Abstract
Recruitment and retention of subjects in cancer prevention, screening, and treatment trials is challenging, especially if subjects are low-income, from minority groups or immigrants with limited English fluency. This article describes our experiences in recruiting 530 female Filipino–American immigrants at community based organizations and churches for a randomized trial that assessed the effect of a small group educational session on breast and cervical cancer screening. We found that a personal invitation from either a female project liaison, a friend, or the Filipino project director were all successful strategies that resulted in over 80% attendance at an educational session that was offered as part of the study. Although non-attendees did not differ from attendees in demographic characteristics, they expressed significantly more barriers to participating in a health study. Attendance at the group session was a significant predictor of retention in the study. We were able to conduct telephone follow-up surveys among 88% of enrollees at 12 month follow-up and 76% at 24 month follow-up. Results and implications are discussed in the hope that they may facilitate future participation of Filipinos and other Asian immigrants in research.
Keywords: recruitment and retention strategies, Filipino–American immigrants, cancer screening study
INTRODUCTION
Recruitment and retention of subjects in cancer screening, prevention, and treatment trials is challenging, especially if subjects are low-income, from minority groups or immigrants with limited English fluency.1–3 We received NCI funding to conduct a large randomized trial with Filipino–American women over 40 years of age to develop and evaluate an intervention to increase breast and cervical cancer screening.4 We used this opportunity to evaluate different recruitment strategies through assessment of recruitment yields and subject feedback. We also assessed barriers to participation in this health study and predictors of retention. We report our experiences in recruiting 530 female Filipino–American immigrants for a health study, in the hope that they may facilitate future recruitment of Filipinos and other Asian immigrants.
METHODS
Overview of Research Design
A total of 530 Filipino women over 40 years of age were recruited at nine community based organizations and six churches in Los Angeles County. After completion of a short interviewer administered face-to-face baseline interview, all women were invited to attend a group session with some of their peers and a female Filipino health educator (mainly physician or nurse). Group sessions lasted 60–90 minutes, and were conducted at community based organizations, churches, or private homes in “Taglish”, which is a mix of English and Tagalog. Women within each participating site were randomized to receive a cancer screening module4 or a physical activity module.5 Because women who were recruited together also wanted to attend the same group session, 5–10 women were randomized to one study condition, and the next group of 5–10 women to the other.
Recommendations of our Filipino community partners and focus group members resulted in the following efforts to tailor the intervention delivery to the target population: A logo was developed Kulusugan ay Kayamanan (Health is Wealth), that was printed on all study materials, including tote bags that were given to women at enrollment. At the group session, women had the opportunity to socialize with each other and the health professional while refreshments and traditional Filipino snacks were served. Women received a small cash payment at the end of the session, in addition to information in English and Tagalog on breast and cervical cancer screening or physical activity.
Telephone interviews were conducted in English or Tagalog 3 and 12 months after the group session to obtain feedback on recruitment methods and barriers to participation, in addition to information on physical activity4 and breast and cervical cancer screening.5 At the end of the 12 month follow-up survey, women were asked for permission to be telephoned one more time, because additional funding had become available for a 24 month follow-up survey.
Recruitment Strategies
It is critical to develop successful recruitment strategies through which a diverse sample of women can be approached, without making these women feel uncomfortable or coercing them to participate. Although one may expect that women feel more comfortable if the initial invitation comes from a community liaison person that they may personally know, some women may feel that there is less coercion if a general announcement is made in church or in a community setting, and if they are not individually approached. On the other hand, women may feel that information about women’s health does not belong in a church setting, or they may be embarrassed about the mention of women’s health issues by a church leader and in the presence of male family members and friends. A third possibility is that those women who are exposed to the church recruitment strategy feel coerced to participate because of the fact that a church leader is perceived as an authority. We used the following recruitment strategies to recruit Filipino–American women 40 years and older into a health study:
Female Project Liaisons
Older Filipino–American women who participated in focus groups during the planning stages of the study stressed the importance of personal invitations rather than mailed invitations or posting flyers. Thus, we hired a female project liaison from each organization, who was informed about the study, and invited other members of her organization to join. The project liaisons worked closely with the study project director in scheduling women for their baseline interview and for an upcoming group session. Project liaisons also helped in locating women who had moved to a new address or changed their phone number for follow-up interviews, thus improving retention in the study.
Word of Mouth Through Friends, Relatives or Press Releases
Many women heard about our study through friends or relatives who had already or were planning to participate. A press release about the study was published in six newspapers that are widely read in the Filipino community.
Presentations by the Filipino Project Director
The female English–Tagalog bilingual Filipino–American Project Director (P.V.) gave short presentations (in Taglish) to women’s groups at churches and at community based organizations to describe the study and enroll women who were willing to participate. Usually, these presentations were scheduled in conjunction with another event such as bingo, ball room dancing, lunch or a committee meeting.
Church Announcements, Flyers, Sign-up Tables
Key informants suggested that recruitment through churches may be effective because a large number of older women go to church frequently (as opposed to the younger generation). Going to church is very much a family event among Filipino–Americans. Attending husbands or daughters may encourage women to participate in a health study, thus providing family support. A number of church leaders agreed to announce the Filipino Women’s Health Study at the end of the mass and in the church newsletter. Study staff set up tables outside the church to distribute flyers, provide information and enroll women who were willing to participate.
Retention Strategies
Three months after the group session, we attempted to recontact all women for a short telephone interview. A second telephone survey was attempted at 12 month after the group session, followed by a thank-you letter and $10 payment upon completion. All women who completed the 12 month follow-up survey were entered into a lottery for a chance to win $300. In April 2000, after about half of all women had been due for their 12 month follow-up survey, all enrollees received a personalized letter with an update on study activities, including the first lottery drawing that had taken place in one of the study sites. A year later, a second letter was sent to all participants with selected study findings and the result of the second lottery drawing. Both letters encouraged women to inform us about changes of address or telephone numbers. Women who completed the 24 month follow-up survey received another thank-you letter and $10 payment.
RESULTS
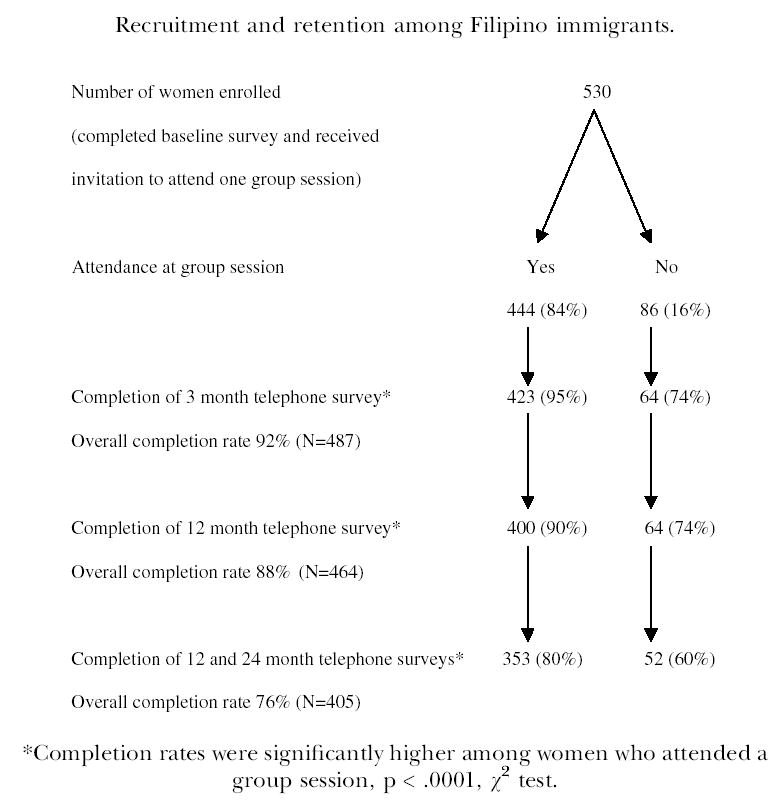
During a 2-year recruitment period (January 1998–January 2000), a total of 530 Filipino women were enrolled. Eighty-four percent of women attended a group session, 92% completed the 3 month follow-up survey, and 88% completed the 12 month follow-up survey (Figure 1). The vast majority of subjects who completed the 12 month follow-up survey (96%) agreed to be recontacted for the 24 month follow-up survey, which was completed by 76% of all women. As shown in Table 1, most women were enrolled through female project liaisons, and the fewest women through flyers, church-announcements and sign-up tables at churches. Because church announcements and sign-up tables were perceived as not very successful by our staff (many women avoided study staff waiting outside the church by exiting through another door), we abandoned this approach after a few months. Attendance at the subsequent group session was high with most recruitment strategies, except recruitment through flyers, church-announcements and sign-up tables. Women who were recruited through these methods were also least likely to complete the 12 month follow-up survey.
FIGURE 1.
Recruitment and retention among Filipino immigrants.
TABLE 1.
Recruitment Methods, Attendance at Group Session, and Completion of Follow-Up Surveys
|
Enrollment in Study |
Completion of Follow-up (%)
|
||||
|---|---|---|---|---|---|
| n | % | Attendance at Group Session (%) | 12 Mos | 24 Mos | |
| Recruitment Method | |||||
| Female project liaisons | 268 | 51 | 83 | 87 | 75 |
| Other (friends, press release) | 138 | 26 | 83 | 88 | 79 |
| Presentations by the project director | 94 | 18 | 86 | 91 | 73 |
| Flyers, church announcements, sign-up tables | 30 | 6 | 70 | 77 | 76 |
| Total | 530 | 100 | 84 | 88 | 76 |
| Attendees (n = 422)*(%) | Non-Attendees (n = 62)*(%) | p** | |||
| Recruitment Site | |||||
| Church | 27 | 36 | |||
| CBO | 73 | 64 | .148 | ||
| Randomization to | |||||
| Screening session | 46 | 66 | |||
| Exercise session | 54 | 34 | .004 | ||
| Felt “pushed” to participate to the point that they felt uncomfortable to say “no” | 3 | 7 | .166 | ||
| Knew the person who invited them | 64 | 45 | .006 | ||
n = number of subjects who completed 3 months survey in which these questions were asked.
χ2 test.
Because retention in the study was significantly higher among women who attended a group session than among women who did not attend (Figure 1), we compared these two groups (Tables 1 and 2). Attendees and non-attendees did not differ by recruitment site and neither attendees nor non-attendees felt coerced to participate in the study. Attendance was significantly better at the exercise sessions than the screening sessions. In addition, attendees were significantly more likely to personally know the person who invited them than non-attendees. Among attendees, 69% stated that knowing the person who invited them was very important for them in deciding to attend the session (15% somewhat important, 16% not important). Answers to an open-ended question “Why did you decide to participate in this study?” confirmed the importance of personal invitations, as many women stated that they joined the study because a friend or another Filipino woman they knew invited them. Most women (71–78%) had no preferences regarding recruitment location and would have participated if they had been recruited through community based organizations or churches.
TABLE 2.
Filipino Women’s Barriers to Participating in a Health Study
| Attendees (n = 422) (%) | Non-Attendees (n = 64) (%) | p* | |
|---|---|---|---|
| Had concerns about participating in the study | 11 | 26 | .001 |
| Specifically concerned about …. | |||
| Time commitment | 17 | 44 | .001 |
| This being a research study | 10 | 19 | .033 |
| Signing the informed consent form | 5 | 11 | .093 |
| Cost | 5 | 8 | .363 |
| Revealing confidential information | 8 | 6 | .804 |
| What husband or family will think about participation | 2 | 3 | .645 |
| (n = 103)** | (n = 22)** | ||
| Losing social security or other benefits | 10 | 9 | 1.00 |
| Immigration status being affected | 1 | 10 | .073 |
| Endorsement of at least one of the 8 specific barriers | 28 | 55 | .001 |
n = number of subjects who completed 3 months survey in which these questions were asked.
χ2 or Fisher’s Exact Test.
These 2 questions were discontinued after the first 125 respondents. After recording the response to these 2 questions, the interviewer clarified that social security or other benefits or immigration status will not be affected by participation in the study.
There were no significant differences between attendees and non-attendees with respect to measured demographic characteristics and baseline rates of screening and physical activity. On average, women were 63 years old, well educated, and the majority preferred to complete the baseline interview in Tagalog. All but one of the enrollees were immigrants (data not shown).
The most frequently mentioned barriers to participating in a research study were the time commitment, followed by the fact that this was a research study (Table 2). Non-attendees were about twice as likely to be concerned about these two aspects of participating in a research study as compared to attendees. Having to sign an informed consent form was another important barrier, especially among non-attendees. Two other barriers, that were of concern for this immigrant population were the possibility of losing social security or other benefits and concerns regarding one’s immigration status. A small but substantial number of women endorsed these barriers, especially among non-attendees. Overall, non-attendees were twice as likely to endorsed at least one specific barrier to participate as compared to attendees (55% vs. 28%, p < .001).
To examine factors that predicted attendance at the group session multivariately, a logistic regression analysis was performed with attendance at the outcome. Predictor variables included: age (continuous), regular physical activity reported at baseline (yes/no), comorbidities reported at baseline (at least 1 vs. none), recruitment site (church vs. CBO), group assignment (screening vs. exercise), endorsement of at least one specific barrier to participate in the study vs. none (assessed at 3 months follow-up) and subject knowing the person who invited her (assessed at 3 months follow-up).
As indicated in Table 3, after controlling for age, comorbidities and recruitment site (which were not bivariately related to attendance) in addition to group assignment and baseline physical activity, two important factors predicted attendance at a group session: Subjects who had at least one specific concern regarding participation in the study were less likely to attend the session. Subjects who personally knew the person who invited them were more likely to attend the session.
TABLE 3.
Logistic Regression Analysis Predicting the Likelihood of Attendance of the Group Session
|
95% CI |
||||
|---|---|---|---|---|
| Odds Ratio | Lower | Upper | p-value | |
| Endorsement of at least one barrier | .31 | .17 | .55 | .0001 |
| Subject knew person who invited her | 2.08 | 1.15 | 3.74 | .02 |
| Group assignment (screening vs. exercise) | .47 | .26 | .84 | .01 |
| Baseline regular physical activity (yes) | .50 | .26 | .97 | .04 |
Finally, we examined predictors of retention at 12 and 24 month follow-up in a logistic regression analysis. Predictor variables included age, group assignment, recruitment strategy (project liaison; project director; flyers, church announcements; other), preferred language of surveys (English/Tagalog), education (highschool or less/more than highschool), comorbidities (yes/no), attendance at a group session (yes/no). All variables except age were bivariately related to 12 or 24 month completion at p < .25. As shown in Table 4, attendance at the group session was a strong predictor of retention both at 12 and 24 month follow-up. Women who had at least one comorbidity were also more likely to be retained in the study. Completion of surveys in English rather than Tagalog was the strongest predictor of retention at 24 months after baseline.
TABLE 4.
Logistic Regression Analyses Predicting the Likelihood of Completion of 12 and 24 Month Follow-up Surveys
|
95% CI |
||||
|---|---|---|---|---|
| Odds Ratio | Lower | Upper | p-value | |
| 12 Month Retention | ||||
| Attendance at group session (yes) | 3.15 | 1.47 | 6.76 | .004 |
| Had at least 1 comorbidity | 2.06 | 1.02 | 4.14 | .05 |
| Preferred English over Tagalog survey | 2.14 | .82 | 5.59 | .12 |
| 24 Month Retention | ||||
| Attendance at group session (yes) | 2.29 | 1.29 | 4.07 | .005 |
| Had at least 1 comorbidity | 1.64 | 1.02 | 2.63 | .05 |
| Preferred English over Tagalog survey | 3.10 | 1.54 | 6.23 | .002 |
DISCUSSION
This study demonstrates that older Filipino–American women can successfully be recruited into a health study and retained for follow-up activities. We attribute this success to our very active and outgoing Filipino–American Project Director, and numerous project liaisons, who informed their peers about the study and invited them to join. Many studies have shown the important contributions that trained peers can make both in recruiting members of their communities and in serving as lay health educators, promoters, or community health advisors. Most of these studies have been conducted in the African–American6–11 and Hispanic community,12,13 but also among Vietnamese,14,15 Chinese,16 Cambodian and Laotians.15 Our report shows that trained peers can play a very important role in recruiting Filipino immigrants as well, without coercing them to participate.
Knowing the person who invited them was an important bivariate and multivariate predictor of attendance at the group session. Thus, face-to-face recruitment was most successful in our sample, when subjects were invited by a friend or acquaintance. While such a recruitment approach might be described as somewhat “opportunistic”, we feel that taking advantage of these preexisting social bonds aided tremendously in our recruitment and retention efforts. Similar recruitment strategies would probably be used if educational sessions such as the one we tested in a research setting were offered as a service to Filipino immigrants at community based organizations.
We limited the role of our community liaisons to recruitment, because our prior research had shown that the majority of Filipino women preferred to learn health information from a female Filipino health professional rather than a trained peer.17 However, studies with other Asian populations have taken a different approach by involving trained peers in health education interventions as well.14,15
We were not able to directly assess which strategy resulted in highest subject recruitment, because we abandoned the least successful approach (recruitment through church announcements and sign-up tables) after a few months. The other three recruitment strategies were maintained throughout the two year recruitment period. However, the fact that women recruited though church sign-up tables were least likely to attend the group session suggests that this method was least effective. Despite this set back, it should be noted that we were able to recruit one quarter of all women at churches, mostly though presentations of the Project Director to existing church groups (such as the choir), and through project liaisons. As one might expect, retention in the study was higher among attendees than among non-attendees of the group session (Figure 1). In fact, attendance emerged as one of the most important predictors of retention both at 12 and 24 month follow-up. This suggests the importance of establishing initial rapport through face-to-face contact for achieving good retention. We also demonstrated that repeated telephone interviews over a 2-year period can be completed in an immigrant population such as ours. We have not found any other studies among Asian immigrants that reported such a long follow-up period, although long time follow-up is desirable in many health studies to determine if newly adopted health behaviors are being maintained.
Because attendance at the group session was an important predictor of retention, we compared barriers to participating in our health study between attendees and non-attendees. The most salient barriers, concern about time commitment and about this being a research study, are similar to those found in other ethnic/racial groups.1,2 Concern about having to sign an informed consent form maybe more typical to immigrant populations which limited English proficiency. Although this barrier was only endorsed by a small number of subjects, this finding supports efforts of our and other research groups to substitute Informed Consent Forms that require the subjects’ signature with Information Sheets that provide the same information but do not have to be signed. A small but substantial proportion of our sample feared losing social security or other benefits and worried about immigration status being affected. These barriers, which might also be present in other immigrant populations, should be addressed during recruitment, since endorsement of at least one barrier was the strongest predictor of attendance at the group session, which in turn predicted retention in the study.
This study was extensively tailored to be attractive to Filipino women. Women were randomized in small groups to their respective intervention/control activity, so friends could attend together. We have previously shown that this group randomization resulted in similar intervention/control groups at baseline.4 All women, including those randomized to the control condition, received something that they valued. This study design not only helps to avoid bias through increased attention in the intervention group (Hawthorne effect), but probably increases participation as well. Finally, women were only required to attend one group session at a convenient time and location. This session was structured to provide education and to encourage healthier behavior in a social and entertaining atmosphere. Experience suggests that research studies that require subjects to attend multiple events6 or that involve medical procedures, invasive testing or major life style changes will probably be less successful in recruiting and retaining subjects, especially among immigrant populations.
Despite our efforts to provide a study experience that is culturally appropriate, retention 24 months after baseline was more successful among women who completed surveys in English rather than Tagalog. This introduces selection bias into results obtained at follow-up since the less acculturated women are less likely to be represented. The fact that women who had at least one comorbidity were more likely to be retained in the study may be due to the fact that these women are more interested in health issues. As with other selection biases, statistical methods can control for baseline differences during the analysis.
In summary, future recruitment efforts among immigrant populations should address specific barriers to participation in a study. Our results suggest that retention for 2 years after enrollment and telephone surveys are feasible in this population, especially if subjects experienced face to face contact with study personnel.
Acknowledgments
Supported by National Cancer Institute Grant R01 CA74576 to the first author.
References
- 1.Giuliano AR, Mokuau N, Hughes C, et al. Participation of minorities in cancer research: The influence of structural, cultural, and linguistic factors. Ann Epidemiol. 2000;10:S22–S34. doi: 10.1016/s1047-2797(00)00195-2. [DOI] [PubMed] [Google Scholar]
- 2.Brown DR, Fouad MN, Basen-Engquist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol. 2000;10:S13–S21. doi: 10.1016/s1047-2797(00)00197-6. [DOI] [PubMed] [Google Scholar]
- 3.Alexander GA, Chu KC, Ho RCS. Representation of Asian Americans in clinical cancer trials. Ann Epidemiol. 2000;10:S61–S67. doi: 10.1016/s1047-2797(00)00198-8. [DOI] [PubMed] [Google Scholar]
- 4.Maxwell AE, Bastani R, Vida P, Warda US. Results of a randomized trial to increase breast and cervical cancer screening among low-income Filipino–American women. Prev Med. 2003;37:102–109. doi: 10.1016/s0091-7435(03)00088-4. [DOI] [PubMed] [Google Scholar]
- 5.Maxwell AE, Bastani R, Vida P, Warda US. Physical activity among older Filipino–American women. Women Health. 2002;36(1):67–79. doi: 10.1300/J013v36n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blumenthal DS, Sung J, Coates R, Williams J, Liff J. Recruitment and retention of subjects for a longitudinal cancer prevention study in an inner-city black community. Health Serv Res. 1995;30:197–205. [PMC free article] [PubMed] [Google Scholar]
- 7.Erwin DO, Spatz TS, Turturro CL. Development of an African–American role model intervention to increase breast self-examination and mammography. J Cancer Educ. 1992;7:311–319. doi: 10.1080/08858199209528188. [DOI] [PubMed] [Google Scholar]
- 8.Lacey L, Tukes S, Manfredi C, Warnecke RB. Use of lay health educators for smoking cessation in a hard-to-reach urban community. J Commun Health. 1991;16:269–282. doi: 10.1007/BF01320335. [DOI] [PubMed] [Google Scholar]
- 9.Earp AL, Altpeter M, Mayne L, Viadro CI, O’Malley MS. The North Carolina Breast Cancer Screening Program: Foundations and design of a model for reaching older, minority, rural women. Breast Cancer Res Treat. 1995;35:7–22. doi: 10.1007/BF00694740. [DOI] [PubMed] [Google Scholar]
- 10.Sung JFC, Coates RJ, Williams JE, et al. Cancer screening intervention among Black women in inner-city Atlanta – Design of a study. Public Health Rep. 1992;107:381–388. [PMC free article] [PubMed] [Google Scholar]
- 11.Eng E, Smith J. Natural helping functions of lay health advisors in breast cancer education. Breast Cancer Res Treat. 1995;35:23–29. doi: 10.1007/BF00694741. [DOI] [PubMed] [Google Scholar]
- 12.Navarro AM, Senn KL, Kaplan RM, McNicholas L, Campo MC, Roppe B. Por La Vida intervention model for cancer prevention in Latinas. J Natl Cancer Inst Monogr. 1995;18:137–145. [PubMed] [Google Scholar]
- 13.Brownstein JN, Cheal N, Ackermann SP, Bassford TL, Campos-Outcalt D. Breast and cervical cancer screening in minority populations: A model for using lay health educators. J Cancer Educ. 1992;7:321–326. doi: 10.1080/08858199209528189. [DOI] [PubMed] [Google Scholar]
- 14.Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CNH. Opening pathways to cancer screening for Vietnamese–American women: Lay health workers hold a key. Prev Med. 1998;27:821–829. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- 15.Chen MS, Anderson J, Moeschberger M, Guthrie R, Kuun P, Zaharlick A. An evaluation of heart health education for Southeast Asians. Am J Prev Med. 1994;1994:205–208. [PubMed] [Google Scholar]
- 16.Jackson JC, Do H, Chitnarong K, et al. Development of cervical cancer control interventions for Chinese immigrants. J Immigr Health. 2002;4:147–157. doi: 10.1023/A:1015650901458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maxwell AE, Bastani R, Warda US. Breast cancer screening and related attitudes among Filipino–American women. Cancer Epidemiol Biomarkers Prev. 1997;6:719–726. [PubMed] [Google Scholar]


