Abstract
As many as 1 in 4 Americans will experience an anxiety disorder at some point in their lives, and many will also suffer the depression, substance abuse, distressing physical signs, and socioeconomic problems that often accompany these disorders when left untreated. Anxiety disorders can be detected using simple screening tools in the physician's office. Early and effective treatment with appropriate medication can significantly reduce the psychic and physical symptoms of anxiety, lowering the overall costs of the disorder to the health care system and society. Many drugs offer safe and effective relief of anxiety symptoms with few side effects or drug-drug interactions, and some offer symptomatic relief within 1 to 2 weeks.
ANXIETY DISORDERS
Exact figures on the prevalence of anxiety in the United States vary somewhat among studies. However, results of numerous surveys have indicated that anxiety disorders are extremely common in the American population.1 In 1993, a follow-up of the 1988 Epidemiologic Catchment Area (ECA) study reported a 1-year prevalence of 12.3% for all anxiety disorders.2 Further, the National Comorbidity Survey calculated a 1-year prevalence for anxiety disorders of 17.2% and suggested that 1 in 4 Americans (24.9%) would experience an anxiety disorder at some point in their lives.3 It is important to note that the lifetime prevalence and 1-year prevalence for anxiety disorders are greater than those for major depression, a disorder that has been a major focus in the medical community.3
Although the principal symptoms of anxiety disorders include fear, excessive worry, nervousness, and obsessions, a multitude of physical symptoms also may be present. These somatic symptoms—which include heart palpitations, gastrointestinal problems, sweating, fainting, and chronic pain—can confound the diagnosis and resist all forms of medical management, unless the underlying anxiety source is identified and treated. Delays in diagnosis and treatment can be expensive for the patient, physician, and society: unnecessary tests and ineffective treatments increase medical costs, and anxiety symptoms may lead to loss of income and productivity, financial dependence, and even suicide. This review describes the management of patients with anxiety disorders in the primary care setting in the context of the economic costs of this disease on the health care system and society.
Types
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),4 classifies anxiety disorders into several groups: generalized anxiety disorder (GAD); phobias; panic disorder; obsessive-compulsive disorder (OCD); posttraumatic stress disorder (PTSD); acute stress disorder; and anxiety disorders due to a general medical condition, induced by a substance, or not otherwise specified. Primary care physicians often categorize anxiety simply as acute or persistent.5
GAD refers to pervasive and excessive worrying and anxious feelings that persist for at least 6 months, more or less constantly; the anxious feelings are typically accompanied by physical sensations such as dry mouth, palpitations, and muscle tension.4 Phobic disorders are characterized by excessive and unrealistic fears about specific objects (e.g., cats, numbers) or situations (e.g., airplane travel, tunnels); the fear of being embarrassed in public is called social phobia.4 Sudden and unprovoked episodes of terrifying fear and discomfort (often accompanied by psychiatric and physical symptoms) are labeled panic attacks; the recurrence of these episodes is known as panic disorder. A possible accompaniment to panic disorder is agoraphobia, the fear of being trapped in a place or situation from which one cannot escape or in which there will be no help in the event of a panic attack.4
OCD causes thoughts and feelings (obsessions) that are difficult to control and that cause significant anxiety; compulsions are ritualistic actions (e.g., washing hands, arranging objects, counting, checking) that tend to relieve the anxiety temporarily. PTSD can follow a severe, generally life-threatening traumatic occurrence such as exposure to natural disasters (e.g., earthquakes), torture, or rape. People suffering from PTSD repeatedly relive the trauma, lose sleep, and become excessively vigilant or “keyed up.” When these responses last less than 4 weeks, the problem is referred to as acute stress disorder.4
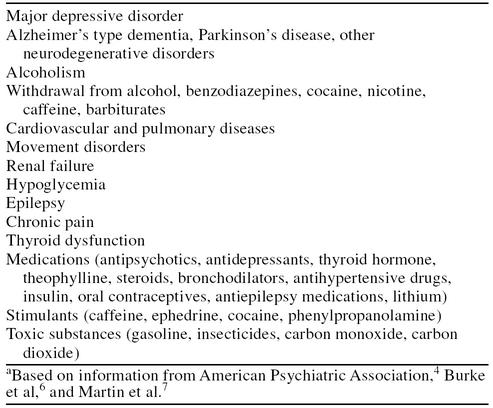
Feelings of anxiety can be associated with a variety of illnesses and may also be triggered by many medications and substances (Table 1).4,6,7 In addition, withdrawal from alcohol, nicotine, barbiturates, benzodiazepines, and caffeine can stimulate the occurrence or recurrence of anxiety. Patients with significant anxiety or phobia that does not meet the DSM-IV criteria for other anxiety disorders are designated as having anxiety disorder not otherwise specified.4,8
Table 1.
Medical Disorders and Substances Associated With Anxiety Symptomsa
Somatic Symptomatology
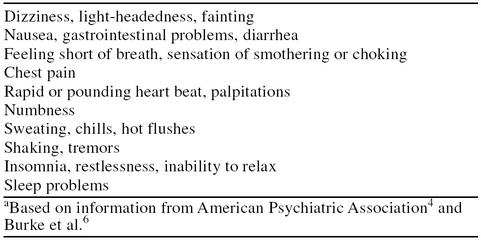
Diagnosing anxiety would be simple if patients told their physicians that they felt anxious or worried all the time or that they consistently feared and avoided certain innocuous objects or situations. Instead, patients with anxiety often consult their primary care physician with one or more distressing physical symptoms, some of which appear to be signs of cardiovascular or other life-threatening illnesses. Table 24,6 lists physical complaints that often accompany anxiety disorders. Many patients are uncomfortable expressing their anxious feelings to a health care professional, preferring to concentrate on physical symptoms, partly because of the stigmas associated with mental illness and psychiatric symptoms.5 Unfortunately, the physician may become sidetracked by numerous and vague symptoms that could indicate dozens of possible medical diagnoses. In addition, physicians are less likely to recognize psychiatric illness if only presented with physical symptoms rather than psychological symptoms—in cases of somatization, one study showed that only 50% of psychiatric illnesses were recognized.9
Table 2.
Physical (Somatic) Signs of Anxietya
However, some specific symptoms can be considered potential markers for anxiety. For example, in one study,10 anxiety was found frequently in patients who had chest pain, fatigue, headache, insomnia, and abdominal pain. In another survey, panic disorder was commonly found in patients who were experiencing chest pain but had no evidence of coronary artery disease.11 The number of different physical symptoms reported by patients may also provide a clue to underlying anxiety. Kroenke and colleagues10 found that whereas anxiety was diagnosed in only 1% of patients who had 1 or no physical complaint and in 7% of those reporting 2 or 3 somatic signs, 48% of patients with 9 or more physical symptoms were found to have anxiety. Anxious patients presenting with physical symptomatology, known as “somatizers,” can be identified by the excessive number of office visits and telephone calls they make to their physicians.5
MANAGEMENT OF ANXIETY DISORDERS IN THE PRIMARY CARE SETTING
Most cases of anxiety are handled, at least initially, in the primary care setting. It has been estimated that 77% of all mental health visits are to primary care physicians.12 Patients with anxious feelings often prefer to visit their family doctor first rather than a psychiatrist,5 and many present to their physician with primarily physical rather than psychological complaints. In managing anxiety disorders, the primary care physician faces several challenges: to detect anxiety disorders in a person complaining of physical ailments, to differentiate an anxiety disorder from a medical problem or substance use that could cause or exacerbate the anxiety, to identify the type of anxiety problem (treatments may differ), and to differentiate anxiety from depression, which coexists with anxiety in the majority of cases.
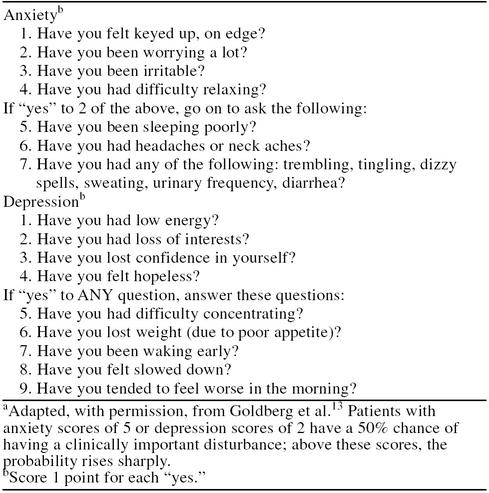
Considering the frequency with which patients with anxiety are seen in the primary care setting, physicians should screen their patients for both anxiety and depressive disorders using simple devices. For example, short questionnaires, such as the one in Table 3, can be given to the patient to complete in the waiting room before the appointment.13 If the results of the questionnaire suggest the possibility of an anxiety disorder, the physician, physician aide, or nurse can investigate further with a more careful dialogue.
Table 3.
Simple Screening Questionnaire for Anxiety and Depressiona
The SWIKIR Anxiety Scale14 (Somatic complaints, Worries, Irritability, Keyed up, Initial insomnia, Relaxation difficulties) evaluates the patient's responses to questions that cover the major signs of anxiety. Patients with 3 or more symptoms may require a more careful evaluation to refine the diagnosis and determine which type of anxiety disorder is present and whether it is accompanied by another problem, such as depression, addictive disorders, or medical problems. Other useful instruments for primary care physicians include the Primary Care Evaluation of Mental Disorders15 and the Well-Being Life Chart.16 The DSM-IV: Primary Care Version offers a convenient algorithm to help physicians identify patients with anxiety and determine the type and possible causes as well.4
The medical interview is the primary means of detecting and determining the principal cause of anxiety in the primary care setting. Physicians should inquire about current symptoms, prior or current medical or psychiatric illnesses, medications and use of anxiety-provoking substances, and stressful events. A physical examination is also needed to rule out medical problems. Findings from the history and physical examination should guide the choice of laboratory or imaging tests. The presence of numerous physical ailments combined with a normal physical examination suggests that a psychiatric illness may be the source of the patient's symptoms. Extensive testing may not be needed or cost-effective.17
In contrast to anxiety, major depression is characterized by a persistent and significant depressed mood, a loss of interest in daily activities, loss of pleasure, sleep problems, feelings of worthlessness, concentration difficulties, loss of initiative, slowed responses, and thoughts of death.4 Depression often accompanies anxiety, and anxiety may be misdiagnosed as depression in the primary care setting.18 The comorbidity of anxiety and depression can make anxious symptoms worse and necessitate more extensive or prolonged treatment than either illness alone.19 Some antidepressants, however, relieve both depressive and anxious symptoms.
Treatment
Anxiety disorders are often treated with anxiolytic or antidepressant medications. In some patients, combining drug and nondrug therapies produces superior results than either form of treatment alone.8
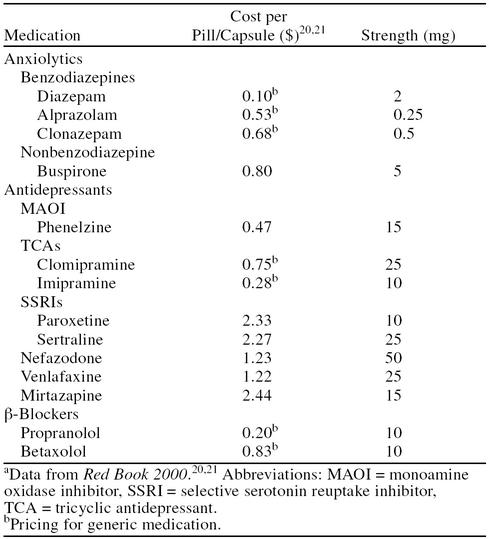
Several classes of drugs relieve the symptoms of anxiety (Table 4).20,21 The benzodiazepines include diazepam, alprazolam, and clonazepam. Benzodiazepines generally work quickly, and are used in the short-term management of acute anxiety, panic disorder, and GAD. However, the side effects of these drugs—particularly sedation, drowsiness, and central nervous system depression—may limit their use in many patients. A physical dependence can also develop with the use of these agents, and patients may experience withdrawal problems, including a recurrence of anxiety, when the drug is tapered.8 Therefore, benzodiazepines are not recommended for long-term treatment unless other treatment options fail.
Table 4.
Medications Used to Treat Anxiety and Anxiety-Depression: Cost of Treatmenta
The monoamine oxidase inhibitors (MAOIs), such as phenelzine, are effective in some patients with anxiety symptoms. However, MAOIs can cause significant adverse reactions when taken with certain foods or with many prescription and over-the-counter medications; these interactions can complicate dosing. β-Blockers have limited use in anxiety, but they have been shown to alleviate somatic symptoms of anxiety and reduce tremor and stage fright in performers and public speakers.22
Buspirone may be as effective as benzodiazepines in reducing anxiety, having a greater effect on the psychic symptoms than on the somatic manifestations.8 This drug causes fewer adverse reactions than the benzodiazepines and has no withdrawal effects.23 Buspirone has a slower onset of action than benzodiazepines and is generally taken twice daily to maintain adequate blood levels. Buspirone does not appear to be useful in panic disorder and may be less effective in patients previously treated with benzodiazepines.23
Tricyclic antidepressants also may be used for anxiety. In particular, clomipramine is approved for the treatment of OCD.24,25 Problems with the tricyclics include cardiovascular side effects, constipation, postural hypotension, urinary retention, and overdose (which can be lethal).7
The selective serotonin reuptake inhibitors (SSRIs) fluoxetine, fluvoxamine, sertraline, citalopram, and paroxetine have both antidepressant and anxiolytic effects. SSRIs are often prescribed for panic disorder, GAD, social phobia, OCD, PTSD, and mixed anxiety and depression.17,26–29
Newer antidepressants are also used for treating anxiety disorders. Venlafaxine has been shown to be effective in the treatment of patients with GAD,30–33 panic disorder,34,35 and social phobia.36 Venlafaxine is generally well tolerated37 and has very few drug-drug interactions.38 Other new antidepressants, such as mirtazapine and nefazodone, have also been used in the treatment of anxiety.39,40
ECONOMIC ASPECTS OF ANXIETY DISORDERS
Despite the high prevalence of anxiety, few studies have attempted to delineate its effects on the total health care budget. Several surveys in the United States and abroad, however, have determined that patients with mental disorders (of which anxiety is the most common) are very high users of the health care system. Anxiety disorders also account for a large percentage of the total costs of mental health care, although the indirect costs (e.g., loss of work, underemployment) dwarf the direct medical costs of managing anxiety illnesses. Prompt detection and successful treatment can help reduce the overall costs of these debilitating disorders to individuals, families, social services, and the health care system.
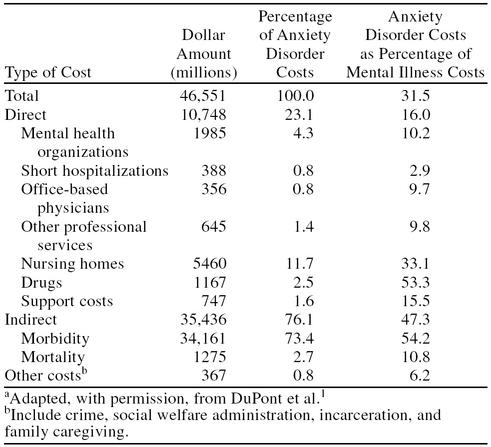
DuPont et al.1 estimated the total economic cost of anxiety disorders using the data set (derived from national surveys) and a cost estimation method developed by Rice41 for use in public and health policy. Core costs were divided into direct costs (medical expenditures) and indirect costs (morbidity and mortality). Cost data for 1985 were adjusted to 1990 dollars to allow for comparison with other studies. The total economic cost in 1990 was estimated to be $46.6 billion; this figure represented 31.5% of the total cost of mental illness in the United States (Table 5).1 Between 1985 and 1990, the expenses related to anxiety increased by 38.3%.1 Direct medical costs (e.g., doctor and hospital visits, medications) accounted for only $10.7 billion. Prescription medications represented 2.5% ($1.2 billion) of the expenses related to anxiety, but they accounted for 53.3% of the drug costs for all mental disorders.1 However, indirect costs accounted for approximately 75% of expenses related to anxiety; these costs included decreased or lost productivity related to the morbidity and mortality of anxiety disorders. Other factors contributing to the total sum included crime and family caregiving (see Table 5).1
Table 5.
Economic Costs of Anxiety Disorders in the United States (calculated for 1990)a
In another survey of expenses related to anxiety, Greenberg et al.42 reported that the total cost in 1990 was approximately $42.3 billion, slightly less than the estimate of $46.6 billion proposed by DuPont et al.1 The Greenberg figure was estimated through the application of multivariate regression techniques to data from the National Comorbidity Survey. The study by DuPont et al.1 also included a category that encompassed expenses due to crime, incarceration, social welfare administration, and family caregiving; this broad category of costs may have contributed to the differences in these estimates.
Although the costs of anxiety are high, much of the expense may actually reflect a lack of diagnosis and effective treatment. Studies that examined the effects of mental illness on usage of the health care system, for example, have documented that patients found to have anxiety disorders consumed a larger share of the health care budget than groups without anxiety. In one study,43 it was detected that over half of the high users of the health care system were “distressed,” as evidenced by either elevated scores on anxiety and depression rating scales or by physician evaluation. This group of “distressed high utilizers” had a lifetime prevalence of GAD of 40.3%, which is nearly 8 times greater than that for the general population.3 The top 10% of health care users, in whom anxiety is prominent, accounted for almost 30% of office visits (vs. 18% in the lowest 50% of users), more than half of outpatient visits to specialists (vs. 7% in the lowest 50% of users), and 48% of hospital days (vs. 9% in the lowest 50% of users).44
This increased usage of the health care system by distressed patients was supported by an analysis of ECA data reporting that about 30% of patients with panic disorder had sought general medical care for substance abuse or emotional problems within the previous 6 months, compared with approximately 4% of persons without an anxiety diagnosis.45 The authors of the study speculated that the physical distresses of panic attacks (heart and respiratory problems) are very likely to prompt a patient to seek medical help.45
A French study46 focused on the costs incurred by patients who had GAD and comorbid medical illnesses (primarily gynecologic and gastrointestinal disorders) or mental disorders (addictive disorders and depression) versus those incurred by GAD patients without comorbidities. Patients with comorbid disorders experienced more severe psychic symptoms and had significantly more emergency department visits, hospitalizations, visits to internal medicine physicians, specialist (but not psychiatrist) consultations, laboratory testing, cardiovascular tests, and imaging techniques. Patients with comorbid disorders also used more medications.46
Another study47 also demonstrated the high cost burden of patients with mental disorders on the health care system. Patients found to have an anxiety disorder or a depressive disorder meeting DSM-III-R criteria had higher medical care costs ($2390) in a 6-month period than patients with anxiety-like disorders who did not meet DSM-III-R criteria ($1098) and those with no anxiety or depression ($1397). In addition, 1 year after diagnosis of mental disorders in this group, health care costs did not decrease. The differences between the groups reflected a higher use of general medical care—not increased mental health care—even after psychiatric diagnosis. However, less than half of the high users with the psychiatric diagnoses sought mental health care or filled prescriptions for antidepressant medications in the 3-month period after diagnosis.47 These data suggest that the burden on the health care system related to anxiety and depression may decrease only when proper diagnosis is accompanied by active and appropriate treatment. Proper treatment is likely to reduce both direct health care costs and indirect costs related to productivity.1 Other investigators, noting the common lifetime prevalence of substance abuse in patients with anxiety, further proposed that treating anxiety disorders early and effectively might (preventively) reduce the prevalence and risk of alcoholism and other addictive disorders.48
These studies confirm that anxiety disorders lead to the excessive use of the health care system and that the severity of symptoms and the presence of comorbid disorders contribute to the overall high health care expenses associated with anxiety. It is probable that prompt recognition of anxiety by the primary care physician, plus the alleviation or elimination of symptoms, can help reduce the number of repeat office visits, diagnostic procedures, emergency department visits for anxiety-related symptoms, unsuccessful medical treatment, hospitalizations, substance abuse, and lost productivity. Prompt recognition of an underlying psychiatric condition also allows for timely referrals to trained clinical psychologists or psychiatrists, since some form of psychotherapy is usually indicated. Therefore, any discussion of the costs of treating anxiety disorders in the primary care setting must consider the real costs of untreated anxiety.
Anxiety disorders may significantly hinder a person's ability to earn a living and support a family and may be correlated with suicide.1,49,50 Persons suffering from anxiety are more likely to be unemployed,1 to receive disability payments, and to require welfare and other types of financial assistance than those without anxiety disorders.45 Anxiety also diminishes quality of life, including social and marital functioning.49 As expensive as the direct costs of anxiety disorders are, they are overshadowed by the indirect costs to the individual, family, and society. Indirect costs accounted for 76.1% of the total costs of anxiety (see Table 5) and encompassed the effects of illness (morbidity) and early death (mortality) on productivity and earnings.1 For 1990, the indirect costs of anxiety morbidity totaled $34.2 billion. Mortality (primarily suicide) led to economic losses of about $1.3 billion.1
REDUCING THE BURDEN ON THE HEALTH CARE SYSTEM
Anxiety disorders impose an enormous burden on the health care system and society, but it appears that much of the related costs are due to a lack of effective diagnosis. These debilitating disorders can be treated successfully and safely, often in the primary care setting, potentially reducing morbidity and mortality, economic costs, and human suffering. The challenges for health care practitioners are to accurately diagnose anxiety disorders early and then prescribe the appropriate therapy.
Making an Appropriate and Early Diagnosis
Anxiety disorders often are not diagnosed or are misdiagnosed as depression or somatic disorders. The reasons for these failures are numerous: patients rarely make an appointment to discuss their anxious feelings with a doctor; they may not recognize their feelings or may be embarrassed by them, or they may believe that anxiety and stress are normal responses to life circumstances. These patients are more likely to present with nausea, pain, headaches, and symptoms of heart disease—physical signs which they expect a physician will consider legitimate medical concerns. Physicians also may automatically manage physical symptoms, which they can evaluate and test objectively.
Therefore, to detect anxiety disorders promptly and accurately, primary care physicians first need to have a high degree of suspicion. As mentioned earlier, physicians should consider the possibility of a psychiatric source when patients present with multiple symptoms and when the symptoms appear to have no physical cause. Some researchers propose that primary care physicians should routinely screen their patients for psychiatric disorders with questionnaires (see Table 3)13 or careful questioning. The early recognition of the common physical and psychological signs of anxiety can help avoid time-consuming, expensive, and unnecessary testing to determine the cause of physical symptoms.
Prescribing Appropriate Therapy
Many types of medications are available to treat anxiety, but they are not all effective for all types of anxiety. Physicians must consider several factors when choosing the appropriate drug: the type of anxiety; the presence of comorbid conditions, especially depression; the patient's age and general medical condition; the severity of symptoms; the use of alcohol or other depressants; and the side effects of and risk for drug-drug interactions associated with the agent.
Ideally, patients with both anxiety and depression should be prescribed a medication proven effective as both an antidepressant and anxiolytic. SSRIs and venlafaxine extended release (XR) are antidepressants also effective in treating anxiety and specific anxiety disorders such as OCD (fluoxetine and paroxetine), social phobia (paroxetine), PTSD (sertraline), panic disorder (paroxetine and sertraline), and GAD (venlafaxine XR and paroxetine).30–33,51–53 Patients with heart disease may be adversely affected by medications that have unwanted cardiovascular effects. Drugs that cause drowsiness or impair thinking, concentration, and balance (e.g., benzodiazepines) may be inappropriate for the elderly and anyone who has to drive a motor vehicle or maintain alertness. Benzodiazepines are not usually considered optimal for long-term therapy because of dependence, although in some instances they are necessary to maintain clinical response. Patients taking medications for other disorders should use anxiety-relieving agents that have insignificant drug-drug interactions; persons who regularly drink alcohol or who have a substance abuse problem should not be prescribed agents that increase the effects of alcohol or other drugs. Patients who experience compliance problems may benefit from agents requiring infrequent dosing. Choosing the most appropriate medication early in treatment can help avoid needless repeat office visits and the frustration associated with trying different drugs and may ultimately reduce the need for short-term hospitalizations.
Implications for Managed Care
While it has been shown that the overall costs of anxiety disorders are significant, much of this expense is due to a lack of correct diagnosis and a consequent undertreatment of the disease. In general, psychiatric illness is often unrecognized in the primary care setting. One reason for this is that the patient typically presents with somatic complaints, leading to a misdiagnosis of the underlying psychiatric problem. Because psychiatric disorders are prevalent and are often managed initially in the primary care setting, detection of them by the physician is important. Time constraints, however, are a key issue, and new, shorter procedures to quickly screen for mental disorders in a primary care setting should aid the busy physician in diagnosis. Third-party reimbursement for the time spent performing mental health evaluations by nonpsychiatrists is also an issue in a managed care setting. The economic analysis of anxiety disorders strongly suggests that prompt diagnosis and effective treatment will reduce the overall financial cost of anxiety disorders. Once a diagnosis has been made, strategies for the successful treatment of anxiety disorders combine both pharmacotherapy and nondrug therapies for long-term management.
CONCLUSION
Anxiety disorders are very common, causing emotional distress and social dysfunction, as well as numerous physical complaints. Despite their prevalence, anxiety disorders are often missed or misdiagnosed because their common presenting manifestations—such as chest pain, breathing problems, insomnia, and chronic pain—mimic many common medical disorders. In addition, coexisting depressive illness or substance abuse frequently complicates anxiety. Physicians should consider anxiety as a possible source whenever patients present with numerous nonspecific symptoms or ailments that do not appear to have a physical basis.
Drug treatment can effectively relieve the symptoms of anxiety. The cost-effective approach to treating anxiety includes early diagnosis and treatment with appropriate screening and medication. Early treatment may reduce the number of office and emergency department visits and unnecessary diagnostic procedures, help avoid unsuccessful treatments of somatic complaints that are due to underlying psychological problems, and prevent the development of comorbid depression or substance abuse. Actively addressing the anxiety disorder also helps patients cope with life stresses and remain employed and functioning within their families and communities. Clearly, the medical expenses of treating anxiety disorders pale in comparison to the medical, social, and personal costs of not treating these common and debilitating disorders.
Drug names: alprazolam (Xanax and others), buspirone (BuSpar), citalopram (Celexa), clonazepam (Klonopin and others), clomipramine (Anafranil and others), diazepam (Valium and others), fluoxetine (Prozac), fluvoxamine (Luvox), mirtazapine (Remeron), nefazodone (Serzone), paroxetine (Paxil), phenelzine (Nardil), propranolol (Inderal and others), sertraline (Zoloft), venlafaxine (Effexor).
Footnotes
Supported by an unrestricted grant from Wyeth-Ayerst Laboratories, Philadelphia, Pa.
REFERENCES
- DuPont RL, Rice DP, Miller LS, et al. Economic costs of anxiety disorders. Anxiety. 1996;2:167–172. doi: 10.1002/(SICI)1522-7154(1996)2:4<167::AID-ANXI2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Anxiety algorithm. In: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Primary Care Version: DSM-IV-PC. Washington, DC: American Psychiatric Association. 1995 47–63. [Google Scholar]
- Hales RE, Hilty DA, Wise MG. A treatment algorithm for the management of anxiety in primary care practice. J Clin Psychiatry. 1997;58(suppl 3):76–80. [PubMed] [Google Scholar]
- Burke WJ, Folks DG, McNeilly DP. Effective use of anxiolytics in older adults. Clin Geriatr Med. 1998;14:47–65. [PubMed] [Google Scholar]
- Martin LM, Fleming KC, Evans JM. Recognition and management of anxiety and depression in elderly patients. Mayo Clin Proc. 1995;70:999–1006. doi: 10.4065/70.10.999. [DOI] [PubMed] [Google Scholar]
- Schweizer E, Rickels K. Strategies for treatment of generalized anxiety in the primary care setting. J Clin Psychiatry. 1997;58(suppl 3):27–33. [PubMed] [Google Scholar]
- Bridges KW, Goldberg DP. Somatic presentation of DSM-III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, et al. Physical symptoms in primary care: predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- Beitman BD, Basha I, Flaker G, et al. Atypical or nonanginal chest pain: panic disorder or coronary artery disease? Arch Intern Med. 1987;147:1548–1552. [PubMed] [Google Scholar]
- Schurman RA, Kramer PD, Mitchell JB. The hidden mental health network: treatment of mental illness by nonpsychiatrist physicians. Arch Gen Psychiatry. 1985;42:89–94. doi: 10.1001/archpsyc.1985.01790240091010. [DOI] [PubMed] [Google Scholar]
- Goldberg D, Bridges K, Duncan-Jones P, et al. Detecting anxiety and depression in general medical settings. BMJ. 1988;297:897–899. doi: 10.1136/bmj.297.6653.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baughman OL III. Rapid diagnosis and treatment of anxiety and depression in primary care: the somatizing patient. J Fam Pract. 1994;39:373–378. [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 Study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- Zajecka J. Importance of establishing the diagnosis of persistent anxiety. J Clin Psychiatry. 1997;58(suppl 3):9–13. [PubMed] [Google Scholar]
- Goldberg RJ. Diagnostic dilemmas presented by patients with anxiety and depression. Am J Med. 1995;98:278–284. doi: 10.1016/S0002-9343(99)80375-1. [DOI] [PubMed] [Google Scholar]
- Nisenson LG, Pepper CM, Schwenk TL, et al. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. 1998;20:21–28. doi: 10.1016/s0163-8343(97)00096-0. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, et al. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry. 1996;153:1293–1300. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Red Book 2000. Montvale, NJ: Medical Economics. 2000. [Google Scholar]
- Red Book Update 2000, vol 19, no. 6. Montvale, NJ: Medical Economics. 2000. [Google Scholar]
- Nutt DJ. The pharmacology of human anxiety. Pharmacol Ther. 1990;47:233–266. doi: 10.1016/0163-7258(90)90089-k. [DOI] [PubMed] [Google Scholar]
- Sussman N. The uses of buspirone in psychiatry. J Clin Psychiatry Monograph. 1994;12(1):3–19. [Google Scholar]
- Clomipramine Collaborative Study Group. Clomipramine in the treatment of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1991;48:730–738. doi: 10.1001/archpsyc.1991.01810320054008. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR, Fryer AJ, Gorman JM, et al. Tricyclic therapy of the DSM-III anxiety disorders: a review with implications for further research. J Psychiatr Res. 1988;22(suppl 1):7–31. doi: 10.1016/0022-3956(88)90067-2. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K. The role of SSRIs in panic disorder. J Clin Psychiatry. 1996;57(suppl 10):51–58. [PubMed] [Google Scholar]
- Rocca P, Fonzo V, Scotta M, et al. Paroxetine efficacy in the treatment of generalized anxiety disorder. Acta Psychiatr Scand. 1997;95:444–450. doi: 10.1111/j.1600-0447.1997.tb09660.x. [DOI] [PubMed] [Google Scholar]
- Jefferson JW. Antidepressants in panic disorder. J Clin Psychiatry. 1997;58(suppl 2):20–25. [PubMed] [Google Scholar]
- Katzelnick DJ, Kobak KA, Greist JH, et al. Sertraline for social phobia: a double-blind, placebo-controlled crossover study. Am J Psychiatry. 1995;152:1368–1371. doi: 10.1176/ajp.152.9.1368. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, DuPont RL, Hedges D, et al. Efficacy, safety, and tolerability of venlafaxine extended release and buspirone in outpatients with generalized anxiety disorder. J Clin Psychiatry. 1999;60:528–535. doi: 10.4088/jcp.v60n0805. [DOI] [PubMed] [Google Scholar]
- Gelenberg AJ, Lydiard RB, Rudolph RL, et al. Efficacy of venlafaxine extended-release capsules in nondepressed outpatinets with generalized anxiety disorder: a 6-month randomized controlled trial. JAMA. 2000;283:3082–3088. doi: 10.1001/jama.283.23.3082. [DOI] [PubMed] [Google Scholar]
- Rickels K, Pollack MH, Sheehan DV, et al. Efficacy of extended-release venlafaxine in nondepressed outpatients with generalized anxiety disorder. Am J Psychiatry. 2000;157:968–974. doi: 10.1176/appi.ajp.157.6.968. [DOI] [PubMed] [Google Scholar]
- Allgulander C, Hackett D, Salinas E. Venlafaxine extended release (ER) in the treatment of generalised anxiety disorder: twenty-four-week placebo-controlled dose-ranging study. Br J Psychiatry. 2001;179:15–22. doi: 10.1192/bjp.179.1.15. [DOI] [PubMed] [Google Scholar]
- Geracioti TD Jr. Venlafaxine treatment of panic disorder: a case series. J Clin Psychiatry. 1995;56:408–410. [PubMed] [Google Scholar]
- Papp LA, Sinha SS, Martinez JM, et al. Low-dose venlafaxine treatment in panic disorder. Psychopharmacol Bull. 1997;34:207–209. [PubMed] [Google Scholar]
- Kelsey JE. Venlafaxine in social phobia. Psychopharmacol Bull. 1995;31:767–771. [PubMed] [Google Scholar]
- Thase ME. Efficacy and tolerability of once-daily venlafaxine extended release (XR) in outpatients with major depression. J Clin Psychiatry. 1997;58:393–398. doi: 10.4088/jcp.v58n0904. [DOI] [PubMed] [Google Scholar]
- Ereshefsky L. Drug-drug interactions involving antidepressants: focus on venlafaxine. J Clin Psychopharmacol. 1996;16(3 suppl 2):37S–53S. doi: 10.1097/00004714-199606002-00009. [DOI] [PubMed] [Google Scholar]
- Hedges DW, Reimherr FW, Strong RE, et al. An open trial of nefazodone in adult patients with generalized anxiety disorder. Psychopharmacol Bull. 1996;32:671–676. [PubMed] [Google Scholar]
- Fawcett J, Barkin RL. A meta-analysis of eight randomized, double-blind, controlled clinical trials of mirtazapine for the treatment of patients with major depression and symptoms of anxiety. J Clin Psychiatry. 1998;59:123–127. [PubMed] [Google Scholar]
- Rice DP, Kelman S, Miller LS, and et al. The Economic Costs of Alcohol and Drug Abuse and Mental Illness. Rockville, Md: US Dept Health Human Services. 1990 Report no. (ADM) 90-1694. [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, et al. Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- Katon W. Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J Clin Psychiatry. 1996;57(suppl 10):11–18. [PubMed] [Google Scholar]
- Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. Br J Psychiatry. 1995;166(suppl 27):19–22. [PubMed] [Google Scholar]
- Souêtre E, Lozet H, Cimarosti I, et al. Cost of anxiety disorders: impact of comorbidity. J Psychosom Res. 1994;38(suppl 1):151–160. doi: 10.1016/0022-3999(94)90145-7. [DOI] [PubMed] [Google Scholar]
- Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152:352–357. doi: 10.1176/ajp.152.3.352. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Price RH. Primary prevention of secondary disorders: a proposal and agenda. Am J Community Psychol. 1993;21:607–633. doi: 10.1007/BF00942174. [DOI] [PubMed] [Google Scholar]
- Markowitz JS, Weissman MM, Ouellette R, et al. Quality of life in panic disorder. Arch Gen Psychiatry. 1989;46:984–992. doi: 10.1001/archpsyc.1989.01810110026004. [DOI] [PubMed] [Google Scholar]
- Rice DP, Miller LS. Health economics and cost implications of anxiety and other mental disorders in the United States. Br J Psychiatry. 1998;173(suppl 34):4–9. [PubMed] [Google Scholar]
- Prozac (fluoxetine hydrochloride). Physicians' Desk Reference. 55th ed. Montvale, NJ: Medical Economics Co. 2001 1127–1132. [Google Scholar]
- Paxil (paroxetine). Physicians' Desk Reference. 55th ed. Montvale, NJ: Medical Economics Co. 2001 3114–3120. [Google Scholar]
- Pollack MH, Zaninelli R, Goddard A, et al. Paroxetine in the treatment of generalized anxiety disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62:350–357. doi: 10.4088/jcp.v62n0508. [DOI] [PubMed] [Google Scholar]