Abstract
Background: Depressive and anxiety disorders commonly occur together in patients presenting in the primary care setting. Although recognition of individual depressive and anxiety disorders has increased substantially in the past decade, recognition of comorbidity still lags. The current report reviews the epidemiology, clinical implications, and management of comorbidity in the primary care setting.
Method: Literature was reviewed by 2 methods: (1) a MEDLINE search (1980–2001) using the key words depression, depressive disorders, and anxiety disorders; comorbidity was also searched with individual anxiety diagnoses; and (2) direct search of psychiatry, primary care, and internal medicine journals over the past 5 years.
Results: Between 10% and 20% of adults in any given 12-month period will visit their primary care physician during an anxiety or depressive disorder episode (although typically for a nonpsychiatric complaint); more than 50% of these patients suffer from a comorbid second depressive or anxiety disorder. The presence of depressive/anxiety comorbidity substantially increases medical utilization and is associated with greater chronicity, slower recovery, increased rates of recurrence, and greater psychosocial disability. Typically, long-term treatment is indicated, although far less research is available to guide treatment decisions. Selective serotonin reuptake inhibitor antidepressants are the preferred treatment based on efficacy, safety, and tolerability criteria. Knowledge of their differential clinical and pharmacokinetic profiles can assist in optimizing treatment.
Conclusion: Increased recognition of the high prevalence and negative psychosocial impact of depression and anxiety disorder comorbidity will lead to more effective treatment. While it is hoped that early and effective intervention will yield long-term benefits, research is needed to confirm this.
Depression and anxiety frequently co-occur, especially in primary care settings. These co-occurrences manifest themselves in several ways and have different clinical courses. This review was written to help the clinician to identify what is and is not important in the diagnosis and treatment of patients with comorbid depression and anxiety in the primary care setting. The scope of this review is limited to major depression and not other forms of depression such as bipolar depression or dysthymic disorder. Literature was reviewed by 2 methods: (1) a MEDLINE search (1980–2001) using key words depression, depressive disorders, and anxiety disorders; comorbidity was also searched with individual anxiety diagnoses; and (2) direct search of psychiatry, primary care, and internal medicine journals over the past 5 years.
The scope and impact of depression and anxiety disorders worldwide are overwhelming. The watershed Global Burden of Disease study found that major depression ranked fourth among all medical illnesses in terms of its disabling impact on the world population.1,2 The authors estimated that by the year 2020 depression would be second only to ischemic heart disease. Anxiety disorders rank close behind major depression, contributing additional disability.
The prevalence of depressive and anxiety disorders in primary care settings is high. Between 10% and 20% of adults in any given 12-month period will visit their primary care physician during an episode of mental illness (although frequently not because of the episode).3 Depression and anxiety disorders contribute to the majority of those visits. If unrecognized and undiagnosed, depression and anxiety disorders contribute to high medical utilization in the primary care setting. Twenty-four percent of high utilizers (the top 10%) have been found to suffer from current major depression and 22%, from an anxiety disorder.4
In primary care, presenting complaints for behavioral problems are more likely to be somatic than psychological. Back pain, chest pain, shortness of breath, heart palpitations, problems with sleep or appetite, and fatigue are among the most frequent presenting symptoms.
Although much work still needs to be done to increase awareness of depression and anxiety, the last decade has witnessed enormous progress in both the recognition and management of these disorders, especially in the primary care setting, which has long been recognized as the “hidden mental health network.”5,6 Since the introduction of the selective serotonin reuptake inhibitors (SSRIs), recognition and appropriate treatment of major depression have risen from an estimated rate of less than 5%7 to a rate that exceeds 50%.8 Appropriate diagnosis and treatment of anxiety disorders still lag far behind, and comorbidity is one of the chief reasons that anxiety disorders go unrecognized and untreated. The following case history illustrates a common presentation.
Case history. A 45-year-old married, working mother of 2 sons (aged 9 and 11 years) presents to her family physician complaining of persistent lower back pain that she says is bothering her during the day and causing her to lose sleep at night. She says she is no longer able to keep up with her housework and wants something to give her relief. Physical examination reveals mild point tenderness in the lumbar area, but with an otherwise completely normal neurologic examination, including no sciatica. On interview, the patient reports being increasingly worried and preoccupied with how her family will be able to afford college expenses for her sons. The worries have begun to include concerns about her children's health and whether her family can keep their heads above water financially. Her worries impede her sleep, and she even finds it difficult to concentrate enough to read detective novels, which she has always loved and read avidly. The patient says she has become increasingly tense and irritable in the past 8 months—frequently snapping at her husband and children, then feeling intensely guilty for hours, often breaking down and crying, feeling she is a bad wife and mother. She is no longer interested in sex. Lately, the patient admits that she does not really care that much about anything—she has lost all of her interests.
MAJOR DEPRESSION AND ANXIETY COMORBIDITY: 4 CLINICAL PRESENTATIONS
The case history summarized above illustrates some of the difficulties faced by a physician in the primary care setting in recognizing and diagnosing comorbid anxiety and depressive disorders. First, the patient frequently presents with a somatic complaint; second, the symptoms of anxiety and depression are typically intermingled with real-life problems; and third, the patient often has little or no insight into the psychological issues. The dilemma of diagnosis, therefore, lies in maintaining an appropriate index of suspicion for the presence of an anxiety or depression diagnosis amid the constant background flow of somatic complaints. An index of suspicion and a familiarity with common patterns of anxiety and depression comorbidity are crucial to the appropriate recognition and treatment of these disorders in the primary care setting.
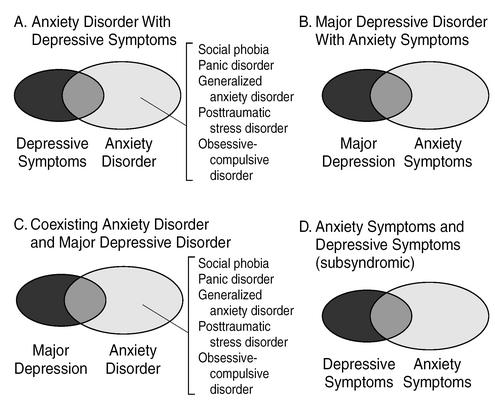
Comorbid major depression and anxiety typically present as 1 of 4 clinical combinations (Figure 1). The patient may meet criteria for an anxiety disorder diagnosis, but suffer from only subsyndromal levels of depression symptoms (see Figure 1, panel A). Alternatively, a patient may meet criteria for major depression, but suffer from only subsyndromal levels of anxiety symptoms (panel B). Thirdly, a patient may present with a full-fledged diagnosis of both an anxiety disorder and major depression (panel C). Finally, a patient may present with symptoms of both anxiety and depression, neither of which is severe enough to meet criteria for a diagnosis (panel D). This latter presentation is referred to as “mixed anxiety-depression.” Surveys of patients in primary care have reported the prevalence of mixed anxiety-depression to be in the range of 1% to 5%.9,10 These symptomatic but subsyndromal patients have been found to have a level of disability that is closer to that of patients who meet full diagnostic criteria for major depressive disorder or an anxiety disorder than to that of patients reporting no anxious-depressive symptomatology.9 The few studies that have prospectively followed these patients report that approximately 1 in 5 will develop a full-blown major depression within the next 12 months.9,11,12
Figure 1.
Depression and Anxiety Comorbidity: 4 Common Clinical Presentations
THE EPIDEMIOLOGY OF COMORBIDITY
In the past decade, large surveys conducted both in the community and in the primary care setting have established one simple but clinically important fact: depression that is not complicated by comorbidity is the exception, not the rule.
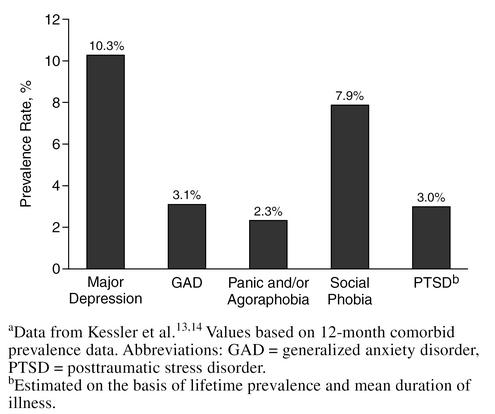
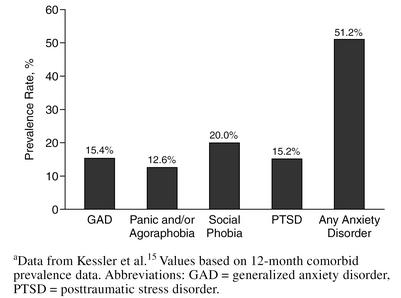
Figure 2 shows the prevalence rates in the community, in any given 12-month period, of individual depression and anxiety disorders. These data confirm that depression and anxiety disorders occur at rates that exceed other common medical illnesses such as hypertension, diabetes, or asthma. Among patients in the community who meet criteria for major depression, approximately 50% are also suffering from an anxiety disorder (Figure 3).
Figure 2.
Prevalence of Major Depression and Anxiety Disorders in the Communitya
Figure 3.
Percentage of Patients With Major Depression Who Also Suffer From a Current Anxiety Disordera
The results shown in Figure 3 are from epidemiologic surveys conducted in the community. But what is the likelihood that a patient who presents in the primary care setting with major depression or an anxiety disorder will also be suffering from a second depressive/anxiety disorder? Large primary care surveys suggest that such comorbidity is even higher in primary care than in the community.10,16 Overall, more than 75% of patients diagnosed with depression in a primary care setting suffer from a current anxiety disorder.16
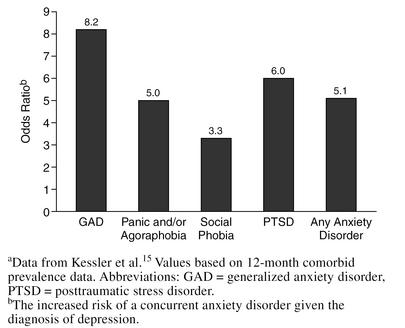
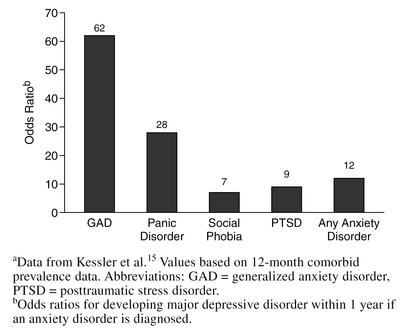
Calculation of odds ratios is a useful method of estimating the likelihood of having a second, concurrent diagnosis given the presence of depression and/or an anxiety disorder. In someone diagnosed with major depression, there is a 3.3-fold to 8.2-fold increased likelihood that the patient is also suffering from a comorbid anxiety disorder (Figure 4).15 Conversely, if a patient carries an anxiety disorder diagnosis, there is very high likelihood (odds ratios from 7 to 62) that the patient will develop major depression within the following year (Figure 5). These data help to quantify the level of diagnostic awareness that a physician must maintain. Given such high odds ratios, it should be routine clinical practice to screen for the presence of major depression given the presence of an anxiety disorder and vice versa.
Figure 4.
Likelihood That a Concurrent Anxiety Disorder Is Also Present in Patients Diagnosed With Major Depressiona
Figure 5.
Likelihood of Developing Major Depressive Disorder Within 1 Year in Patients Diagnosed With an Anxiety Disordera
Put another way, the presence of an anxiety disorder is the single biggest clinical risk for the development of depression. A common scenario appears to be the following: exposure to significant life stressors such as interpersonal conflict, some type of personal loss, or some type of life threat leads to clinical levels of anxiety.17–20 The experience of anxiety may, in turn, serve as a compounding stressor that facilitates further decompensation, leading (especially in patients with a genetic/familial diathesis) to major depression. Time-series analyses21 confirm that the new onset of an anxiety disorder puts a patient at significant increased risk of developing major depression in the ensuing year. This risk is extremely high (more than 20-fold) in the case of panic disorder and generalized anxiety disorder (GAD). The risk levels off after the first year, but continues to persist as a 2-fold or greater risk for many years after that.
WHAT ARE THE CONSEQUENCES OF COMORBIDITY?
Patients who have depression and anxiety comorbidity have higher severity of illness, higher chronicity, and significantly greater impairment in work functioning, psychosocial functioning, and quality of life than patients not suffering from comorbidity.16,17,21,22
One of the most important clinical reasons to screen for comorbidity is that unrecognized depression/anxiety comorbidity is associated with an increased rate of psychiatric hospitalization21 and an increased rate of suicide attempts.23,24 For example, suicide attempt rates are 70% higher in patients with comorbid major depression and panic disorder than in those with major depression alone and more than 4 times higher than in patients suffering from uncomplicated panic disorder.24 Among anxiety disorders, posttraumatic stress disorder (PTSD) has the highest rate of comorbid psychiatric disorders, including alcohol abuse. Comorbid depression and anxiety have also been shown to significantly increase the suicide attempt risk above what is contributed by major depression alone.21 The results of a large national survey found that anxiety comorbidity was associated with a 2.5-fold increased likelihood of hospitalization, with patients suffering from concurrent panic disorder being most at risk (odds ratio = 3.2).21
The presence of comorbidity increases the chronicity of each disorder, slows recovery, and increases the likelihood of a recurrence once the patient has recovered.17,21,22,25 As will be discussed in a later section, the chronicity/recurrence risk associated with comorbidity often requires that the patient be treated for a longer time with medication. Such patients must be educated about the early warning signs of these highly recurrent disorders.
SCREENING FOR DEPRESSION AND ANXIETY: THE PRIME-MD
The presence of an anxiety disorder may serve to mask the presence of depression and vice versa. This is partly due to the overlap of symptoms in these disorders. For example, insomnia and loss of appetite may be symptoms of both illnesses. Incomplete diagnosis may be due to the assumption that once the first diagnosis has been made, one's diagnostic work is accomplished. As noted previously, all of the available epidemiologic data suggest that the presence of one disorder significantly increases the likelihood that the other disorder may also be present.
Relatively few scales are available that screen for depression and anxiety and have been validated in the primary care setting.26 Scales meeting these criteria include the Primary Care Evaluation of Mental Disorders (PRIME-MD),27 the Symptom Driven Diagnostic System for Primary Care (SDDS-PC),28 and the Center for Epidemiologic Studies Depression Scale (CES-D).29 The CES-D is a subscale of a larger, population-based research screening tool, the General Health Questionnaire (GHQ).
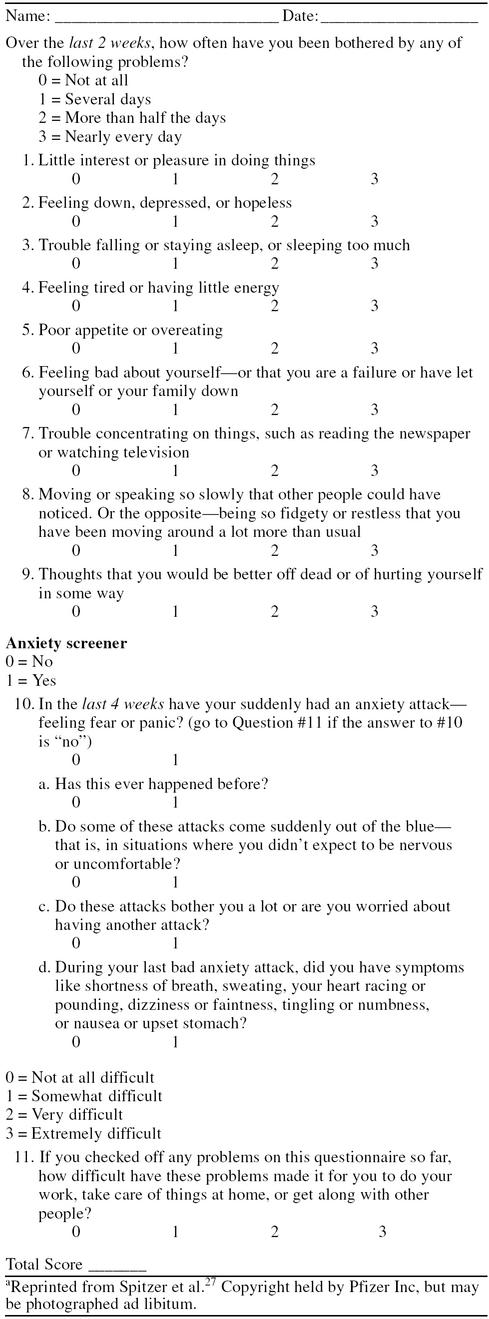
Table 1 gives the depression and anxiety screening questions from the Patient Health Questionnaire (PHQ), the patient-rated module of the PRIME-MD. The positive predictive value of the PRIME-MD for detecting major depression and anxiety disorders in the primary care setting is above 90%. Setting the threshold score higher yields increased diagnostic specificity, but lowers the sensitivity (i.e., more cases are missed).30 For example, a score of 9 on the first 9 items, which screen for depression, is associated with a diagnostic sensitivity of 95% and a specificity of 84%, while a score of 12 is associated with a sensitivity of 83% and a specificity of 92%. While screening is no substitute for diagnosis, it can serve to identify, to a high probability, which patients are likely to have a diagnosis.
Table 1.
Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire Screenera
THE MASKING EFFECT OF MEDICAL COMORBIDITY
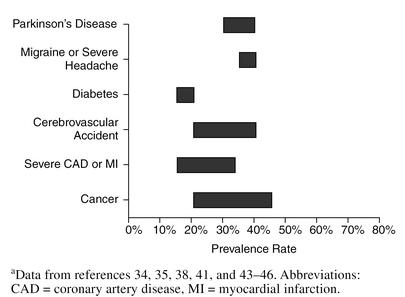
The depression/anxiety comorbidity story would not be complete without emphasizing the additional complication of general medical comorbidity. Patients in primary care who have a depression or anxiety disorder diagnosis report an average of 2 to 3 concurrent chronic medical illnesses, a rate that is more than double that reported by patients who do not suffer from depression or anxiety.31 Conversely, patients with diagnosed general medical illnesses, especially chronic conditions, are at significantly increased risk for developing depression and/or anxiety disorders. Studies indicate that 20% to 50% of patients with many common medical illnesses will develop depression (see Figure 6 for examples).32–46 The rates for anxiety disorders are similarly high.
Figure 6.
Rates of Depression in Patients With Medical Illnessa
Despite these high rates of concurrent illness, the presence of a primary general medical diagnosis markedly reduces the detection rate of depression and anxiety disorders: only 1 of every 5 patients who present with depression or anxiety and medical comorbidity receive appropriate treatment for their psychiatric illness.27 This low detection rate is unfortunate because more than 80% of these patients, in any given year, will visit their primary care physicians. In contrast, less than 2% will see a psychiatrist or other mental health specialist without having first visited their primary care physician.27
The consequences of unrecognized anxiety and depressive disorders are many, including a significant increase in the utilization of medical services, as well as increased rates of disability given equivalent levels of medical illness severity.4,47 In addition, unrecognized anxiety or depressive comorbidity has been shown to lead to a 3-fold increased likelihood of nonadherence to treatment.48 For example, among diabetics, the presence of major depression is associated with significantly poorer glycemic control.49
Depression appears to represent an especially important risk factor for the development of some types of general medical illness, most notably vascular disease. Longitudinal data on elderly hypertensive patients suggest that for every 5-point increase in score on the CES-D, there is an 18% increase in the risk of myocardial infarction (MI) or stroke and a 25% increase in overall mortality.50 The prevalence rate of major depression following an MI is 20%. Additionally, depression that develops post-MI is associated with a significantly increased risk of subsequent MI and death, with adjusted odds ratios for the latter in the range of 4 to 6.34,51,52 It is still an open question as to whether aggressive early treatment of depression in the immediate post-MI period will lead to more favorable outcomes, including improved functioning and quality of life and reduced mortality. Preliminary research suggests that early treatment intervention may be both safe and efficacious.53
MOOD/ANXIETY DISORDER COMORBIDITY: PHARMACOLOGIC TREATMENT
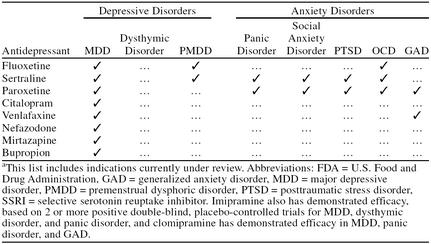
SSRIs have become the first-line treatment for both major depression and the anxiety disorders. Table 2 summarizes the diagnoses for which the SSRIs and other new generation antidepressants have U.S. Food and Drug Administration FDA)–approved indications. As can be seen, paroxetine and sertraline represent the most broad-spectrum antidepressants in terms of the range of anxiety disorders for which efficacy has been established. Paroxetine has recently shown positive results for PTSD and GAD,54,55 while double-blind studies of sertraline in GAD are currently underway.
Table 2.
FDA-Approved Indications for SSRIs and Atypical Antidepressantsa
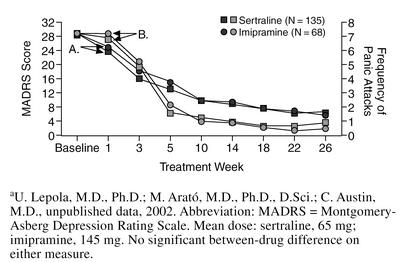
Because of the relative lack of treatment research on comorbidity, no medication to date has been approved by the FDA for the treatment of comorbid major depressive disorder and an anxiety disorder (Figure 1, panel C). However, there are controlled studies of sertraline in the treatment of major depression and comorbid panic disorder (U. Lepola, M.D., Ph.D.; M. Arató, M.D., Ph.D., D.Sci.; C. Austin, M.D., unpublished data, 2002), OCD,56 and PTSD.57,58 In addition, results of a study of venlafaxine for the treatment of major depression and GAD have recently been reported.59
The question at hand is, If an antidepressant has demonstrated efficacy in each disorder individually, is that result sufficient to ensure efficacy in both disorders when they occur comorbidly? The answer to this is unclear. While we may be inclined to accept such indirect evidence of efficacy, it is no substitute for actual controlled trials.
There are several reasons why clinical trials in patients with comorbid depression and anxiety are vital and why direct evidence of efficacy is important for appropriate treatment. It is possible that the antidepressant simply may not work as well in patients with combined anxiety and depression. For example, there is ample evidence that imipramine is effective for the treatment of both major depression and panic disorder.60,61 Yet the first study ever conducted that evaluated its efficacy in the treatment of comorbid depression and panic disorder did not confirm its efficacy in both disorders.62 Direct study of efficacy in patients with comorbidity is also important because the dose requirements, the time to response, and the minimally effective duration of acute treatment may all be different. In addition, information is needed on when, and to what extent, there may be a discordance between the response of one or the other comorbid disorder and how to effectively treat patients in whom one disorder has responded, but the other has not.
Figure 7 illustrates the efficacy results from one of the few available comorbidity studies (U. Lepola, M.D., Ph.D.; M. Arató, M.D., Ph.D., D.Sci.; C. Austin, M.D., unpublished data, 2002). Both sertraline and imipramine demonstrated equivalent efficacy in the treatment of both panic disorder and major depression. Approximately 1 of 4 patients discontinued imipramine due to side effects, while only half that number (12%) discontinued sertraline due to side effects (p < .05). Interestingly, 40% of the patients who discontinued each drug were responders at the time of discontinuation. These patients are at significantly greater risk of relapse and represent one of the chief clinical challenges in the treatment of comorbidity: the long-term treatment.
Figure 7.
Time Course of Improvement in (A) MADRS Score and (B) Panic Attack Frequency During 26 Weeks of Treatment of Concurrent Panic Disorder and Major Depressiona
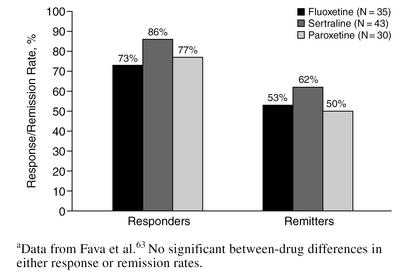
The clinical presentations of a major depressive episode or an individual anxiety disorder are far more thoroughly studied than the comorbid presentation of these disorders. Figure 1, panels A and B, is a diagrammatic illustration of a clinical presentation of patients who present with one diagnosis, major depressive disorder or anxiety disorder, and subsyndromal symptoms of the other diagnosis. There have been many reports demonstrating the efficacy of SSRIs and newer antidepressants in anxious depression, but few report head-to-head comparisons, so it is difficult to make within-class treatment decisions based solely on efficacy. One of the few studies that has reported a direct comparison (Figure 8) found equivalent antidepressant efficacy at the end of acute treatment for fluoxetine, sertraline, and paroxetine.63
Figure 8.
Comparison of Treatment Outcome Among Selective Serotonin Reuptake Inhibitors in Anxious Depressiona
Almost no literature is available that evaluates the efficacy of SSRIs or other antidepressants in the treatment of subsyndromal depression/anxiety. For many years, this group of patients was treated symptomatically with benzodiazepines, but some studies suggest that this treatment strategy is no better than modest amounts of supportive counseling64 and may actually iatrogenically contribute to the development of major depression,65 as well as the development of physical dependence on benzodiazepines.66 At present, no study of low-dose SSRI therapy is available in this patient population.
There is one final but important note about the pharmacologic treatment of depression and anxiety in primary care, whether the disorder occurs individually or comorbidly. Virtually all of the published treatment research is based on studies conducted in specialty psychiatry settings, many of which are academic or research-oriented. The prognosis and response to treatment of patients diagnosed with depression and/or anxiety in the primary care setting appear to be significantly superior to the results that are routinely reported on the basis of research in specialty settings.67 This means that published treatment results can only be generalized with caution to primary care and that the results are likely to represent an underestimate of prognosis and treatment response.
TOLERABILITY AND SAFETY
In addition to efficacy, the extensive use of the newer antidepressants in primary care depends on 2 factors: simplicity of use and a generally favorable safety and tolerability profile. The 2 factors are related since simplicity of use refers not only to the ease of a once-a-day dosing schedule (nefazodone is an exception) and an uncomplicated titration schedule but also to the fact that the newer antidepressants have very wide therapeutic windows and therefore are relatively safe in terms of overdose risk. As a result, treatment with SSRIs, for example, does not require the limiting of prescriptions to small numbers of pills and the close spacing of physician visits that treatment with the tricyclics require. Simplicity of use also refers to the generally low drug-drug interaction profile of most SSRIs and other newer antidepressants.
The safety and tolerability profile of the newer antidepressants is especially appealing in the primary care setting because of the information summarized above concerning the frequency of occurrence and the clinical implications of depression/anxiety comorbidity. Patients with concurrent depression and anxiety disorders have a longer time to response and higher risk of recurrence than patients presenting with either disorder alone. As a result, patients with depression/anxiety comorbidity are likely to benefit from a longer-term course of treatment. It is well established that compliance with long-term treatment is directly proportional to both simplicity of use and tolerability.
A related group of patients in whom safety and tolerability are paramount is the elderly. This is due, in part, to the markedly increased likelihood of additional drug treatment, as well as physiologic changes in drug metabolism and excretion.
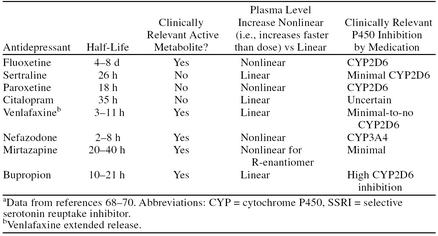
From a pharmacokinetic standpoint, the SSRIs and other newer antidepressants have a relatively clean profile. Yet, as can be seen in Table 3, there are within-class differences that need to be kept in mind. Fluoxetine has a substantially longer half-life, which is further extended by the long half-life of its clinically active metabolite norfluoxetine. A consequence of this long half-life is that fluoxetine requires a much longer washout before it is safe to switch to drugs whose concomitant use with fluoxetine is contraindicated. In the case of intolerability, it may take longer to clear the drug from the system.
Table 3.
Pharmacokinetic Profile of Marketed SSRIs and Atypical Antidepressantsa
The potential for drug-drug interactions is summarized in the P450 column of Table 3. Drug-drug interactions may come from the impact of a coadministered drug that inhibits a cytochrome P450 isoenzyme on SSRI metabolism or, conversely, the degree to which an SSRI inhibits P450 isosenzymes, thereby altering the metabolism and blood levels of coadministered drugs. Sertraline and citalopram have the “cleanest” pharmacokinetic profile in terms of short-to-intermediate half-life, lack of clinically relevant active metabolites, linear pharmacokinetics, and lack of potential for drug-drug interactions, although relatively few P450 pharmacokinetic data in humans are available at this point for citalopram. The literature is extensive that reviews the potential drug interaction profiles of the SSRIs and is beyond the scope of the current article.71 It should be emphasized, though, that the actual incidence of clinically relevant toxicity due to SSRI drug interactions is uncertain and may be low.
Tolerability of SSRIs and Newer Antidepressants
The SSRIs and other newer antidepressants have a generally favorable side effect profile. During long-term treatment (3 months or longer), tolerance develops to the majority of adverse events observed early in treatment, and they disappear or become much milder. But other adverse events may become more prominent over the course of long-term therapy, not so much because of increased severity, but because patients may be less able or willing to tolerate these adverse events over time.
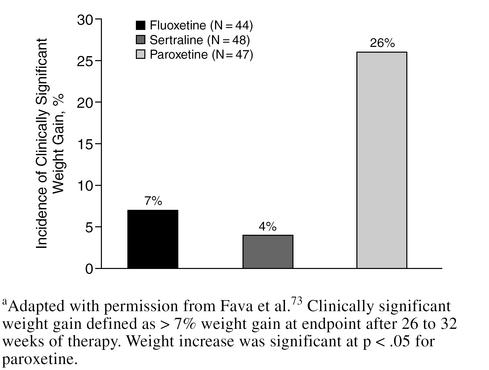
Perhaps the most prominent example of an adverse event leading to discontinuation during long-term antidepressant therapy is clinically significant weight gain. In a study of imipramine treatment of panic disorder, weight gain was the single biggest reason for medication discontinuation.72 Many of the SSRIs and newer antidepressants appear to offer advantages over tricyclic antidepressants and monoamine oxidase inhibitors in terms of weight gain, but little is known about the comparative differences in weight gain among the newer antidepressants themselves. Figure 9 summarizes the results of a study comparing the effects of fluoxetine, sertraline, and paroxetine on weight during long-term treatment. For both fluoxetine and sertraline, change in weight was not significantly different from baseline. However, at least 1 of every 4 patients treated with paroxetine gained > 7% of body weight after 26 to 32 weeks of treatment.73 The reason why treatment with paroxetine is more likely to be associated with significant weight gain is uncertain, but may relate to its more prominent anticholinergic effect.74
Figure 9.
Comparison of the Effect of Long-Term Selective Serotonin Reuptake Inhibitor Treatment on Weighta
Another adverse event that might be tolerated in the short run, but with the potential to lead to discontinuation in the long run, is sexual dysfunction. Nefazodone, bupropion, and mirtazapine appear to have the most favorable profile in terms of sexual dysfunction among all the newer agents.75,76
Not much is known about long-term outcome in patients who develop sexual dysfunction during acute treatment with SSRIs. There is evidence that sexual dysfunction is, at least in part, dose related and that reductions in dose will frequently alleviate sexual dysfunction. An analysis of long-term data from a study of sertraline in the treatment of depression has found that tolerance develops to sexual dysfunction in the majority of patients.77 One would assume that tolerance may be a class effect, but more data are needed to confirm this. There are few direct comparisons of the impact of SSRIs on sexual functioning based on systematic assessment. In one such study, no significant difference was found for the incidence of sexual dysfunction with sertraline (13.5%) versus citalopram (20%).78
EFFECTS OF MISSING DOSES AND ABRUPT TREATMENT DISCONTINUATION
One of the practical aspects of medication treatment with SSRIs and other antidepressants is the fact that patients, for various reasons, may not take their medication for several days. This form of temporary noncompliance leads to unplanned visits to the emergency room or to night or weekend calls to a physician's answering service. Such abrupt medication discontinuation may also occur when there is some medical reason for rapidly stopping treatment.
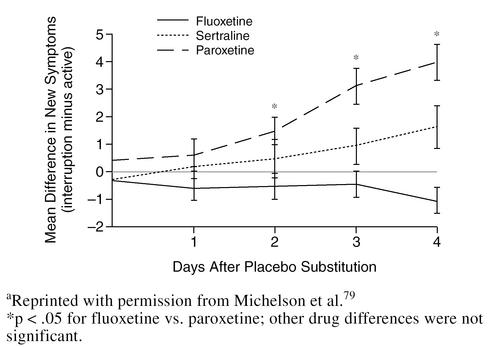
Several studies have directly compared the effect of abruptly discontinuing SSRI treatment.79,80 As might be expected on the basis of its very long half-life, fluoxetine had no discontinuation effects whatsoever (Figure 10). Even though paroxetine and sertraline have similar elimination half-lives, sertraline was found to have milder withdrawal effects after abrupt discontinuation of treatment than paroxetine, possibly because of the anticholinergic effects associated with the latter drug.79,80 The potential for a withdrawal syndrome after discontinuing paroxetine has recently been added to its product labeling.
Figure 10.
Effect of Abrupt Selective Serotonin Reuptake Inhibitor Discontinuation on Occurrence of Withdrawal Symptomsa
CONCLUSION
The co-occurrence of depression and anxiety disorders is extremely common in primary care. The clinical implications of depression/anxiety comorbidity include increased risk of suicide, increased risk of psychiatric hospitalization, increased disability, decreased compliance with treatment of medical illness, and markedly increased utilization of medical services. Patients with depression/anxiety comorbidity tend to have more chronic and recurrent forms of illness that require long-term treatment. This puts a premium on medications, such as the SSRIs, that have broad-spectrum efficacy (notably sertraline and paroxetine), wide therapeutic windows, and favorable pharmacokinetic and drug-interaction profiles (such as sertraline and citalopram) and are well tolerated in terms of side effects (such as weight gain), contributing to compliance with long-term treatment.
Despite the high prevalence and important clinical implications of depression/anxiety comorbidity, very little prospective treatment research is available. The appropriate recognition and treatment of depression and anxiety disorder comorbidity truly represent the last therapeutic frontier in the management of psychiatric illness in the primary care setting.
Drug names: bupropion (Wellbutrin and others), citalopram (Celexa), fluoxetine (Prozac and others), mirtazapine (Remeron), nefazodone (Serzone), paroxetine (Paxil), sertraline (Zoloft), venlafaxine (Effexor).
Footnotes
Dr. Hirschfeld received an honorarium from Pfizer Inc to support the editorial expenses involved in the preparation of this manuscript and has been a consultant and a speakers/advisory board member for Pfizer Inc.
REFERENCES
- Murray CJL, Lopez AD. eds. The Global Burden of Disease, vol 1: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass: Harvard University Press. 1996 [Google Scholar]
- Murray CJL, Lopez AD. eds. The Global Burden of Disease, vol 2: Global Health Statistics. A Compendium of Incidence, Prevalence, and Mortality Estimates for Over 200 Conditions. Cambridge, Mass: Harvard University Press. 1996 [Google Scholar]
- Kirmayer LJ, Robbins JM, Dworkind M, et al. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–741. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, et al. Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- Schurman RA, Kramer PD, Mitchell JB. The hidden mental health network: treatment of mental illness by nonpsychiatrist physicians. Arch Gen Psychiatry. 1985;42:89–94. doi: 10.1001/archpsyc.1985.01790240091010. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Keller MB, Klerman GL, Lavori PW, et al. Treatment received by depressed patients. JAMA. 1982;248:1848–1855. [PubMed] [Google Scholar]
- Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279:526–531. doi: 10.1001/jama.279.7.526. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Katon W, Broadhead WE, et al. Subsyndromal (“mixed”) anxiety-depression in primary care. J Gen Intern Med. 1994;9:507–512. doi: 10.1007/BF02599221. [DOI] [PubMed] [Google Scholar]
- Sartorius N, Ustun TB, Lecrubier Y, et al. Depression comorbid with anxiety: results from the WHO study on psychological disorders in primary health care. Br J Psychiatry Suppl. 1996;6:38–43. [PubMed] [Google Scholar]
- Broadhead WE, Blazer DG, George LK, et al. Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA. 1990;264:2524–2528. [PubMed] [Google Scholar]
- Murphy JM, Sobol AM, Olivier DC, et al. Prodromes of depression and anxiety: the Stirling County study. Br J Psychiatry. 1989;155:490–495. doi: 10.1192/bjp.155.4.490. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson C, McGonagle KA, et al. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 1996;168(suppl 30):17–30. [PubMed] [Google Scholar]
- Olfson M, Fireman B, Weissman MM, et al. Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry. 1997;154:1734–1740. doi: 10.1176/ajp.154.12.1734. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, et al. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry. 1996;153:1293–1300. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Cooke DJ. Vulnerability factors and depression. Br J Psychiatry. 1981;138:183–184. doi: 10.1192/bjp.138.2.183b. [DOI] [PubMed] [Google Scholar]
- Prudo R, Harris T, Brown GW. Psychiatric disorder in a rural and an urban population, 3: social integration and the morphology of affective disorder. Psychol Med. 1984;14:327–345. doi: 10.1017/s0033291700003597. [DOI] [PubMed] [Google Scholar]
- Finlay-Jones R, Brown GW. Types of stressful life event and the onset of anxiety and depressive disorders. Psychol Med. 1981;11:803–815. doi: 10.1017/s0033291700041301. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang PE, Wittchen HU, et al. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Arch Gen Psychiatry. 1998;55:801–808. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Wells KB, Meredith LS, et al. Comorbid anxiety disorder and the functioning and well-being of chronically ill patients of general medical providers. Arch Gen Psychiatry. 1996;53:889–895. doi: 10.1001/archpsyc.1996.01830100035005. [DOI] [PubMed] [Google Scholar]
- Lepine JP, Chignon JM, Teherani M. Suicide attempts in patients with panic disorder. Arch Gen Psychiatry. 1993;50:144–149. doi: 10.1001/archpsyc.1993.01820140070008. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Stang P, Wittchen HU, et al. Lifetime panic-depression comorbidity in the National Comorbidity Survey: association with symptoms, impairment, course and help-seeking. Br J Psychiatry. 2000;176:229–235. doi: 10.1192/bjp.176.3.229. [DOI] [PubMed] [Google Scholar]
- Coryell W, Endicott J, Andreasen NC, et al. Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry. 1988;145:293–300. doi: 10.1176/ajp.145.3.293. [DOI] [PubMed] [Google Scholar]
- Schade CP, Jones ER Jr, Wittlin BJ. A ten-year review of the validity and clinical utility of depression screening. Psychiatr Serv. 1998;49:55–61. doi: 10.1176/ps.49.1.55. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Broadhead WE, Leon AC, Weissman MM, et al. Development and validation of the SDDS-PC screen for multiple mental disorders in primary care. Arch Fam Med. 1995;4:211–219. doi: 10.1001/archfami.4.3.211. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AS, Klap R, Shelbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- Evans DL, Staab JP, Petitto JM, and et al. Depression in the medical setting: biopsychological interactions and treatment considerations. J Clin Psychiatry. 1999 60(suppl 4):40–55.discussion 56. [PubMed] [Google Scholar]
- Katon W, Sullivan MD. Depression and chronic medical illness. J Clin Psychiatry. 1990 51(suppl). 3–11.discussion 12–14. [PubMed] [Google Scholar]
- Carney C. Diabetes mellitus and major depressive disorder: an overview of prevalence, complications, and treatment. Depress Anxiety. 1998;7:149–157. [PubMed] [Google Scholar]
- Forrester AW, Lipsey JR, Teitelbaum ML, et al. Depression following myocardial infarction. Int J Psychiatry Med. 1992;22:33–46. doi: 10.2190/CJ9D-32C2-8CM7-FT3D. [DOI] [PubMed] [Google Scholar]
- Gonzalez MB, Snyderman TB, Colket JT, et al. Depression in patients with coronary artery disease. Depression. 1996;4:57–62. doi: 10.1002/(SICI)1522-7162(1996)4:2<57::AID-DEPR3>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Schleifer SJ, Macari-Hinson MM, Coyle DA, et al. The nature and course of depression following myocardial infarction. Arch Intern Med. 1989;149:1785–1789. [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- Ebrahim S, Barer D, Nouri F. Use of the Nottingham Health Profile with patients after a stroke. J Epidemiol Community Health. 1986;40:166–169. doi: 10.1136/jech.40.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustman PJ, Griffith LS, Clouse RE. Depression in adults with diabetes. Semin Clin Neuropsychiatry. 1997;2:15–23. doi: 10.1053/SCNP00200015. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE, Sheline YI, et al. Depression and coronary heart disease: a review for cardiologists. Clin Cardiol. 1997;20:196–200. doi: 10.1002/clc.4960200304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egberts AC, Leufkens HG, Hofman A, et al. Incidence of antidepressant drug use in older adults and association with chronic diseases: the Rotterdam Study. Int Clin Psychopharmacol. 1997;12:217–223. doi: 10.1097/00004850-199707000-00006. [DOI] [PubMed] [Google Scholar]
- Chemerinski E, Robinson RG. The neuropsychiatry of stroke. Psychosomatics. 2000;41:5–14. doi: 10.1016/S0033-3182(00)71168-6. [DOI] [PubMed] [Google Scholar]
- Slaughter JR, Slaughter KA, Nichols D, et al. Prevalence, clinical manifestations, etiology, and treatment of depression in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 2001;13:187–196. doi: 10.1176/jnp.13.2.187. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology. 2000;54:308–313. doi: 10.1212/wnl.54.2.308. [DOI] [PubMed] [Google Scholar]
- Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. Am J Psychiatry. 1998;155:4–11. doi: 10.1176/ajp.155.1.4. [DOI] [PubMed] [Google Scholar]
- McQuaid JR, Stein MB, Laffaye C, et al. Depression in a primary care clinic: the prevalence and impact of an unrecognized disorder. J Affect Disord. 1999;55:1–10. doi: 10.1016/s0165-0327(98)00191-8. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Lustman PJ, Anderson RJ, Freedland KE, et al. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23:934–942. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Applegate WB, Berge K, et al. Change in depression as a precursor of cardiovascular events. SHEP Cooperative Research Group (Systoloc Hypertension in the elderly) Arch Intern Med. 1996;156:553–561. [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation. 1996;93:1976–1980. doi: 10.1161/01.cir.93.11.1976. [DOI] [PubMed] [Google Scholar]
- Glassman A, O'Connor CM, and Harrison W. Sertraline treatment of major depression in patients with acute MI or unstable angina [poster]. Presented at the 154th annual meeting of the American Psychiatric Association; May 5–10, 2001; New Orleans, La. [Google Scholar]
- Pollack MH, Zaninelli R, Goddard A, et al. Paroxetine in the treatment of generalized anxiety disorder: results of a placebo-controlled, flexible dosage trial. J Clin Psychiatry. 2001;62:350–357. doi: 10.4088/jcp.v62n0508. [DOI] [PubMed] [Google Scholar]
- Beebe KL, Pitts CD, Ruggerio L, and et al. Paroxetine in the treatment of PTSD [poster]. Presented at the 154th annual meeting of the American Psychiatric Association; May 5–10, 2001; New Orleans, La. [Google Scholar]
- Hoehn-Saric R, Ninan P, Black DW, et al. Multicenter double-blind comparison of sertraline and desipramine for concurrent obsessive-compulsive and major depressive disorders. Arch Gen Psychiatry. 2000;57:76–82. doi: 10.1001/archpsyc.57.1.76. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry. 2001;58:485–492. doi: 10.1001/archpsyc.58.5.485. [DOI] [PubMed] [Google Scholar]
- Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- Silverstone PH, Salinas E. Efficacy of venlafaxine extended release in patients with major depressive disorder and comorbid generalized anxiety disorder. J Clin Psychiatry. 2001;62:523–529. doi: 10.4088/jcp.v62n07a04. [DOI] [PubMed] [Google Scholar]
- Anderson IM. SSRIs versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. Depress Anxiety. 1998;7(suppl 1):11–17. [PubMed] [Google Scholar]
- Jefferson JW. Antidepressants in panic disorder. J Clin Psychiatry. 1997;58(suppl 2):20–24. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Goldenberg IM, et al. Influence of depression on the treatment of panic disorder with imipramine, alprazolam and placebo. J Affect Disord. 1993;28:27–38. doi: 10.1016/0165-0327(93)90074-t. [DOI] [PubMed] [Google Scholar]
- Fava M, Rosenbaum JF, Hoog SL, et al. Fluoxetine vs sertraline and paroxetine in major depression: tolerability and efficacy in anxious depression. J Affect Disord. 2000;59:119–126. doi: 10.1016/s0165-0327(99)00131-7. [DOI] [PubMed] [Google Scholar]
- Catalan J, Gath D, Edmonds G, et al. The effects of non-prescribing of anxiolytics in general practice, 1: controlled evaluation of psychiatric and social outcome. Br J Psychiatry. 1984;144:593–602. doi: 10.1192/bjp.144.6.593. [DOI] [PubMed] [Google Scholar]
- Smith BD, Salzman C. Do benzodiazepines cause depression? Hosp Community Psychiatry. 1991;42:1101–1102. doi: 10.1176/ps.42.11.1101. [DOI] [PubMed] [Google Scholar]
- Nelson J, Chouinard G. Guidelines for the clinical use of benzodiazepines: pharmacokinetics, dependency, rebound and withdrawal. Canadian Society for Clinical Pharmacology. Can J Clin Pharmacol. 1999;6:69–83. [PubMed] [Google Scholar]
- Lydiard RB, Perera P, Batzar E, et al. From the bench to the trench: a comparison of sertraline treatment of major depression in clinical and research patient samples. Primary Care Companion J Clin Psychiatry. 1999;1:154–162. doi: 10.4088/pcc.v01n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preskorn SH. Clinically relevant pharmacology of selective serotonin reuptake inhibitors: an overview with emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clin Pharmacokinet. 1997;32(suppl 1):1–21. doi: 10.2165/00003088-199700321-00003. [DOI] [PubMed] [Google Scholar]
- Richelson E. Pharmacokinetic drug interactions of new antidepressants: a review of the effects on the metabolism of other drugs. Mayo Clin Proc. 1997;72:835–847. doi: 10.4065/72.9.835. [DOI] [PubMed] [Google Scholar]
- Hiemke C, Hartter S. Pharmacokinetics of selective serotonin reuptake inhibitors. Pharmacol Ther. 2000;85:11–28. doi: 10.1016/s0163-7258(99)00048-0. [DOI] [PubMed] [Google Scholar]
- Harvey AT, Preskorn SH. Cytochrome P450 enzymes: interpretation of their interactions with selective serotonin reuptake inhibitors, part 2. J Clin Psychopharmacol. 1996;16:345–355. doi: 10.1097/00004714-199608000-00002. [DOI] [PubMed] [Google Scholar]
- Noyes R Jr, Garvey MJ, Cook BL, et al. Problems with tricyclic antidepressant use in patients with panic disorder or agoraphobia: results of a naturalistic follow-up study. J Clin Psychiatry. 1989;50:163–169. [PubMed] [Google Scholar]
- Fava M, Judge R, Hoog SL, et al. Fluoxetine versus sertraline and paroxetine in major depressive disorder: changes in weight with long-term treatment. J Clin Psychiatry. 2000;61:863–867. doi: 10.4088/jcp.v61n1109. [DOI] [PubMed] [Google Scholar]
- Bourin M, Chue P, Guillon Y. Paroxetine: a review. CNS Drug Rev. 2001;7:25–47. doi: 10.1111/j.1527-3458.2001.tb00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RM. Management of sexual side effects of antidepressant therapy. J Clin Psychiatry. 1999 60(suppl 14):27–30.discussion 31–35. [PubMed] [Google Scholar]
- Hirschfeld RM. Sexual dysfunction in depression: disease- or drug-related? Depress Anxiety. 1998;7(suppl 1):21–23. doi: 10.1002/(sici)1520-6394(1998)7:1+<21::aid-da6>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Pohl R, Holland P, Chung H, and et al. Effectiveness of sertraline in long-term treatment of panic disorder: treatment response, sexual functioning, and BMI. In: New Research Abstracts of the 154th Annual Meeting of the American Psychiatric Association; May 9, 2001; New Orleans, La. Abstract NR629:170. [Google Scholar]
- Ekselius L, von Knorring L. Effect on sexual function of long-term treatment with selective serotonin reuptake inhibitors in depressed patients treated in primary care. J Clin Psychopharmacol. 2001;21:154–160. doi: 10.1097/00004714-200104000-00006. [DOI] [PubMed] [Google Scholar]
- Michelson D, Fava M, Amsterdam J, et al. Interruption of selective serotonin reuptake inhibitor treatment: double-blind, placebo-controlled trial. Br J Psychiatry. 2000;176:353–358. doi: 10.1192/bjp.176.4.363. [DOI] [PubMed] [Google Scholar]
- Rosenbaum JF, Fava M, Hoog SL, et al. Selective serotonin reuptake inhibitor discontinuation syndrome: a randomized clinical trial. Biol Psychiatry. 1998;44:77–87. doi: 10.1016/s0006-3223(98)00126-7. [DOI] [PubMed] [Google Scholar]