Abstract
Background: It has been suggested that patients with somatoform disorders are high utilizers of medical care, yet interpretation of studies has been difficult because of variant methods of diagnosis. The goal of this study was to compare 5 different methods of classification on the same group of subjects and to examine prevalence rates of somatoform disorders and medical utilization.
Method: Subjects completed a demographic questionnaire in the physician's office and the somatization section of the Diagnostic Interview Schedule (DIS) by telephone. Subsequently, their medical charts were examined. Using the 5 methods of diagnosis, somatizers were compared with nonsomatizers for level of utilization of medical services. The setting was a medical school–based family practice residency training center. Participants were 119 patients waiting to see their family doctors. The main outcome measures were prevalence of somatization symptoms and chart information (utilization, number of health problems).
Results: One subject met the Diagnostic and Statistical Manual (DSM-IV)–based DIS criteria for somatization disorder. With the Bucholz modification for scoring the DIS, 10 subjects were diagnosed with somatization disorder. With the abridged Escobar criteria of 6 symptoms, 7 subjects met diagnostic criteria, while 28 met the criteria for multisomatoform disorder of 3 symptoms, as suggested by Kroenke. The diagnosis of undifferentiated somatoform disorder, requiring only 1 unexplained symptom, was obtained by 94 of the subjects.
Conclusion: Findings from this study revealed widely divergent prevalence rates of somatoform disorders, depending on methods of diagnosis used. Correlation with rates of medical utilization is suggested as an external criterion for validating diagnostic methods.
It has been stated that somatization is a frequent occurrence in the primary care medical setting.1–3 Individuals with the tendency to express and experience their emotional distress in physical terms would be expected to seek medical care frequently. Rather than interpret their distress as emotional in origin and subsequently seek mental health services, they go to primary care physicians with physical symptoms.4 However, in the absence of organic pathology or disease processes to diagnose and treat, the medical appointment ends up being frustrating to both the patient and the physician.5
The cost of medical care for patients with the tendency to somatize may be inordinately high because of frequent appointments, laboratory studies, and expensive and invasive specialized procedures.6 Early recognition of patients with somatization tendencies would be beneficial so that more effective treatment could begin sooner7 and unnecessary services could be avoided.
Kirmayer and associates3 have noted the paucity of research on somatizing patients in primary care settings and have emphasized the need for such studies, rather than those carried out in tertiary care or specifically psychiatric settings. Many somatizing patients never come to the attention of a mental health professional, even though such services could be very helpful, especially in collaboration with the primary care physician. It is surprising that there are so few studies on somatization in primary care and family medicine settings6,8–12; this may be due to the absence of diagnostic methods relevant to primary care.13
Differing methods of diagnosing somatization have hampered research in this area.8 The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)14 lists 2 relevant conditions: somatization disorder (which requires at least 8 symptoms distributed across 4 categories of symptoms) and undifferentiated somatoform disorder (which requires only 1 unexplained physical symptom). DSM-IV also includes the diagnosis of somatoform disorder not otherwise specified, but because of its broad inclusiveness, this category is not seen as useful in research studies or relevant in our work. Compared with the earlier DSM-III-R15 criteria for somatization disorder, the fourth edition criteria are divided into 4 symptom groupings, as well as being condensed and simplified, based on literature review and field trial results. The DSM-III-R criteria, which required 13 unexplained symptoms, had been criticized as overly restrictive,1,16 resulting in few identified cases. It is not clear whether the DSM-IV modifications will result in a more useful diagnostic category. The diagnosis of undifferentiated somatoform disorder, on the other hand, has been criticized as unvalidated and probably too inclusive,17 since it requires only 1 unexplained symptom.
Alternative, potentially more useful methods of diagnosing somatization have been suggested. Escobar and colleagues18 have proposed abridged diagnostic criteria, based on the DSM-III-R. This approach requires only 6 symptoms for females and 4 for males. On the basis of their research using this method, they have found that it does identify high utilizers of medical services and thus is a valid approach. The Primary Care edition of the DSM-IV (DSM-IV-PC)19 describes a condition called multisomatoform disorder, which is comparable to a moderately severe undifferentiated somatoform disorder. This category requires 3 or more current unexplained physical symptoms and a history of physical symptoms. Kroenke and colleagues17 evaluated this designation with their work on the PRIME-MD (Primary Care Evaluation of Mental Disorders)20 and provided data on its utility and validity.
Another approach involves a modification in the method of gathering information about symptoms. The Diagnostic Interview Schedule (DIS),21 a structured interview method based on the DSM, has frequently been used in research studies for making diagnoses of various mental disorders, including somatization disorder. However, this method in particular has been criticized as too restrictive in the area of somatization disorder.8,11 As a result, Bucholz and colleagues22 have used a modification of the weighting used in scoring probes for various physical symptoms. This change in scoring results in a broader definition of somatization that includes all clinically significant symptoms, irrespective of medically or medication-explained causes. The results of their research support the utility of this method.
The purpose of our study was to evaluate the prevalence of somatoform disorders in a family practice office and to explore the rates of utilization of medical services in patients with these conditions. In addition, because of the confusion over which method of categorization to use, multiple methods were used to assess the relative prevalence of somatoform disorders and their association with utilization. The 5 methods of categorization were (1) the standard DSM-IV diagnosis requiring at least 8 symptoms, distributed as specified over 4 symptom categories, based on standard scoring of the DIS; (2) standard DSM-IV diagnosis, based on the modified scoring method used by Bucholz and associates22; (3) the abridged definition using the Escobar criteria of 6 symptoms for females and 4 for males12,18; (4) the multisomatoform disorder diagnosis from the DSM-IV-PC, requiring 3 or more symptoms; and (5) the DSM-IV diagnosis of undifferentiated somatoform disorder, requiring only 1 unexplained symptom.
METHOD
Subjects
All patients in the practice at least 1 year, 18 years old or above, waiting to see their physician in a medical school–based family practice residency training center were invited to participate in the study. They represented patients of 22 resident and faculty physicians. Patients with cognitive problems that would limit their ability to participate (e.g., mental retardation, status post cerebrovascular accident) were not included in the sample.
Procedure
The Institutional Review Board of the sponsoring institution granted approval of the research protocol. The procedure was explained both in writing and orally by the research assistant, and subjects signed an informed consent form. Subjects completed a battery of instruments that included personality scales, demographic data, and lifestyle habits. Within a week of their office visit, patients were called by a research assistant and administered the somatization section of the DIS.21 Results from the personality scales and lifestyle habits questionnaire are not included in this article; only the demographic data and the DIS are discussed.
Once complete self-report and interview data from subjects were obtained, their medical charts were examined for data on utilization of services during the preceding year. Specific areas considered were number of visits for chronic problems, acute problems, nurse checks, health maintenance (well check-ups), and laboratory studies; number of chronic and acute problems listed by the physician in the chart; number of telephone calls to the practice; and weight of the chart.
Categorization Criteria
The DSM-IV requires at least 8 symptoms, distributed over 4 symptom groups (4 pain symptoms, 2 gastrointestinal symptoms, 1 sexual symptom, and 1 pseudoneurologic symptom). The Bucholz modification requires the same number of symptoms, but is more lenient in determining whether the cause for the symptom is organic or not. The Escobar method is based on the DSM-III-R criteria of 13 symptoms; however to meet Escobar criteria, females are required to have only 6 symptoms and males to have 4. The multisomatoform disorder of Kroenke requires only 3 unexplained physical symptoms. The undifferentiated somatoform disorder category requires only 1 unexplained physical symptom.
RESULTS
A total of 172 patients filled out complete initial demographic information while waiting to see their physicians. The mean ± SD age was 51.54 ± 17.58 years, with 52% female and 81% white. About 49% were currently married, with the remaining subjects distributed among the divorced, single, and widowed groups. Thirty-two percent were high school graduates only, and an additional 58% had at least some college education. The remaining 10% did not graduate from high school.
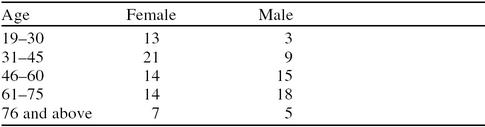
Although efforts were made to contact all of these subjects later by telephone to administer the somatization section of the DIS, only 119 could be reached, even though the noncontacted subjects had been called as often as 5 times and were called at times they indicated they would probably be available. An analysis of the demographic differences between those contacted and those not contacted revealed that those reached rated themselves as being in worse health (t = 2.62; p < .01). This may account for why they were more accessible by telephone. Of the 119 subjects, 58% were female and 82% were white, with a mean age of 51.5 years (range, 19–91 years). The breakdown of subjects by age and sex can be found in Table 1.
Table 1.
Categorization of 119 Subjects by Age and Sex
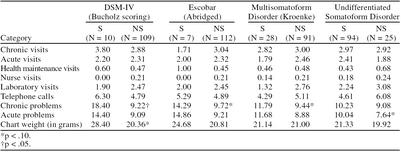
With the standard DIS method of diagnosis, 1 subject (0.8%) met DSM-IV criteria for somatization disorder. (Although the DIS is based on DSM-III-R, adequate information is gathered to make a diagnosis according to DSM-IV criteria.) With the Bucholz modification of the DIS scoring, 10 subjects (8%) met DSM-IV criteria for somatization disorder. (Application of the DSM-III-R criteria of 13 symptoms did not identify any subjects meeting this standard.) With the Escobar abridged criteria, 7 subjects (6%) met criteria for somatization. With the Kroenke approach, 28 (24%) met criteria for multisomatoform disorder. Ninety-four subjects (79%) had 1 unexplained symptom for at least 6 months, thus meeting the DSM-IV criterion for undifferentiated somatoform disorder. Utilization rates for somatizers and nonsomatizers, as determined by 4 of the diagnostic methods, can be found in Table 2. Because only 1 subject met DSM-IV criteria by standard scoring, results based on this method are not included in Table 2.
Table 2.
Utilization Rates for Somatizers (S) and Nonsomatizers (NS)
The 1 subject identified as having somatization disorder by the standard DSM-IV criteria was markedly different from the other subjects in this sample. Compared with other subjects, this subject had more than 4 times as many chronic problems listed in the chart (p < .001) and more than 5 times as many acute problems (p < .001). This subject made almost 5 times as many phone calls to the practice (p < .01) and had a chart that was more than 3 times as heavy (p < .001). The 10 subjects identified with somatization disorder using the Bucholz scoring modification of the DIS had more chronic problems listed in their charts (p < .05) than those not identified as somatizers by the Bucholz method. There was also a trend for somatizers to have heavier charts (p < .10). Application of both the Escobar abridged and the multisomatoform disorder criteria resulted in trends for subjects identified by these methods to have more chronic problems listed in their charts than those not identified as somatizers (p < .10). Subjects diagnosed with undifferentiated somatoform disorder tended to have more acute problems listed in their chart (p < .10).
DISCUSSION
Confusion related to the multiple methods available for diagnosing somatization disorder, as well as interest in whether current methods have relevance in primary care settings, provided the impetus for our study. In addition, reports that standard administration of the DIS in diagnosing somatization disorder might be overly stringent led us to apply other approaches.
Different rates of prevalence with the methods used were to be expected, given the varied rigor of each approach. Applying DSM-IV criteria identified 1 subject with somatization disorder, whereas application of the DSM-III-R criteria did not identify any. This would suggest that modifications made in diagnosis from one edition of the DSM to the other have not led to a great increase in the rate of identified prevalence. However, the 1 subject with this diagnosis was clearly different from the rest of the sample, suggesting that this approach, although not very sensitive, is quite discriminating. Using the Bucholz modification for scoring of the DIS resulted in the identification of 10 subjects with somatization disorder. The fact that these 10 subjects had more chronic problems supports the value of this approach to diagnosis. However, the Bucholz modification clearly did not discriminate as powerfully as standard scoring of the DIS. The Escobar abridged criteria, which had been recommended as a more sensitive method, identified only 7 (about 6%) of 119 subjects, indicating that even with the Escobar relaxed requirement of fewer symptoms compared with DSM criteria, relatively few patients were identified.
In considering the use of methods of diagnosis that differ in restrictiveness, the trade-offs related to decision theory need to be considered. While the standard DSM-IV method identified a subject who clearly showed traits widely accepted as characteristic of a somatization disorder, only 1 subject met this level of symptomatology. While finding the “real” prevalence for somatization disorder can be seen as an elusive and somewhat arbitrary pursuit, research findings from previous studies, estimates made by scholars of this topic, and correlations with rates of utilization can provide a helpful perspective.
DeGruy et al.6 reported a prevalence of 9% for patients in a family medicine academic training center. Kirmayer and Robbins8 have estimated a rate in primary care settings of about 25% to 30%, and Wickramaskera1 has estimated an even higher rate (50%). However, their estimates are based on a broader spectrum of somatization disorders, rather than the more narrow condition described in DSM-IV criteria or researched by deGruy and colleagues.6
Because of the interest in rates of medical utilization and the presumption that such rates are related to diagnosis, an alternative approach to determining validity is available. Exploring rates of medical utilization for groups with various diagnoses would provide one pragmatic index of validity. In applying the external validity criterion of utilization, Escobar abridged criteria, multisomatoform disorder, and undifferentiated somatoform disorder seem to have little value. The latter diagnosis fit 79% of the subjects, and, on this basis alone, its validity can be questioned. However, multisomatoform disorder identified only 24%, a rate consistent with estimates that have been made,8 but higher than the 8.2% rate reported in the original study on multisomatoform disorder.17 It also had been presented as a method that might have particular value in the primary care medical setting17; however, it was not effective in discriminating rates of medical utilization.
It was surprising that the diagnostic approaches used in our study generally did not detect more differences in utilization between those diagnosed as somatizers and those who were not. It may be that although somatization disorders did occur in subjects, effective management by this particular group of academically based physicians contained the level of medical utilization. It has been suggested that patients seen in residency training offices may be different than those seen in community practices.23 Replication in community practices would be informative regarding the generalization of our findings.
One of the limitations of our study stems from our inability to reach a number of subjects by telephone who had originally been contacted in the office. As a result, we were not able to administer the DIS to them. From our analysis, we learned that those we reached were less functional and so may not be as representative of the patients treated in that practice. A possible effect of this bias would be overrepresentation of less functional patients. Accordingly, it could be expected that somatizing patients, because they are less functional,7 may be included in higher than expected numbers in our sample. It is surprising then, that we did not identify a higher rate of somatization, especially with the DIS.
Although our study considered different methods of classifying patients as somatizers, it should be remembered that somatization is a process that can be observed along a continuum of severity. The various cutoff points recommended represent basically arbitrary divisions intended to maximize the predictive ability of the classifications created.
Regardless of method of classification used, somatizing patients will continue to be a challenge to family physicians. There is some evidence that physicians are able to make valid distinctions between somatizers and nonsomatizers without the use of structured methods.24 However, to advance systematic research and practice in this area, there is a need for a formal classification method, and this method must be appropriate and useful within a primary care setting.13 Based on our findings, neither multisomatoform disorder, the Escobar abridged approach, nor undifferentiated somatoform disorder seem especially promising in further research, since none showed significant ability to differentiate high and low utilizers of medical care. Somatization disorder (particularly with the scoring modification developed by Bucholz) deserves further research, given that it was able to partially discriminate the groups based on medical utilization. A continuing challenge with methods for diagnosing somatization disorder will be to weigh the advantages of brevity and convenience against the greater discriminating power of longer methods. While briefer methods have particular appeal especially in busy primary care settings, it is still important that these methods provide clinically relevant and useful information.
Footnotes
Portions of this work were presented at the meetings of the American Psychological Association, Toronto, Ontario, Canada, August 1996, and the Association for Applied Psychophysiology and Biofeedback, Orlando, Fla., April 1998.
REFERENCES
- Wickramaskera I. Somatization: concepts, data, and predictions from the High Risk Model of Threat Perception. J Nerv Ment Dis. 1995;183:15–23. doi: 10.1097/00005053-199501000-00004. [DOI] [PubMed] [Google Scholar]
- Noyes R, Holt C, Kathol R. Somatization: diagnosis and management. Arch Fam Med. 1995;4:790–795. doi: 10.1001/archfami.4.9.790. [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Robbins J, Paris J. Somatoform disorders: personality and the social matrix of somatic distress. J Abnorm Psychiatry. 1994;103:125–136. doi: 10.1037//0021-843x.103.1.125. [DOI] [PubMed] [Google Scholar]
- Lipkowski Z. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145:1358–1368. doi: 10.1176/ajp.145.11.1358. [DOI] [PubMed] [Google Scholar]
- Margo K, Margo G. The problem of somatization in family practice. Am Fam Physician. 1994;49:1873–1879. [PubMed] [Google Scholar]
- deGruy F, Columbia L, Dickinson P. Somatization disorder in a family practice. J Fam Pract. 1987;25:45–51. [PubMed] [Google Scholar]
- Smith GR Jr, Monson RA, Ray DC. Psychiatric consultation in somatization disorder: a randomized controlled study. N Engl J Med. 1986;314:1407–1413. doi: 10.1056/NEJM198605293142203. [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Robbins J. Three forms of somatization in primary care: prevalence, co-occurrence, and sociodemographic characteristics. J Nerv Ment Dis. 1991;179:647–655. doi: 10.1097/00005053-199111000-00001. [DOI] [PubMed] [Google Scholar]
- Bridges K, Goldberg D. Somatic presentation of DSM III disorders in primary care. J Psychosom Res. 1985;29:647–655. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Robbins JM, Dworkind M, et al. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–741. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- Katon W, Lin E, Von Korff M, et al. Somatization: a spectrum of severity. Am J Psychiatry. 1991;148:34–40. doi: 10.1176/ajp.148.7.A34. [DOI] [PubMed] [Google Scholar]
- Escobar J, Burnam M, Karno M, et al. Somatization in the community. Arch Gen Psychiatry. 1987;44:713–718. doi: 10.1001/archpsyc.1987.01800200039006. [DOI] [PubMed] [Google Scholar]
- McWhinney I, Epstein R, Freeman T. Rethinking somatization. Ann Int Med. 1997;126:747–750. doi: 10.7326/0003-4819-126-9-199705010-00037. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised. Washington, DC: American Psychiatric Association. 1987 [Google Scholar]
- Othmer E, DeSouza C. A screening test for somatization disorder. Am J Psychiatry. 1985;42:1146–1149. doi: 10.1176/ajp.142.10.1146. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, de Gruy F, et al. Multisomatoform disorder: an alternative to undifferentiated somatoform disorder for the somatizing patient in primary care. Arch Gen Psychiatry. 1997;54:352–358. doi: 10.1001/archpsyc.1997.01830160080011. [DOI] [PubMed] [Google Scholar]
- Escobar J, Manu P, Matthews D, et al. Medically unexplained physical symptoms, somatization disorder and abridged somatization: studies with the Diagnostic Interview Schedule. Psychiatr Dev. 1989;7:235–245. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Primary Care Version. Washington, DC: American Psychiatric Association. 1995 [Google Scholar]
- Spitzer RL, Williams JBW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 Study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, et al. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Bucholz B, Dinwiddle S, Reich T, et al. Comparison of screening proposals for somatization disorder empirical analyses. Comp Psychiatry. 1993;34:59–64. doi: 10.1016/0010-440x(93)90037-5. [DOI] [PubMed] [Google Scholar]
- Nagel R, Lynch D, Tamburrino M. Validity of the MOS depression screener: comparative results from training center and community settings. Fam Med. 1998;30:362–365. [PubMed] [Google Scholar]
- McGrady A, Lynch D, Nagel R, and et al. Application of the high risk model of threat perception to a primary care patient population. J Nerv Ment Dis. In press. [DOI] [PubMed] [Google Scholar]