Abstract
In order to examine the effectiveness of applying a static magnetic field (SMF) for increasing bone mineral density (BMD), we assessed the degree of osteopenia by dual-energy X-ray absorptiometry (DEXA), the metabolism measuring system, and histological examination of bone tissue in an ovariectomized (OVX) rat model. Thirty-six female Wistar rats (8 weeks old, 160–180 g) were divided into three groups. The rats in the OVX-M group were exposed to SMF for 12 weeks after ovariectomy. The ovariectomized rats in the OVX-D group were not exposed to SMF as a control. The rats in the normal group received neither ovariectomy nor exposure to SMF. Twelve-week exposure to SMF in the OVX-M group inhibited the reduction in BMD that was observed in the OVX-D group. Moreover, in the OVX rats, before exposure to SMF, there was no clear difference in the level of locomotor activity between the active and resting phases, and the pattern of locomotor activity was irregular. After exposure of OVX rats to SMF, the pattern of locomotor activity became diphasic with clear active and resting phases, as was observed in the normal group. In the OVX-M group, the continuity of the trabecular bone was maintained more favorably and bone mass was higher than the respective parameters in the OVX-D group. These results demonstrate that exposure to SMF increased the level of locomotor activity in OVX rats, thereby increasing BMD.
Keywords: locomotor activity, ovariectomized (OVX) rat, static magnetic fields (SMF), thermography
Introduction
The biological response to exposure to static magnetic field (SMF) has recently been widely discussed from the perspective of possible health benefits as well as potential adverse effects. With respect to the possible health benefits, it has been reported that local SMF stimulation is beneficial for pain, nerve regeneration (1), imflammation (2), blood flow (3) and united fractures (4). SMF has been used to provide pain relief from neck and shoulder pain and knee pain due to ischemic conditions of the blood microcirculation (5–7).
Osteoporosis patients with climacteric disturbance are frequently encountered in Oriental medicine clinics, but their osteoporosis is rarely treated. The ovariectomized (OVX) rat has been usually used as a model of osteopenia to study climacteric disturbance (8).
After menopause or ovariectomy, women tend to develop osteopenia and menopausal symptoms, including hot flashes, abnormal feelings, palpitations and insomnia. In particular, ovariectomy before menopause has been reported to cause osteoporosis and severe menopausal symptoms because of sudden estrogen deficiency (9–11). It has recently been reported that application of SMF is useful for the treatment of a decrease in bone mineral density (BMD) (12,13).
In a previous study, we found that traditional Chinese medicine alternative climacteric disturbance and inhibited the decrease in BMD observed in post-menopausal women.
In the present study, we exposed OVX rats, which served as an experimental osteopenia model, to SMF and obtained interesting findings.
Materials and Methods
Study Animals and Environmental Conditions
This study was approved by the Animal Committee of Kansai College in Osaka, Japan. Female Wistar rats (age, 7 weeks; body weight, ∼150 g) were purchased from Japan Crea Co., Ltd (Shizuoka, Japan). The animals were housed individually in cages and kept in a room maintained at a temperature of 23.0 ± 1.0°C with a relative humidity (RH) of 55.0 ± 5.0% and a 12 h/12 h light-dark cycle (light, 9:00 a.m.–9:00 p.m.). Solid rodent chow and tap water were given ad libitum. After 1 week of acclimation under these conditions, animals showing favorable growth were selected and used for further studies.
Experimental Groups
Thirty-six rats aged 8 weeks were divided into 3 groups of 12 rats each. The rats in the OVX-M group underwent ovariectomy at 8 weeks of age and then, starting at 12 weeks of age, they underwent 12 week exposure to SMF. The rats in the OVX-D group underwent ovariectomy at 8 weeks of age and were not subsequently exposed to SMF. The rats in the normal group did not undergo ovariectomy or exposure to SMF.
Experimental Schedule and Conditions for Exposure
In the OVX-M group, two 200 mT magnets (Pip-Fujimoto Co., Ltd, Osaka, Japan) were fixed along opposite sides of the cage (there was an average of 30 mT of magnetic force at the center of the cage), and each rat was exposed to SMF all day for 12 weeks (Fig. 1A–C). In the OVX-D group, which was the control group, two 0 mT magnetic stones were similarly placed, and no magnetic field was applied.
Figure 1.
Schematic diagram of magnet show its top plan view (A) and photograph (B). The mean magnetic force at the center of the cage was 30 mT (C).
After ovariectomy, the rats in the OVX-M and OVX-D groups were not exposed to the respective magnetic stones for 4 weeks; then, the respective magnetic stones were placed along opposite sides of the cage of each rat for 12 weeks.
Observations
Measurement of Body Weight (BW), Serum Total Cholesterol (T-chol) Level and Urinary Deoxypyridinoline (Dpd) Level Before and After 12 weeks of Exposure to SMF
The BW of each rat was measured before and after 12 weeks of exposure to SMF in the OVX-M group, and at the respective time points in the OVX-D and normal groups. Blood samples (1.5 mL) were collected from the cervical vein under ether anesthesia, and the serum T-chol level was determined using the Serum Test Kit (Wako Pure Chemicals Industry Ltd, Wakayama, Japan).
Measurement of Tail Surface Temperature Before and After Exposure to SMF
The tail surface temperature was measured using a thermograph (TVS-2300 MkIIST, Japan Abionics Co., Ltd, Tokyo, Japan) in all rats. To avoid the influence of the haircoat, the tail temperature, which is used as an indicator of the peripheral circulation, was measured (14). The tail surface temperature was measured before and after 12 weeks of exposure to SMF in the OVX-M group, and at the respective time points in the OVX-D and normal groups. After 15 min of acclimation to the environment of a windless room maintained at a temperature of 15.0 ± 1.0°C and a relative humidity of 50.0 ± 10.0%, the tail surface temperature was measured in conscious animals. The thermography device was at a distance of 1 m from the rat during measurement of the tail surface temperature.
Measurement of Locomotor Activity Before and After Exposure to SMF
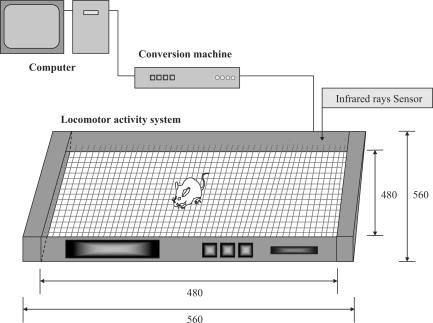
The level of locomotor activity was measured using a metabolism measuring system (SCANET MV-10; MELQUEST Toyama, Japan). Locomotor activity was measured over a 24 hour period (1 day) before starting magnetic stimulation and after 12 weeks of exposure to SMF in the OVX-M group, and at the respective time points in the OVX-D and normal groups. The level of total locomotor activity at 30 min intervals was shown graphically over a 24 hour period and this was used as the daily behavioral pattern (Fig. 2). The daily locomotor activity was defined as the total locomotor activity over a 24 hour period. The level of locomotor activity in the daytime (9:00 a.m.–9:00 p.m.) and nighttime (9:00 p.m.–9:00 a.m.) was measured (15).
Figure 2.
Locomotor activity system.
Measurement of Bone Mineral Density (BMD), Bone area and Urinary Deoxypyridinoline (Dpd) Level
After 12 week exposure to SMF in the OVX-M group and at the respective time points in the OVX-D and normal groups, all rats were sacrificed and their tibia bones were removed. The BMD was measured by dual-energy X-ray absorptiometry (DEXA) using the DCR-600R Dichroma scan (Aloca Co., Ltd, Tokyo, Japan). Histological examination of the tibia bones was performed as described by Ueno (16), and morphological measurements were made (17). Urine samples were collected by pooling for 24 hours using rat metabolic cages, and the urinary level of Dpd was measured by the Elisa method (18).
Statistical Analysis
The data obtained in each group are expressed as mean ± standard error. The significance of time-related differences between the groups was assessed by the Wilcoxon rank sum test, and the level of significance was set at P < 0.05.
Results
Changes in BW and T-chol Level Before and After Exposure to SMF
Before exposure to SMF, BW and serum T-chol levels at 12 weeks were higher in the OVX-M and OVX-D groups than in normal group (P < 0.001), suggesting a tendency of obesity in animals in the OVX-M and OVX-D groups (Figs 3 and 4).
Figure 3.
Change in BW of OVX and normal rats before and after 12 weeks of exposure to SMF. OVX-D and normal groups were not exposed to SMF. Significant difference from normal group, mean ± SEM. **P < 0.01.
Figure 4.
Change in Serum T-Chol of OVX and normal rats before and after 12 weeks of exposure to SMF. OVX-D and normal groups were not exposed to SMF. Significant difference from normal group, mean ± SEM. **P < 0.01.
Changes in Tail Surface Temperature Before and After Exposure to SMF
Before exposure to SMF, the tail surface temperature was significantly lower in the OVX-M and OVX-D groups than in the normal group (P < 0.0001). After 12 weeks of exposure to SMF, there was no significant difference in the tail surface temperature between the OVX-M group and normal group (Fig. 5).
Figure 5.
Change in tail surface temperature of OVX and normal rats before and after 12 weeks of exposure to SMF. OVX-D and normal groups were not exposed to SMF. Significant difference from normal group, mean ± SEM. ***P < 0.001. Significant difference from OVX-M group, mean ± SEM. †††P < 0.001. Significantly different between before and after in OVX-M group, ##P < 0.01.
Changes in Locomotor Activity Before and After Exposure to SMF
Before exposure to SMF, in the normal group, the pattern of locomotor activity was regular. In the OVX-M and OVX-D groups, there was no clear difference in the pattern of locomotor activity between the active and resting phases and the pattern of locomotor activity was irregular. After exposure of the OVX-M group to SMF, the pattern of locomotor activity became diphasic with clear active and resting phases, similar to that observed in the normal group (Fig. 6).
Figure 6.
Change of locomotor activity of OVX-M, OVX-D and normal groups 24 hours of exposure to SMF. In OVX rats, before exposure to SMF, there was no clear difference between the active and resting phases, and the pattern of activity was irregular. After exposure, the pattern of activity became diphasic, with clear active and resting phases as was observed in the normal group.
Moreover, the daily level of locomotor activity at 12 weeks was significantly higher in the normal group than in the OVX-D group (P < 0.01). The daily level of locomotor activity at 12 weeks of age after exposure to SMF in the OVX-M group was significantly higher than that in the OVX-D group (P < 0.01) (Fig. 7).
Figure 7.
Change in locomotor activity of OVX and normal rats before and after 12 weeks of exposure to SMF. OVX-D and normal groups were not exposed to SMF. Significant difference from normal group, mean ± SEM. *P < 0.05, **P < 0.01. Significant difference from OVX-M group, mean ± SEM. †P < 0.05.
Change in BMD, Bone area and Urinary Dpd Level (Table 1)
Table 1.
BMD, bone area and urinary Dpd level in OVX and normal rats after 12 week exposure to SMF
| Bone mineral density (g cm−2) | Bone area (%) | Urinary Dpd levels (nmol per mmol Cre) | |
|---|---|---|---|
| OVX-M | 154.3 ± 2.1†††** | 32.7 ± 2.4†††* | 116.2 ± 14.8†† |
| OVX-D | 136.4 ± 3.5*** | 17.9 ± 2.9*** | 139.6 ± 13.6* |
| Normal | 179.8 ± 2.5 | 50.7 ± 5.8 | 82.4 ± 6.0 |
OVX-D and normal groups were not exposed to SMF. Significant difference from the normal group, mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001. Significant difference from OVX-M group, mean ± SEM. ††P < 0.01, †††P < 0.001.
After 12 weeks of exposure to SMF, urinary Dpd levels were high and bone resorption was significantly enhanced in OVX-D group compared with the normal group. BMD was significantly lower in the OVX-M and OVX-D groups than in the normal group (P < 0.01) (P < 0.001) (Table 1). However BMD was significantly higher in the OVX-M group than in the OVX-D group (P < 0.0001).
Histological findings of osteoporosis were observed in the OVX-D group. In the OVX-M group, the continuity of the trabecular bone was maintained more favorably and the bone area of the OVX-M group was higher than that of the OVX-D group (P < 0.001). The urinary Dpd level was also higher in the OVX-M group than in the normal group (P < 0.01), but it was significantly lower in the OVX-M group than in the OVX-D group (P < 0.05) (Table 1).
Discussion
Patients with climacteric disturbance with osteoporosis are frequently encountered in the orthopedics clinic, but the effects of static magnetic therapies on climacteric disturbance symptoms have rarely been investigated.
On the other hand, OVX rats have been widely studied and are used as a model of osteopenia and climacteric disturbance since they have reduced secretion of estrogens due to ovariectomy. Estrogens induce the growth of reproductive organs and the proliferation of mammary glands, facilitate Ca deposition to bones and reduce serum T-chol level. Therefore, a variety of symptoms are induced when there is a deficiency of estrogens (19,20).
In the present study, the serum T-chol level increased in the OVX-M and OVX-D groups after ovariectomy, indicating a possible decreased secretion of estrogens. The urinary Dpd level directly reflects bone resorption and is a good index for the following reasons: Dpd is released in association with the decomposition of type I collagen during bone resorption; it is not released at the time of bone formation; the Dpd level is not affected by intake of meals; and Dpd is excreted into the urine without being metabolized. Because the urinary Dpd levels were higher in the OVX-M and OVX-D groups after ovariectomy than in the normal group, it was confirmed that bone resorption was enhanced by ovariectomy.
The tail surface temperature of OVX rats showed a clear rise after prolonged exposure to SMF for 12 weeks, suggesting that exposure to SMF improves peripheral circulation. Using a metabolism measuring system, it was confirmed that in ovariectomized rats, the locomotor activity was higher after 12 weeks of exposure to SMF than before exposure. Furthermore, it has been reported that SMF therapy relieved pain in patients with frozen shoulder and low back pain (21). Therefore, the increase in locomotor activity was presumably ascribable to the removal of pain rather than to the induction of stress by SMF.
The mechanism of action of SMF may be as follows: the magnetic force increases the release of acetylcholine (ACh) from cholinergic vasodilator nerve endings by inhibiting the effect of cholinesterase, resulting in vasodilation. In other words, the recovery of circulation might cause some effects by altering BMD.
The effects of application of a 1 mT SMF for 10 min on the cutaneous microcirculatory system included enhanced vasodilatation with increased vasomotion under noradrenaline-induced high vascular tone, and vasoconstriction with reduced vasomotion under ACh-induced low vascular tone. Briefly, these phenomena suggest that SMF can modulate vascular tone due to the biphasic modification of vasomotion in cutaneous tissue (22).
A 130 mT (Ferrite) magnet was externally attached to neck and shoulder continuously for up to 3 weeks. The subchronic effects caused by continuous exposure to 130 mT for 3 weeks included significantly enhanced long-lasting vasodilatation in accordance with increased vasomotion compared with the control (sham exposure) group that had been exposed to dummy magnets (23).
We previously reported that administration of oriental medicine for the treatment of menopausal symptoms in post-menopausal women improved the menopausal symptoms and inhibited the reduction in BMD (24). In the present study, after exposure to SMF, the irregular pattern of locomotor activity of ovariectomized rats changed to a night-day diphasic pattern as was observed in the normal rats, and there was a significant increase in overall locomotor activity.
Physical therapy including therapeutic exercise of bone was reported to be very effective for osteoporosis (25). Briefly, since the dynamic exercise of bone is considered to improve the bone structure and increase BMD, physical therapy is generally preferable to drug therapy, which may cause side effects. In Japanese individuals, it was confirmed by a quantitative ultrasound method that BMD among people who habitually exercised was significantly higher than that among people who ate nutritious foods but did not exercise (26). These results suggest that the increased BMD in the OVX-M group was partially ascribable to increased locomotor activity. However, the possibility that SMF directly affects the bone cannot be ruled out.
Although BMD may increase to some extent by application of SMF, BMD may not necessarily be markedly increased by it alone. We consider it important to combine application of SMF with Western medicine or exercise therapy.
References
- 1.Veliks V, Ceihnere E, Svkis I, Aivars J. Static magnetic field influence on rat brain function detected by heart rate monitoring. Bioelectromagnetics. 2004;25:211–15. doi: 10.1002/bem.10186. [DOI] [PubMed] [Google Scholar]
- 2.Taniguchi N, Kanai S, Kawamoto M, Endo H, Higashino H. Study on application of static magnetic field for adjuvant arthritis rats. Evid based complement alternat med. 2004;1:187–92. doi: 10.1093/ecam/neh024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bassett A. Therapeutic uses of electric and magnetic fields in orthopedics. In: Carpenter DO, Ayrapetyan S, editors. Biological Effects of Electric and Magnetic Fields Beneficial and Harmful Effects. San Diego: Academic Press; 1994. pp. 13–48. [Google Scholar]
- 4.Kotani H, Kawaguchi H, Shimoaka T, Iwasaka M, Ueno S, Ozawa H, et al. Strong static magnetic field stimulates bone formation to a definite orientation in vitro and in vivo. J Bone Miner Res. 2002;17:1814–21. doi: 10.1359/jbmr.2002.17.10.1814. [DOI] [PubMed] [Google Scholar]
- 5.Vallbona C, Hazlewood CF, Jurida G. Response of pain to static magnetic fields in postpolio patients: A double-blind pilot study. Arch Phys Med Rehabll. 1997;78:1200–3. doi: 10.1016/s0003-9993(97)90332-4. [DOI] [PubMed] [Google Scholar]
- 6.Kanai S, Okano H, Orita M, Abe H. Clinical study of neck and shoulder pain for therapeutic effectiveness with application of static magnetic field. J Jpn Sco Pain Clin. 1996;3:11–17. [Google Scholar]
- 7.Segal AN, Toda Y, Huston J, Saeki Y. Two configurations of static magnetic fields for treating rheumatoid arthritis of the knee: A double-blind clinical trial. Arch Phys Med Rehabll. 2001;82:1453–60. doi: 10.1053/apmr.2001.24309. [DOI] [PubMed] [Google Scholar]
- 8.Hidaka S, Okamoto Y, Nakajima K, Suekawa M, Liu SY. Preventive effects of traditional Chinese (Kampo) medicines on experimental osteoporosis induced by ovariectomy in rats. Calcified Tissue International. 1997;61:239–46. doi: 10.1007/s002239900329. [DOI] [PubMed] [Google Scholar]
- 9.Jiu LJ, Morikawa N, Omi N, Ezawa I. The effect of Tochu bark on bone metabolism in the rat model with ovariectomized osteoporosis. J Natr Scivit. 1994;261:40–7. doi: 10.3177/jnsv.40.261. [DOI] [PubMed] [Google Scholar]
- 10.Harada K, Nakata Y. Effects of Kampo Therapy on serum estrogen levels and bone mineral content in climacteric disorder. JPN J Orient Med. 1995:521–7. [Google Scholar]
- 11.Yamaguchi K, Yashita T, Kato M. Pharmacological effects of three products of Chinese herbal remedies on experimental osteoporosis induced by ovariectomy in rats. Oyo Yakuri. 1997;57:13–30. [Google Scholar]
- 12.Xu S, Tomita N, Ohhata R, Ikada Y. Static magnetic field effects on bone formation of rats with an ischemic bone model. Bio-Medical Materials and Engineering. 2001;11:257–63. [PubMed] [Google Scholar]
- 13.Yan QC, Tomita N, Ikada Y. Effects of static magnetic field on bone formation of rat femurs. Medical Engineering & Physics. 1998;20:397–402. doi: 10.1016/s1350-4533(98)00051-4. [DOI] [PubMed] [Google Scholar]
- 14.Kanai S, Okano H, Abe H. Efficacy of Toki-shigyakuka-gosyuyu-syokyo-to (Danggui-Sini-Jia-Wuzhuyu-Shengjiang-Tang) on peripheral circulation in autonomic disorders. 1997;25:69–78. doi: 10.1142/S0192415X9700010X. [DOI] [PubMed] [Google Scholar]
- 15.Ohki-Hamazaki H, Watase K, Yamamoto K, Ogura H, Yamano M, Yamada K, Maeno H, Imaki J, Kikuyama S, Wada E, Wada K. Mice lacking bombesin receptor subtype-3 develop metabolic defects and obesity. Nature. 1997;390:165–9. doi: 10.1038/36568. [DOI] [PubMed] [Google Scholar]
- 16.Ueno T. Comparative study of various methods for identification of osteoid matrix in decalcified bone. Jpn Oral Biol. 1985;27:495–508. [Google Scholar]
- 17.Taniguchi N, Kanai S. Study of static magnetic fields to osteopenia model rat. J Jpn Biomagnetism and Bioelectromagnetics Soc. 2003;16:74–5. [Google Scholar]
- 18.Eastell R. Biochemical markers of bone resorption compared with estimates from radiotracer kinetic studies in osteoporosis. J bone Miner. 1997;12:59–65. doi: 10.1359/jbmr.1997.12.1.59. [DOI] [PubMed] [Google Scholar]
- 19.Ettinger B, Genant HK, Cann CE. Postmenopausal bone loss is prevented by treatment with low-dosage estrogen with calcium. Ann Int Med. 1897;106:40–5. doi: 10.7326/0003-4819-106-1-40. [DOI] [PubMed] [Google Scholar]
- 20.Bollen AM, Eyred DR. Bone. 1994;15:31–4. doi: 10.1016/8756-3282(94)90888-5. [DOI] [PubMed] [Google Scholar]
- 21.Kanai S, Okano H, Susuki R, Abe H. Therapeutic effectiveness of static magnetic fields for low back pain monitored with thermography and deep body thermometry. J Jpn Soc Pain Clin. 1998;5:5–10. [Google Scholar]
- 22.Okano H, Ohkubo C. Modulatory effects of static magnetic fields on blood pressure in rabbits. Bioelectromagnetics. 2001;22:408–18. doi: 10.1002/bem.68. [DOI] [PubMed] [Google Scholar]
- 23.Kanai S, Taniguchi N, Kawamoto M, Endo H, Higashino H. Effect of static magnetic field on pain associated with frozen shoulder. Pain Clinic. 2004;16:173–9. [Google Scholar]
- 24.Kanai S, Taniguchi N. The effect of Kami-kihi-to on the maintenance of bone mass in patients with osteoporosis. J Orient Med. 1988;49:59–66. [Google Scholar]
- 25.Hayashi Y. Physical training. J J Clin Med. 1998;56:1551–6. [PubMed] [Google Scholar]
- 26.Suzuki Y, Uehara R, Ide M. Osteoporosis in rheumatoid arthritis. J J Clin Med. 1998;56:1598–603. [PubMed] [Google Scholar]