers stated, “Prompt spectacle correction may lead to long-term stable alignment and measurable stereoacuity, with relatively few patients requiring surgery.”43 In the Coats study, mean time from onset by history to optical correction of the esotropia was 5.1 months, and for patients in this study, mean time was 3.1 months. Coats and coworkers emphasized the need for full cycloplegic correction at the time of diagnosis. All patients in the current study were corrected with spectacles containing full cycloplegic refraction. Thus, despite full cycloplegic correction and the short interval from onset to treatment, deterioration requiring strabismus surgery was common for those patients.
The early-onset group in this study is similar to the group reported by Baker and Parks42 (Table 8). Age at onset is similar, and in both groups, most children with early onset had intermittent esotropia on initial examination. Incidence of deterioration of optical control in the Baker and Parks study was similar to that of my patient population, both much higher than the incidence of deterioration in the study by Coats and coworkers.43 In the Baker and Parks study, all surgical procedures were for esotropia without oblique dysfunction. In the current study group, four patients had only horizontal rectus muscle surgery for esotropia, four had inferior oblique surgery in addition to horizontal rectus surgery, and one had superior oblique surgery in addition to horizontal rectus surgery.
TABLE 8.
COMPARISON OF EARLY-ONSET ACCOMMODATIVE ESOTROPIA GROUPS FROM PREVIOUS STUDIES TO THE CURRENT STUDY
| VARIABLE | BAKER, PARKS (1980) | COATS ET AL (1998) | CURRENT STUDY |
|---|---|---|---|
| Patient number | 21 | 17 | 21 |
| Mean age at diagnosis, months | 8.1 | 9.0 | 8.6 |
| Mean follow-up, months | 88 | 34 | 126 |
| Incidence of intermittent esotropia | 71% | NA | 57% |
| Incidence of amblyopia | 62% | 0% | 10% |
| Incidence of strabismus surgery | 48% | 18% | 43% |
It is likely that there is some overlap between early-onset accommodative esotropia and infantile esotropia (nonaccommodative), and many early-onset accommodative esotropia patients behave more like infantile esotropia patients than typical accommodative esotropia patients. A mixed form of esotropia occurs in infancy where there is an accommodative component to infantile esotropia and some accommodative esotropia remains after surgical correction,7,61 but even in infants who have good alignment with hypermetropic correction, bifoveal fusion is rare, and the esotropia is much less stable than in later-onset accommodative esotropia. Even though the delay from onset (by history) to diagnosis of the accommodative esotropia was fairly short, and intermittent esotropia was common in the early-onset group, bifoveal fusion was rare in the early-onset group and common in the control group. Oblique dysfunction was more common in the early-onset group. Mean hypermetropia was high in the early-onset group, but early-onset accommodative esotropia occurred with hypermetropia as low as 1.75 D. This has significance in the management of esotropia in infancy. In an infant presenting with esotropia with a moderate amount of hypermetropia, full cycloplegic correction should be prescribed, especially if the deviation is of moderate amplitude and is intermittent. Even if surgery is required in the mixed accommodative esotropia/nonaccommodative infantile esotropia patient, the surgery will be more predictable and the postoperative deviation will be more stable if the amount of accommodative component is determined by prescribing glasses preoperatively. In some cases, the esotropia will be entirely accommodative, and unnecessary surgery and probable secondary surgical exotropia will be avoided. Infantile esotropia, accommodative or nonaccommodative, can only be managed appropriately if one has determined the basic deviation.
DETERIORATION OF CONTROL OF ACCOMMODATIVE ESOTROPIA
Deterioration of accommodative esotropia in this series is similar to that reported by Raab7 and Dickey and Scott.15 Raab found inferior oblique overaction to be associated with deterioration, but found that abnormal distance-near relationship was not a contributing factor. Dickey and Scott identified age at onset as a significant factor in deterioration of accommodative esotropia and also found that high accommodative convergence to accommodation relationship measured by the gradient method did not contribute to deterioration. Ludwig and coworkers14 found a 30.3% deterioration rate and found deterioration to be more common in patients with an abnormal distance-near relationship. In their study, age at onset and amblyopia were not contributing factors.
In the current series, younger age at diagnosis, oblique dysfunction, and abnormal distance-near relationship contributed to deterioration of the accommodative esotropia with resultant strabismus surgery. Fully accommodative esotropia was associated with a lower incidence of deterioration. Prior to the onset of accommodative esotropia, there is an opportunity for bifoveal fusion to develop, but in early-onset accommodative esotropia, this window of opportunity is small. In children with constant esotropia at diagnosis, or in those who were not orthophoric after optical correction, there might have been no opportunity for the development of bifoveal fusion. Oblique dysfunction (incomitance) and abnormal distance-near relationship cause a lack of stability of control, leading to a loss of fusion and often deterioration of optical control of the accommodative esotropia.
One of the most significant contributing factors in this series is oblique muscle dysfunction. Raab also found inferior oblique overaction to be a contributing factor. If Miller and Guyton55 are correct in their suggestion that oblique dysfunction and A and V patterns are the result of loss of fusion, it makes sense that the esotropia control may deteriorate from that loss. Perhaps deterioration and A-V patterns are both isolated manifestations of that loss of fusion, and the oblique dysfunction, despite being associated with deterioration, is not actually a cause. But oblique dysfunction with A or V pattern could be a direct cause of the deterioration of the accommodative esotropia. The instability associated with the incomitant deviation would cause some intermittent suppression even if the eyes were still aligned in primary position, and it would eventually lead to primary position deviation.
The mechanism of deterioration of accommodative esotropia is not well explained. One might expect that some gradual contracture of medial rectus muscles related to incomitance, small-angle intermittent esotropia with correction, or less than full-time wear of spectacles would be a reasonable explanation. Are there other explanations? Do some of these patients “lose fusion”? In patients requiring surgery, mean time from diagnosis and initiation of spectacle treatment to surgery was 38 months. But one patient had surgery 13 years after diagnosis. What would cause this patient to lose fusion after that amount of time? The mechanical explanation of muscle contracture related to instability of control appears to be the best explanation.
In several large accommodative esotropia case series, authors have defined a high AC/A relationship as near deviation greater than distance deviation.6,7,14,45 In this thesis, this finding is described as an abnormal distance-near relationship, as it may not always represent a high AC/A relationship. In a patient wearing hypermetropic spectacles, a greater amount of accommodation per unit distance is required on near fixation than in an emmetrope.62 This increase in required accommodation is significant with spectacle power of +3.00 D or more, and the near esodeviation may be greater than the distance esodeviation, not because of a high AC/A relationship but because of the increased accommodative effort on near fixation required by the optical system of spectacle correction of the hypermetropic eye. As stated by Sampson, “…it should be obvious that the true synkinetic response between convergence and accommodation in high refractive errors is actually unaltered, but erroneously measured, when spectacle lenses are used to correct the refractive error.”62 Havertape and coworkers63 suggested that arbitrarily using the difference of near and distance esodeviation measurements to determine high AC/A relationship may be inaccurate. They found that in many patients with an abnormal distance-near relationship, AC/A relationship was normal when measured by the gradient method. Arnoldi and Shainberg64 also cautioned that an abnormal distance-near relationship did not necessarily correlate with AC/A relationship.
In this study, abnormal distance-near relationship was related to deterioration of accommodative esotropia with resultant strabismus surgery, but incidence of abnormal distance-near relationship was lower in this study than in previously published studies. The significant factor associated with deterioration of accommodative esotropia is instability, that is, intermittent esotropia on near fixation in the case of abnormal distance-near relationship. Ludwig and coworkers14 found that an abnormal distance-near relationship contributed to a greater incidence of deterioration of control of accommodative esotropia, but Raab7 found that an abnormal distance-near relationship was not associated with deterioration of accommodative esotropia, and Dickey and Scott15 found that high gradient AC/A did not contribute to deterioration of control of the esotropia with spectacles.
The data from this patient population suggest that the majority of accommodative esotropia patients with an abnormal distance-near relationship do not need bifocals. Many patients with an abnormal distance-near relationship were not treated with bifocals because they had an intermittent esotropia or esophoria on near fixation or a constant esotropia on distance fixation. There was no statistically significant difference in the rate of deterioration between those patients with an abnormal distance-near relationship wearing bifocals and those with an abnormal distance-near relationship not wearing bifocals. Even in the patient wearing bifocals, it is likely that esotropia is present intermittently when a child fixates on objects closer than 33 cm or fixates on near objects without using the bifocal. Treatment with bifocals did not contribute better stability in this study, but this finding is influenced by patient selection, as patients wearing bifocals were more likely to have a larger abnormal distance-near relationship than patients not wearing bifocals.
Not only is there a questionable need for bifocals in abnormal distance-near relationship, the use of bifocals is not without consequences. Pratt-Johnson and Tillson65 found that patients wearing bifocals for accommodative esotropia and an abnormal distance-near relationship had no better sensory outcome than patients not wearing bifocals with the same problem. Arnoldi and Shainberg64 studied patients with a high AC/A relationship measured by the gradient method. At 5-year follow-up, those patients not wearing bifocals had better control of the near esodeviation than those wearing bifocals. In both groups, the near deviation decreased during the 5-year follow-up, but in patients wearing bifocals, the gradient AC/A relationship increased.
Some patients in this study had an abnormal distance-near relationship related to undercorrected hypermetropia on at least one examination, and these patients had normalization of the distance-near relationship after the hypermetropia was fully corrected. A prescription change of as little as .50 D normalized the distance-near relationship in some patients. A cycloplegic refraction should be done on any patient presenting with an apparent abnormal distance-near relationship. If hypermetropia is undercorrected, a new spectacle correction without bifocals should be prescribed. This study demonstrates that many of these patients will have good alignment without bifocals and that unnecessary prescribing of bifocals can be avoided by following this procedure. Undercorrection of hypermetropia may explain the higher incidence of abnormal distance-near relationship and higher deterioration rate in some studies of accommodative esotropia compared with this study. Also, bifocals should not be prescribed as the initial optical correction when the diagnosis of accommodative esotropia is first considered. The deviation in accommodative esotropia is caused by accommodative effort, and prior to spectacle prescription, the deviation on near fixation is often greater than the distance deviation. An abnormal distance-near relationship cannot be diagnosed until the patient is wearing a full cycloplegic refraction. In this study, the majority of patients with an apparent abnormal distance-near relationship on initial examination never wore bifocals during their follow-up.
CONCLUSIONS
The overriding factor in treatment of accommodative esotropia is management of refractive error. On the basis of this study, the following conclusions regarding hypermetropia management and accommodative esotropia can be made:
Accommodative esotropia usually does not resolve. The most important factor in predicting resolution of accommodative esotropia is the amount of hypermetropia at the time of diagnosis. The possibility that undercorrecting hypermetropia hastens its resolution is not supported by this study.
Age at onset appears to be a variable for long-term stability of accommodative esotropia. In the early-onset patients, incidence of high-level stereoacuity is much lower, and incidence of deterioration of control requiring strabismus surgery is much higher.
Accommodative esotropia is usually stable, and deterioration of control is not the rule. Oblique muscle dysfunction is not common in the diagnosed population, but it is frequently present in patients with deterioration of control.
Abnormal distance-near relationship is associated with deterioration of accommodative esotropia. Patients wearing less than full cycloplegic correction may appear to have an abnormal distance-near relationship, but with prescription of full cycloplegic correction, the distance-near relationship is normal.
Undercorrection of hypermetropia should be pursued with care. Undercorrection can easily be accomplished in many patients, but in others it may allow development of an abnormal distance-near relationship, which in turn can lead to deterioration of accommodative esotropia. The risk of aggressive undercorrection may outweigh potential benefits of that approach.
Strengths of this study include a comparatively large patient population with long-term mean follow-up by a single investigator, allowing for a consistent treatment philosophy. The study’s weakness is its retrospective nature. Data collection was done by the author, a potential source of bias. Retrospective cohort and case-control studies are not ideal methods to prove a hypothesis but may show trends and result in questions deserving further study. This is especially true in the section concerning the natural history of hypermetropia and the effect of undercorrection of hypermetropia. A prospective, randomized clinical trial was not practical for this thesis, because it would require many years to complete, but would be appropriate to further study the effect of undercorrection of hypermetropia. Nevertheless, this is the first study, to the author’s knowledge, that addresses the influence of undercorrection of hypermetropia on the natural history of hypermetropia.
ACKNOWLEDGMENTS
Thanks to Joost Felius, PhD, Retina Foundation of the Southwest, Dallas, Texas, for his invaluable assistance in the statistical analysis of the data used in this thesis.
REFERENCES
- 1.Donders FC. Strabismus convergens, the result of hypermetropia. In: On the Anomalies of Accommodation and Refraction of the Eye. London: The New Sydenham Society; 1864:291–309.
- 2.Swan KC. Symposium: Accommodative esotropia. Classification and diagnosis. Trans Am Acad Ophthalmol Otolaryngol. 1957;61:383–389. [PubMed] [Google Scholar]
- 3.Parks MM. Accommodative esotropia: cause and treatment. Am Orthopt J. 1955;5:74–79. [PubMed] [Google Scholar]
- 4.Parks MM. Symposium: Accommodative esotropia. Physiology and etiology. Am Orthopt J. 1955;4:5–11. [PubMed] [Google Scholar]
- 5.Mohney BG. Common forms of childhood esotropia. Ophthalmology. 2001;108:805–809. doi: 10.1016/s0161-6420(00)00639-4. [DOI] [PubMed] [Google Scholar]
- 6.Parks MM. Abnormal accommodative convergence in squint. Arch Ophthalmol. 1958;59:364–380. doi: 10.1001/archopht.1958.00940040070008. [DOI] [PubMed] [Google Scholar]
- 7.Raab EL. Etiologic factors in accommodative esotropia. Trans Am Ophthalmol Soc. 1982;80:657–694. [PMC free article] [PubMed] [Google Scholar]
- 8.Mulvihull A, MacCann A, Flitcroft I. Outcome in refractive accommodative esotropia. Br J Ophthalmol. 2000;84:746–749. doi: 10.1136/bjo.84.7.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson ME, Bluestein EC, Parks MM. Binocularity in accommodative esotropia. J Pediatr Ophthalmol Strabismus. 1993;30:233–236. doi: 10.3928/0191-3913-19930701-04. [DOI] [PubMed] [Google Scholar]
- 10.Birch EE. Binocular sensory outcomes in accommodative ET. J AAPOS. 2003;7:369–373. doi: 10.1016/j.jaapos.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Raab EL. Outcome of deteriorated accommodative esotropia. Trans Am Ophthalmol Soc. 1989;87:185–193. [PMC free article] [PubMed] [Google Scholar]
- 12.Raab EL. Monitoring of controlled accommodative esotropia. Trans Am Ophthalmol Soc. 2001;99:225–231. [PMC free article] [PubMed] [Google Scholar]
- 13.Raab EL. Follow-up monitoring of accommodative esotropia. J AAPOS. 2001;5:246–251. doi: 10.1067/mpa.2001.117570. [DOI] [PubMed] [Google Scholar]
- 14.Ludwig IH, Parks MM, Getson PR, et al. Rate of deterioration in accommodative esotropia correlated to the AC/A relationship. J Pediatr Ophthalmol Strabismus. 1988;25:8–12. doi: 10.3928/0191-3913-19880101-04. [DOI] [PubMed] [Google Scholar]
- 15.Dickey CF, Scott WE. The deterioration of accommodative esotropia: frequency, characteristics, and predictive factors. J Pediatr Ophthalmol Strabismus. 1988;25:172–175. doi: 10.3928/0191-3913-19880701-06. [DOI] [PubMed] [Google Scholar]
- 16.Berk AT, Kocak N, Ellidokuz H. Treatment outcomes in refractive accommodative esotropia. J AAPOS. 2004;8:384–388. doi: 10.1016/j.jaapos.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Gobin MH, Putteman A. La correction chirurgicale du strabisme accommodatif, 20 ans d’experience. Bull Soc Belge Ophtalmol. 1984;210:107–112. [PubMed] [Google Scholar]
- 18.Fells P. Symposium on the management of fully accommodative esotropia. In: Campos EC, ed. Strabismus and Ocular Motility Disorders London: Macmillan Press Ltd; 1990.
- 19.Berard P. Traitement chirurgical de l’esotropie accommodative. Bull Soc Belge Ophtalmol. 1994;253:111–118. [PubMed] [Google Scholar]
- 20.Semmlow J, Putteman A, Vercher J, et al. Surgical modification of the AC/A ratio and the binocular alignment at distance; its influence on accommodative esotropia: a study of 21 cases. Binocul Vis Strabismus Q. 2000;15:121–130. [PubMed] [Google Scholar]
- 21.Molteno ACB, Kindon R. A comparative trial of Gobin’s method versus conventional surgery for refractive/accommodative esotropia uncorrected by non-surgical methods. Binocul Vis Strabismus Q. 2000;15:351–356. [PubMed] [Google Scholar]
- 22.Jampolsky A, von Noorden GK, Spiritus M. Unnecessary surgery in fully refractive accommodative esotropia. Aust NZ J Ophthalmol. 1991;19:370–371. doi: 10.1111/j.1442-9071.1991.tb00691.x. [DOI] [PubMed] [Google Scholar]
- 23.von Noorden GK, Avilla CW. Refractive accommodative esotropia: a surgical problem? Int Ophthalmol. 1992;16:45–48. doi: 10.1007/BF00917072. [DOI] [PubMed] [Google Scholar]
- 24.Kushner BJ. Surgery or not for fully accommodative esotropia. Binocul Vis Strabismus Q. 2000;15:315–316. [PubMed] [Google Scholar]
- 25.Costenbader FD. Symposium: Accommodative esotropia. Clinical course and management. Am Orthopt J. 1954;4:12–16. [PubMed] [Google Scholar]
- 26.Costenbader FD. Symposium: Accommodative esotropia. Principles of treatment. Trans Am Acad Ophthalmol Otolaryngol. 1957;61:390–394. [PubMed] [Google Scholar]
- 27.Cooper EL. Accommodative esotropia in clinical practice. Am Orthopt J. 1963;13:42–48. [PubMed] [Google Scholar]
- 28.Parks MM, Mitchell PR, Wheeler MB. Concomitant deviations. In: Tasman W, Jaeger EA, eds. Clinical Ophthalmology Philadelphia: Lippincott Williams & Wilkins; 2005: chap 12.
- 29.Trigler L, Siatkowski M. Managing accommodative esotropia. EyeNet. 2002 Jan;:29–31. [Google Scholar]
- 30.Swan KC. Accommodative esotropia long range follow-up. Ophthalmology. 1983;90:1141–1145. doi: 10.1016/s0161-6420(83)34415-8. [DOI] [PubMed] [Google Scholar]
- 31.Raab EL, Spierer A. Persisting accommodative esotropia. Arch Ophthalmol. 1986;104:1777–1779. doi: 10.1001/archopht.1986.01050240051038. [DOI] [PubMed] [Google Scholar]
- 32.Brown EVL. Net average yearly changes in refraction of atropinized eyes from birth to beyond middle life. Arch Ophthalmol. 1938;19:719–734. [Google Scholar]
- 33.Slataper FJ. Age norms of refraction and vision. Arch Ophthalmol. 1950;43:466–481. [Google Scholar]
- 34.Parks MM. Management of acquired esotropia. Br J Ophthalmol. 1974;58:240–247. doi: 10.1136/bjo.58.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wright KW. Esodeviations. In: Wright KW, Spiegel PH, ed. Pediatric Ophthalmology and Strabismus. New York: Springer-Verlag; 2003:204–223.
- 36.Raab EL. Hypermetropia in accommodative esotropia. J Pediatr Ophthalmol Strabismus. 1984;21:194–197. [PubMed] [Google Scholar]
- 37.Repka MX, Wellish K, Wisnicki HJ, et al. Changes in the refractive error of 94 spectacle-treated patients with acquired accommodative esotropia. Binocular Vision. 1989;4:15–21. [Google Scholar]
- 38.Knapp P. The clinical management of accommodative esotropia. Am Orthopt J. 1967;17:8–13. [PubMed] [Google Scholar]
- 39.Lambert SR. Emmetropization in children with refractive accommodative esotropia. In: Scott AB, ed. Festschrift for Arthur Jampolsky San Francisco, Calif: The Smith-Kettlewell Eye Research Institute; 2000:17–22.
- 40.Lambert SR, Lynn M, Sramek J, et al. Clinical features predictive of successfully weaning from spectacles those children with accommodative esotropia. J AAPOS. 2003;7:7–13. doi: 10.1067/mpa.2003.S1091853102420101. [DOI] [PubMed] [Google Scholar]
- 41.Pollard ZF. Accommodative esotropia during the first year of life. Am J Ophthalmol. 1976;94:1912–1913. doi: 10.1001/archopht.1976.03910040622009. [DOI] [PubMed] [Google Scholar]
- 42.Baker JD, Parks MM. Early-onset accommodative esotropia. Am J Ophthalmol. 1980;90:11–21. doi: 10.1016/s0002-9394(14)75070-6. [DOI] [PubMed] [Google Scholar]
- 43.Coats DK, Avilla CW, Paysse EA, et al. Early-onset refractive accommodative esotropia. J AAPOS. 1998;2:275–278. doi: 10.1016/s1091-8531(98)90083-0. [DOI] [PubMed] [Google Scholar]
- 44.Pollard ZF, Greenberg MF. Unusual presentations of accommodative esotropia. Trans Am Ophthalmol Soc. 2000;98:119–125. [PMC free article] [PubMed] [Google Scholar]
- 45.Ludwig IH, Imberman SP, Thompson HW, et al. Long-term study of accommodative esotropia. Trans Am Ophthalmol Soc. 2003;101:155–161. [PMC free article] [PubMed] [Google Scholar]
- 46.Jampolsky A. A simplified approach to strabismus diagnosis. In: Pediatric Ophthalmology and Strabismus: Transactions of the New Orleans Academy of Ophthalmology. St Louis: Mosby; 1971:34–92.
- 47.Jampolsky A. What do we really know about strabismus and its management? In: Taylor D, Hoyt CS, eds. Pediatric Ophthalmology and Strabismus. Edinburgh: Elsevier Ltd; 2005:1001–1010.
- 48.Bateman JB, Christmann LM, Dankner SR, et al. Esotropia and exotropia. In: Preferred Practice Pattern San Francisco: American Academy of Ophthalmology; 2002:1–30.
- 49.Rosenbaum AL, Bateman JB, Bremer DL, et al. Cycloplegic refraction in esotropic children. Ophthalmology. 1981;88:1031–1034. doi: 10.1016/s0161-6420(81)80032-2. [DOI] [PubMed] [Google Scholar]
- 50.Fawcett S, Leffler J, Birch EE. Factors influencing stereoacuity in accommodative esotropia. J AAPOS. 2000;4:15–20. doi: 10.1016/s1091-8531(00)90006-5. [DOI] [PubMed] [Google Scholar]
- 51.Clarke WN, Noel LP. Stereoacuity testing in the monofixation syndrome. J Pediatr Ophthalmol Strabismus. 1990;27:161–163. doi: 10.3928/0191-3913-19900501-14. [DOI] [PubMed] [Google Scholar]
- 52.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 53.Fawcett SL, Birch EE. Validity of the Titmus and Randot circles tasks in children with known binocular vision disorders. J AAPOS. 2003;7:333–338. doi: 10.1016/s1091-8531(03)00170-8. [DOI] [PubMed] [Google Scholar]
- 54.Wilson ME, Parks MM. Primary inferior oblique overaction in congenital esotropia, accommodative esotropia, and intermittent exotropia. Ophthalmology. 1989;96:950–955. doi: 10.1016/s0161-6420(89)32774-6. [DOI] [PubMed] [Google Scholar]
- 55.Miller MM, Guyton DL. Loss of fusion and the development of A or V patterns. J Pediatr Ophthalmol Strabismus. 1994;31:220–224. doi: 10.3928/0191-3913-19940701-06. [DOI] [PubMed] [Google Scholar]
- 56.Ingram RM, Arnold PE, Lucas J. Emmetropisation, squint, and reduced visual acuity after treatment. Br J Ophthalmol. 1991;75:414–416. doi: 10.1136/bjo.75.7.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atkinson J, Anker S, Bobler W, et al. Normal emmetropization in infants with spectacle correction for hyperopia. Invest Ophthalmol Vis Sci. 2000;41:3726–3731. [PubMed] [Google Scholar]
- 58.Ingram RM, Gill LE, Lambert TW. Effect of spectacles on changes of spherical hypermetropia in infants who did, and did not, have strabismus. Br J Ophthalmol. 2000;84:324–326. doi: 10.1136/bjo.84.3.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kushner BJ. Does overcorrecting minus lens therapy for intermittent exotropia cause myopia? Arch Ophthalmol. 1999;117:638–642. doi: 10.1001/archopht.117.5.638. [DOI] [PubMed] [Google Scholar]
- 60.Shippman S, Weseley CR, Cohen KR. Accommodative esotropia in adults. J Pediatr Ophthalmol Strabismus. 1993;30:368–371. doi: 10.3928/0191-3913-19931101-06. [DOI] [PubMed] [Google Scholar]
- 61.Havertape SA, Whitfill CR, Cruz OA. Early-onset accommodative esotropia. J Pediatr Opthalmol Strabismus. 1999;36:69–73. doi: 10.3928/0191-3913-19990301-05. [DOI] [PubMed] [Google Scholar]
- 62.Sampson WG. Correction of refractive errors: effect on accommodation and convergence. Trans Am Acad Ophthalmol Otolaryngol. 1971;75:124–132. [PubMed] [Google Scholar]
- 63.Havertape SA, Cruz OA, Miyazaki EA. Comparison of methods for determining the AC/A ratio in accommodative esotropia. J Pediatr Ophthalmol Strabismus. 1999;36:178–183. doi: 10.3928/0191-3913-19990701-05. [DOI] [PubMed] [Google Scholar]
- 64.Arnoldi K, Shainberg M. High AC/A: Bifocals? Surgery? Or nothing at all? Am Orthopt J. 2005;55:62–75. doi: 10.3368/aoj.55.1.62. [DOI] [PubMed] [Google Scholar]
- 65.Pratt-Johnson JA, Tillson G. The management of esotropia with high AC/A ratio (convergence excess) J Pediatr Ophthalmol Strabismus. 1985;22:238–242. doi: 10.3928/0191-3913-19851101-09. [DOI] [PubMed] [Google Scholar]