Abstract
Background: There is emerging evidence that postpartum women are at risk for the development or worsening of obsessive-compulsive disorder. The purpose of this study was to provide data regarding the demographics, phenomenology, associated psychiatric comorbidity, family history, and response to open treatment with fluvoxamine in subjects with postpartum-onset obsessive-compulsive disorder.
Method: Seven consecutive subjects were recruited from an outpatient obstetrical practice and by advertisement. Subjects completed the Structured Clinical Interview for DSM-IV, the Yale-Brown Obsessive Compulsive Scale, and a semistructured interview for family history, demographic data, and clinical features. Three of the 7 subjects participated in a 12-week, open-label trial of fluvoxamine treatment of postpartum-onset DSM-IV obsessive-compulsive disorder.
Results: The women described a mean age at onset of 28 years, and 4 subjects had a chronic course. Six subjects reported onset after the birth of their first child, and the mean time to onset was 3.7 weeks postpartum. All subjects experienced both obsessions and compulsions and reported aggressive obsessions that involved their children. None of the subjects acted on their obsessions to harm the children, but 5 reported dysfunctional mother-child behavior. All 7 subjects met criteria for at least 1 comorbid psychiatric disorder, with a mood disorder the most common. Family histories were notable for high rates of mood disorders and psychoactive substance use disorders in first-degree relatives. Two of the 3 subjects who entered the open-label trial of fluvoxamine experienced a positive response, defined as a 30% or greater decrease in the total score of the Yale-Brown Obsessive Compulsive Scale.
Conclusion: Obsessive-compulsive disorder may present in the postpartum period and become chronic. Symptoms of the disorder may adversely affect the mother-child relationship, and it is important to assess for obsessions and compulsions in postpartum women who present with anxiety and/or depression. Fluvoxamine may be effective in reducing the symptoms of postpartum-onset obsessive-compulsive disorder. Controlled studies are needed to confirm these findings.
Several lines of evidence suggest that postpartum women are at increased risk for the development or worsening of obsessive-compulsive disorder (OCD). First, retrospective surveys of women with OCD have found that a substantial portion had new onset or exacerbation of OCD during the postpartum period. For example, a retrospective study of outpatients with OCD found that 27 (69%) of 39 women had onset or worsening of OCD with pregnancy or childbirth.1 In that study, the onset of OCD was triggered by the birth of the first child in 6 women (22%) and the birth of subsequent children in 2 (7.5%). Similarly, worsening of OCD was triggered by the birth of the first child in 4 women (15%) and the birth of subsequent children in 2 (7.5%). All had obsessive fears of harming themselves or others, and of those who reported worsening of OCD symptoms, all had a fear of harming the child. Compulsions were also present in each patient. Another retrospective study of a group of outpatient women with OCD reported that 7 (29%) of 24 women with a past history of OCD had postpartum exacerbation of OCD, and 9 (37%) had postpartum depression.2
Second, case reports and case series have described new onset of OCD in the postpartum period. One report described 2 women who developed new onset of OCD in the puerperium.3 The first patient was a 30-year-old woman with no psychiatric history who presented at 4 weeks postpartum with obsessive thoughts of harming her infant and overwhelming anxiety that she might act on the thoughts. She did not have symptoms of depression or psychosis. The second patient was a 34-year-old woman with no psychiatric history who, beginning on the third postpartum day, developed obsessive thoughts of hurting her infant and generalized anxiety. She also did not report depressive or psychotic symptoms. Both women avoided their infants in fear of acting on the thoughts about hurting them. Another retrospective case series described 15 women who experienced the onset of OCD in the postpartum period.4 The mean ± SD time of onset of OCD symptoms was 2.2 ± 1.2 weeks after delivery. Eight women (53%) had no history of psychiatric illness. Seven had a history of panic attacks (N = 5) or generalized anxiety disorder (N = 2). All patients described the obsessive thoughts as their predominant source of distress, and 9 developed secondary major depression 2 to 3 weeks after the onset of OCD. None of the women had compulsions, but all of them avoided their infants and modified their behavior with the children. No woman was psychotic, and the obsessional thoughts were never acted upon. Treatment with serotonin reuptake inhibitors led to complete remission in 4 patients and partial remission in the remaining 11. The authors proposed that postpartum OCD may be a distinct clinical entity with features that include early postpartum onset; repetitive, intrusive thoughts about harming the baby; avoidant behavior; anxiety; panic attacks; secondary depression; and disruption of the mother-infant relationship.4
Third, the obsessions in postpartum OCD may more frequently be associated with aggressive themes than in OCD unrelated to the puerperium. In one study, women with OCD had significantly more aggressive obsessions than men at the onset of OCD.5 The authors related the increased frequency of aggressive obsessions to motherhood and the fear of harming the infant, although they did not report how many women experienced OCD onset in the postpartum period. In another study, aggressive obsessions were found to be more common in women with postpartum-onset major depression compared with women with major depression of non–postpartum onset.6
The purpose of the present study was to provide further data regarding the demographic and phenomenological characteristics and pharmacologic treatment response of a consecutive series of women with postpartum-onset OCD. In addition, this is the first study in postpartum women to systematically assess psychiatric comorbidity using a structured clinical interview and family history of psychiatric illness.
METHOD
Subjects were recruited from the obstetrical clinical outpatient practice at the University of Cincinnati Medical Center and from advertisement for a study of postpartum women with anxiety. Nine potential subjects were identified. Two were excluded from the study because they did not meet DSM-IV criteria for OCD. Seven met the inclusion criteria of 18 years of age or older and the diagnosis of OCD that had developed in the postpartum period. Of the 7 subjects, 5 responded to the advertisement, and 2 were referred from the obstetrical outpatient practice.
After provision of written informed consent, subjects underwent psychiatric evaluation with the Structured Clinical Interview for DSM-IV7 and completed the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).8 Data on demographic and clinical features were obtained by semistructured interview. Family history of any psychiatric disorder in first-degree relatives was determined by semistructured interview using the family history method.9
Three of the 7 subjects were enrolled in an open-label, 12-week trial of fluvoxamine maleate after providing written informed consent following a discussion of the risks and benefits of treatment. Subjects were excluded from the fluvoxamine trial if they had a lifetime diagnosis of schizophrenia, bipolar I disorder, or dementia; current pregnancy or lactation; inadequate birth control; alcohol or other substance dependence within 6 months before enrollment; active suicidality or homicidality; clinically unstable medical disease; history of seizure, stroke, or significant head trauma; use of fluoxetine within 4 weeks or use of other antidepressants within 2 weeks before enrollment; use of depot neuroleptics within 90 days before enrollment; or prior treatment for OCD with fluvoxamine. Of the 4 subjects who did not enter the fluvoxamine trial, 3 were excluded because they wished to continue breast-feeding, and 1 was excluded because of a diagnosis of bipolar I disorder.
After completing the evaluation, subjects received unblinded fluvoxamine, 50 mg/day. The dose was increased on a flexible schedule as tolerated at a maximum rate of 50 mg weekly with a maximum dose of 300 mg/day. Subjects received no other psychotropic medication except for zolpidem tartrate, 5 to 10 mg at bedtime, as needed for insomnia. Psychotherapy was not initiated during the study. Subjects returned for evaluation at completion of weeks 1, 2, 3, 4, 6, 8, and 12 of the study. Subjects also reported any treatment-related adverse events at these times, and pill counts were performed to assess compliance.
The primary outcome measure was the Y-BOCS. Response was defined as ≥ 30% decrease in the Y-BOCS total score, which corresponded to a clinical impression of significant improvement in symptoms and is in the middle of the range defined as improvment in studies of OCD. Secondary outcome measures were the total score changes in the Hamilton Rating Scale for Depression (HAM-D)10 and the Hamilton Rating Scale for Anxiety (HAM-A).11
RESULTS
The age of the subjects at the time of presentation ranged from 26 to 42 years (mean ± SD = 31.7 ± 6.9 years). The sample included 6 white and 1 Hispanic women. Six (86%) of the subjects were married and 1 (14%) was single. All of the subjects completed high school, 4 (57%) had some college, 1 (14%) had completed vocational training, and 1 (14%) had a graduate degree. Two subjects (29%) worked outside the home full time, 3 (43%) had part time work, and 2 (29%) were homemakers.
The reported age at onset of OCD varied from 19 years to 41 years; the mean ± SD age at onset was 28.1 ± 6.8 years; the mean duration of OCD was 3.7 ± 4.5 years with a range of 2 weeks to 11 years. Four of the subjects had experienced the onset of OCD in a past postpartum period and had persistent symptoms, and 3 presented to the study with new onset OCD after a recent delivery. All of the subjects reported that the OCD began in the postpartum period (up to 12 weeks postpartum). Six subjects (86%) noted onset of OCD after the birth of the first child. The time to onset following the birth of the child ranged from 2 days to 12 weeks postpartum with a mean ± SD onset of 3.7 ± 4.9 weeks postpartum (data from 5 subjects).
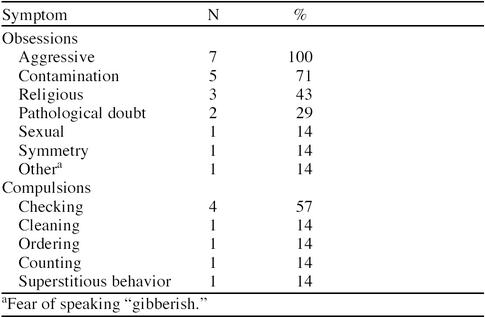
All subjects reported a history of both obsessions and compulsions. At the initial evaluation, the total Y-BOCS score for the 7 subjects ranged from 9 to 28 (mean ± SD = 19.4 ± 8.3). The obsession subtotal score ranged from 7 to 17 (mean ± SD = 11.4 ± 3.3), and the compulsion subtotal score ranged from 0 to 16 (mean ± SD = 8.0 ± 5.9) Table 1 summarizes the content of obsessions and compulsions in the 7 subjects. All of the subjects reported aggressive obsessions that involved their children. The number of aggressive obsessions experienced by each subject ranged from 2 to 4 (mean ± SD = 2.9 ± 0.9). None of the subjects acted on obsessions to harm the children. Five subjects (71%) reported dysfunctional mother-child behavior as a result of the symptoms of OCD. One subject avoided her infant, causing a disruption in the mother-infant relationship. Two subjects noted difficulty allowing their children to participate in usual childhood activities such as school field trips because of fear of something bad happening to them. One of these 2 subjects also took her children to the doctor often for checkups and frequently checked on them by phone when they were outside the home. One subject reported a desire for her infant to be “back in (my) belly” because of fear of something bad happening to the baby. She also could not be separated from her infant and did not allow anyone (including her husband) to hold the infant. Finally one subject continued to breast-feed her 14-month-old child despite her desire to stop breast-feeding because of worsening anxiety when she attempted weaning.
Table 1.
Obsessions and Compulsions in 7 Women With Postpartum-Onset Obsessive-Compulsive Disorder
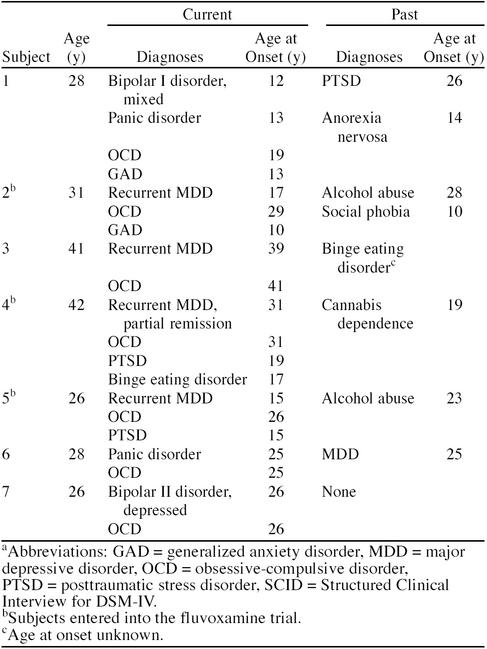
All 7 subjects with postpartum-onset OCD met DSM-IV criteria for at least 1 comorbid psychiatric disorder, with a mood disorder the most common (N = 7, 100%) (Table 2). None of the subjects had a history of psychotic symptoms. In 5 of the subjects, comorbid psychiatric disorders preceded the onset of OCD. The time course of the mood disorder and OCD in the postpartum period varied. In subjects 1, 3, 4, and 5, major depression and OCD co-occurred in the postpartum period. Subject 7 experienced hypomania the first week postpartum and then developed major depression and OCD at the same time in the second week. Subject 2 was depressed during her pregnancy and developed OCD along with persistent depression after the birth of her child. Finally, subject 6 experienced the onset of panic disorder and OCD at the same time 12 weeks postpartum after weaning the baby and developed depression 4 months later. Comorbid anxiety disorders were present in 5 subjects, 3 of whom had posttraumatic stress disorder as a result of sexual and/or physical abuse. Three other subjects (subjects 2, 3, and 6) had histories of sexual abuse but did not meet DSM-IV criteria for posttraumatic stress disorder. Three of the 6 subjects who experienced physical and/or sexual abuse were victimized by first-degree relatives. All 7 subjects had prior psychiatric treatment before the development of OCD, with 4 reporting prior treatment with antidepressant medication and 3, psychotherapy alone. After the OCD symptoms began, 3 subjects received treatment with antidepressant medication and 1 had only psychotherapy. Only 2 subjects were receiving active treatment at the time of the evaluation (1 with an antidepressant medication and 1 with psychotherapy alone).
Table 2.
Current and Past DSM-IV SCID Diagnoses in 7 Subjects With Postpartum-Onset Obsessive-Compulsive Disordera
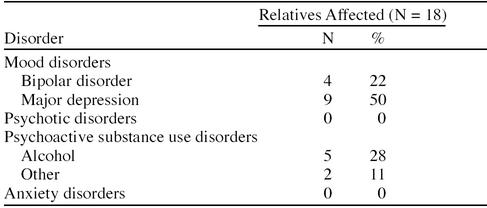
A history of psychiatric disorders was found in 18 (30%) of 60 first-degree relatives (Table 3). Mood disorders and psychoactive substance use disorders were the only disorders reported. Anxiety disorders, including OCD, were not reported in relatives by the subjects, although 2 subjects described their mothers as being anxious but could not provide enough detail to support a definitive diagnosis.
Table 3.
Psychiatric Disorders in the First-Degree Relatives of 7 Subjects With Postpartum-Onset OCD
As noted in Table 2, subjects 2, 4, and 5 entered the open trial of fluvoxamine for treatment of OCD. Subjects 2 and 4 completed the 12-week trial. Subject 5 dropped out of the study after 3 weeks of treatment due to a car accident that was unrelated to the study. The final doses of fluvoxamine for subjects 2, 4, and 5 were 300 mg/day, 200 mg/day, and 150 mg/day, respectively. Subject 2 experienced side effects that included headache, heartburn, dry mouth, and insomnia. The insomnia required treatment with zolpidem, 5 to 10 mg at bedtime as needed. Subject 4 reported side effects of headache, dry mouth, drowsiness, heart palpitations, and anorgasmia. Subject 5 reported anorgasmia.
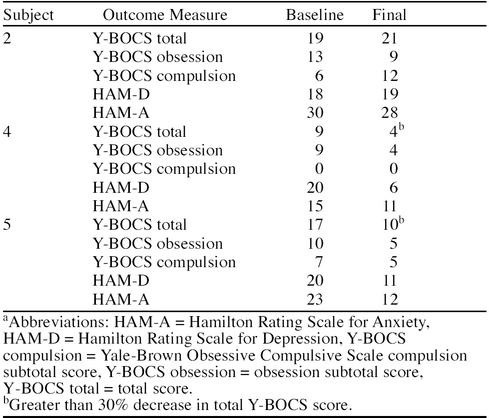
Table 4 summarizes the results of the fluvoxamine open trial in the 3 subjects. Subject 2 experienced no improvement with fluvoxamine treatment. This subject also had a past history of nonresponse to 3 trials of other serotonin reuptake inhibitors (sertraline, fluoxetine, and paroxetine) and 1 trial of a tricyclic antidepressant (desipramine). Subject 4 had a positive response to fluvoxamine treatment evidenced by a 56% decrease in the total Y-BOCS score. The HAM-D and HAM-A scores also decreased by 70% and 27% respectively. Subject 5 completed 3 weeks of treatment and also had a positive response to treatment evidenced by 41% decrease in total Y-BOCS score. The HAM-D and HAM-A scores decreased by 45% and 48%, respectively.
Table 4.
Response to Fluvoxamine Treatment in 3 Subjects With Postpartum-Onset OCDa
DISCUSSION
The characteristics of this group of 7 women with postpartum-onset OCD were similar to those in other reports of women with postpartum obsessions and compulsions in several ways. The onset of OCD was triggered by the birth of the first child more often than subsequent children.1 The predominance and number of aggressive obsessions were consistent with previous reports.1,3–6 The women experienced dysfunction in their maternal role, but none of the subjects acted on thoughts to harm the child or others.3,4 Finally, as noted in other reports,2,4 mood and other anxiety disorders were common comorbid conditions, but psychosis did not occur.
In contrast to the previous case series of patients with postpartum-onset OCD,4 the mean onset of postpartum OCD after delivery was later in the present group of women (3.7 ± 4.9 weeks vs. 2.2 ± 1.2 weeks). Furthermore, a prior history of a mood disorder occurred in 4 (57%) of the subjects, but did not occur in the previous case series.4 Depression developed simultaneously with OCD in most of the subjects in the present study, but developed after OCD in all of the subjects with depression in the previous series.4 The presence of compulsions was consistent with some1 but not all past reports.4 Finally, the mothers in the present study reported a variety of dysfunctional behavior with their children as a result of the OCD, ranging from avoidance of the child to excessive involvement with the child. This range of behavior differs from the previous case series in which all of the mothers avoided their infants.4
In spite of these differences, the similarities noted in women who present with postpartum-onset OCD suggest that this disorder may have some distinctive phenomenological features, most notably, the presence of aggressive obsessions. This type of obsession has been found in women with obessive-compulsive symptoms associated with postpartum-onset major depression (but not meeting criteria for OCD)6 and in the present study and others3,4 of women with postpartum-onset OCD. However, prospective studies comparing the symptoms of non–childbearing-related OCD with postpartum OCD are needed to confirm these potentially distinctive phenomenological features of postpartum-onset OCD. The family history findings of mood and substance use disorders in first-degree relatives of patients with postpartum OCD are similar to findings in other patients with OCD, although the non–childbearing-related OCD patients also had family members with anxiety disorders.12 The family history method used in the present study underestimates the amount of illness among first-degree relatives.9 Family interview studies are needed to confirm these findings and to determine if other diagnoses like anxiety disorders are also found in the first-degree relatives of patients with postpartum-onset OCD. Six of the subjects had a history of sexual and/or physical abuse. The relationship between abuse experiences and postpartum OCD is unclear, but may be related to the presence of mood and substance use disorders in families, as relatives with these disorders may be more likely to abuse their family members.13
The puerperium appears to be a time of increased risk for the onset or worsening of OCD, but this may be a chance association of the puerperium and OCD.4 A controlled study of the onset and prevalence of postpartum OCD is needed to determine whether the postpartum is indeed a time of risk for OCD. There has been speculation that changes in estrogen and progesterone in the puerperium may alter serotonergic function, placing some women at risk for psychiatric disorders.4,6 Oxytocin has also been implicated in the etiology of postpartum OCD because of the finding that oxytocin is elevated in the cerebrospinal fluid of some patients with OCD.14 Oxytocin is elevated in the third trimester and early puerperium and is thought to be involved in the initiation of maternal behavior in animals.15 It has also been hypothesized that the obsessions about safety and germs and compulsions such as checking and washing are pathological correlates of normal maternal behavior.16
Mood disorders were common comorbid conditions in this sample of subjects with postpartum-onset OCD. This is consistent with the past reports of twice the expected rate of postpartum depression in women with preexisting OCD2 and the high comorbidity of OCD and mood disorders.17 The co-occurrence of depression and obessive-compulsive symptoms has been associated with a poor prognosis and a lower rate of recovery.18 Four women in the present study with past postpartum-onset OCD and comorbid mood disorders continued to experience chronic OCD symptoms in spite of fluctuations in mood symptoms. Only 1 woman was taking antidepressant medication at the time of the study, suggesting that this syndrome is inadequately treated.
The findings of the open-label, preliminary trial of fluvoxamine in 3 patients suggest that fluvoxamine may be effective in reducing the symptoms of postpartum-onset OCD. Two of the 3 subjects improved with treatment. The subject who did not improve had a history of poor response to multiple previous trials of antidepressants and may not be representative of most subjects with postpartum-onset OCD. This trial was limited by its uncontrolled nature and the small number of subjects, and a larger, controlled study is needed to confirm the responsiveness of postpartum-onset OCD to fluvoxamine. Nonetheless, the results are similar to other case reports of the responsiveness of postpartum-onset OCD to serotonin reuptake inhibitors.4
In summary, obsessive-compulsive symptoms may develop in the postpartum period and may be associated with a poor prognosis. The symptoms may also adversely affect the mother-child relationship, although the long-term effects on the children are unknown. It is therefore important to assess for the presence of obsessions and compulsions when evaluating any woman who presents with anxiety and/or depression in the postpartum period. As most of the women in this sample had a prior history of psychiatric disorders before pregnancy, it is important to monitor carefully for the development of postpartum psychiatric disorders in women with psychiatric histories. Because of the preferential efficacy of serotonin reuptake inhibitors in the treatment of OCD in general19 and the preliminary results of this open trial showing efficacy of fluvoxamine in the treatment of postpartum-onset OCD, serotonin reuptake inhibitors should be considered when treating a woman with postpartum obsessive-compulsive symptoms.
Drug names: desipramine (Norpramin and others), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), sertraline (Zoloft), zolpidem (Ambien).
Footnotes
Supported by an unrestricted educational grant from Solvay Pharmaceuticals.
REFERENCES
- Buttolph ML, Holland A. Obsessive-compulsive disorders in pregnancy and childbirth. In: Jenike MA, Baer L, Minichiello WE, eds. Obsessive-Compulsive Disorders: Theory and Management. 2nd ed. Chicago, Ill: Year Book. 1990 [Google Scholar]
- Williams KE, Koran LM. Obsessive-compulsive disorder in pregnancy, the puerperium, and the premenstruum [CME] J Clin Psychiatry. 1997;58:330–334. doi: 10.4088/jcp.v58n0709. [DOI] [PubMed] [Google Scholar]
- Sichel DA, Cohen LS, Rosenbaum JF, et al. Postpartum onset of obsessive-compulsive disorder. Psychosomatics. 1993;34:277–279. doi: 10.1016/S0033-3182(93)71893-9. [DOI] [PubMed] [Google Scholar]
- Sichel DA, Cohen LS, Dimmock JA, et al. Postpartum obsessive compulsive disorder: a case series. J Clin Psychiatry. 1993;54:156–159. [PubMed] [Google Scholar]
- Lensi P, Cassano GB, Correddu G, et al. Obsessive-compulsive disorder: familial-developmental history, symptomatology, comorbidity and course with special reference to gender-related differences. Br J Psychiatry. 1996;169:101–107. doi: 10.1192/bjp.169.1.101. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Peindl KS, Gigliotti T, et al. Obsessions and compulsions in women with postpartum depression. J Clin Psychiatry. 1999;60:176–180. doi: 10.4088/jcp.v60n0305. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, and et al. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, version 2.0). New York, NY: Biometric Research, New York State Psychiatric Institute. 1995 [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, et al. The family history method using diagnostic criteria: reliability and validity. Arch Gen Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety disorders by rating. Br J Med Psychol. 1959;32:50–65. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Rasmussen SA, Eisen JL. Epidemiology and clinical features of obsessive-compulsive disorder. In: Jenike MA, Baer L, Minichiello WE, eds. Obsessive-Compulsive Disorders: Theory and Management. 2nd ed. Chicago, Ill: Year Book. 1990 [PubMed] [Google Scholar]
- Hudson JI, Pope HG. Does childhood sexual abuse cause fibromyalgia? Arthritis Rheum. 1995;38:161–163. doi: 10.1002/art.1780380203. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Goodman WK, North WG, et al. Elevated cerebrospinal fluid levels of oxytocin in obsessive-compulsive disorder: comparison with Tourette's syndrome and healthy controls. Arch Gen Psychiatry. 1994;51:782–792. doi: 10.1001/archpsyc.1994.03950100030003. [DOI] [PubMed] [Google Scholar]
- Petersen CA, Prange AJ. Induction of maternal behaviour in virgin rats after intracerebroventricular administration of oxytocin. Proc Natl Acad Sci U S A. 1979;76:6661–6665. doi: 10.1073/pnas.76.12.6661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epperson CN, McDougle CJ, Price LH. Intranasal oxytocin in obsessive-compulsive disorder. Biol Psychiatry. 1996;40:547–549. doi: 10.1016/0006-3223(96)00120-5. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Hudson JI, Phillips KA, et al. Clinical and theoretical implications of a possible link between obsessive-compulsive and impulse control disorders. Depression. 1993;1:121–132. [Google Scholar]
- Coryell W, Endicott J, Winokur G. Anxiety syndromes as epiphenomena of primary major depression: outcome and familial psychopathology. Am J Psychiatry. 1992;149:100–107. doi: 10.1176/ajp.149.1.100. [DOI] [PubMed] [Google Scholar]
- Pigott TA, Seay SM. A review of the efficacy of selective serotonin reuptake inhibitors in obsessive-compulsive disorder. J Clin Psychiatry. 1999;60:101–106. doi: 10.4088/jcp.v60n0206. [DOI] [PubMed] [Google Scholar]