Abstract
Background: This article examines the nature of psychological trauma and posttraumatic stress disorder (PTSD) in 504 patients recruited from primary care settings.
Method: Patients were screened for anxiety in waiting rooms at 14 general medical settings, and those with a sufficient number and severity of anxiety symptoms were administered a standardized diagnostic clinical interview. Those who met DSM-IV criteria for an anxiety disorder and who were willing to participate were included in this study. Of the 504 patients, 185 met DSM-IV criteria for PTSD.
Results: Results indicated that 418 (83%) of primary care patients in our sample reported at least 1 traumatic event in their lifetime. The most prevalent traumas experienced by the entire sample of participants were witnessing others being seriously injured or killed, serious accidents, and rape. Of those participants with PTSD, rape was the strongest predictor of a PTSD diagnosis. Analyses examining gender differences indicated that, for women, a history of other unwanted sexual contact or witnessing a sexual assault, being attacked with a weapon or with intent to kill, or witnessing someone being injured were found to be risk factors for a PTSD diagnosis. Examination of clinical characteristics indicated a high rate of comorbidity of psychiatric disorders among patients with PTSD, including high rates of alcohol/substance abuse, depression, and suicide attempts.
Conclusion: These findings emphasize the continued need to assess patients presenting at general medical facilities about trauma history.
In recent years, there has been a growing interest in the impact of mental disorders within medical settings as patients have increasingly sought mental health treatment through primary and general health care settings. Previous research has found that individuals with mental disorders are more likely to seek help from a nonpsychiatric physician rather than from a mental health professional.1 Moreover, recent studies2–6 have suggested that individuals exposed to trauma are high users of health care services. For example, Koss et al.5 found that female crime victims had 2.5 times more nonpsychiatric physician visits and health care costs than nonvictimized individuals. Additionally, in a study examining the economic burden of anxiety disorders in medical facilities, Greenberg and colleagues4 found that a diagnosis of posttraumatic stress disorder (PTSD) was a significant risk factor for increased medical utilization.
Several studies have examined the type of traumatic event experienced and its relationship to the onset of PTSD. One of the traumatic stressors most consistently found to be associated with PTSD is sexual assault, and most notably, rape.7–9 In a sample of 4008 women, Resnick et al.8 reported a lifetime PTSD prevalence rate of 32% for women who had been raped, nearly 3 times greater than the overall lifetime PTSD rate of 12% in women. Other studies10,11 confirm that initial rates of PTSD following a completed sexual assault are extremely high, with one study12 reporting a lifetime prevalence of PTSD of 80% in women who had reported being raped. In addition to sexual assault, other traumas most associated with a high probability of PTSD included combat exposure and physical assault.8,13
Examination of gender differences from previous research has revealed that males and females differ in rates of both exposure to traumatic stressors and subsequent PTSD. In the National Comorbidity Study, Kessler et al.7 found that, although men were more likely than women to experience at least 1 trauma overall, women were more than twice as likely as men to develop PTSD (10.4%, 5.0%, respectively). This is consistent with recent findings by Breslau et al.,14 who found that the risk of PTSD was more than 2-fold higher in women than in men. Kessler et al.7 hypothesized that this finding may not necessarily indicate increased vulnerability in developing PTSD for women, but rather that women experience more severe traumas that are associated with a higher probability of developing PTSD. Other reported gender differences include an increased risk for substance abuse for men with PTSD and an increased risk for anxiety and depression for women with PTSD.15
Although past findings indicate that PTSD and a history of trauma exposure are risk factors for increased medical utilization, studies report that PTSD is greatly underdiagnosed in a variety of clinical settings. For example, Davidson and Smith16 found that out of 12 patients meeting criteria for PTSD, only 1 received a diagnosis for PTSD in a general psychiatric outpatient clinic. In primary care settings, psychiatric diagnoses such as PTSD may be overlooked due to several factors, including lack of clinician awareness of PTSD symptoms, failure to ask patients about traumatic experiences, and, most importantly, a limited amount of time to obtain a complex medical and trauma history.17 High rates of comorbidity may also cause the PTSD diagnosis to be underreported because of overlapping symptoms with better known disorders (e.g., depression).
Information on PTSD in a primary care sample is needed to provide clinicians and researchers with knowledge to assist clinicians in identifying and assessing trauma victims, particularly since general medical facilities are typically the first place where patients with PTSD present with symptoms. This study examined key components of PTSD and trauma exposure in patients visiting general medical facilities, including the types of traumatic events experienced, the relationship between these traumatic events and PTSD, and the number of traumatic stressors patients have experienced. Additionally, past literature7 suggests gender differences in the rates of both exposure to traumatic stressors and PTSD. This relationship, as well as differences in gender across comorbid disorders including alcohol/substance use, depression, and anxiety disorders, was examined.
METHOD
Design
This study is part of the larger Primary Care Anxiety Project, a prospective, naturalistic, longitudinal, multisite study of anxiety disorders in patients presenting at general medical clinics. Participants are recruited from 14 primary care, general internal medicine, and family medicine clinics in the Hanover, N.H.; Boston, Mass.; Worcester, Mass.; and Providence, R.I., areas. The practices were selected to represent a variety of general medical settings. The recruitment sites are located in rural, urban, and suburban areas and include large hospital-based clinics and small private practices. Inclusion criteria are that participants must be a minimum of 18 years of age and English speaking. Further, they must be a patient at the recruitment site and be scheduled for a general medical appointment on the day of recruitment. Exclusion criteria are active psychosis, no current address and phone number, and pregnancy.
Procedures
Recruitment began in July 1997. Participants were recruited on the day of a visit to the medical practice, while waiting for their appointment. Primary care patients who were awaiting shots, tests, or other limited services at the primary care practice were not eligible. A research assistant approached eligible patients in the practice waiting room. After complete description of the study, written informed consent was obtained. Potential participants then completed a questionnaire screening for symptoms of anxiety. Patients screened positive if they endorsed experiencing any anxiety symptoms. To ensure that the screen identified nearly all primary care patients with an anxiety disorder(s), a validation study of the screen was conducted. The screen was intentionally designed to cast a broad net to increase the sensitivity of detecting anxiety disorders. Thus, we anticipated a large number of false-positives (positive on the screen but negative [did not meet criteria for anxiety disorders] on the Structured Clinical Interview for DSM-IV [SCID-IV]18), but very few false-negatives (negative screen but positive SCID-IV). In the validation study, 75 patients from the various recruitment sites completed the screen and were scheduled for a SCID-IV regardless of the results of the screen. Results indicated that the screen did an excellent job at detecting the potential presence of an anxiety disorder. Of the 42 patients who screened negative (no anxiety symptoms), none subsequently met criteria for an anxiety disorder after completion of the SCID-IV (false-negative rate of 0%).
Those who screened positive for anxiety symptoms were then assessed using the SCID-IV.18 The psychotic screen, mood, anxiety, substance use, and eating disorders modules of the SCID-IV were administered. Interviewers, who ranged in education from having a bachelor's degree to having a Ph.D., received a rigorous training program in administration of the study instruments. Three thousand seven hundred fifty primary care patients were administered the screening questionnaire, and 1890 screened positive. The SCID-IV was then administered to 1492 of the potential participants who screened positive (398 patients who screened positive declined to participate). Of patients who completed the SCID-IV, 504 met criteria for 1 or more of the following index anxiety disorders and were enrolled in the study: panic disorder with or without agoraphobia, agoraphobia without history of panic disorder, generalized anxiety disorder (GAD), social phobia, PTSD, or mixed anxiety-depressive disorder.
Trauma history was assessed during the structured interview, using a revised version of the Trauma Assessment for Adults developed by Resnick and colleagues.19 Participants were asked if they had ever experienced any of the following occurrences: (1) military combat experience or military service in a war zone; (2) serious accident at work, in a car, or elsewhere; (3) forced sexual contact or rape; (4) attack with a gun, knife, or other weapon; (5) attack without a weapon but with the intent to kill or seriously injure; (6) any other situation in which they were seriously injured or suffered physical damage; (7) any other situation in which they feared they might be killed or seriously injured; (8) witnessing someone be seriously injured or killed; (9) witnessing someone be sexually abused or assaulted; (10) any other extraordinarily stressful situation or event.
All statistical analyses were conducted using SAS, Version 6.12, using PROC FREQ, PROC T-TEST, PROC ANOVA, and PROC LOGISTIC. All t tests conducted were 2-tailed.
RESULTS
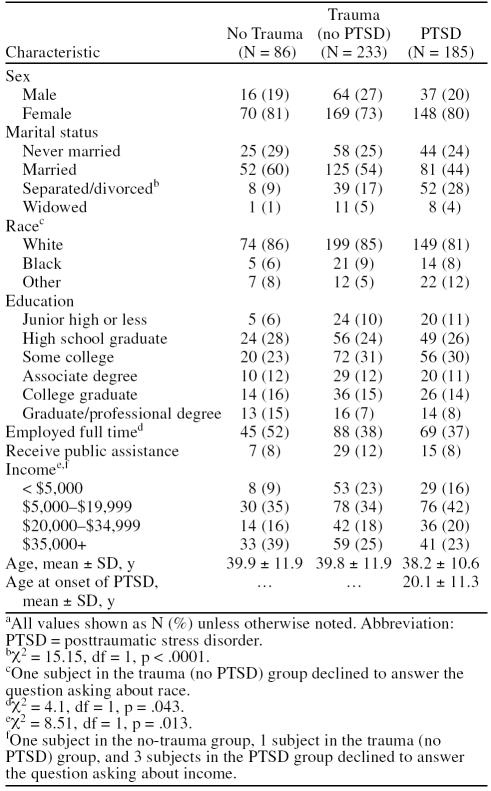
Of the 504 participants with an anxiety diagnosis, 418 (83%) reported experiencing at least 1 traumatic event. Of these, 185 participants (44% of those with trauma histories) met full DSM-IV criteria for PTSD at intake; both men and women with a reported trauma history were found to have high frequencies of PTSD at intake (34.3% and 41.7%, respectively). Demographic characteristics of the no-trauma, trauma (no PTSD), and PTSD groups are reported in Table 1. The majority of participants were white (84%), female (77%), and married at the time of intake (51%). The mean ± SD age of the PTSD group at the time of intake was 38.2 ± 10.6 years, while the mean age at onset of PTSD was 20 years, indicating that the average participant had PTSD for over 17 years. A Cochran-Mantel-Haenszel chi-square analysis revealed a significant trend in divorce/separation rate relative to trauma and PTSD (χ2 = 5.87, df = 1, p < .05; see Table 1). Subsequent analyses indicated significant differences in divorce/separation rates between the no-trauma (9%) and PTSD groups (28%; χ2 = 12.0, df = 1, p < .001) and the trauma (no PTSD) (17%) and PTSD groups (28%; χ2 = 7.814, df = 1, p < .001). No other significant differences were found across gender, race, education, or income at the .01 level.
Table 1.
Demographic Characteristics by Trauma Statusa
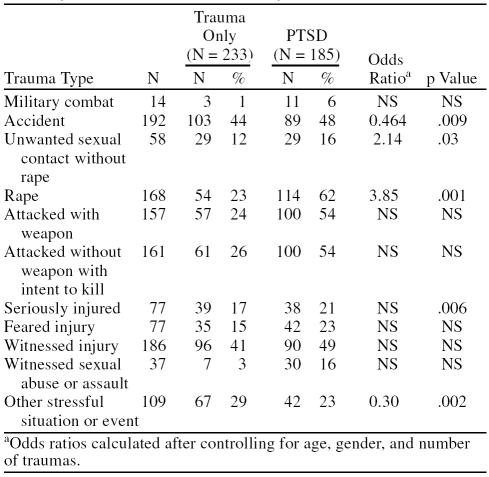
Of the 504 participants, the most frequently occurring lifetime trauma experienced was being involved in a serious accident (38%), followed by witnessing someone being injured (37%), being raped (33%), and being attacked with the intent to kill (32%; Table 2). After age, gender, and number of other traumas were controlled for, results from a logistic regression examining the association between PTSD and trauma type indicated that rape and other unwanted sexual contact were the strongest predictors of a PTSD diagnosis. For example, examination of odds ratios indicated that participants who reported a lifetime history of being raped were nearly 4 times more likely to develop PTSD than those with anxiety who had other traumas.
Table 2.
Logistic Regression of Predictors of Posttraumatic Stress Disorder (PTSD) Across Trauma Types Among Primary Care Patients With Anxiety Disorders
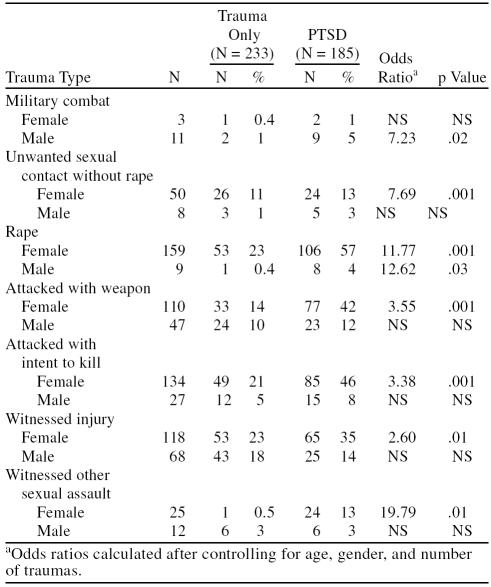
Several gender differences were also found in the types of traumatic events experienced. Men reported significantly higher levels of combat exposure (9% vs. 1%), being attacked with a weapon (40% vs. 28%), and being injured (27% vs. 12%) than did women in our sample. In contrast, women reported a significantly higher incident rate of unwanted sexual contact than men (54% vs. 15%). Men and women also differed in the traumas that most predicted a PTSD diagnosis (Table 3). In women, significant odds ratios predicting PTSD at intake included rape or other unwanted sexual contact (or witnessing a sexual assault), being attacked with a weapon or with an intent to kill, and witnessing someone else being seriously injured. In men, only rape and military combat were found to be significantly associated with being diagnosed with PTSD at intake (see Table 3).
Table 3.
Logistic Regression of Predictors of Posttraumatic Stress Disorder (PTSD) Across Trauma Types by Gender
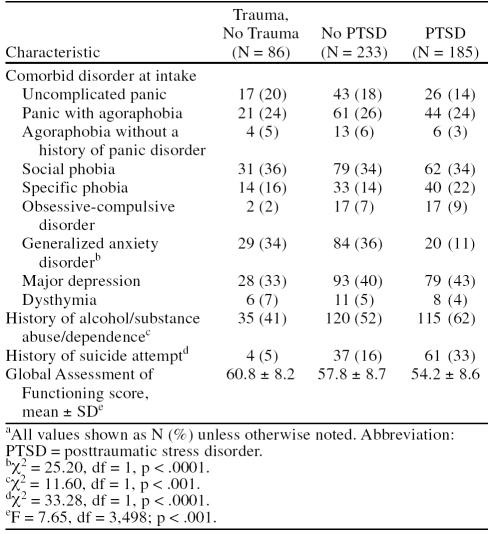
Examination of intake comorbidity indicates that participants in the PTSD group had high rates of comorbid disorders (Table 4). For example, 43% of patients in the PTSD group also had comorbid major depression, 34% met criteria for social phobia, and 62% met DSM-IV criteria for a lifetime history of alcohol/substance abuse problems. Several significantly different clinical characteristics were found across the no-trauma, trauma (no PTSD), and PTSD groups. Patients in the PTSD group had significantly higher lifetime rates of alcohol or substance use than did patients without PTSD. No significant differences in alcohol or substance use were found between the trauma (no PTSD) group and the no-trauma group. A significant main effect of trauma history was found in predicting participants' Global Assessment of Functioning (GAF) score, a measure of overall psychological, social, and occupational functioning (F = 7.65, df = 2,405; p < .001). A series of pairwise comparisons indicated that participants with no lifetime history of trauma had significantly higher GAF scores, indicating that they had better overall functioning than those patients reporting experiencing traumatic events, regardless of PTSD status. No significant differences were found between the trauma (no PTSD) group and the PTSD group on GAF scores. Examination of past suicide attempts using a Cochran-Mantel-Haenszel chi-square analysis revealed significant differences in the no-trauma, trauma (no PTSD), and PTSD groups (χ2 = 33.28, p < .0001; see Table 4). Subsequent follow-up analyses indicated that the relative number of lifetime suicide attempts significantly increased as a function of trauma and PTSD status. Rates of lifetime suicide attempts increased from 5% for the no-trauma group to 16% for the trauma (no PTSD) group to 33% for the PTSD group.
Table 4.
Clinical Characteristics of the No-Trauma, Trauma (no PTSD), and PTSD Groupsa
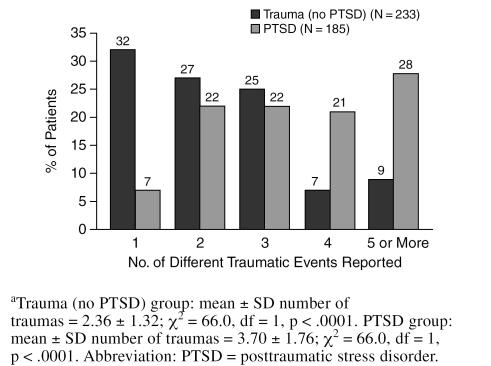
Frequency of traumatic exposure is reported in Figure 1. Of the 418 participants who indicated previous trauma exposure, 331 (79%) reported experiencing multiple events. Those with PTSD reported significantly more traumatic events than the trauma (no PTSD) group. For example, 49% of the PTSD group endorsed experiencing 4 or more traumatic events compared with 15% of the trauma (no PTSD) group. Examination of gender differences indicated that both male and female participants reported similar levels of lifetime trauma exposure. Inspection of participants' overall level of functioning indicated that GAF score was significantly related to the number of traumatic events experienced (F = 36.70, df = 1,502; p < .0001). Patients who were exposed to several traumatic events had significantly lower GAF scores, indicating generally worse functioning, than patients who experienced fewer traumatic events.
Figure 1.
Number of Different Traumatic Events Experienced by the Trauma (no PTSD) Group and the PTSD Groupa
DISCUSSION
This study was conducted to examine the relationships of traumatic events and PTSD in patients utilizing primary care facilities. An overwhelming majority of patients in our sample reported experiencing at least 1 traumatic experience in their lifetime (83%). This finding is similar with previous research that also reported high levels of traumatic exposure.8,15 Examination of gender differences indicated that although men and women differed in their reported frequency of specific traumatic events, the overall percentage of traumatic exposure and PTSD diagnosis did not differ significantly by gender. The traumatic event most associated with a diagnosis of PTSD in this sample was rape, regardless of gender, a finding that is consistent with previous research.7,12,20 Additionally, being attacked with a weapon and attacked with intent to seriously injure or kill were also significantly associated with a PTSD diagnosis in women.7 For men, experiencing military combat increased the risk of developing PTSD by nearly 7-fold. However, it should be noted that participants in this study were primarily a non–combat trauma sample, with relatively few participants reporting a history of combat experience. Thus, this finding should be interpreted with caution, as it is difficult to compare it with past studies on combat-related PTSD.
Although witnessing or experiencing a single traumatic event in a lifetime is distressing in and of itself, a majority of patients in the sample reported experiencing multiple traumatic events, particularly those who met DSM-IV criteria for PTSD at intake. The PTSD group, on average, had experienced many more traumas than the trauma-exposed non-PTSD subsample. For example, 49% of the PTSD group endorsed experiencing 4 or more traumatic events compared with 15% of the trauma (no PTSD) group. This is consistent with a previous study which suggests that prior trauma exposure is a risk factor for the development of PTSD resulting from a subsequent traumatic event.21 For example, high rates of childhood trauma have been reported in Vietnam combat veterans with PTSD, suggesting a vulnerability to future trauma exposure.22,23 Other potential hypotheses include that early-onset PTSD leads to increased risk of subsequent trauma exposure, thereby increasing the number of traumas patients with PTSD experience over a lifetime. Additionally, other researchers12,24 have hypothesized that frequent trauma exposure may also be a marker of individuals with heightened emotional vulnerability, which helps to explain the high risk of PTSD in such a population.
Examination of clinical characteristics of the sample indicates that participants with PTSD had high rates of comorbidity with other disorders, which is congruent with previous studies.7,25,26 Although anxiety disorders in general have been shown to have high comorbidity rates, it is interesting to note that, when compared with participants with other anxiety disorders, the PTSD group had significantly higher comorbid major depression and a greater history of both alcohol/substance abuse problems and suicide attempts/gestures. A disturbing but consistent finding indicates that a diagnosis of PTSD is a significant risk factor for suicide attempts or gestures.27 While only 6% of the no-trauma group reported a history of suicide gestures or attempts, this proportion increased to 17% of the trauma (no PTSD) group and 38% of the PTSD group. Within this sample, this suicide-PTSD link was found to be even stronger than the relationship between suicide and major depression.
Potential limitations of our study included the lack of blinding of raters to the trauma and anxiety disorders diagnoses of subjects and the lack of a healthy control group. Additionally, participants may have been hesitant to discuss their trauma history during initial face-to-face interviews. Given patient embarrassment, denial, and dissociation, the results of the current study may underreport the occurrence of traumatic events. Resnick et al.8 noted that anonymity of telephone interviews might contribute to higher and more accurate counts of traumatic events. A final limitation concerns the assessment instrument used to obtain reports of traumatic exposure. The measure allowed us to obtain a tally only of the number of different traumatic events reported, not of the total number of traumas experienced. For example, if a participant endorsed that he/she was attacked with a weapon during his/her lifetime, it is not known if the participant had been attacked with a weapon more than once.
Despite these limitations, our results with a sample seeking treatment at primary care settings emphasize the continued need to assess the trauma history of patients with seemingly unrelated medical illnesses. Physicians' increased awareness will enable them to properly address this concern and should increase the likelihood that patients with PTSD receive appropriate care. Proper assessment is critical, as patients may not volunteer trauma histories due to embarrassment or avoidance. They also might feel that the trauma has no bearing on their present complaint. Additionally, accurate screening for trauma and PTSD in primary care facilities is crucial, as the clinical presentation of PTSD symptoms may overlap with other psychiatric disorders or somatic complaints, making it very difficult to make an accurate diagnosis. As Brady28 states, “… diminished interest, restricted range of affect, sleep difficulties, and poor concentration are all overlapping symptoms of PTSD and depression. Irritability, hypervigilance, and increased startle reflex are symptoms of PTSD that overlap with GAD. When exposed to reminders of the trauma, individuals with PTSD also have physiologic reactivity that may present as panic attacks.”(p13) Thus, if PTSD is not assessed appropriately, specific pharmacologic interventions could potentially be dangerous to a patient with PTSD, particularly if he/she is self-medicating or suicidal. For example, benzodiazepines could be potentially lethal when taken in combination with other drugs or alcohol. Moreover, proper diagnosis of PTSD in primary care settings may actually assist in reducing the long-term economic burden of PTSD. Greenberg et al.4 reported that indirect costs associated with undiagnosed or misdiagnosed anxiety disorders, including PTSD, would be greatly reduced if more effective recognition and treatment occurred in primary care settings.
Recently, the Expert Consensus Guidelines for the treatment of PTSD were published; they included a primary care treatment guide that advocates querying patients about their trauma histories, especially patients who present with depression, anxiety, or substance abuse problems.29 Further psychosocial and pharmacologic interventions are recommended to primary care physicians, including early intervention and prevention strategies and recommended psychological treatments and referral, as well as recommended doses for somatic treatment. If incorporated into clinical practice, these guidelines would greatly assist clinicians in remaining alert to the symptoms of PTSD and offering patients appropriate pharmacologic and psychotherapeutic treatment options.
This study was an initial examination of PTSD findings reported at intake of a large primary care anxiety project. Because of the longitudinal and prospective design of this study, future research on this study will enable us to examine how individuals with PTSD function over time, including chronicity, remission, and relapse rates and both the incidence and influence of comorbid disorders. Additionally, this design will allow us to examine how new traumas contribute to the course of PTSD, which may help researchers and clinicians understand the long-term course of this disorder and aid in the development of new intervention strategies to treat it.
Acknowledgments
Presented at the 20th annual conference of the Anxiety Disorders Association of America, March 23–26, 2000; Washington, D.C.
The Primary Care Anxiety Project is conducted with the participation of the following investigators: Martin B. Keller, M.D. (Chairperson), Risa B. Weisberg, Ph.D.; Steven E. Bruce, Ph.D.; Regina T. Dolan, Ph.D.; Meredith Warshaw, M.S.S., M.A. (Brown University School of Medicine); Robert Birnbaum, M.D.; Randall Paulsen, M.D. (Beth Israel Deaconess Medical Center); Larry Culpepper, M.D.; Thomas Gilbert, M.D. (Boston University Medical Center, Codman Square Community Health Center); Mark Fagan, M.D. (Rhode Island Hospital); David Fried, M.D. (Coastal Medical, Renaissance Group); Gertrude Manchester, M.D.; Ann Massion, M.D. (UMASS Medical Center); Donya Powers, M.D. (Partners in Family Health, Inc.); Bruce Ditzion, M.D. (Mount Auburn Hospital); Richard Lain, M.D. (Memorial Hospital of Rhode Island [Internal and Family Medicine]); John Wasson, M.D.; Deborah Johnson (Buck Road Clinic, Gifford Family Health Center, Mount Ascutney, Ottauquechee Health Center, and White River Junction Family Practice); Ernst Berndt, Ph.D.; Stan Finkelstein, M.D. (Massachusetts Institute of Technology).
Footnotes
A complete list of the investigators who participated in the Primary Care Anxiety Research Program appears at the end of the article.
This Primary Care Anxiety Project is supported by an unrestricted grant from Pfizer Pharmaceuticals, Inc.
Financial disclosure: Dr. Culpepper is a consultant for Pfizer, Forest Labs, Lilly, and Wyeth-Ayerst. Dr. Keller is a consultant for or has received honoraria from Pfizer Inc, Bristol-Myers Squibb, Forest Laboratories, Wyeth-Ayerst Laboratories, Merck, Inc., Janssen, Eli Lilly, Organon, and Pharmacia/Upjohn; has received grant/research support from Wyeth-Ayerst, SmithKline Beecham, Upjohn, Pfizer Inc, Bristol-Myers Squibb, Merck, Inc., Forest Laboratories, Zeneca, and Organon, Inc.; and is an advisory board member for Wyeth-Ayerst, Pfizer Inc, Bristol-Myers Squibb, Eli Lilly, Forest Laboratories, Organon, SmithKline Beecham, Merck, Inc., Janssen, Mitsubishi Pharmaceuticals, Pharmacia/Upjohn, Scirex, Vela Pharmaceuticals, Sepracor Pharmaceuticals, Somerset Pharmaceuticals, and Sanofi-Synthelabo.
REFERENCES
- Bland RC, Newman SC, Orn H. Help-seeking for psychiatric disorders. Can J Psychiatry. 1997;42:935–941. doi: 10.1177/070674379704200904. [DOI] [PubMed] [Google Scholar]
- Friedman MJ. Posttraumatic stress disorder. J Clin Psychiatry. 1997;58(suppl 9):33–36. [PubMed] [Google Scholar]
- Friedman MJ, Schnurr PP. The relationship between trauma, post-traumatic stress disorder and physical health. In: Friedman MH, Charney DS, Deutch AY, eds. Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. Philadelphia, Pa: Lippincott-Raven Publishers. 1995 507–524. [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Koss MP, Woodruff WJ, Koss PG. Relationship of criminal victimization to health perceptions among women medical patients. J Consult Clin Psychol. 1990;58:147–152. doi: 10.1037//0022-006x.58.2.147. [DOI] [PubMed] [Google Scholar]
- Switzer GE, Dew MA, Thompson K, et al. Posttraumatic stress disorder and service utilization among urban mental health center clients. J Trauma Stress. 1999;12:25–39. doi: 10.1023/A:1024738114428. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Resnick H, Kilpatrick DG, Dansky BS, et al. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Hanson RK. The psychological impact of sexual assault on women and children: a review. Ann Sex Res. 1990;3:187–232. [Google Scholar]
- Foa EB, Riggs DS. Posttraumatic stress disorder and rape. In: Pynoos RS, ed. Posttraumatic Stress Disorder: A Clinical Review. Lutherville, Md: Sidran Press. 1994 [Google Scholar]
- Rothbaum B, Foa EB, Riggs DS, et al. A prospective examination of post-traumatic stress disorder in rape victims. J Trauma Stress. 1992;5:455–475. [Google Scholar]
- Breslau N, Davis GC, Andreski MA, et al. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski MA, et al. Sex differences in post traumatic stress disorder. Arch Gen Psychiatry. 1997;54:1044–1048. doi: 10.1001/archpsyc.1997.01830230082012. [DOI] [PubMed] [Google Scholar]
- Green BL. Psychosocial research in traumatic stress: an update. J Trauma Stress. 1994;7:341–362. doi: 10.1007/BF02102782. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Smith RD. Traumatic experiences in psychiatric outpatients. J Trauma Stress. 1990;3:459–474. [Google Scholar]
- Davidson JRT, Conner KM. Management of posttraumatic stress disorder: diagnostic and therapeutic issues. J Clin Psychiatry. 1999;60:33–38. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, and et al. Structured Clinical Interview for DSM-IV Axis I Disorders. New York, NY: Biometrics Research, New York State Psychiatric Institute. 1997 [Google Scholar]
- Resnick HS, Best CL, Freedy JR, and et al. Trauma Assessment for Adults. Charleston, SC: Crime Victims Research and Treatment Center, Department of Psychiatry, Medical University of South Carolina. 1993 [Google Scholar]
- Foa EB, Rothbaum B, Steketee GS. Treatment of rape victims. J Interpersonal Violence. 1993;8:256–276. [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, et al. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, et al. Childhood physical abuse and combat-related PTSD in Vietnam veterans. Am J Psychiatry. 1993;150:235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Zaida LJ, Foy DW. Childhood abuse experiences and combat-related PTSD. J Trauma Stress. 1994;7:33–42. doi: 10.1007/BF02111910. [DOI] [PubMed] [Google Scholar]
- Breslau N. Epidemiology of trauma and posttraumatic stress disorder. In: Yehuda, R, ed. Psychological Trauma. Washington, DC: American Psychiatric Press. 1998 1–29. [Google Scholar]
- Deering CG, Glover SG, Ready D, et al. Unique patterns of comorbidity in posttraumatic stress disorder from different sources of trauma. Compr Psychiatry. 1996;37:336–346. doi: 10.1016/s0010-440x(96)90015-2. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Best CL, et al. Vulnerability-stress factors in development of posttraumatic stress disorder. J Nerv Ment Dis. 1992;180:424–430. doi: 10.1097/00005053-199207000-00004. [DOI] [PubMed] [Google Scholar]
- Briere J, Zaidi Y. Sexual abuse histories and suicide in female psychiatric room patients. Am J Psychiatry. 1989;146:1602–1606. doi: 10.1176/ajp.146.12.1602. [DOI] [PubMed] [Google Scholar]
- Brady KT. Posttraumatic stress disorder and comorbidity: recognizing the many faces of PTSD. J Clin Psychiatry. 1997;58(suppl 9):12–15. [PubMed] [Google Scholar]
- Expert Consensus Guideline Series: Treatment of Posttraumatic Stress Disorder. J Clin Psychiatry. 1999. 60(suppl 16):1–76. [Google Scholar]