Abstract
Background: Weight gain is a significant side effect associated with typical and atypical antipsychotic agents. It has the potential to add to the increased morbidity and mortality associated with schizophrenia and schizoaffective disorder. Because the newer antipsychotic medications have proved to be superior to traditional agents in controlling the positive and negative symptoms of schizophrenia, it is additionally critical to address the relationship of these newer agents to weight gain.
Method: Prior to the availability of novel antipsychotic medication, we looked at a group of 17 residents, of whom 71% had significant weight gain on treatment with traditional antipsychotic medications between 1991 and 1994. This prompted our interest in weight gain, especially after the introduction of novel antipsychotic medications, and our decision to look closely at their diets and help them make changes that would minimize their weight gain. We monitored the effect of a comprehensive primary intervention strategy on controlling obesity in a retrospective study of 32 patients with DSM-IV schizophrenia or schizoaffective disorders. All patients were residents in an adult care facility for formerly homeless persons with serious mental illness. Intervention consisted of complete medical and psychiatric care; switch to a patient-optimal atypical drug; low-calorie, monitored diet; nutritional education; and supportive care.
Results: There was no significant change in mean body weight at 12 and 18 months after initiation of intervention. Weight gain was observed in only 30% of study patients after the intervention as opposed to 71% at the start of the study. In general, as the negative symptoms of schizophrenia improved, patients were found to become more receptive to education and to become proactive in their health care. The lack of weight gain was consistently seen with all 3 agents tested—clozapine, olanzapine, and risperidone.
Conclusion: A patient's diet appears to be a better predictor of weight gain than the choice of novel antipsychotic medication. Clinicians might prescribe nutritional and lifestyle changes alongside medication with weight gain potential.
Antipsychotic agents form an important armamentarium in the management of patients with schizophrenia. With the development of the atypical class of agents, superior efficacy has been established for both positive and negative symptoms of schizophrenia concurrent with the minimization of side effects generally associated with the older agents. As a rule, atypical agents have been shown to produce fewer extrapyramidal symptoms and less sexual dysfunction and have lower risk for tardive dyskinesia than traditional antipsychotics.1 However, the problem of treatment-associated weight gain appears to persist with these newer agents.
The induction of obesity by antipsychotic agents has been documented since the introduction of chlorpromazine in the mid-1950s and extended to other so-called “low-potency” agents such as thioridazine and mesoridazine. Later, “high-potency” agents such as piperazine phenothiazines and haloperidol were added to this list.2 Atypical antipsychotic agents may have an even greater potential for inducing obesity than traditional antipsychotics. Clozapine has been shown in a randomized double-blind study to cause greater weight gain than haloperidol.3 Variable weight gain has also been associated with olanzapine and risperidone.4 The causes for such weight gain may be multifactorial, and the demonstration of a direct association with drug efficacy has been controversial. For example, in an open-label study of 21 patients with schizophrenia, clozapine treatment efficacy as measured by improvement in total score on the Brief Psychiatric Rating Scale (BPRS) was correlated significantly (p = .01) with weight gain over a 16-week period.5 On the contrary, another study failed to show any significant correlation between these 2 parameters after 12 weeks of clozapine treatment.6 Completing the spectrum, a third study—a chart review—of 36 patients with schizophrenia found a “nearly” significant but not truly statistically significant correlation between weight gain and decrease in BPRS score.7 Further, the relative obesity-inducing potential of different atypical antipsychotics has not been definitively established, although some comparative data are available. In a group of patients with bipolar disorder, olanzapine was shown to cause a 6-fold greater increase in body weight than risperidone over a 12-week treatment period.8
With a view to shedding more light on some of these questions, we developed a multifaceted primary intervention program that addressed health and nutrition issues in the controlled environment of a supportive residence for formerly homeless persons living with serious and persistent mental illness.
METHOD
Background
Prior to the availability of novel antipsychotic medication, we looked at a group of 17 residents, of whom 71% had significant weight gain on treatment with traditional antipsychotic medications between 1991 and 1994. This prompted our interest in weight gain, especially after the introduction of novel antipsychotic medications, and our decision to look closely at their diets and help them make changes that would minimize their weight gain.
Setting
The retrospective study was conducted in a 57-bed residential care center for adults (Project Renewal, Manhattan, N.Y.). Residents of the center were previously homeless adults with severe, persistent mental illness. Comprehensive care was provided to these individuals by a team of mental health workers, social workers, nurses, a part-time psychiatrist, and ancillary staff.
Subjects
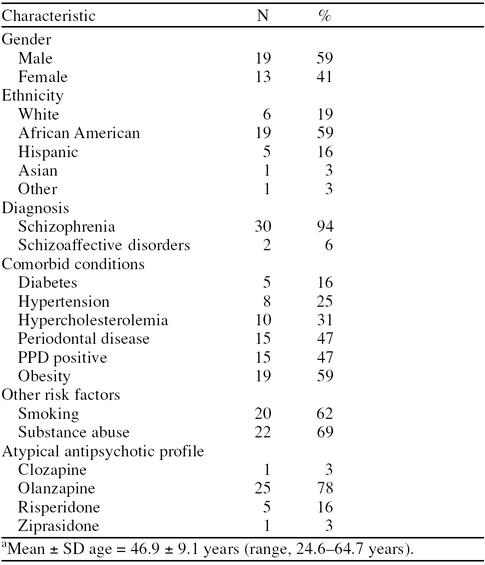
Thirty-two adult residents (mean age = 46.9 years) who had been on treatment with atypical antipsychotics for at least 1 year were selected for the study. No attempt was made to standardize the medication used. Comorbid conditions included diabetes (N = 5; 16%), hypertension (N = 8; 25%), hypercholesterolemia (N = 10; 31%), periodontal disease (N = 15; 47%), PPD positivity (N = 15; 47%), and obesity (N = 19; 59%) (Table 1). Additional risk factors included smoking (N = 20; 62%) and substance abuse (N = 22; 69%).
Table 1.
Patient Characteristics of 32 Patientsa
Study Design
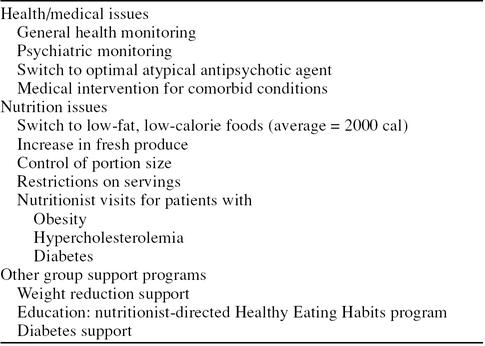
A comprehensive intervention strategy (Table 2) was designed to address issues of overall health (general medical and psychiatric), nutrition (weight gain and unhealthy eating habits), and other supportive care (weight reduction support, diabetes support, and nutritional education explaining healthy eating habits and the consequences of nutrition habits on physical health). Body weight was monitored before the intervention and at 12 and 18 months thereafter.
Table 2.
Features of Comprehensive Intervention Strategy in Study Subjects
Health/medical issues.
All patients were provided general medical care and psychiatric care. The efficacy of atypical antipsychotic agents was monitored, and agents were switched if necessary. Appropriate medical intervention was provided for comorbid conditions such as diabetes, hypertension, and hypercholesterolemia.
Nutritional issues.
Patients were provided a low-fat, low-calorie diet (average = 2000 calories) with increased fresh produce. Typically, a lunch menu consisted of chicken, turkey, or tuna salad. More soups were offered along with one serving of bread. Rich desserts were replaced with servings of fresh fruit. Crystal Lite or water was served with each meal, replacing sugar- or caffeine-laden drinks. Portion size was decreased for all foods, except vegetables and lettuce and/or salad. Servings were limited to one per person. Nighttime snacks were eliminated, except for patients with diabetes. Support groups were formed for weight reduction and diabetes. A “Healthy Eating Habits” group was initiated by the nutritionist to educate patients regarding proper eating habits and consequences of nutrition on physical health.
Statistical Analysis
Assuming that the change to a new novel agent combined with the dietary and medical intervention would result in either weight stabilization (mean change = 0) or weight loss (mean change < 0), a 1-tailed t test was performed at the end of 1 year. At the time of second analysis (18 months), 3 subjects were unavailable for remeasurement. Therefore, the null hypothesis was based on a possibility of no weight change (either gain or loss), and a 2-tailed t test was performed.
RESULTS
Patients
Of the 32 patients enrolled, 1 patient was dropped from the analysis because we believed that weight gain in that patient may have been confounded by the cessation of smoking, an independent risk factor for developing obesity. Three other patients became unavailable for weight measurements after 1 year. Therefore, data from a total of 31 and 28 patients were evaluated at 12 and 18 months after intervention, respectively.
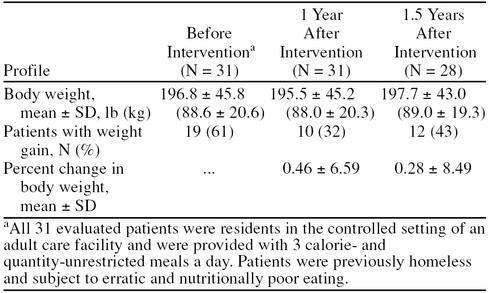
Body Weight
The mean ± SD body weight of the 31 patients at the start of the intervention study was 196.8 ± 45.8 lb (88.6 ± 20.6 kg). One year after healthy eating habits and more nutritious and low-calorie diets were initiated, the mean weight for the group was 195.5 ± 45.2 lb (88.0 ± 20.3 kg). After 1½ years, the mean body weight remained at 197.7 ± 43.0 lb (89.0 ± 19.3 kg). None of these values was found to be statistically significantly different after the intervention (Table 3).
Table 3.
Body Weight Profile of Patients Before and After Intervention Strategy
At the start of the study, 19 (61%) of 31 patients showed weight gain (see Table 3). In contrast, 1 year after intervention, only 10 (32%) of 31 patients had gained weight, and there was no statistically significant difference in mean body weight on the new management regimen. After 18 months, 12 (43%) of 28 patients had increasing body weight, again with no difference in mean body weight over time (see Table 3). The percent change in body weight was not statistically significant at either timepoint after study intervention (1- and 2-tailed t tests at 1 and 1½ years, respectively, 99.5% confidence interval).
The lack of effect on body weight was found to be independent of the atypical antipsychotic agent administered. Effects were similar whether the patient was prescribed clozapine, olanzapine, or risperidone.
General
As we have noted above, on entry into the residence, many of these previously homeless individuals have been found to gain weight. This has been attributed to a stable supportive environment and is believed to be the consequence of receiving regularly scheduled meals (3 per day) in the residence dining room. Indeed, a chart review has indicated that many of these patients may continue to gain weight for a period of up to 3 years even when they are not receiving weight-enhancing agents such as the atypical antipsychotic medications. In this study group, patients who were apathetic, with little or no motivation to attend programs or work outside the residence, appeared to gain the most weight. As general psychiatric conditions improved with treatment, patients were seen to become more interested in personal care and more receptive to educational measures. Since all medications were provided under supervised conditions, compliance was 100%.
DISCUSSION
The health burdens of obesity, in terms of both morbidity and economics, are many. Superimposed over the medical complications of schizophrenia, the overall effects of obesity can be tremendous. Diabetes, hypertension, hyperlipidemia, and sleep apnea are a few examples of complications that are exaggerated by obesity in people with schizophrenia.9 In addition, the overall mortality rate in this population has been reported to be almost double that of the general population.10 Weight gain associated with antipsychotics may also be detrimental to treatment compliance and needs to be addressed with individual patients.11 Given the potential for such adverse effects of weight gain and the superior efficacy of atypical antipsychotics in the treatment of patients with schizophrenia and schizoaffective disorders, the control of obesity in this group of patients is clinically important.
Our study shows that body weight in patients receiving atypical antipsychotic medications can be controlled with proper diet and education. A lack of weight gain was observed in less motivated patients. In fact, we attribute the efficacy of the medication in treating the negative symptoms of schizophrenia as being the causative factor for patient motivation.
The evidence from our patients, who were managed in a controlled setting, provides the first proof that a patient's diet may be a better predictor of weight gain than the physician's selection of a specific agent. In view of these data, recent reports that some atypical antipsychotics may be better than others at minimizing weight gain must be revisited.8,12 Our study did not indicate any differences in body weight responses between clozapine, olanzapine, and risperidone. None of these agents was found to cause significant increases in body weight when administered in a setting of low-calorie, nutritious diets and rigorous educational efforts. Our patients belied the oft-held opinion that persons living with schizophrenia are difficult candidates for education. On the contrary, as patients' symptoms improved with the atypical medication, they seemed more interested in personal care and life improvement. They began to discuss their daily diets and started thinking and talking about their food choices. The group educators were then able to suggest substitutions for sugar-filled foods, high-calorie foods, and high-fat foods. In time, as patients noticed the direct effects of their diet on blood pressure, blood sugar levels, and body weight, they were found to make more concerted efforts to change their daily habits. Thus, patients with schizophrenia and related disorders appear to be no different from the general population in trying to lose weight.
Thus, weight gain in patients with schizophrenia treated with atypical antipsychotic agents may be multifactorial and independent of the medication prescribed. The data presented here are encouraging, and it is hoped that the positive results will motivate further study in this area.
The applicability of these results to treatment with other psychotropic medications commonly associated with weight gain remains for future investigations to determine. Still, the issues raised here may be relevant in weight gain resulting from other medications. Since most prescribing of psychotropic medication takes place in outpatient psychiatric and primary care settings, investigations aimed at similar interventions in ambulatory populations seem appropriate. In advance of such study, interested clinicians might well choose to prescribe nutritional and lifestyle changes along with psychotropic medications that have the potential to cause weight gain.
Drug names: chlorpromazine (Thorazine and others), clozapine (Clozaril and others), haloperidol (Haldol and others), mesoridazine (Serentil), olanzapine (Zyprexa), risperidone (Risperdal), thioridazine (Mellaril and others).
REFERENCES
- Weiden PJ, Aquila R, Dalheim L, et al. The routine use of atypical antipsychotic agents, 1: common treatment goals: switching of antipsychotics. J Clin Psychiatry Audiograph. 1997;1(1) [Google Scholar]
- Bernstein JG. Induction of obesity by psychotropic drugs. Ann N Y Acad Sci. 1987;499:203–215. doi: 10.1111/j.1749-6632.1987.tb36212.x. [DOI] [PubMed] [Google Scholar]
- Bustillo JR, Buchanan RW, Irish D, et al. Differential effect of clozapine on weight: a controlled study. Am J Psychiatry. 1996;153:817–819. doi: 10.1176/ajp.153.6.817. [DOI] [PubMed] [Google Scholar]
- Emanuel M, Dalheim L, and Aquila R. Weight gain and atypical antipsychotics. Presented at the 38th annual meeting of the New Clinical Drug Unit; June 10–11, 1998; Boca Raton, Fla. [Google Scholar]
- Leadbetter R, Shutty M, Pavalonis D, et al. Clozapine-induced weight gain: prevalence and clinical relevance. Am J Psychiatry. 1992;149:68–72. doi: 10.1176/ajp.149.1.68. [DOI] [PubMed] [Google Scholar]
- Umbricht DSG, Pollack S, Kane JM. Clozapine and weight gain. J Clin Psychiatry. 1994;55(9, suppl B):157–160. [PubMed] [Google Scholar]
- Lamberti JS, Belnier T, Schwarzkopf SB. Weight gain among schizophrenic patients treated with clozapine. Am J Psychiatry. 1992;149:689–690. doi: 10.1176/ajp.149.5.689. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Gusille C, Demomilos C, and et al. Atypical antipsychotic use in a bipolar disorder clinic. Presented at the 21st Congress of the College of International Neuropsychopharmacology; July 11, 1998; Glasgow, Scotland. [Google Scholar]
- Breakey WR, Fischer PJ, Kramer M, et al. Health and mental problems of homeless men and women in Baltimore. JAMA. 1989;262:1352–1357. [PubMed] [Google Scholar]
- Brown S. Excess mortality of schizophrenia: a meta-analysis. Br J Psychiatry. 1997;171:502–508. doi: 10.1192/bjp.171.6.502. [DOI] [PubMed] [Google Scholar]
- Fleischhacker WW, Meise U, Gunther V, et al. Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatr Scand Suppl. 1994;382:11–15. [PubMed] [Google Scholar]
- Masand PS. ed. JCP Visuals. January1999 1–8. [Google Scholar]