Abstract
Methylphenidate is a central nervous system stimulant drug that has become the primary drug of choice in treating attention-deficit/hyperactivity disorder in children. Side effects are usually mild and are generally well tolerated by patients. Along with increases in prescribing frequency, the potential for abuse has increased. Intranasal abuse produces effects rapidly that are similar to the effects of cocaine in both onset and type. The clinical picture of stimulant abuse produces a wide array of psychiatric symptoms. There is little in the literature to differentiate methylphenidate from other stimulants when they are abused. The need for education of all involved with the use of methylphenidate is discussed to help prevent an increasing pattern of methylphenidate abuse.
Methylphenidate is a central nervous system (CNS) stimulant drug that has become the primary drug of choice in treating attention-deficit/hyperactivity disorder (ADHD) in children. It has also been used to treat other disorders such as depression, narcolepsy, brain injury, cancer, pain, and cognitive disorders and to treat patients with human immunodeficiency virus infection.1 However, its most impressive effect has been the reduction of symptoms seen in ADHD, a condition found in approximately 3% to 5% of the general population of school-age children,2 occurring more frequently in boys.3 Many children, adolescents, and adults with ADHD can benefit from the therapeutic effects of methylphenidate with minimum side effects.4–8 The most common side effects are insomnia, stomachache, headache, and anorexia.8–10 When these side effects do occur in treatment, they usually can be managed effectively or diminish in severity with time to a tolerable level.6,9,10 This stimulant medication is generally safe when used as prescribed; it produces few serious adverse events when used orally in therapeutic doses. However, the entire therapeutic profile starts to change when it is abused.
As ADHD is more accurately diagnosed and treated appropriately with stimulant medication, there will be a continued increase in the amount of methylphenidate prescribed and dispensed.11,12 Given this increasing number of patients receiving methylphenidate and the increased availability of methylphenidate, there is an increased potential for this medication to be abused. Abuse often entails the use of large doses, which may be taken intranasally or intravenously. This article will review the pharmacology of methylphenidate and look at its psychiatric side effects when abused. Patterns of abuse, including intranasal use, will also be discussed to help the primary care practitioner become more aware of some of the potential problems when monitoring and supervising the use of methylphenidate.
HISTORY
Methylphenidate, synthesized in 194413 and patented in 1954, was first marketed by Ciba-Geigy Pharmaceutical Company as Ritalin. It was initially first used in 1955 for a number of indications. The 1957 Physicians' Desk Reference stated that it was “indicated in chronic fatigue and lethargic and depressed states, including those associated with tranquilizing agents and other drugs; disturbed senile behavior; psychoneuroses and psychoses associated with depression; and in narcolepsy.”14(p441) Methylphenidate is currently available from Novartis Pharmaceuticals Corporation in both immediate-release and sustained-release tablets for oral administration and is U.S. Food and Drug Administration (FDA)–approved for the treatment of attention-deficit/hyperactivity disorder and narcolepsy.9 It has unlabeled uses in depression in the elderly, cancer patients, and poststroke patients.15
Methylphenidate has become the drug of first choice prescribed by many physicians for the initial treatment of ADHD. Usual doses range from 10 to 60 mg/day depending on the age and the response of the child.9,15,16 ADHD can continue in adulthood, and many patients with ADHD may need to continue to take methylphenidate indefinitely.17,18
PHARMACOLOGIC EFFECTS
Methylphenidate is classified as a CNS stimulant. Its proposed mechanism of action is the release and increase of CNS dopamine.19,20 This release is secondary to its effect on the dopamine transport mechanism, which results in an increased amount of postsynaptic dopamine. This increase provides the needed stimulation and proposed activation of the motor inhibitory system in the orbital-frontal-limbic axis.21 This activation results in an increase in inhibition of impulsiveness. Therefore, this medication assists children with ADHD by helping them focus their attention when necessary.
The exact mechanism of action of methylphenidate is dissimilar to that of the amphetamines and cocaine, yet the net effect is an increase in synaptic dopamine. Radiographic studies with (11C)-labeled methylphenidate and cocaine have found the binding of both drugs to be localized in the same brain region, the striatum.22 When methylphenidate is abused, it is the stimulation of D1 dopamine receptors in the nucleus accumbens23 and striato-orbitofrontal cortex24 that is thought to be related to the euphoria and repeated use.
PHARMACOKINETICS
Upon oral administration, methylphenidate is rapidly and completely absorbed from the gastrointestinal tract. Peak concentrations occur 1 to 2 hours25 after dose administration. The pharmacokinetic half-life of methylphenidate is approximately 2 hours25 and ranges from 2 to 7 hours.26 The pharmacologic clinical effects are seen from 4 to 6 hours after an oral dose of immediate-release methylphenidate and 3 to 9 hours after sustained-release methylphenidate.15,26,27 Methylphenidate is metabolized through de-esterification to ritalinic acid.25 Less than 1% of methylphenidate is excreted unchanged in the urine, while 80% of an oral dose is excreted as ritalinic acid.25 Recently, the discovery of the formation of the metabolite ethylphenidate has been reported.28 This can occur when methylphenidate is used concurrently with ethanol and may be a contributing factor in toxicity.
When methylphenidate and cocaine are administered intravenously, their pharmacokinetics are quite similar. Volkow and colleagues22 found that the percentage of each drug taken up by the brain and their rates of uptake were parallel. However, the clearance from the brain of cocaine (t½ = 20 minutes) was faster than that of methylphenidate (t½ > 90 minutes).22 In addition, the receptor-binding affinities for cocaine and methylphenidate are similar at the dopamine transporter in the basal ganglia and the striatum. Intravenous methylphenidate reaches peak concentrations in the basal ganglia in 8 to 15 minutes, whereas the associated “high” feeling peaked in 1 to 3 minutes.29
A well-known pharmacology text states that the pharmacologic properties of methylphenidate “are essentially the same as those of the amphetamines.”30(p221) Another reference states that “the pharmacologic actions of methylphenidate are qualitatively similar to the amphetamines,”16(p2038) while another describes methylphenidate as “a mild CNS stimulant with actions similar to the amphetamines.”15(p773) These same texts also warn of an abuse potential similar to that of the amphetamines,30 as well as the potential overuse and abuse of methylphenidate, especially in patients with “a history of drug dependence or alcoholism.”15(p773),16(p2040) This warning is also clearly stated in the product information statement.9 These brief reminders of the abuse potential of methylphenidate may need stronger emphasis to sensitize practitioners to the high risk of abuse in certain patient populations.
DOSAGE
While the dosage range varies for children, the average daily dose of methylphenidate for adults is 20 to 30 mg/day.8,15 Most texts recommend that the daily dose should not exceed 60 mg, although some individuals may require higher doses.15,16,30 This limit of 60 mg/day appears to be arbitrary and not based on clinical research. Studies for adults with ADHD suggest 1 mg/kg/day as the usual dose with lower doses producing less response.31,32 These dosages refer to the therapeutic oral dose.
When methylphenidate is abused intranasally, the effects are usually similar to intranasal use of amphetamines and crack cocaine.22 Doses for intranasal methylphenidate abuse have been reported as high as 200 mg.33 Intravenous doses in abuse have been reported in the range of 40 mg to 1000 mg.34,35
ABUSE POTENTIAL
The potential for abuse is emphasized throughout the literature and should serve as a warning to clinicians. However, this warning is often overshadowed by the many patients who have a positive therapeutic response to oral methylphenidate and do not abuse it. When used intranasally, methylphenidate has receptor effects similar to those of cocaine. A rapid release of synaptic dopamine occurs, producing subjective effects of an instant “high” and an intensely gratifying euphoria. Thus, the clinical picture of abuse is often quite similar to that of cocaine. Volkow and colleagues22,24 have found that the localization of methylphenidate binding with dopaminergic pathways was “identical” with that of cocaine and a similar “high” was described by patients receiving both drugs intravenously.
Because cocaine is one of the most rewarding and reinforcing drugs,36 statements such as “Subjective effects similar to cocaine's are produced by amphetamine, dextroamphetamine, methamphetamine, phenmetrazine, methylphenidate, and diethylpropion”37 can give health care providers a reference by which to judge the abuse potential of methylphenidate. Methylphenidate can be transformed from a therapeutic agent to an abused and addictive substance when this drug is taken in excessive amounts and used through intranasal and intravenous routes.
Availability is often an integral part of a drug's abuse potential, and the availability of methylphenidate is certainly increasing. According to the Drug Enforcement Agency (DEA), the production of methylphenidate in the United States has increased from 1361 kilograms in 1985 to 10,410 kilograms in 1995 with a 6-fold increase in production from 1990 to 1995.35 In addition, the number of children diagnosed with ADHD has increased 2.5-fold in this same time period.11 Currently, methylphenidate is controlled by the DEA by its assignment of schedule II status, which means the drug “has a high potential for abuse … and may lead to severe psychological and physical dependence.”38 Although these drugs are indicated in the treatment of medical conditions, schedule II medications are subject to strict regulations.
Ignorance of this potential for abuse starts early as described in a survey of school-aged children who were asked about the drug Ritalin.39 No child thought that this drug or other treatment for ADHD could lead to abuse. However, 16% of these children reported that they were asked to sell, give, or trade stimulant medication.39 Abuse has also been reported in family members.40
How fast a drug works often predicts its abuse potential and reinforcement liability.41 Various investigators have supported this hypothesis by comparing the kinetic time course in the brain with the “high” subjects' experience. Specifically, when methylphenidate is given intravenously, subjects reported “highs” paralleling the kinetics of cocaine rather than the kinetics of methylphenidate. As mentioned previously, when administered intravenously, these drugs are indistinguishable and have a parallel rate of uptake into the brain (cocaine: 4–6 minutes, methylphenidate: 4–8 minutes).22,23
ABUSE PATTERNS
In the early 1960s, the abuse potential of methylphenidate was questioned in a case report of a patient who was taking 125 tablets of methylphenidate daily.42 Subsequent reports of oral methylphenidate abuse appeared in the literature including reports of methylphenidate hallucinations,43–45 paranoia,45 euphoria,46 and delusional disorder.47
Intravenous abuse of methylphenidate associated with psychosis was noted in 196343 followed by several reports of intravenous abuse in the early 1970s.44,45,48 Subsequently, a prospective study described the intravenous abuse patterns, morbidity, and mortality associated with methylphenidate.49 The sole source of methylphenidate for these patients involved the diversion of prescription medication.
Intranasal Abuse
Intranasal abuse has not been scientifically assessed, but the occurrence and effects have been demonstrated through case reports in the literature. The first report of intranasal abuse of methylphenidate33 appeared in 1991. A 16-year-old boy with a 2-year history of methylphenidate abuse reported using his prescription medication to get “high.” He was using up to 200 mg/day intranasally.33 He became anxious and “out of control” and was admitted to the hospital for treatment in a depressed and suicidal state. A DEA document reports 2 cases of health professionals abusing intranasal methylphenidate.35 This document also mentions 2 deaths attributed to intranasal use; however, specific data are not reported.35
An additional case of abuse by a 15-year-old boy with ADHD50 was reported in 1998. The boy had a 2-week history of methylphenidate abuse that started with feelings of euphoria and ended in paranoia, depression, and suicidal ideation.50 He was using intranasal doses of 60 mg of sustained-release methylphenidate. A recent case in the literature51 describes the death of a 19-year-old teen following abuse of intranasal methylphenidate. The teenager lost consciousness, fell, hit his head, and then went into cardiopulmonary arrest. Toxicologic analyses confirmed the presence of methylphenidate and alcohol.
TOXICITY
Acute Toxicity
Acute toxicity due to methylphenidate overdose results in symptoms similar to those of acute amphetamine intoxication. Reports of psychiatric symptoms that have occurred include euphoria, delirium, confusion, toxic psychosis, and hallucinations.8,16 Such symptoms should not be unexpected as methylphenidate's pharmacologic effects are “basically the same as those of amphetamines.”52 Cases of psychosis with methylphenidate abuse have been reported when the drug is used in “runs,” similar to amphetamine abuse.52
There are limited data in the literature regarding the psychiatric side effects of methylphenidate when it is abused. Most of the data are found in case reports and are often reported as similar to the psychiatric side effects of amphetamines or cocaine. The clinical picture of the effects of high-dose methylphenidate resembles that of amphetamine intoxication and psychosis. The presentation of this psychiatric picture is often quite dramatic, but is transient and has been seen with all major stimulants, including methylphenidate.53
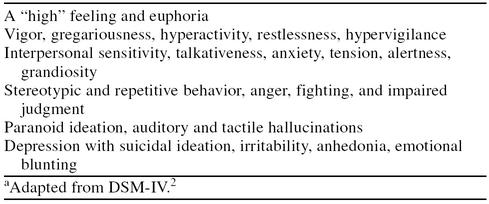
Psychiatric symptoms of extreme anger with threats of aggressive behavior may occur in methylphenidate abuse. When high doses are taken, delirium, aggressiveness, panic states, and hallucinations have been observed.7,54,55 In fact, the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),2 does not differentiate between amphetamines and methylphenidate in regard to the signs and symptoms of toxicity. DSM-IV goes on further to state: “Most of the effects of amphetamine and amphetamine-like drugs are similar to cocaine.”2(p205) Methylphenidate may be more potent than amphetamine when abused.54 Although the DSM-IV lists cocaine and amphetamine problems separately, the clinical profile of each is quite similar. Psychological and behavioral symptoms of amphetamine use are listed in Table 1.
Table 1.
Psychological and Behavioral Symptoms of Amphetamine Usea
Stimulant Toxicity
When abused, methylphenidate produces toxicity similar to other CNS stimulant overdoses. The clinical picture of stimulant intoxication produces a wide array of symptoms including schizophrenic symptoms, manic-like states, psychoses, depressions (especially during withdrawal), and various types of anxiety conditions including panic states.52–54 Motor and behavioral symptoms of overdose may include bruxism, repeated touching or stereotypic confusion, disoriented behavior, punding, obsessive-compulsive tendencies, aggressiveness, and repetitive behaviors.53,55
Psychiatric symptoms of stimulant overdose may include hallucinations, delusions, paranoia, confusion, disorientation, and loose association of ideas. Ellingwood56 studied amphetamine abusers and found that patients developed auditory hallucinations (N = 14), visual hallucinations (N = 15), and experiences of estrangement and/or depersonalization (N = 8). In addition, marked preoccupation with facial features (N = 10) was reported.56 Psychotic symptoms usually arise with chronic abuse, but may also appear acutely with large doses of stimulants. These psychiatric and physical side effects resolve over a period of hours to weeks.53 The dose required to produce psychic or motor disturbance varies considerably. Some abusers may experience increasing effects after multiple doses (similar to sensitization), while others experience severe effects from small doses (reverse tolerance).2,53
In addition, homicide related to amphetamine intoxication has been reported.55 Paranoid ideation, which can be very frightening to the stimulant user, is often present when violence occurs. This suspiciousness combined with impaired judgment and insight can be a catalyst for violence and murder.57,58 Ellingwood59 reported a series of cases in which amphetamines were related to homicide, detailing the amphetamine-induced alterations in behavior and thought that led to homicide. These included reduced impulse control, paranoia, panic, and emotional instability (N = 13).
To summarize, the psychiatric side effects of methylphenidate are quite similar to those of cocaine and amphetamines, giving more support to the idea that almost all CNS stimulants will produce a similar clinical picture. A person using cocaine can experience nervousness,57,58 restlessness,58 agitation,57 suspiciousness,60 paranoia,61–63 hallucinations and delusions,61,63 impaired cognitive functions,64 delirium,65 violence,57,58,62,65,66 suicide,67 and homicide.67–70
CONCLUSION
The potential for methylphenidate abuse has been addressed primarily through regulatory measures. These include regulating the amount of methylphenidate able to be filled at pharmacies during a specified time period and adding a higher level of surveillance by assigning it to schedule II status. Other measures to reduce abuse include encouraging tablet counts by parents and considering changing to stimulants that do not require a dose in the middle of the day, thereby decreasing handling by children in schools. Given the potential for abuse, methylphenidate merits being maintained as a schedule II drug despite parental requests to deregulate it.35
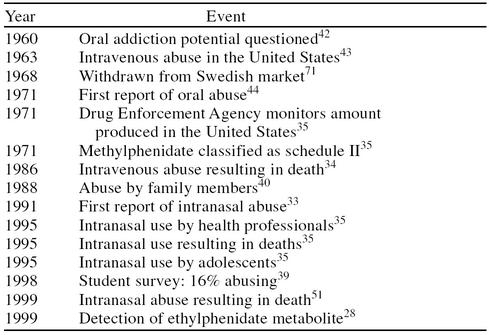
Prevention of methylphenidate abuse needs to be a shared responsibility between the practitioner, the parents, and the patient. All participants in therapy need to be educated about the abuse potential of methylphenidate. The history and emerging patterns of abuse as outlined in Table 2 will help sensitize practitioners and patients to the risk of abuse. Practitioners need to address such issues as the consequences of excessive use or intranasal use as well as other abuse patterns. The use of methylphenidate by anyone other than the patient to whom it was prescribed needs to be addressed and caution maintained throughout therapy. The extreme consequences of abuse and addiction, resulting in legal repercussions, psychiatric symptoms and disorders, as well as death and homicide, need to be discussed seriously.
Table 2.
A Brief History of Methylphenidate Abuse
Education must originate with the prescriber. Increasing practitioner awareness of the pharmacologic, psychological, and physiologic similarities with cocaine is essential to avoid potential abuse. The medical and treatment communities need to be aware of these potential problems, and primary care practitioners need to be aware of the problems associated with methylphenidate abuse, recognize the abuse patterns, and take a strong position in educating all those concerned with methylphenidate use.
Drug names: amphetamine (Adderall), dextroamphetamine (Dexedrine and others), methamphetamine (Desoxyn), methylphenidate (Ritalin and others).
REFERENCES
- Challman TD, Lipsky JJ. Methylphenidate: its pharmacology and uses. Mayo Clin Proc. 2000;75:711–721. doi: 10.4065/75.7.711. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- Sharma V, Newcorn JH, Matier-Sharman K, and et al. Attention deficit and disruptive behavior disorders. In: Tasman A, Kay J, Lieberman JA, eds. Psychiatry. Philadelphia, Pa: Saunders. 1997 669 [Google Scholar]
- Diagnosis and treatment of attention deficit hyperactivity disorder (ADHD) NIH Consens Statement Nov 16–18. 1998;16:1–37. [PubMed] [Google Scholar]
- Biederman J. Attention-deficit/hyperactivity disorder: a life-span perspective. J Clin Psychiatry. 1998;59(suppl 7):4–16. [PubMed] [Google Scholar]
- Findling RL, Dogin JW. Psychopharmacology of ADHD: children and adolescents. J Clin Psychiatry. 1998;59(suppl 7):42–49. [PubMed] [Google Scholar]
- Wender PH. Pharmacotherapy of attention-deficit/hyperactivity disorder in adults. J Clin Psychiatry. 1998;59(suppl 7):76–79. [PubMed] [Google Scholar]
- Rappley MD. Safety issues in the use of methylphenidate: an American perspective. Drug Saf. 1997;17:143–148. doi: 10.2165/00002018-199717030-00001. [DOI] [PubMed] [Google Scholar]
- Ritalin [package insert]. Summit, NJ: Novartis. 1999. [Google Scholar]
- Firestone P, Musten LM, Pisterman S, et al. Short-term side effects of stimulant medication are increased in preschool children with attention-deficit/hyperactivity disorder: a double-blind placebo-controlled study. J Child Adolesc Psychopharmacol. 1998;8:13–25. doi: 10.1089/cap.1998.8.13. [DOI] [PubMed] [Google Scholar]
- Zito JM, Safer DJ, dosReis S, et al. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283:1025–1030. doi: 10.1001/jama.283.8.1025. [DOI] [PubMed] [Google Scholar]
- Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics. 1996;98:1084–1088. [PubMed] [Google Scholar]
- Panizzon L. La preparazione di piridil-e piperidil-arilacetonitrili e di alcuni prodotti di trasformazione (Parte I) Chimica Acta. 1944;27:1748–1757. [Google Scholar]
- NM M. Ritalin (methylphenidate). Physicians' Desk Reference. 11th ed. Oradell, NJ: Medical Economics. 1956 441–442. [Google Scholar]
- Hebel SK. ed. Drug Facts and Comparisons. St. Louis, Mo: Facts and Comparisons. 2000 773–774. [Google Scholar]
- McEvoy GK. ed. American Hospital Formulary Service Drug Information. Bethesda, Md: American Society of Health-Systems Pharmacists. 1999 2038–2040. [Google Scholar]
- Wender PH. Attention-Deficit Hyperactivity Disorder in Adults. New York, NY: Oxford University Press. 1995 [DOI] [PubMed] [Google Scholar]
- Spencer T, Biederman J, Wilens TE, et al. Adults with attention-deficit/hyperactivity disorder: a controversial diagnosis. J Clin Psychiatry. 1998;59(suppl 7):59–68. [PubMed] [Google Scholar]
- Gatley SJ, Volkow ND, Gifford AN, et al. Dopamine-transporter occupancy after intravenous doses of cocaine and methylphenidate in mice and humans. Psychopharmacology (Berl) 1999;146:93–100. doi: 10.1007/s002130051093. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, et al. Reinforcing effects of psychostimulants in humans are associated with increases in brain dopamine and occupancy of D2 receptors. J Pharmacol Exp Ther. 1999;291:409–415. [PubMed] [Google Scholar]
- Barkely RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry. 1995;52:456–463. doi: 10.1001/archpsyc.1995.03950180042006. [DOI] [PubMed] [Google Scholar]
- Fowler JS, Volkow ND. PET imaging studies in drug abuse. Clin Toxicol. 1998;36:163–174. doi: 10.3109/15563659809028936. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, et al. Association of methylphenidate-induced craving with changes in right striato-orbitofrontal metabolism in cocaine abusers: implications in addiction. Am J Psychiatry. 1999;156:19–26. doi: 10.1176/ajp.156.1.19. [DOI] [PubMed] [Google Scholar]
- Patrick KS, Mueller RA, Gualtieri CT, and et al. Pharmacokinetics and actions of methylphenidate. In: Meltzer HY, ed. Psychopharmacology: The Third Generation of Progress. 3rd ed. New York, NY: Raven Press. 1987 1390 [Google Scholar]
- Fox AM, Rieder MJ. Risks and benefits of drugs used in the management of the hyperactive child. Drug Saf. 1993;9:42. doi: 10.2165/00002018-199309010-00004. [DOI] [PubMed] [Google Scholar]
- Elia J, Ambrosini PJ, Rapoport JL. Treatment of attention-deficit/hyperactivity disorder. N Engl J Med. 1999;340:780–788. doi: 10.1056/NEJM199903113401007. [DOI] [PubMed] [Google Scholar]
- Markowitz JS, Logan BK, Diamond F, et al. Detection of the novel metabolite ethylphenidate after methylphenidate overdose with alcohol coingestion. J Clin Psychopharmacol. 1999;19:362–366. doi: 10.1097/00004714-199908000-00013. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Gatley SJ, et al. Temporal relationships between the pharmacokinetics of methylphenidate in the human brain and its behavioral and cardiovascular effects. Psychopharmacology (Berl) 1996;123:26–33. doi: 10.1007/BF02246277. [DOI] [PubMed] [Google Scholar]
- Hoffman BB, Lefkowitz RJ. Catecholamines, sympathomimetic drugs, and adrenergic receptor antagonists. In: Hardman JG, Limbird LE, Molinoff PB, et al, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: McGraw-Hill. 1996 221–224. [Google Scholar]
- Spencer T, Wilens T, Biederman J, et al. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry. 1995;52:434–443. doi: 10.1001/archpsyc.1995.03950180020004. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Biederman J, Spencer TJ, et al. Pharmacotherapy of adult attention deficit/hyperactivity disorder: a review. J Clin Psychopharmacol. 1995;15:270–279. doi: 10.1097/00004714-199508000-00006. [DOI] [PubMed] [Google Scholar]
- Jaffe SL. Intranasal abuse of prescribed methylphenidate by an alcohol and drug abusing adolescent with ADHD. J Am Acad Child Adolesc Psychiatry. 1991;30:773–775. [PubMed] [Google Scholar]
- Levine B, Caplan YH, Kauffman G. Fatality resulting from methylphenidate overdose. J Anal Toxicol. 1986;10:209–210. doi: 10.1093/jat/10.5.209. [DOI] [PubMed] [Google Scholar]
- Methylphenidate Review Document. Washington, DC: Drug and Chemical Evaluation Section, Office of Diversion Control, Drug Enforcement Administration. 1995 1–114. [Google Scholar]
- Johnson CE, Fischman MW. The pharmacology of cocaine related to its abuse. Pharmacol Rev. 1989;41:3–52. [PubMed] [Google Scholar]
- O'Brien CP. Drug addiction and drug abuse. In: Hardman JG, Limbird LE, Molinoff PB, et al, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: McGraw-Hill. 1996 571 [Google Scholar]
- Drug Enforcement Administration. Schedule II. Drugs of abuse. Available at: http://www.usdoj.gov/dea/concern/abuse/chap1/control/sched2.html. Accessed April 5, 2000. [Google Scholar]
- Musser CJ, Ahmann PA, Theye FW, et al. Stimulant use and the potential for abuse in Wisconsin as reported by school administrators and longitudinally followed children. J Dev Behav Pediatrics. 1998;19:187–192. doi: 10.1097/00004703-199806000-00006. [DOI] [PubMed] [Google Scholar]
- Fulton AI, Yates WR. Family abuse of methylphenidate. Am Fam Pract. 1988;38:143–145. [PubMed] [Google Scholar]
- Oldendorf WH. Some relationships between addiction and drug delivery to the brain. NIDA Res Monogr. 1992;120:13–25. [PubMed] [Google Scholar]
- Rioux B. Is Ritalin an addiction-producing drug? Dis Nerv Syst. 1960;21:346–349. [PubMed] [Google Scholar]
- McCormick TC Jr, McNeel TW. Acute psychosis and Ritalin abuse. Tex State J Med. 1963;59:99–100. [Google Scholar]
- Lucas AR, Weiss M. Methylphenidate hallucinosis. JAMA. 1971;217:1079–1081. [PubMed] [Google Scholar]
- Spensley J, Rockwell DA. Psychosis during methylphenidate abuse. N Engl J Med. 1972;286:880–881. doi: 10.1056/NEJM197204202861607. [DOI] [PubMed] [Google Scholar]
- Corrigall R, Ford T. Methylphenidate euphoria. J Am Acad Child Adolesc Psychiatry. 1996;35:1421. doi: 10.1097/00004583-199611000-00005. [DOI] [PubMed] [Google Scholar]
- Bloom AS, Russell LJ, Weisskopf B, et al. Methylphenidate-induced delusional disorder in a child with attention deficit disorder with hyperactivity. J Am Acad Child Adolesc Psychiatry. 1988;27:88–89. doi: 10.1097/00004583-198801000-00013. [DOI] [PubMed] [Google Scholar]
- Wiley RF. Abuse of methylphenidate (Ritalin) New Engl J Med. 1971;285:464. [PubMed] [Google Scholar]
- Parran TW, Jasinski DR. Intravenous methylphenidate abuse: prototype for prescription drug abuse. Arch Intern Med. 1991;151:781–783. [PubMed] [Google Scholar]
- Garland EJ. Intranasal abuse of prescribed methylphenidate. J Am Acad Child Adolesc Psychiatry. 1998;37:573–574. doi: 10.1097/00004583-199806000-00006. [DOI] [PubMed] [Google Scholar]
- Massello W, Carpenter DA. A fatality due to the intranasal abuse of methylphenidate (Ritalin) J Forensic Sci. 1999;44:220–221. [PubMed] [Google Scholar]
- Kroft C, Cole JO. Adverse behavioral effects of psychostimulants. In: Kane JM, Lieberman JA, eds. Adverse Effects of Psychotropic Drugs. New York, NY: Guilford Press. 1992 159. [Google Scholar]
- Schuckit MA. Drug and Alcohol Abuse: A Clinical Guide to Diagnosis and Treatment. 4th ed. New York, NY: Plenum Medical Book Co. 1995 133–135. [Google Scholar]
- Segal DS, Janowsky DS. Psychostimulant-induced behavioral effects: possible models of schizophrenia. In: Lipton MA, DiMascio A, Killam KF, eds. Psychopharmacology: A Generation of Progress. New York, NY: Raven Press. 1978 1113–1122. [Google Scholar]
- Volavka J. Neurobiology of Violence. Washington, DC: American Psychiatric Press. 1995 203–205. [Google Scholar]
- Ellingwood EH. Amphetamine psychosis, 1: description of the individuals and process. J Nerv Ment Dis. 1967;144:277–283. [Google Scholar]
- Inciardi JA. The crack-violence connection within a population of hard-core adolescent offenders. NIDA Res Monogr. 1990;103:92–111. [PubMed] [Google Scholar]
- McCormick RA, Smith M. Aggression and hostility in substance abusers. Addict Behav. 1995;20:555–562. doi: 10.1016/0306-4603(95)00015-5. [DOI] [PubMed] [Google Scholar]
- Ellingwood EH. Assault and homicide associated with amphetamine abuse. Am J Psychiatry. 1971;127:1170–1176. doi: 10.1176/ajp.127.9.1170. [DOI] [PubMed] [Google Scholar]
- Sherer MA. Intravenous cocaine: psychiatric effects, behavioral mechanisms. Biol Psychiatry. 1988;24:865–885. doi: 10.1016/0006-3223(88)90222-3. [DOI] [PubMed] [Google Scholar]
- Satel SL, Southwick SM, Gawin FH. Clinical features of cocaine-induced paranoia. Am J Psychiatry. 1991;148:495–498. doi: 10.1176/ajp.148.4.495. [DOI] [PubMed] [Google Scholar]
- Miller NS, Gold MS, Mahler JC. Violent behaviors associated with cocaine use: possible pharmacological mechanisms. Int J Addict. 1991;26:1077–1088. doi: 10.3109/10826089109058942. [DOI] [PubMed] [Google Scholar]
- Manschreck TC, Laughery JA, Weisstein CC, et al. Characteristics of freebase cocaine psychosis. Yale J Biol Med. 1988;61:115–122. [PMC free article] [PubMed] [Google Scholar]
- Bolla KI, Cadet J, London ED. The Neuropsychiatry of Chronic Cocaine Abuse. J Neuropsychiatr Clin Neurosci. 1998;10:280–289. doi: 10.1176/jnp.10.3.280. [DOI] [PubMed] [Google Scholar]
- Wetli CV, Fishbain DA. Cocaine-induced psychosis and sudden death in recreational cocaine users. J Forensic Sci. 1985;30:873–880. [PubMed] [Google Scholar]
- Marzuk PM, Tardiff K, Leon AC, et al. Prevalence of cocaine use among residents of New York City who committed suicide during a one-year period. Am J Psychiatry. 1992;149:371–375. doi: 10.1176/ajp.149.3.371. [DOI] [PubMed] [Google Scholar]
- Tardiff K, Marzuk PM, Leon AC, et al. Cocaine, opiates, and ethanol in homicides in New York City. J Forensic Sci. 1995;40:387–390. [PubMed] [Google Scholar]
- Marzuk PM, Tardiff K, Leon AC, et al. Fatal injuries after cocaine use as a leading cause of death among young adults in New York City. N Engl J Med. 1995;332:1753–1757. doi: 10.1056/NEJM199506293322606. [DOI] [PubMed] [Google Scholar]
- Lowry PW, Hassig SE, Gunn RA, et al. Homicide victims in New Orleans: recent trends. Am J Epidemiol. 1988;128:1130–1136. doi: 10.1093/oxfordjournals.aje.a115055. [DOI] [PubMed] [Google Scholar]
- Budd RD. Cocaine abuse and violent death. Am J Drug Alcohol Abuse. 1989;15:375–382. doi: 10.3109/00952998908992798. [DOI] [PubMed] [Google Scholar]
- Perman ES. Speed in Sweden. N Engl J Med. 1970;283:760–761. doi: 10.1056/NEJM197010012831410. [DOI] [PubMed] [Google Scholar]