Abstract
Background: Physicians in the United States write approximately 10 million new prescriptions for oral corticosteroids each year. Common side effects of corticosteroids include weight gain, osteoporosis, and diabetes mellitus. This article reviews the available literature on psychiatric and cognitive changes during corticosteroid therapy.
Method: A search of the MEDLINE and psycINFO databases was conducted to find clinically relevant articles on psychiatric and cognitive side effects with corticosteroids using search terms including corticosteroid, prednisone, mania, depression, psychosis, mood, memory, and cognition.
Results: Symptoms of hypomania, mania, depression, and psychosis occur during corticosteroid therapy as do cognitive changes, particularly deficits in verbal or declarative memory. Psychiatric symptoms appear to be dose-dependent and generally occur during the first few weeks of therapy. Patients who must remain on corticosteroids may benefit from pharmacotherapeutic approaches, such as lithium and the new antipsychotic medications.
Conclusion: Mood and cognitive changes with corticosteroids appear to be common but generally mild and reversible side effects. More studies are needed to determine effective treatment for steroid-induced psychiatric disorders.
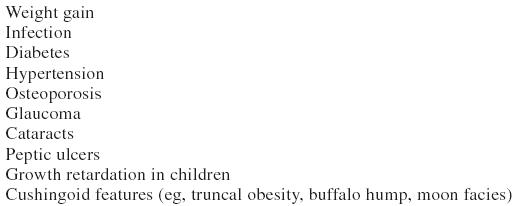
Since the late 1940s, prescription corticosteroids have been used to treat common medical problems such as asthma, allergies, rheumatoid arthritis, and dermatological diseases.1 The systemic side effects of these medications, such as diabetes, osteoporosis, glaucoma, and cataracts, are well known to physicians (Table 1). Psychiatric side effects, as illustrated by the case below, can also occur.
Table 1.
Systemic Side Effects of Corticosteroids
Case study.
Patient A is a 43-year-old woman with no past psychiatric history who was diagnosed with Behçet's disease 4 years ago requiring chronic corticosteroid therapy. Since beginning prednisone, 10–20 mg daily, she reported “severe mood swings” that worsened when the dose was increased. She had episodes of elevated or irritable mood, increased energy, decreased sleep (3 hours each night), racing thoughts, and pressured speech. However, she also had periods of depressed mood, increased appetite and weight gain, poor concentration, loss of interest, and suicidal ideation. The prednisone dose could not be reduced without a worsening of symptoms of Behçet's disease. Psychiatric medications taken over the past 3 years with poor or modest results included fluoxetine, sertraline, amitriptyline, alprazolam, valproic acid, and carbamazepine.
Had prednisone therapy not been mentioned, most physicians would have suspected the patient had severe bipolar disorder, refractory to treatment. These psychiatric symptoms are classified as substance-induced mood disorders, psychotic disorders, or delusions in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.2 This category includes psychiatric disturbances due to other prescription medications (e.g., digitalis, antihypertensives), as well as illicit drugs (e.g., cocaine, heroin), and requires evidence by history, physical examination, or laboratory findings that the symptoms are temporarily or etiologically related to the substance use. This review briefly examines clinically relevant evidence on mood symptoms, psychosis, and cognitive changes resulting from corticosteroid use and the treatment of these symptoms.
PREVALENCE AND TYPE OF PSYCHIATRIC CHANGES DURING CORTICOSTEROID THERAPY
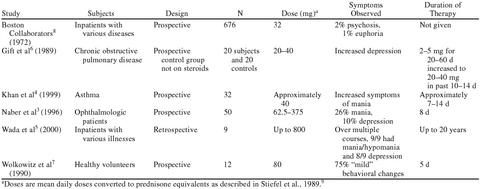
A search of the MEDLINE and psycINFO databases using search terms including corticosteroid, prednisone, mania depression, psychosis, mood, memory, and cognition and hand searches to find studies on the nature and prevalence of psychiatric symptoms with corticosteroids yielded 6 reports with pertinent data (1996–10/2000) after excluding case reports, anecdotal observations, and studies not using clearly defined diagnostic criteria (Table 2). Naber et al.3 used a semistructured interview and the Profile of Mood States (POMS) to prospectively examine patients (N = 50) on short courses of high-dose steroids. They found that 26% of patients with ophthalmologic disorders (i.e., retinitis and uveitis), who were initially free of psychiatric illness, developed mania and 10% developed depression during corticosteroid therapy. No psychotic symptoms (such as hallucinations or delusions) were observed. In all cases, the symptoms began within the first 3 days of therapy and continued throughout the 8 days of the study. Gender, age, or history of prior corticosteroid treatment did not predict response. These findings suggest that symptoms of mania are more common than depression during short courses of high-dose steroids.
Table 2.
Studies Examining Psychiatric Symptoms in Corticosteroid-Treated Patients
Recent findings by our group also suggest manic but not depressive symptoms may be common with steroids. Khan et al.4 found statistically significant increases in scores on the Young Mania Rating Scale but not on the Hamilton Rating Scale for Depression in asthma patients (N = 32) receiving 1- to 2-week courses of prednisone at approximately 40 mg/day.
Similarly, Wada et al.,5 in a retrospective examination of 9 patients with more than one episode of steroid-induced mood changes, found that 85% of the episodes were primarily manic in nature. The findings again seem to support a preponderance of manic symptoms with these medications.
Gift et al.6 found increased symptoms of depression in a group of patients with chronic obstructive pulmonary disease (COPD) who were receiving corticosteroids. In this study, the corticosteroid-treated group had significantly higher scores on the Beck Depression Inventory and Brief Symptom Inventory (p < .01) than the controls. These findings could suggest an increase in depressive symptoms with steroids. However, this study did not use measures for mania. Therefore, increased depression scores could have been observed as part of a mixed state, combining features of mania and depression, or even pure mania, as both mania and depression can share symptoms such as decreased concentration, agitation, and insomnia.
Wolkowitz et al.7 examined psychiatric side effects in a group of 12 healthy volunteers receiving 80 mg/day of prednisone for 5 days. Most subjects reported some symptoms, including depressed or elevated mood, irritability, lability, insomnia, increased energy, anxiety, or depersonalization, but no group mean changes in psychiatric rating scales could be demonstrated perhaps due to the heterogeneity of symptoms.
Psychiatric side effects with corticosteroids appear to be dose-dependent. The Boston Collaborative Drug Surveillance Program (BCDSP, N = 676)8 examined psychiatric symptoms in patients free of psychiatric disease prior to steroid treatment. Diagnoses during steroid exposure included psychosis, mania, and clinical depression. Severe psychiatric illness was uncommon (1.3%) with doses less than 40 mg/day of prednisone, but increased to 18.4% at doses above 80 mg/day of prednisone, strongly supporting that these symptoms are dose dependent.
EFFECTS OF CORTICOSTEROIDS ON MEMORY
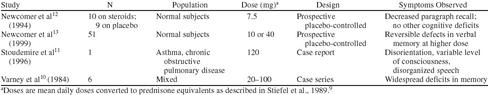
Cognitive impairment has been reported during systemic corticosteroid administration (Table 3). Even severe cognitive impairment consistent with dementia or delirium has been reported.10,11 Varney et al.10 reported a case series of 6 patients (aged 25–65 years) who developed significant and widespread reversible cognitive function deficits, including attention, concentration, and verbal memory, while taking 20 to 100 mg of prednisone daily. Stoudemire et al.11 reported the case of a 40-year-old woman with asthma and chronic obstructive pulmonary disease who developed disorientation and disorganized speech on 100 mg of prednisone daily.
Table 3.
Studies Examining Cognitive Effects of Corticosteroids
Milder cognitive deficits are generally those of declarative (verbal) memory assessed by using instruments such as word lists. Deficits in declarative memory have been observed even in subjects receiving only 4 to 5 days of dexamethasone or prednisone treatment.7,12,13 Newcomer et al.12 reported reductions in paragraph recall, a test of declarative memory, in normal subjects given dexamethasone for 4 days compared to placebo. Seven days after the last dose of dexamethasone, the subjects showed a return to normal performance on the memory test. More recently, Newcomer et al.13 reported a reversible and dose-dependent impairment in declarative memory with high-dose hydrocortisone (160 mg/day = 40 mg/day prednisone equivalents) but not low-dose hydrocortisone (40 mg/day = 10 mg/day prednisone equivalents) administration.
TREATMENT OF CORTICOSTEROID-INDUCED PSYCHIATRIC SYMPTOMS
Dose reduction or discontinuation of the systemic corticosteroid is associated with improvement in psychiatric symptoms in many studies.8,14,15 One study suggested lithium therapy may prevent corticosteroid-induced psychiatric disturbances.16 Anecdotal evidence supports that lithium may be effective for the acute treatment of corticosteroid-induced psychiatric symptoms including both mania17 and depression.18 Other reports suggest valproic acid,19 neuroleptics,8,20–23 and atypical antipsychotics24 can also be useful for these symptoms.
On the other hand, some data suggest that tricyclic antidepressants can lead to a significant worsening of symptoms. Hall et al.20,25 found that tricyclic antidepressants were associated with increased agitation and psychosis in 4 patients receiving steroid therapy. Blazer et al.21 reported a poor response to tricyclic antidepressants in 2 patients with depression during corticosteroid therapy. However, the use of a newer selective serotonin reuptake inhibitor, fluoxetine, was reported to improve symptoms of depression during corticosteroid therapy in one patient.26 No data were found on the pharmacologic treatment of cognitive changes associated with corticosteroid usage. However, the cognitive deficits reported in Table 3 were reversible with discontinuation of corticosteroids.
PATIENT CARE ISSUES
Symptoms observed during corticosteroid therapy frequently include mania. Mania or hypomania appear to be more common than depression.3–5 The risks of psychiatric side effects increase at higher dosages.8
Any patient who is begun on systemic corticosteroid treatment should be advised of potential side effects, including behavioral changes. As data suggest the rapid onset of psychiatric side effects, the patient should be seen in follow-up soon after initiating therapy, preferably within a week. Along with monitoring weight, glucose, and blood pressure, the patient should be asked about mood swings and symptoms of depression and observed for signs of mania, such as increased energy, rapid speech, and insomnia.
Cognitive effects of corticosteroids appear to occasionally include severe disturbances consistent with dementia or delirium,10,11 but no population-based studies were found examining the prevalence of these symptoms during corticosteroid therapy. Studies in persons free of medical morbidity suggest milder and specific reversible and dose-dependent deficits in verbal or declarative memory even during several days of corticosteroid administration.7,12,13 The types of cognitive deficits observed are consistent with hippocampal dysfunction.27 The hippocampus is a brain region with a high concentration of glucocorticoid receptors.28 Whether these memory deficits are common and clinically significant in patients receiving prescription corticosteroids remains unanswered. Physicians and patients may be less aware of memory loss with corticosteroids than mood changes. Thus, this potential side effect should also be discussed with patients and monitored by physicians.
Minimal data were found on the treatment of corticosteroid-induced psychiatric disturbances. However, until more studies are performed, some treatment principles can be suggested. Treatment should begin with dose reduction and discontinuation, if possible, thus avoiding the addition of a second medication with its own potential side effects. In the past, this has been difficult because of a limited number of treatment options for most inflammatory disorders. However, with the advent of alternative pharmaceutical regimens (such as methotrexate for rheumatoid arthritis and leukotrienes for asthma), this is a more feasible option. In cases in which psychiatric symptoms are severe, pharmacotherapy should be initiated.
The only controlled treatment study for steroid-induced psychiatric symptoms used lithium.16 If used, lithium should be started at 600 to 900 mg/day and a blood level (10–12 hours after the last dose) obtained in approximately 5 days. Blood levels of 0.5 to 1.0 mEq/L are used for bipolar disorder. Although mood stabilizers such as lithium and valproic acid appear to be effective, carbamazepine should probably be avoided as this medication induces the metabolism of some corticosteroids,29,30 potentially lowering plasma levels of the steroid and increasing symptoms of the underlying disease process.
As antipsychotics do not require monitoring of blood levels, and the newer atypical agents are rarely associated with dystonic reactions or extrapyramidal side effects, these medications may be safe and effective for psychiatric symptoms during corticosteroid therapy. Dosages of olanzapine starting at 2.5 mg at night and increasing up to 20 mg/day may be useful. Anecdotal data suggest that tricyclic antidepressants, but perhaps not the newer antidepressants, can lead to a worsening of symptoms. As depressive symptoms are common in persons with chronic medical illnesses, it can be difficult if not impossible, to determine if corticosteroids are responsible. Further investigations on the use of antidepressants are needed to determine the risks versus benefits for depression during steroid therapy. Antidepressants should probably be avoided as first-line treatment in persons with mood symptoms likely secondary to corticosteroids. If an antidepressant is used, physicians should probably consider prescribing a selective serotonin reuptake inhibitor (e.g., fluoxetine, 20 mg/day) rather than a tricyclic agent (e.g., amitriptyline).
The cognitive effects of corticosteroids appear to be dose-dependent and reversible with discontinuation of the medication. Therefore, the same treatment principle of reducing the dosage and, if possible, discontinuing therapy, as recommended with mood disturbances, seems reasonable. No specific pharmacotherapies for cognitive impairment have been reported in humans. In animals, agents that enhance the reuptake of serotonin and inhibit the release of glutamate (e.g., phenytoin) appear to prevent and even reverse hippocampal damage, including cognitive changes associated with corticosteroids.31,32 Future research should focus on the use of these approaches in humans who require long-term corticosteroid therapy.27
CONCLUSION
Corticosteroids are given for a variety of common illnesses on both an outpatient and inpatient basis. Therefore, the psychiatric side effects of these medications are of concern to all physicians. The data available on incidence and prevalence are scant, and few controlled studies have been performed evaluating treatment for steroid-induced psychiatric problems. However, the available data suggest that the psychiatric symptoms during corticosteroid therapy are dose dependent, often occur early in treatment, and include mania, depression, lability, and psychosis. Future research on the pharmacotherapy of both mood and cognitive symptoms with corticosteroids is needed.
Drug names: alprazolam (Xanax and others), amitriptyline (Elavil and others), carbamazepine (Tegretol and others), dexamethasone (Decadron and others), fluoxetine (Prozac), olanzapine (Zyprexa), phenytoin (Dilantin and others), sertraline (Zoloft), valproic acid (Depakene).
Footnotes
Supported, in part, by the National Alliance for Research on Schizophrenia and Depression (NARSAD), Great Neck, N.Y.; the Sarah M. and Charles E. Seay Center for Basic and Applied Research in Psychiatric Illness, Dallas, Tex.; the John Schemerhorn Psychiatric Fund, Dallas, Tex.; and the Theodore and Vada Stanley Foundation, Bethesda, Md. (Dr. Brown).
REFERENCES
- Brown ES, Suppes T. Mood symptoms during corticosteroid therapy: a review. Harv Rev Psychiatry. 1998;5:239–246. doi: 10.3109/10673229809000307. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association. 2000 143–146. 338,–343. 405–409. [Google Scholar]
- Naber D, Sand P, Heigl B. Psychopathological and neuropsychological effects of 8-days' corticosteroid treatment: a prospective study. Psychoneuroendocrinology. 1996;21:25–31. doi: 10.1016/0306-4530(95)00031-3. [DOI] [PubMed] [Google Scholar]
- Khan DA, Brown ES, Suppes T, et al. Mood changes during prednisone bursts for asthma [abstract] Am J Respir Crit Care Med. 1999;159:A919. [Google Scholar]
- Wada K, Yamada N, Suzuki H, et al. Recurrent cases of corticosteroid-induced mood disorder: clinical characteristics and treatment. J Clin Psychiatry. 2000;61:261–267. doi: 10.4088/jcp.v61n0404. [DOI] [PubMed] [Google Scholar]
- Gift AG, Wood RM, Cahill CA. Depression, somatization and steroid use in chronic obstructive pulmonary disease. Int J Nurs Stud. 1989;26:281–286. doi: 10.1016/0020-7489(89)90009-6. [DOI] [PubMed] [Google Scholar]
- Wolkowitz OM, Rubinow D, Doran AR, et al. Prednisone effects on neurochemistry and behavior. Arch Gen Psychiatry. 1990;47:963–968. doi: 10.1001/archpsyc.1990.01810220079010. [DOI] [PubMed] [Google Scholar]
- The Boston Collaborative Drug Surveillance Program. Acute adverse reactions to prednisone in relation to dosage. Clin Pharmacol Ther. 1972;13:694–698. doi: 10.1002/cpt1972135part1694. [DOI] [PubMed] [Google Scholar]
- Stiefel FC, Breitbart WS, Holland JC. Corticosteroids in cancer: neuropsychiatric complications. Cancer Invest. 1989;7:479–491. doi: 10.3109/07357908909041378. [DOI] [PubMed] [Google Scholar]
- Varney NR, Alexander B, Macindoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141:369–372. doi: 10.1176/ajp.141.3.369. [DOI] [PubMed] [Google Scholar]
- Stoudemire A, Anfinson T, Edwards J. Corticosteroid-induced delirium and dependency. Gen Hosp Psychiatry. 1996;18:196–202. doi: 10.1016/0163-8343(96)00005-9. [DOI] [PubMed] [Google Scholar]
- Newcomer JW, Craft S, Hershen T, et al. Glucocorticoid-induced impairment in declarative memory performance in adult humans. J Neurosci. 1994;14:2047–2053. doi: 10.1523/JNEUROSCI.14-04-02047.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer JW, Selke G, Melson AJ, et al. Decreased memory performance in healthy humans induced by stress-level cortisol treatment. Arch Gen Psychiatry. 1999;56:527–533. doi: 10.1001/archpsyc.56.6.527. [DOI] [PubMed] [Google Scholar]
- Lewis DA, Smith RE. Steroid-induced psychiatric syndromes. J Affect Disord. 1983;5:319–332. doi: 10.1016/0165-0327(83)90022-8. [DOI] [PubMed] [Google Scholar]
- Bender BG, Lerner JA, Kollasch E. Mood and memory changes in asthmatic children receiving corticosteroids. J Am Acad Child Adolesc Psychiatry. 1988;27:720–725. doi: 10.1097/00004583-198811000-00010. [DOI] [PubMed] [Google Scholar]
- Falk WE, Mahnke MW, Poskanzer DC. Lithium prophylaxis of corticotropin-induced psychosis. JAMA. 1979;241:1011–1012. [PubMed] [Google Scholar]
- Kemp K, Lion JR, Magram G. Lithium in the treatment of a manic patient with multiple sclerosis: a case report. Dis Nerv Syst. 1977;38:210–211. [PubMed] [Google Scholar]
- Terao T, Yoshimura R, Shiratuchi T, et al. Effects of lithium on steroid-induced depression. Biol Psychiatry. 1997;41:1225–1226. doi: 10.1016/s0006-3223(97)00019-x. [DOI] [PubMed] [Google Scholar]
- Himelhoch S, Haller E. Extreme mood lability associated with systemic lupus erythematosus and stroke successfully treated with valproic acid. J Clin Psychopharmacol. 1996;16:469–470. doi: 10.1097/00004714-199612000-00019. [DOI] [PubMed] [Google Scholar]
- Hall RCW, Popkin MK, Stickney RN, et al. Presentation of the steroid psychosis. J Nerv Ment Dis. 1979;167:229–236. doi: 10.1097/00005053-197904000-00006. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Petrie WM, Wilson WP. Affective psychosis following renal transplant. Dis Nerv Syst. 1976;37:663–667. [PubMed] [Google Scholar]
- Silva RG, Tolstunov L. Steroid-induced psychosis: report of a case. J Oral Maxillofacial Surg. 1995;53:183–186. doi: 10.1016/0278-2391(95)90398-4. [DOI] [PubMed] [Google Scholar]
- Baloch N. Steroid psychosis: a case report. Br J Psychiatry. 1974;124:545–546. doi: 10.1192/bjp.124.6.545. [DOI] [PubMed] [Google Scholar]
- Brown ES, Khan DA, Suppes T. Treatment of corticosteroid-induced mood changes with olanzapine [letter] Am J Psychiatry. 1999;156:968. doi: 10.1176/ajp.156.6.968. [DOI] [PubMed] [Google Scholar]
- Hall RCW, Popkin MK, Kirkpatrick B. Tricyclic exacerbation of steroid psychosis. J Nerv Ment Dis. 1978;166:738–742. [PubMed] [Google Scholar]
- Wyszynski AA, Wyszynski B. Treatment of depression with fluoxetine in corticosteroid-dependent central nervous systems Sjogren's syndrome. Psychosomatics. 1993;34:173–177. doi: 10.1016/S0033-3182(93)71910-6. [DOI] [PubMed] [Google Scholar]
- Brown ES, Rush AJ, McEwen BS. Hippocampal remodeling and damage by corticosteroids: implications for mood disorders. Neuropsychopharmacology. 1999;21:474–484. doi: 10.1016/S0893-133X(99)00054-8. [DOI] [PubMed] [Google Scholar]
- De Kloet, Vreugdenhil E, Oitzl M, et al. Brain corticosteroid receptor balance in health and disease. Endocrinol Rev. 1998;19:269–301. doi: 10.1210/edrv.19.3.0331. [DOI] [PubMed] [Google Scholar]
- Putignano P, Kaltsas GA, Satta MA, et al. The effects of anti-convulsant drugs on adrenal function. Horm Metab Res. 1998;30:389–397. doi: 10.1055/s-2007-978903. [DOI] [PubMed] [Google Scholar]
- Patsalos PN, Duncan JS. Antiepileptic drugs: a review of clinically significant drug interactions. Drug Saf. 1993;9:156–184. doi: 10.2165/00002018-199309030-00003. [DOI] [PubMed] [Google Scholar]
- Magarinos AM, McEwen BS, Flugge G, et al. Chronic psychosocial stress causes apical dendritic atrophy of hippocampal CA3 pyramidal neurons in subordinate tree shrews. J Neurosci. 1996;16:3534–3540. doi: 10.1523/JNEUROSCI.16-10-03534.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magarinos AM, Deslandes A, McEwen BS. Effects of antidepressants and benzodiazepine treatments on the dendritic structure of CA3 pyramidal neurons after chronic stress. Eur J Pharmacol. 1999;371:113–122. doi: 10.1016/s0014-2999(99)00163-6. [DOI] [PubMed] [Google Scholar]