Abstract
Background: This study examines whether women who become depressed at one reproductive cycle event, e.g., postpartum, are likely to become depressed at other such events.
Method: Seventy-two women in treatment for major depression were asked to complete a questionnaire assessing mood at 4 different reproductive cycle events, i.e., while premenstrual, taking oral contraceptives, postpartum, or perimenopausal. All diagnoses were made using DSM-III-R criteria. Rank-order correlations (r) were determined between mood ratings for different reproductive cycle event pairs.
Results: Significant correlations were found between premenstrual and perimenopausal mood ratings (r = 0.41) and between postpartum and perimenopausal mood ratings (r = 0.64). Development of severe depression during the latter 2 events was strongly correlated (r = 0.87). Women who developed severe depression during at least 2 reproductive cycle events were more likely to have bipolar disorder, a family psychiatric history, and a younger age at onset.
Conclusion: These findings suggest that there may be a unique subgroup of women who are vulnerable to depression at reproductive cycle events.
There has been increased interest in mood disorders among women. It is apparent that rates of depression are higher among women than men, even across different cultures and nations.1,2 Although theories abound to explain this discrepancy, the reasons remain unclear.
One possible explanation is the relationship of mood disorders to the reproductive cycle. There is a general consensus on the phenomenology and epidemiology of premenstrual dysphoric disorder, postnatal blues, and postpartum depression. For example, we know that 7% to 14% of women will develop postpartum depression and that a well-established risk factor is bipolar illness.3 Oral contraceptive dysphoria, however, has been little studied, and perimenopausal depression remains controversial.4
Although most reproductive cycle events have been well studied, surprisingly little attention has been given to associations among them. For example, are women who develop depression at one such event also likely to develop depression at others? If so, do these women share common and unique characteristics? The present study attempts to explore these issues in a group of women being treated for depression in an outpatient setting.
METHOD
The study population consists of 72 consecutive women treated for a major depressive episode by 2 of the authors (R.J.G. and P.S.M.) in their private outpatient psychiatric practices. Some of the women had recently entered treatment for depression, and others were already in partial or full remission. After complete description of the study to the subjects, verbal consent was obtained. The State University of New York Institutional Review Board regarded this study as exempt from full board review.
All patients who were asked to participate in the study agreed to do so. Diagnoses were assigned clinically according to DSM-III-R criteria. At a baseline visit, data were recorded regarding patient demographics and family and past psychiatric history. During the same visit, subjects completed a questionnaire eliciting nonparametric responses regarding mood for each of 4 reproductive cycle events (i.e., during premenstruation, oral contraceptive use, postpartum, and perimenopause).
Twenty patients who were still in treatment after 6 months were readministered the questionnaire, focusing on the time period prior to the index evaluation. A weighted kappa coefficient was used to assess the 6-month test-retest reliability for each question. Agreement was fair to good, with kappa values ranging from 0.47 to 0.60.
To assess how much patient mood may have influenced retrospective reporting on the questionnaire, the authors (R.J.G. and P.S.M.) also completed the questionnaire for 20 randomly selected patients. The authors' ratings were based on history elicited from the patients and were made blind to the patients' ratings. Kappa values ranged from 0.64 to 1.00 for each question, indicating good-to-excellent agreement between physician- and patient-rated mood changes at each reproductive cycle event.
Correlations between mood ratings for different reproductive cycle events were calculated using the Spearman rho rank-order correlation coefficient (r). Women complaining of severe depression at 2 or more reproductive cycle events were compared with the remainder of the sample on several variables. Independent t tests were employed for statistical comparisons of parametric variables between groups. Pearson chi-square tests were employed for comparisons between nonparametric variables.
RESULTS
The study population had a mean ± SD age of 43 ± 12 years (range, 19–75 years). Eight (11%) of the 72 subjects carried a diagnosis of bipolar disorder. Comorbid anxiety disorders were common (N = 23; 32%), but substance use disorders (N = 9; 12%) and personality disorders (N = 7; 10%) were infrequent. Thirty-five subjects (49%) were suffering from an acute episode of major depression, and the rest were in partial or full remission as determined by clinicians' observations.
Because of the wide variability in age and experience in our sample, not all women were able to comment on every reproductive cycle event. For example, although all women could comment on mood prior to menstruation, only 50 of the women had taken oral contraceptives, 58 women had had children, and 24 had been through or were going through menopause. Within these subgroups, 50% (36/72) rated themselves as having severe premenstrual depression, 14% (7/50) as having severe depression following oral contraceptive use, 33% (19/58) as having severe postpartum depression, and 17% (4/24) as having severe depression around menopause.
Table 1 demonstrates moderate direct correlations between premenstrual and perimenopausal mood ratings and between oral contraceptive and perimenopausal mood ratings, although the latter did not reach statistical significance. A moderate-to-strong correlation was found between postpartum and perimenopausal mood ratings.
Table 1.
Correlations Between Retrospective Mood Ratings at 4 Reproductive Cycle Events
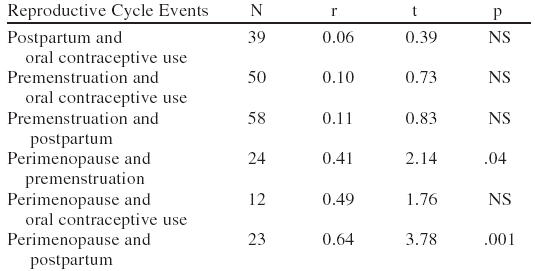
There was a strong direct correlation (r = 0.87) for ratings of severe depression in the postpartum and perimenopausal periods (t = 8.1, df = 22, p = .000). No other reproductive cycle event pair ratings reached statistical significance.
To see if the presence of acute depression caused a retrospective reporting bias, we investigated whether these women were more likely to report severe depression at past reproductive cycle events than women in partial or full remission from depression. We found no significant between-group differences in reporting of reproductive cycle event–related depression.
To determine whether women who reported severe depression at 2 or more reproductive cycle events formed a unique subgroup, these subjects (N = 14) were compared with the remaining subjects (N = 58) on 6 variables. The former subgroup reported an earlier age at onset (t = 4.3, df = 61, p = .04), earlier age at first treatment (t = 5.2, df = 61, p = .03), diagnosis of bipolar disorder (χ2 = 5.6, df = 1, p = .02), and a family psychiatric history (χ2 = 4.2, df = 1, p = .04). They were not more likely to report a family history of bipolar illness (χ2 = 0.28, df = 1, NS), however, or a past history of psychiatric hospitalizations (χ2 = 0.56, df = 1, NS).
DISCUSSION
Among the 72 subjects, relatively few reported perimenopausal depression or oral contraceptive dysphoria compared with premenstrual dysphoria and postpartum depression. This finding is consistent with epidemiologic and longitudinal studies reporting no general increase in depression rates during perimenopause.5,6
We also found, however, a correlation between perimenopausal mood ratings and ratings at other reproductive cycle events, especially between perimenopausal depression and postpartum depression. This suggests that there may be a subgroup of women who have a specific vulnerability to developing reproductive cycle event–related depression.
In support of this hypothesis are previous studies demonstrating correlations between perimenopausal depression and depression at other reproductive cycle events,7 premenstrual dysphoria and postnatal blues,8,9 premenstrual dysphoria and postpartum depression,10,11 and oral contraceptive dysphoria and premenstrual dysphoria.12
The present study provides further support for this hypothesis by demonstrating that women who report reproductive cycle event–related depression have an earlier age at onset and first treatment, are more likely to carry a diagnosis of bipolar disorder, and report a stronger family history of mental illness than other depressed women. These findings suggest unique characteristics and perhaps a more biologically driven illness for this subgroup of depressed women.
One limitation in a study of this sort is potential for retrospective overreporting of reproductive cycle event–related depression, especially premenstrual dysphoria.13 This may not have been a major factor in the present study, however, given the good 6-month test-retest reliability of reproductive cycle event mood ratings and correlation with independent physician evaluation. Other limitations include lack of structured diagnostic interviews and standardized measures of depression severity and retrospective reporting of family psychiatric history.
Further research is needed to prospectively evaluate correlations between reproductive cycle events and to explore more fully the characteristics of the subgroup of women with affective vulnerability to these events. If subsequent research supports our findings, then a clinical implication is that women with reproductive cycle event–related depression should be warned and monitored for the emergence of perimenopausal depression.
Footnotes
Presented in a poster session at the annual meeting of the Academy of Psychosomatic Medicine, Nov. 15, 1996, San Antonio, Tex.
REFERENCES
- Kessler RC, McGonagle KA, Swartz M, et al. Sex and depression in the National Comorbidity Survey, I: lifetime prevalence, chronicity, and recurrence. J Affect Disord. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–299. [PubMed] [Google Scholar]
- Pop VJM, Essed GGM, DeGeus CA, et al. Prevalence of post partum depression. Acta Obstet Gynecol Scand. 1993;72:354–358. doi: 10.3109/00016349309021112. [DOI] [PubMed] [Google Scholar]
- Schmidt PJ, Rubinow DR. Menopause-related affective disorders: a justification for further study. Am J Psychiatry. 1991;148:844–852. doi: 10.1176/ajp.148.7.844. [DOI] [PubMed] [Google Scholar]
- Busch CM, Zonderman AB, Costa P. Menopausal transition and psychological distress in a nationally representative sample. J Aging Health. 1994;6:209–228. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Stewart DE, Boydell KM. Psychologic distress during menopause: associations across the reproductive life cycle. Int J Psychiatry Med. 1993;23:157–162. doi: 10.2190/026V-69M0-C0FF-7V7Y. [DOI] [PubMed] [Google Scholar]
- Kennerley H, Gath D. Maternity blues, III: associations with obstetric, psychological, and psychiatric factors. Br J Psychiatry. 1989;155:367–373. [PubMed] [Google Scholar]
- O'Hara MW, Schlechte JA, Lewis DA, et al. Prospective study of postpartum blues: biological and psychosocial factors. Arch Gen Psychiatry. 1991;48:801–806. doi: 10.1001/archpsyc.1991.01810330025004. [DOI] [PubMed] [Google Scholar]
- Dalton K. Prospective study into puerperal depression. Br J Psychiatry. 1971;118:689–692. doi: 10.1192/bjp.118.547.689. [DOI] [PubMed] [Google Scholar]
- Pearlstein TB, Frank E, Rivera-Tovar A, et al. Prevalence of axis I and axis II disorders in women with late luteal phase dysphoric disorder. J Affect Disord. 1990;20:129–134. doi: 10.1016/0165-0327(90)90126-s. [DOI] [PubMed] [Google Scholar]
- Dennerstein L, Morse CA, Varnavides K. Premenstrual tension and depression: is there a relationship? J Psychosom Obstet Gynaecol. 1988;8:45–52. [Google Scholar]
- Rubinow DR, Roy-Byrne P, Hoban C, et al. Prospective assessment of menstrually related mood disorders. Am J Psychiatry. 1984;141:684–686. doi: 10.1176/ajp.141.5.684. [DOI] [PubMed] [Google Scholar]


