Abstract
Approximately one quarter of patients who present to physicians for treatment of chest pain have panic disorder. Panic disorder frequently goes unrecognized and untreated among patients with chest pain, leading to frequent return visits and substantial morbidity. Panic attacks may lead to chest pain through a variety of mechanisms, both cardiac and noncardiac in nature, and multiple processes may cause chest pain in the same patient. Panic disorder is associated with elevated rates of cardiovascular diseases, including hypertension, cardiomyopathy, and, possibly, sudden cardiac death. Furthermore, patients with panic disorder and chest pain have high rates of functional disability and medical service utilization. Fortunately, panic disorder is treatable; selective serotonin reuptake inhibitors, benzodiazepines, and cognitive-behavioral psychotherapy all effectively reduce symptoms. Preliminary studies have also found that treatment of patients who have panic disorder and chest pain with benzodiazepines results in reduction of chest pain as well as relief of anxiety.
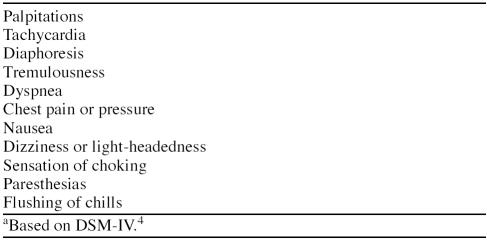
Panic disorder (PD) is a common and potentially disabling psychiatric condition that occurs in 1 to 4 of every 100 people.1–3 PD is manifest by recurrent panic attacks along with persistent worry or behavior change that results from such attacks.4 Patients with PD have increased rates of other psychiatric disorders5,6 and medical illnesses,7–10 as well as substantial functional disability from their symptoms.11–13 Because panic attacks are associated with multiple somatic symptoms that are also seen in common medical conditions (Table 1),4 patients with PD frequently present to primary care and emergency settings, and they use medical services at a much higher rate than do those without PD.14
Table 1.
Somatic Symptoms Associated With Panic Attacksa
Chest pain is a common symptom of panic attacks; 22% to just over 70% of panic attacks are associated with chest pain.15,16 Likewise, between 18% and 25% of all patients who present to emergency departments with chest pain have PD.17,18 Rates of PD are even higher among cardiology outpatients who present for an evaluation of their chest pain.19–21 Such patients often undergo expensive cardiac workups; nevertheless, their PD frequently remains undiagnosed and untreated.17,18 This failure to recognize PD is unfortunate given the profound functional incapacity associated with PD and the array of effective treatments for this condition.
In this article, we review mechanisms by which panic attacks may lead to chest pain and discuss the scope and severity of cardiovascular morbidity associated with PD. We next review the literature describing high rates of functional morbidity and medical service utilization seen in patients having PD; these factors are also discussed with regard to the specific population with PD and chest pain. Finally, we discuss the psychopharmacologic and psychotherapeutic treatment of PD and review treatment studies that specifically focus on patients with PD and chest pain.
MECHANISMS OF CHEST PAIN IN PANIC DISORDER
Panic disorder may cause chest pain via a number of mechanisms. These include cardiac mechanisms (in which pain is caused by coronary spasm or ischemia) and noncardiac mechanisms (in which pain is caused by musculoskeletal, esophageal, or other processes unrelated to the heart). These mechanisms may not exist independent of one another, as there is evidence to suggest that multiple causes of chest pain—both cardiac and noncardiac—may be at work in any given patient with PD.22
Noncardiac Mechanisms
Postulated noncardiac mechanisms for chest pain include musculoskeletal, esophageal, and anxiety-related processes. Hyperventilation during panic attacks may lead to musculoskeletal chest pain, with strain or spasm of intercostal chest wall muscles.23 Esophageal dysmotility can be caused by acute anxiety24; this dysmotility may lead to esophageal spasm, a well-described cause of noncardiac chest pain. In addition, studies have found significant overlap in psychological responses to pain and anxiety,25 and patients suffering from anxiety may interpret their experience as painful.26 Further, as pointed out by Fordyce,27 if patients seek help for this pain experience and get relief from analgesic medications with anxiolytic properties (such as morphine or muscle relaxants), their experience of anxiety as pain is reinforced.
Cardiac Mechanisms
In contrast, panic attacks may lead to chest pain through mechanisms that directly affect coronary vasculature. Both autonomic activation and hyperventilation (via alkalosis) during panic attacks can lead to coronary artery spasm.28,29 This coronary spasm can then lead to myocardial ischemia and cardiac chest pain. Additionally, panic attacks can provoke ischemic pain in patients with coronary disease simply by increasing myocardial oxygen demand through increases in heart rate and blood pressure, mediated by the autonomic nervous system.
Microvascular Ischemia
Small-vessel coronary ischemia also appears to be associated with PD and may be another cardiac mechanism of chest pain. The sympathetic nervous system, one of the essential control mechanisms of small-vessel resistance,30 is activated during panic attacks. This sympathetic activation causes increased microvascular tone in coronary arteries,31 and it appears that panic attacks increase resistance in small cardiac vessels.32 A study of 29 patients with syndrome X (chest pain, a positive exercise stress test, and normal coronary arteries) found that hyperventilation or mental stress reliably produced chest pain in 34% of patients.33 This chest pain was associated with reduced coronary blood flow and was thought to be suggestive of increased microvascular resistance. Such hyperventilation or mental stress during a panic attack may result in increased microvascular tone and chest pain in these patients.
Co-Occurrence of PD and Myocardial Ischemia
Myocardial ischemia and PD may coexist and exacerbate one another during episodes of chest pain. Physiologic changes in cardiorespiratory function during panic attacks can lead to stimulation of the locus ceruleus (a brain territory rich in noradrenergic neurons), causing increases in anxiety and sympathetic tone. Such increased sympathetic tone can lead to tachycardia, hypertension, and myocardial ischemia. The pain of ischemia can then lead to increased anxiety, with further stimulation of the locus ceruleus; a cycle of progressive anxiety and ischemia can result.30,32,34,35 Katon and colleagues20 point out that this pattern can lead to a diagnosis of crescendo angina, as standard antianginal medications may no longer be effective in these circumstances.
Further clouding of the diagnostic and etiologic picture comes from the fact that hyperventilation, a common symptom of panic attacks, induces electrocardiographic (ECG) changes that resemble ischemia in persons both with and without apparent heart disease.36–45 While there are some indications that these are typically false-positive ECG changes,38–40 they may also represent true myocardial ischemia, especially in patients with known coronary artery disease28,46 or coronary artery spasm.28,46–49
Combinations of Mechanisms
In practice, the association of chest pain and PD may result from multiple etiologies, and the same patient may manifest several. A study of patients with chest pain found significant overlap of ECG, esophageal, and psychiatric abnormalities. One third of the patients had ST depression during exercise, two thirds had either esophageal reflux or dysmotility, and one half had scores outside normal ranges on psychological testing.22 Given that patients with PD can have abnormalities of coronary vasculature, esophageal motility, and psychological testing in association with panic attacks, determining the mechanism of chest pain in any given patient with PD can be difficult.
In summary, there are many mechanisms by which PD can lead to chest pain. Such mechanisms can include noncardiac processes such as musculoskeletal pain, esophageal dysmotility, and anxiety itself. In addition, the physiologic effects of a panic attack can lead to coronary artery spasm and small-vessel ischemia, resulting in coronary chest pain. Furthermore, myocardial ischemia and panic attacks can coexist and exacerbate one another through effects on the sympathetic nervous system. Consideration of each of these mechanisms in patients with PD and chest pain will allow for optimal treatment of both panic attacks and associated medical conditions.
CARDIOVASCULAR MORBIDITY AND MORTALITY IN PANIC DISORDER
Studies of patients with PD have found elevated rates of certain cardiovascular disorders, including hypertension, idiopathic cardiomyopathy, microvascular angina, and, possibly, sudden cardiac death.10,35,49–60 Furthermore, some longitudinal studies of patients with PD suggest higher rates of death from cardiovascular causes, especially among men.61–64
Hypertension
Panic disorder appears to be associated with elevated rates of hypertension. Episodic hypertension during panic attacks is common.49–51 Furthermore, in a study of 195 primary care patients, Katon and colleagues10 found significantly higher rates of baseline hypertension in PD patients (13.6%) compared with controls (4.4%). Such hypertension—both during panic attacks and at baseline—may contribute to elevated rates of cardiovascular mortality in this population.
Microvascular Angina
Panic disorder is associated with elevated rates of microvascular angina. Microvascular angina is a condition in which a patient with chest pain has coronary blood flow abnormalities in small cardiac vessels despite normal coronary angiography.52 An association between microvascular angina and PD has been hypothesized because of the reliance of small coronary vessels on the sympathetic nervous system. During a panic attack, there is significant sympathetic discharge, potentially resulting in vasoconstriction of small coronary vessels and microvascular angina. This process can lead to ischemic damage to the myocardium despite the presence of a normal angiogram. This hypothesized association between PD and microvascular angina has been bolstered by a small study in which Roy-Byrne and associates53 found high rates of PD (40%) among 15 patients with microvascular angina.
Cardiomyopathy
Evidence also exists for an association between PD and idiopathic cardiomyopathy. Patients with idiopathic cardiomyopathy have elevated rates of PD, and in these patients the PD often precedes the development of the cardiomyopathy. A study of patients undergoing evaluation for heart transplantation found that 83% of patients with idiopathic cardiomyopathy, compared with 0% to 6% of patients with other diagnoses, met criteria for definite or probable PD.54 Even subclinical cardiomyopathic changes (increased left ventricular mass and size) are found significantly more often in patients with PD than in those without PD.55 It is believed that the increase in peripheral catecholamines produced during panic attacks contributes to cardiomyopathy; this belief is consistent with the observation that catecholamine-producing pheochromocytomas are associated with development of cardiomyopathy.56 Other mechanisms by which PD may cause cardiomyopathy include recurrent tachycardia (with associated dilated cardiomyopathy)57 and microvascular angina (with resulting small-vessel ischemia and cardiomyopathy).35,53 Alternatively, the significant hemodynamic and neuroendocrine changes associated with cardiomyopathy may secondarily cause PD via changes in locus ceruleus activity.35
Sudden Cardiac Death
There also appears to be an association between PD and sudden cardiac death. Sudden cardiac death has been linked to anxiety symptoms in a number of community studies. A large epidemiologic study of 2280 men found that those with 2 or more anxiety symptoms had more than 4 times the risk of sudden cardiac death than did those without such symptoms.58 Three prospective epidemiologic studies59,65,66 have shown that “phobic anxiety” (anxiety similar to the anticipatory anxiety of panic attacks) is associated with a significantly increased risk of sudden cardiac death; these studies have shown that persons with the highest levels of anxiety suffer sudden cardiac death 4 to 6 times more frequently than do those without anxiety symptoms.
The postulated mechanism by which phobic anxiety—and possibly PD—is related to sudden cardiac death involves dysregulation of normal autonomic influence on cardiac activity, as measured by heart rate variability. Decreased heart rate variability suggests pathologic variation in autonomic regulation and is an established risk factor for sudden cardiac death independent of ventricular function or ectopy.67–69 Patients with phobic anxiety have been shown to have decreased heart rate variability,68 and such patients have been found to have rates of sudden cardiac death up to 6 times higher than those for nonanxious patients.59,65,66
Studies of patients with PD have suggested that decreased heart rate variability occurs in this disorder as well. Two studies by Yeragani and colleagues69,70 demonstrated that patients with PD had shown significantly decreased heart rate variability in both supine and standing positions and in response to isoproterenol infusions. Klein and associates71 also found significantly decreased variability in a small study of 10 patients with PD, while 1 study of patients with PD or social phobia found no such differences in heart rate variability.72 Given the link between phobic anxiety, decreased heart rate variability, and sudden cardiac death, it seems quite feasible that PD, with its associated decrease in heart rate variability, may predispose to sudden cardiac death as well.
Overall Cardiovascular Mortality
In addition to links between PD and specific cardiovascular disorders, preliminary evidence exists to show that PD is associated with increased overall cardiovascular mortality. In a 35-year follow-up of 115 former psychiatric inpatients with PD, Coryell and colleagues61,62 found elevated rates of cardiovascular mortality in both men and women, with the incidence in men approximately twice the expected rate (p < .01). Another longitudinal study by Coryell and coworkers63 followed 155 outpatients with anxiety neurosis (a DSM-III diagnosis that appears to encompass both PD and generalized anxiety disorder). They found a similar trend toward elevated cardiovascular mortality in men; however, these findings were not statistically significant given the low overall death rate among the subjects.
As noted by Fleet and Beitman73 in their review of this topic, limitations of these studies include inexact diagnostic methods via chart review, lack of control for comorbid medical conditions, and relatively small numbers of patients. A large community survey of over 5000 persons found that, when demographic characteristics were controlled, patients with PD had a greater risk of myocardial infarction than patients with no psychiatric disorder (odds ratio = 4.5; p < .003).64 This study had the advantage of using structured interviews for the diagnosis of PD; however, it relied on patient self-report of medical conditions. These 3 preliminary studies61–64 suggest a small but significant association between PD and an increased risk of death by cardiovascular causes.
The general trend toward increased cardiovascular mortality among patients with PD may be due to a number of factors. Elevated rates of hypertension, microvascular angina, cardiomyopathy, and, possibly, sudden cardiac death may play a significant role in increasing mortality due to cardiovascular disease. Furthermore, other cardiac risk factors, especially those related to lifestyle, may be more prevalent in patients with PD. A study of 102 patients with PD or agoraphobia found that significantly more women—but not men—with these diagnoses had higher rates of elevated cholesterol than expected.74 Given the profound effects of PD on function and quality of life,11–13,75,76 patients with PD may be less motivated or able to maintain healthy lifestyles; rates of smoking, alcohol consumption, sedentary lifestyle, and poor diet may therefore be higher in these individuals. For instance, increased anxiety sensitivity (the tendency to become dysphoric in the face of symptoms of arousal such as tachycardia and tachypnea) is elevated in patients with panic disorder and may be associated with an aversion to exercise, thus contributing to poor cardiac health.
Further study is indicated to delineate which cardiovascular conditions are more common in PD and to investigate whether rates of lifestyle factors associated with cardiovascular disease are elevated in PD patients. In addition, additional research is needed to follow up the evidence suggesting higher rates of cardiovascular mortality among patients with PD. It is also critical to establish whether treatment of the PD results in normalization of cardiovascular risk.
UTILIZATION OF MEDICAL SERVICES AND FUNCTIONAL MORBIDITY IN PANIC DISORDER
Patients with PD can have extreme anxiety and frequent somatic symptoms as a result of recurrent panic attacks. These patients frequently visit primary care offices and emergency departments with symptoms of their undiagnosed and untreated PD and have difficulties maintaining employment or relationships given the disabling nature of their symptoms.75–82 Low rates of physician recognition and treatment of PD can perpetuate high medical service utilization and result in continued functional disability. At least 35% of patients with PD view their physical and emotional health as fair or poor11; this fact is remarkable given that these patients are frequently young and otherwise healthy.
Medical Service Utilization
A number of studies have examined the use of medical services by patients with PD. Patients with PD frequently present to general medical physicians rather than to mental health providers; more than three quarters are first seen in the emergency room or by a primary care physician.75 Furthermore, it can often take years for a diagnosis of PD to be made. In one report, the average panic patient saw 10 or more physicians before receiving a correct diagnosis.76 Data from the National Institute of Mental Health Epidemiologic Catchment Area Study (ECA)77 showed that outpatient medical services were used significantly more by patients with PD than by patients with and without other psychiatric diagnoses. Additional study has found the rate of PD patients' use of emergency department services to be more than 5 times the rate of use by patients with another psychiatric diagnosis and more than 25 times the rate of patients without a psychiatric diagnosis.11,14,78
Simon and VonKorff79 reported that patients with PD use primary care services approximately 3 times more often than do other patients; further, the odds ratio for patients with PD to have high use of outpatient medical services (defined as 6 or more visits in 6 months) was higher than for any other psychiatric diagnosis. In addition, a large community study found that medical and psychiatric inpatient hospitalizations are significantly more common in patients with PD than in the general population.11 Simpson and associates80 also found high rates of medication use, diagnostic tests, and medical hospitalizations in patients with PD. In that study, the mean number of primary care visits progressively increased each year in the 10 years preceding diagnosis, consistent with the other reports that suggest high rates of medical service utilization in PD and a substantial interval between initial presentation and correct diagnosis.
Functional Morbidity With PD
Studies that have examined quality of life among patients with PD found substantial disability in a variety of psychosocial realms. Data from the ECA77 found that PD patients had significantly higher rates of perceived poor physical health, social disability, marital dysfunction, and financial dependency (with 27% on disability or welfare), as well as greater psychiatric comorbidity with elevated rates of attempted suicide.13 Furthermore, these impairments in perceived health and financial and occupational function were present even in patients with panic attacks but without PD.11 Further analysis of the ECA data found that, among patients with anxiety disorders, PD was associated with the highest rates of unemployment and financial dependence; these effects were independent of comorbid depression.81 Investigations other than the ECA study have confirmed the findings of significant functional disability in patients with PD. A review by Edlund and Swann12 discussed the high social morbidity associated with PD, and Katon and associates,82 in 1995, found that both patients with PD and those with infrequent panic attacks had significantly greater social, family and vocational disability than did controls.
Functional Morbidity With Chest Pain and Normal Coronary Arteries
A number of researchers have also examined functional disability and persistence of symptoms in patients with chest pain and normal coronary arteries, of whom approximately 40% have PD.19–21 Ockene and coworkers83 followed 37 patients with chest pain and normal coronary arteries for 6 to 37 months. At follow-up, 70% of such patients had continued chest pain, 51% reported being unable to work due to their symptoms, and 47% had their usual daily activities limited by chest pain despite normal angiograms. Similarly, Lavey and Winkle84 followed 45 patients with chest pain and normal coronary arteries for a mean of 3.5 years after their normal angiogram. Fully 82% of the patients continued to see physicians for cardiac complaints, and, of the patients whose activities had been limited by symptoms, 79% continued to have functional limitations to the same or greater degree. Finally, a larger study following 1977 chest pain patients without significant coronary artery disease for a mean of 6 years found that 70% of such patients continued to have chest pain over this period, and fully half reported being unable to exert themselves as a result of their symptoms.85
Functional Morbidity With PD and Chest Pain
The above studies suggest that patients with PD and chest pain have substantial functional morbidity, since patients with PD make up a sizeable portion of patients with chest pain and normal coronary arteries. However, no direct study of patients with chest pain and PD was completed until a study by Beitman and colleagues86 in 1991. This study of patients with chest pain and normal coronary angiograms found that patients with PD had greater functional disability at follow-up 38 months later than did those without PD. The patients with PD had high rates of persistent chest pain (72%); 22% found that their chest pain had worsened after their normal angiogram. Further, nearly half (47%) of these patients had difficulty with ordinary activities due to their symptoms, and 31% felt that their general health had worsened over this period. The patients also had work difficulties, missing more than 16 workdays in the previous year due to their symptoms. Despite this significant disability, only one third of the patients were prescribed psychotropic medications, and less than a quarter sought psychiatric care. These rates of persistent chest pain, worsening health perception, and inability to complete daily activities were significantly worse than in matched patients with normal angiograms but no PD. Further, the patients with normal angiograms and PD reported worse social adjustment, higher anxiety, and more psychological distress than their counterparts without PD.
In summary, PD is associated with high rates of medical service utilization and functional disability. Virtually all psychosocial aspects of life are affected by PD, with patients having problems with social, financial, and occupational function. Furthermore, it appears that the specific population of patients having chest pain and PD has similarly high rates of psychosocial morbidity, as well as persistent symptoms that adversely affect function.
TREATMENT OF PANIC DISORDER IN PATIENTS WITH CHEST PAIN
Panic disorder, as described above, can have profound effects on social, financial, and occupational function, as well as on elevated rates of cardiovascular disease. Fortunately, PD is highly treatable, as borne out by a number of trials using both pharmacologic and psychotherapeutic treatments. Selective serotonin reuptake inhibitors (SSRIs),1,87,88 venlafaxine,89 and tricyclic antidepressants90–93 are among the antidepressants with proven efficacy in PD, with rates of response of approximately 50% to 70% over several months. Benzodiazepines,88,94–98 especially alprazolam and clonazepam, have also been proved effective in PD. Furthermore, cognitive-behavioral therapy (CBT), the best studied of the psychotherapies for PD, appears to be comparable to medication in the treatment of PD.99–102 Treatment of patients with PD can be individualized on the basis of a patient's preference for medication or psychotherapy, prior history of response, presence of comorbidity, and severity of symptoms.
Antidepressants
For patients who wish to take medications to treat their PD, SSRIs (e.g., paroxetine, sertraline) are considered a first-line treatment. SSRIs are effective and have a favorable side effect profile, no risk of dependence, and relatively few drug interactions, making them a good choice for patients who are able to tolerate a delay of several weeks before the medication becomes effective. Furthermore, SSRIs effectively treat depression and other comorbid anxiety disorders that frequently co-occur with PD. Because patients may experience initial, usually transient, side effects of jitteriness, shakiness, and increased anxiety when beginning an SSRI, starting doses of these medications are lower than when used for depression, for example, 10 mg/day of paroxetine or fluoxetine or 25 mg/day of sertraline. This dose is maintained for several days, and then increased to standard daily doses of SSRIs, for example 20 mg of paroxetine or fluoxetine. The dose may be increased further if there is no response in several weeks. Compared with the dose and duration of treatment for depression, both higher doses of SSRIs103 and longer waiting periods for full response (8–12 weeks) may be required in the treatment of PD.
Along with treating the symptoms of PD, SSRIs may have favorable effects on the risk of sudden cardiac death by increasing heart rate variability. Tucker and colleagues104 studied 17 patients with PD and found that treatment with paroxetine, 20 mg/day, not only reduced panic attacks but also increased heart rate variability in these patients. Follow-up studies of this promising small trial are indicated to further examine the effects of SSRIs on heart rate variability.
Benzodiazepines
Benzodiazepines are another treatment option for PD. These medications have the advantage of a rapid onset of efficacy, and they can be used to abort ongoing panic attacks. The high-potency benzodiazepines, specifically alprazolam and clonazepam, are frequently used for PD, although it is likely that all benzodiazepines at adequate doses are effective. Clonazepam has a long half-life that limits the frequency of dosing and reduces the likelihood of interdose rebound symptoms, making it useful for maintenance therapy. Clonazepam can be started at 0.25 to 0.5 mg at bedtime and titrated upward; it appears that doses from 1 to 2 mg/day may best balance efficacy and minimization of side effects, although some patients require doses outside this range.97 While there is concern about abuse of benzodiazepines, there is little evidence to suggest that clinically indicated use of these agents leads to either dose escalation or recreational use in patients without an abuse diathesis.105,106 However, benzodiazepines are best avoided in patients with a predisposition to the abuse of alcohol or other substances. Further, benzodiazepines alone are generally ineffective for comorbid depression. SSRIs and benzodiazepines are often used concomitantly in the treatment of PD, combining the rapid effects of benzodiazepines with the long-term therapeutic effects of the antidepressants. The benzodiazepine can be maintained or slowly tapered and discontinued once therapeutic effect has been achieved.
Psychotherapy
Psychotherapeutic approaches to treatment have also been proved effective in PD. These treatments—of which CBT is the best studied—are useful for those patients who do not wish to take medication, and therapeutic response is at least as robust as with pharmacotherapy and potentially longer lasting.98,107–109 CBT comprises psychoeducation, cognitive restructuring, and exposure to stimuli that trigger panic attacks (e.g., physical sensations or feared situations) to reduce symptoms of PD. CBT requires a significant commitment of time and energy by the patient, but it avoids medication side effects and drug interactions.
Treatment Studies in Patients With PD and Chest Pain
These interventions are likely to be beneficial for patients experiencing chest pain as a part of their panic attacks, although such treatments are not well studied in this specific population. Two preliminary studies of benzodiazepines in patients with PD and chest pain have shown promise. In an open-label, flexible-dose trial, Beitman and associates110 administered alprazolam for 8 weeks to 10 cardiology patients with chest pain, normal coronary arteries, and PD. Alprazolam decreased the rate of both chest pain and panic attacks significantly in this population, as 7 of 8 participants who completed the trial had 50% or greater reduction in their panic attack frequency. The patients also had significant improvements on measures of anxiety and depression as well as in Clinical Global Impressions scale scores, suggesting that this intervention not only reduced symptoms but also improved quality of life.
A second study of 27 patients with chest pain, PD, and normal coronary arteries used a double-blind, placebo-controlled, flexible-dose trial of clonazepam for 6 weeks.111 Fifty-eight percent of the clonazepam-treated patients had at least a 50% reduction in their Hamilton Rating Scale for Anxiety score, compared with 14% of placebo-treated patients (p = .038). Further, two thirds of clonazepam-treated patients responded with a reduction of panic attacks to half of their initial frequency compared with 47% of placebo-treated patients. This finding represented a trend that suggested efficacy of clonazepam, but the trend did not reach statistical significance.
These 2 small studies suggest that benzodiazepines, long proved effective in the treatment of PD, also appear effective in the specific population of patients experiencing chest pain and PD. Larger treatment studies of benzodiazepines in this population are warranted, given the potential for reduction in cardiovascular morbidity, functional impairment, and utilization of medical services in these patients. Furthermore, trials studying SSRIs and CBT, the other first-line treatments for PD, are needed to establish the efficacy of these treatments in patients with panic and chest pain.
CONCLUSIONS
Panic disorder is a common and often disabling anxiety disorder with profound effects on quality of life. Chest pain is a common symptom of panic attacks, and persons with PD often present to acute care settings or to cardiologists for evaluation of their chest pain. The postulated mechanisms by which chest pain occurs in patients with PD are varied, and several relevant mechanisms of chest pain may be at work in the same patient. Musculoskeletal and esophageal mechanisms may account for panic-related chest pain, as may interpretation of anxiety as pain. Cardiac mechanisms involving coronary spasm, microvascular vasoconstriction, or worsening of ongoing myocardial ischemia may also result in chest pain during a panic attack.
In addition, PD is associated with elevated rates of comorbid cardiovascular disease, with increased rates of hypertension, cardiomyopathy, microvascular ischemia, and, possibly, sudden cardiac death. This cardiac comorbidity in patients with PD may involve increased catecholamine levels, coronary artery spasm, or autonomic dysregulation as measured by decreased heart rate variability. Further, it appears that patients with PD have increased overall mortality from cardiovascular causes; this increased mortality may be a result of the above cardiovascular disorders or elevations of other risk factors such as smoking or high cholesterol.
It should be emphasized that the observed increases in cardiovascular mortality with PD have been relatively small, and the associated deaths have generally occurred 20 or more years after initial diagnosis of PD. Therefore, patients with PD who are young and otherwise healthy can still be reassured that they are not at imminent risk of an acute cardiovascular event as a result of panic attacks.
Patients with PD utilize medical services at high rates, with substantial elevations in use of emergency services, primary care visits, diagnostic tests, and hospitalizations. Moreover, patients with PD have substantial functional impairment, with high rates of unemployment, financial dependency, and social isolation. This impairment also applies to patients with chest pain and normal coronary arteries who have persistent symptoms and limited function as a result of their chest pain. If this chest pain is associated with PD, such symptom severity and functional limitations appear to be even greater.
Fortunately, an array of effective pharmacologic and psychotherapeutic treatments for PD exists. SSRIs and other antidepressants, benzodiazepines, and CBT have all been found to be beneficial in double-blind trials for PD. In the specific population of patients with PD and chest pain, preliminary studies using benzodiazepines to treat patients with PD and chest pain are promising, with reductions both in overall anxiety and chest pain.
Given the high incidence of PD and the existence of effective treatments, it is imperative that physicians recognize and treat PD in patients presenting with chest pain. Further studies of the mechanisms by which PD causes both chest pain and cardiac morbidity will improve understanding of the relationship between PD and the cardiovascular system. Finally, it is hoped that further treatment studies in this population will delineate effective methods to reduce both the symptoms of PD and its attendant morbidity and mortality.
Drug names: alprazolam (Xanax and others), clonazepam (Klonopin and others), fluoxetine (Prozac and others), paroxetine (Paxil), sertraline (Zoloft), venlafaxine (Effexor).
Footnotes
The authors report no financial affiliation or other relationship relevant to the subject matter of this article.
REFERENCES
- Simon NM, Pollack MH. The current status of the treatment of panic disorder: pharmacotherapy and cognitive-behavioral therapy. Psychiatr Ann. 2000;30:689–696. [Google Scholar]
- Myers JK, Weissmann MM, Tischler GL, et al. Six-month prevalence of psychiatric disorders in three communities: 1980–1982. Arch Gen Psychiatry. 1984;41:959–967. doi: 10.1001/archpsyc.1984.01790210041006. [DOI] [PubMed] [Google Scholar]
- Weissmann MM, Merikangas KR. The epidemiology of anxiety and panic disorders: an update. J Clin Psychiatry. 1986;47(suppl 6):11–17. [PubMed] [Google Scholar]
- NM M. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Press. 1994 397–403. [Google Scholar]
- Bowen R, South M, Hawkes J. Mood swings in patients with panic disorder. Can J Psychiatry. 1994;39:91–94. doi: 10.1177/070674379403900205. [DOI] [PubMed] [Google Scholar]
- Savino M, Perugi G, Simonini E, et al. Affective comorbidity in panic disorder: is there a bipolar connection? J Affect Disord. 1993;28:155–163. doi: 10.1016/0165-0327(93)90101-o. [DOI] [PubMed] [Google Scholar]
- Karajgi B, Rifkin A, Doddi S, et al. The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990;147:200–201. doi: 10.1176/ajp.147.2.200. [DOI] [PubMed] [Google Scholar]
- Kaplan DS, Masand PS, Gupta S. The relationship of irritable bowel syndrome (IBS) and panic disorder. Ann Clin Psychiatry. 1996;8:81–88. doi: 10.3109/10401239609148805. [DOI] [PubMed] [Google Scholar]
- Lydiard RB, Greenwald S, Weissman MM, et al. Panic disorder and gastrointestinal symptoms: findings from the NIMH Epidemiologic Catchment Area project. Am J Psychiatry. 1994;151:64–70. doi: 10.1176/ajp.151.1.64. [DOI] [PubMed] [Google Scholar]
- Katon W, Vitaliano PP, Russo J, et al. Panic disorder: epidemiology in primary care. J Fam Prac. 1986;23:233–239. [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Ouellette R, et al. Panic attacks in the community: social morbidity and health care utilization. JAMA. 1991;265:742–746. [PubMed] [Google Scholar]
- Edlund MJ, Swann AC. The economic and social costs of panic disorder. Hosp Community Psychiatry. 1987;38:1277–1288. doi: 10.1176/ps.38.12.1277. [DOI] [PubMed] [Google Scholar]
- Markowitz J, Weissman MM, Oullette R, et al. Quality of life in panic disorder. Arch Gen Psychiatry. 1989;46:984–992. doi: 10.1001/archpsyc.1989.01810110026004. [DOI] [PubMed] [Google Scholar]
- Katon W. Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J Clin Psychiatry. 1996;57(suppl 10):11–18. [PubMed] [Google Scholar]
- Katon W. Panic disorder and somatization: a review of 55 cases. Am J Med. 1984;77:101–106. doi: 10.1016/0002-9343(84)90443-1. [DOI] [PubMed] [Google Scholar]
- Barlow DB, Vermilyea J, Blanchard EB, et al. The phenomenon of panic. J Abnorm Psychol. 1985;94:320–328. [PubMed] [Google Scholar]
- Fleet RP, DuPuis G, Marchand A, et al. Panic disorder in emergency chest pain patients: prevalence, comorbidity, suicidal ideation, and physician recognition. Am J Med. 1996;101:371–380. doi: 10.1016/S0002-9343(96)00224-0. [DOI] [PubMed] [Google Scholar]
- Yingling KW, Wulsin LR, Arnold LM, et al. Estimated prevalences of panic disorder and depression among consecutive patients seen in an emergency department with acute chest pain. J Gen Int Med. 1993;8:231–235. doi: 10.1007/BF02600087. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Dupuis G, Marchand A, et al. Detecting panic disorder in emergency department chest pain patients: a validated model to improve recognition. Ann Behav Med. 1997;19:124–131. doi: 10.1007/BF02883329. [DOI] [PubMed] [Google Scholar]
- Katon W, Hall ML, Russo J, et al. Chest pain: relationship of psychiatric illness to coronary arteriographic results. Am J Med. 1988;84:1–9. doi: 10.1016/0002-9343(88)90001-0. [DOI] [PubMed] [Google Scholar]
- Cormier LE, Katon W, Russo, et al. Chest pain with negative diagnostic studies: relationship to psychiatric illness. J Nerv Ment Dis. 1988;176:351–358. doi: 10.1097/00005053-198806000-00004. [DOI] [PubMed] [Google Scholar]
- Cooke RA, Chambers JB, Anggiansah A, and et al. Chest pain and normal coronary arteries: a clinical evaluation with esophageal function tests, exercise ECG, end-tidal CO2 measurement and psychiatric scores. Eur Heart J. 1991 12(suppl). 103–108.2044542 [Google Scholar]
- Potts AG, Bass C. Chest pain with normal coronary arteries: psychological aspects. In: Kaski JC, ed. Chest Pain With Normal Coronary Angiograms. Norwell, Mass: Kluwer Academic Publishers. 1999 13–32. [Google Scholar]
- Young LD. The effect of psychological and environmental stressors on peristaltic esophageal contractions in healthy volunteers. Psychophysiology. 1987;24:132–141. doi: 10.1111/j.1469-8986.1987.tb00265.x. [DOI] [PubMed] [Google Scholar]
- Gross RT, Collins FC. On the relationship between anxiety and pain: a methodological confounding. Clin Psychol Rev. 1981;1:375–386. [Google Scholar]
- Cinciripini PM, Williamson D, and Epstein LH. The behavioral treatment of migraine headaches. In: Taylor CB, Ferguson J, eds. Comprehensive Textbook of Behavioral Medicine. New York, NY: SP Medical and Scientific Books. 1993 207–227. [Google Scholar]
- Fordyce WE. Behavioral Methods for Chronic Pain and Illness. St. Louis, Mo: Mosby. 1976 24–28. [Google Scholar]
- Yasue H, Nagao M, Omote S, et al. Coronary arterial spasm and Prinzmetal's variant of angina induced by hyperventilation and Tris-buffer infusion. Circulation. 1978;58:56–62. doi: 10.1161/01.cir.58.1.56. [DOI] [PubMed] [Google Scholar]
- Rasmussen K, Ravnsbaek J, Funch-Jensen P. Esophageal spasm in patients with coronary artery spasm. Lancet. 1986;1:174–176. doi: 10.1016/s0140-6736(86)90651-3. [DOI] [PubMed] [Google Scholar]
- Katon WJ. Chest pain, cardiac disease, and panic disorder. J Clin Psychiatry. 1990;51(suppl 5):27–30. [PubMed] [Google Scholar]
- Bohlen HG. Arteriolar closure mediated by hyper-responsiveness to norepinephrine in hypertensive rats. Am J Physiol. 1979;236:H157–H164. doi: 10.1152/ajpheart.1979.236.1.H157. [DOI] [PubMed] [Google Scholar]
- Katon W, Roy-Byrne PP. Panic disorder in the medically ill. J Clin Psychiatry. 1989;50:299–302. [PubMed] [Google Scholar]
- Chauhan A, Mullins PA, Taylor G, et al. Effect of hyperventilation and mental stress on coronary blood flow in syndrome X. Br Heart J. 1993;69:516–524. doi: 10.1136/hrt.69.6.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svensson TH. Peripheral, autonomic regulation of the locus coeruleus neurons in the brain: putative implications for psychiatric illness and psychopharmacology. Psychopharmacology (Berl) 1987;92:1–7. doi: 10.1007/BF00215471. [DOI] [PubMed] [Google Scholar]
- Zaubler TS, Katon W. Panic disorder and medical comorbidity: a review of the medical and psychiatric literature. Bull Menninger Clin. 1996;60(suppl 2A):A12–A38. [PubMed] [Google Scholar]
- Aronson PR. Hyperventilation syndrome: a comparative study of the effects of tranquilizers and a sedative upon the electrocardiogram. Clin Pharmacol Ther. 1964;5:553–562. doi: 10.1002/cpt196455553. [DOI] [PubMed] [Google Scholar]
- Biberman L, Sarma RN, Surawicz B. T-wave abnormalities during hyperventilation and isoproterenol infusion. Am Heart J. 1971;81:166–174. doi: 10.1016/0002-8703(71)90127-x. [DOI] [PubMed] [Google Scholar]
- Jacobs WF, Battle WE, Ronan JA. False-positive ST-T wave changes secondary to hyperventilation and exercise: a cineangiographic correlation. Ann Intern Med. 1974;81:479–482. doi: 10.7326/0003-4819-81-4-479. [DOI] [PubMed] [Google Scholar]
- Lary D, Goldschlager N. Electrocardiogram changes during hyperventilation resembling myocardial ischemia in patients with normal coronary arteriograms. Am Heart J. 1974;87:383–390. doi: 10.1016/0002-8703(74)90081-7. [DOI] [PubMed] [Google Scholar]
- McHenry PL, Cogan OJ, Elliott WC, et al. False positive ECG response to exercise secondary to hyperventilation: cineangiographic correlation. Am Heart J. 1970;79:683–687. doi: 10.1016/0002-8703(70)90288-7. [DOI] [PubMed] [Google Scholar]
- Wasserburger RH, Lorenz TH. The effect of hyperventilation and Pro-Banthine on isolated RS-T segment T-wave abnormalities. Am Heart J. 1956;51:666–669. doi: 10.1016/s0002-8703(56)80004-5. [DOI] [PubMed] [Google Scholar]
- Wasserberger RH, Siebecker KL, Lewis WC. The effect of hyperventilation on the normal adult electrocardiogram. Circulation. 1956;13:850–854. doi: 10.1161/01.cir.13.6.850. [DOI] [PubMed] [Google Scholar]
- Wenkos MH, Logue RB. Unstable T waves in leads II and III in persons with neurocirculatory asthenia. Am Heart J. 1946;31:711–713. doi: 10.1016/0002-8703(46)90498-x. [DOI] [PubMed] [Google Scholar]
- Thompson WP. The electrocardiogram in the hyperventilation syndrome. Am Heart J. 1943;25:372–379. [Google Scholar]
- Scherf D, Schlachman M. The electrocardiographic changes caused by hyperventilation. Am J Med Sci. 1947;213:342–347. [PubMed] [Google Scholar]
- Yasue H, Omote S, Takizawa A, et al. Comparison of coronary arteriographic findings during angina pectoris associated with S-T elevation or depression. Am J Cardiol. 1981;47:539–546. doi: 10.1016/0002-9149(81)90536-1. [DOI] [PubMed] [Google Scholar]
- Mortensen SA, Vilhelmson R, Sande E. Prinzmetal's variant of angina (PVA): circadian variation in response to hyperventilation. Acta Med Scand Suppl. 1981;644:38–41. doi: 10.1111/j.0954-6820.1981.tb03116.x. [DOI] [PubMed] [Google Scholar]
- Neill WA, Hattenhauer M. Impairment of myocardial oxygen supply due to hyperventilation. Circulation. 1975;52:854–858. doi: 10.1161/01.cir.52.5.854. [DOI] [PubMed] [Google Scholar]
- Balon R, Ortiz A, Pohl R, et al. Heart rate and blood pressure during placebo-associated panic attacks. Psychosom Med. 1988;50:434–438. doi: 10.1097/00006842-198807000-00010. [DOI] [PubMed] [Google Scholar]
- Freedman RR, Ianni P, Ettegui E, et al. Ambulatory monitoring of panic disorder. Arch Gen Psychiatry. 1985;42:244–248. doi: 10.1001/archpsyc.1985.01790260038004. [DOI] [PubMed] [Google Scholar]
- White WB, Baker CH. Episodic hypertension secondary to panic disorder. Arch Int Med. 1986;146:1129–1130. [PubMed] [Google Scholar]
- Cannon RO, Watson RM, Rosing DR, et al. Angina caused by reduced vasodilator reserve of the small coronary arteries. J Am Coll Cardiol. 1983;1:1359–1373. doi: 10.1016/s0735-1097(83)80037-0. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Schmidt P, Cannon RO, et al. Microvascular angina and panic disorder. Int J Psychiatry Med. 1989;19:315–325. doi: 10.2190/5j4t-penr-2g3f-aue0. [DOI] [PubMed] [Google Scholar]
- Kahn JP, Drusin RE, Klein DF. Idiopathic cardiomyopathy and panic disorder: clinical association in cardiac transplant candidates. Am J Psychiatry. 1987;144:1327–1330. doi: 10.1176/ajp.144.10.1327. [DOI] [PubMed] [Google Scholar]
- Kahn JP, Gorman JM, King DL, et al. Cardiac left ventricular hypertrophy and chamber dilatation in panic disorder patients: implications for idiopathic dilated cardiomyopathy. Psychiatry Res. 1990;321:55–61. doi: 10.1016/0165-1781(90)90135-r. [DOI] [PubMed] [Google Scholar]
- Van Vleit PD, Burchell HB, Titus JL. Focal myocarditis associated with pheochromocytoma. N Engl J Med. 1966;274:1102–1108. doi: 10.1056/NEJM196605192742002. [DOI] [PubMed] [Google Scholar]
- Gillette PC, Smith RT, Garson A, et al. Chronic supraventricular tachycardia: a curable cause of congestive cardiomyopathy. JAMA. 1985;253:391–392. doi: 10.1001/jama.253.3.391. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Sparrow D, Vokonas PS, et al. Symptoms of anxiety and risk of coronary heart disease: the Normative Aging Study. Circulation. 1994;90:2225–2229. doi: 10.1161/01.cir.90.5.2225. [DOI] [PubMed] [Google Scholar]
- Haines AP, Imeson JD, Meade TW. Phobic anxiety and ischaemic heart disease. Br Med J. 1987;295:297–299. doi: 10.1136/bmj.295.6593.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Colditz GA, Acherio A, et al. Prospective study of phobic anxiety and risk of coronary heart disease in men. Circulation. 1994;89:1992–1997. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- Coryell W. Panic disorder and mortality. Psychiatr Clin North Am. 1988;2:433–440. [PubMed] [Google Scholar]
- Coryell W, Noyes R, Clancy J. Excess mortality in panic disorder: a comparison with primary unipolar depression. Arch Gen Psychiatry. 1982;139:701–703. doi: 10.1001/archpsyc.1982.04290060051010. [DOI] [PubMed] [Google Scholar]
- Coryell W, Noyes R, House JD. Mortality among outpatients with anxiety disorders. Am J Psychiatry. 1986;143:508–510. doi: 10.1176/ajp.143.4.508. [DOI] [PubMed] [Google Scholar]
- Weissmann MM, Markowitz JS, Ouellette MD, et al. Panic disorder and cardiovascular/cerebrovascular problems: results from a community survey. Am J Psychiatry. 1990;147:1504–1508. doi: 10.1176/ajp.147.11.1504. [DOI] [PubMed] [Google Scholar]
- Van Ravenswaaij-Arts CA, Kollee LA, Hopman JW, et al. Heart rate variability. Ann Intern Med. 1993;119:436–447. doi: 10.7326/0003-4819-118-6-199303150-00008. [DOI] [PubMed] [Google Scholar]
- Myerberg RJ, Kessler KM, Castellanos A. Sudden cardiac death: epidemiology, transient risk, and intervention assessment. Ann Intern Med. 1993;119:1187–1197. doi: 10.7326/0003-4819-119-12-199312150-00006. [DOI] [PubMed] [Google Scholar]
- Odemuyiwa O, Malik M, Farrell T, et al. Comparison of the predictive characteristics of heart rate variability index and left ventricular ejection fraction for all-cause mortality, arrhythmic events, and sudden death after acute myocardial infarction. Am J Cardiol. 1991;68:434–439. doi: 10.1016/0002-9149(91)90774-f. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Sparrow D, Vokonas PS. Decreased heart rate variability in men with phobic anxiety (data from the Normative Aging Study) Am J Cardiol. 1995;175:882–885. doi: 10.1016/s0002-9149(99)80680-8. [DOI] [PubMed] [Google Scholar]
- Yeragani VK, Rohl R, Berger R, et al. Decreased heart rate variability in panic disorder patients: a study of power-spectral analysis of heart rate. Psychiatry Res. 1993;46:89–103. doi: 10.1016/0165-1781(93)90011-5. [DOI] [PubMed] [Google Scholar]
- Yeragani VK, Rohl R, Srinivasan K, et al. Effects of isoproterenol infusions on heart rate variability in patients with panic disorder. Psychiatry Res. 1995;56:289–293. doi: 10.1016/0165-1781(95)02608-y. [DOI] [PubMed] [Google Scholar]
- Klein E, Cnaai E, Harel T, et al. Altered heart rate variability in panic disorder patients. Biol Psychiatry. 1995;37:18–24. doi: 10.1016/0006-3223(94)00130-U. [DOI] [PubMed] [Google Scholar]
- Asmundson GJG, Stein MB. Vagal attenuation in panic disorder: an assessment of parasympathetic nervous system function and subjective reactivity to respiratory manipulations. Psychosom Med. 1994;56:187–193. doi: 10.1097/00006842-199405000-00002. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Beitman BD. Cardiovascular death from panic disorder and panic-like anxiety: a critical review of the literature. J Psychsom Res. 1998;44:71–80. doi: 10.1016/s0022-3999(97)00135-9. [DOI] [PubMed] [Google Scholar]
- Hayward C, Taylor CB, Roth WT, et al. Plasma lipid levels in patients with panic disorder or agoraphobia. Am J Psychiatry. 1989;146:917–919. doi: 10.1176/ajp.146.7.917. [DOI] [PubMed] [Google Scholar]
- Katerndahl DA, Realini JP. Where do panic attack sufferers seek care? J Fam Pract. 1995;40:237–243. [PubMed] [Google Scholar]
- Sheehan DV, Ballenger JC, Jacobsen G. Treatment of endogenous anxiety with phobic, hysterical, and hypochondriacal symptoms. Arch Gen Psychiatry. 1980;37:51–59. doi: 10.1001/archpsyc.1980.01780140053006. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Kessler LG. eds. Epidemiologic Field Methods in Psychiatry: The NIMH Epidemiologic Catchment Area Program. Orlando, Fla: Academic Press. 1985 20–45. [Google Scholar]
- Regier DA, Myers JK, Kramer M, et al. The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41:934–941. doi: 10.1001/archpsyc.1984.01790210016003. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M. Somatization and psychiatric disorder in the Epidemiologic Catchment Area study. Am J Psychiatry. 1991;148:1494–1500. doi: 10.1176/ajp.148.11.1494. [DOI] [PubMed] [Google Scholar]
- Simpson RJ, Kazmierczak T, Power KG, et al. Controlled comparison of patients with panic disorder. Br J Gen Pract. 1994;44:352–356. [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Portera L, Weissmann MM. The social costs of panic disorder. Br J Psychiatry. 1995;166(suppl 27):19–22. [PubMed] [Google Scholar]
- Katon W, Hollifield M, Chapman T, et al. Infrequent panic attacks: psychiatric comorbidity, personality characteristics, and functional disability. J Psychiatr Res. 1995;29:121–131. doi: 10.1016/0022-3956(95)00006-q. [DOI] [PubMed] [Google Scholar]
- Ockene IS, Shay MJ, Alpert JS, et al. Unexplained chest pain in patients with normal coronary arteriograms. N Engl J Med. 1980;303:1249–1252. doi: 10.1056/NEJM198011273032201. [DOI] [PubMed] [Google Scholar]
- Lavey EB, Winkle RA. Continuing disability of patients with chest pain and normal coronary arteriograms. J Chronic Dis. 1979;32:191–196. doi: 10.1016/0021-9681(79)90064-x. [DOI] [PubMed] [Google Scholar]
- Papanicolaou MN, Califf RM, Hlatky MA, et al. Prognostic implications of angiographically normal and insignificantly narrowed coronary arteries. Am J Cardiol. 1986;58:1181–1187. doi: 10.1016/0002-9149(86)90378-4. [DOI] [PubMed] [Google Scholar]
- Beitman BD, Kushner MG, Basha I, et al. Follow-up status of patients with angiographically normal coronary arteries and panic disorder. JAMA. 1991;265:1545–1549. [PubMed] [Google Scholar]
- Jobson KO, Davidson JRT, Lydiard BR, et al. Algorithm for treatment of panic disorder with agoraphobia. Psychopharmacol Bull. 1995;31:483–485. [PubMed] [Google Scholar]
- Rosenbaum JF, Pollack MH, and Fredman SJ. The pharmacotherapy of panic disorder. In: Rosenbaum JF, Pollack MH, eds. Panic Disorder and Its Treatment. New York, NY: Marcel Dekker. 1998 153–180. [Google Scholar]
- Pollack MH, Worthington JJ, Otto MW, et al. Venlafaxine for panic disorder: results from a double-blind, placebo-controlled study. Psychopharmacol Bull. 1996;32:667–670. [PubMed] [Google Scholar]
- NM M. Cross-National Collaborative Panic Study SPI. Drug treatment of panic disorder: comparative efficacy of alprazolam, imipramine, and placebo. Br J Psychiatry. 1992;160:191–205. doi: 10.1192/bjp.160.2.191. [DOI] [PubMed] [Google Scholar]
- Lydiard RB, Morton WA, Emmanuel NP, et al. Preliminary report: placebo-controlled, double-blind study of the clinical and metabolic effects of desipramine in panic disorder. Psychopharmacol Bull. 1993;29:183–188. [PubMed] [Google Scholar]
- Zitrin CM, Klein DF, Woerner MG, et al. Treatment of phobias, I: comparison of imipramine hydrochloride and placebo. Arch Gen Psychiatry. 1980;37:63–72. doi: 10.1001/archpsyc.1983.01790020019002. [DOI] [PubMed] [Google Scholar]
- Uhlenhuth EH, Matuzas W, Glass RM. Response of panic disorder to fixed doses of alprazolam or imipramine. J Affect Disord. 1989;17:261–270. doi: 10.1016/0165-0327(89)90009-8. [DOI] [PubMed] [Google Scholar]
- Dunner DL, Ishiki D, Avery DH, et al. Effect of alprazolam and diazepam in anxiety and panic attacks in panic disorder: a controlled study. J Clin Psychiatry. 1986;47:458–460. [PubMed] [Google Scholar]
- Tesar GE, Rosenbaum JF, Pollack MH, et al. Double-blind, placebo-controlled comparison of clonazepam and alprazolam for panic disorder. J Clin Psychiatry. 1991;52:69–76. [PubMed] [Google Scholar]
- Charney DS, Woods SW. Benzodiazepine treatment of panic disorder: a comparison of alprazolam and lorazepam. J Clin Psychiatry. 1989;50:418–423. [PubMed] [Google Scholar]
- Rosenbaum JF, Moroz G, and Bowden CL. for the Clonazepam Panic Disorder Dose-Response Study Group. Clonazepam in the treatment of panic disorder with or without agoraphobia: a dose-response study of efficacy, safety, and discontinuance. J Clin Psychopharmacol. 1997 17:390–400. [DOI] [PubMed] [Google Scholar]
- Worthington JJ III, Pollack MH, Otto MW, et al. Long-term experience with clonazepam in patients with a primary diagnosis of panic disorder. Psychopharmacol Bull. 1998;34:199–205. [PubMed] [Google Scholar]
- Craske MG, Brown TA, Barlow DA. Behavioral treatment of panic disorder: a two-year follow-up. Behav Ther. 1991;22:289–304. [Google Scholar]
- Klosko JS, Barlow DS, Tassarini R, et al. A comparison of alprazolam and behavior therapy in treatment of panic disorder. J Consult Clin Psychol. 1990;58:77–84. doi: 10.1037//0022-006x.58.1.77. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Lucas JA, Schimdt NB, et al. Group cognitive-behavioral treatment of panic disorder. Behav Res Ther. 1993;31:279–287. doi: 10.1016/0005-7967(93)90026-q. [DOI] [PubMed] [Google Scholar]
- Ost LG, Wesling BE. Applied relaxation vs cognitive behavior therapy in the treatment of panic disorder. Behav Res Ther. 1995;33:145–158. doi: 10.1016/0005-7967(94)e0026-f. [DOI] [PubMed] [Google Scholar]
- Ballenger JC, Wheadon DE, Steiner M, et al. Double-blind, fixed-dose, placebo-controlled study of paroxetine in the treatment of panic disorder. Am J Psychiatry. 1998;155:36–42. doi: 10.1176/ajp.155.1.36. [DOI] [PubMed] [Google Scholar]
- Tucker P, Adamson P, Miranda R Jr, et al. Paroxetine increases heart rate variability in panic disorder. J Clin Psychopharmacol. 1997;17:370–376. doi: 10.1097/00004714-199710000-00006. [DOI] [PubMed] [Google Scholar]
- Nagy LM, Krystal JH, Woods SW. Clinical and medication outcome after short-term alprazolam and behavioral group treatment of panic disorder: 2.5 year naturalistic follow-up. Arch Gen Psychiatry. 1989;46:993–999. doi: 10.1001/archpsyc.1989.01810110035005. [DOI] [PubMed] [Google Scholar]
- Noyes R Jr, Borrows GD, Reich JH, et al. Diazepam versus alprazolam for the treatment of panic disorder. J Clin Psychiatry. 1996;57:349–355. [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, et al. A comparison of cognitive therapy, applied relaxation, and imipramine in the treatment of panic disorder. Br J Psychiatry. 1994;164:759–769. doi: 10.1192/bjp.164.6.759. [DOI] [PubMed] [Google Scholar]
- Fava GA, Zielezny M, Savron G, et al. Long-term effects of behavioural treatment for panic disorder with agoraphobia. Br J Psychiatry. 1995;166:87–92. doi: 10.1192/bjp.166.1.87. [DOI] [PubMed] [Google Scholar]
- Gould R, Otto MW, Pollack MH. A meta-analysis of treatment outcome for panic disorder. Clin Psychol Rev. 1995;15:819–844. [Google Scholar]
- Beitman BD, Basha IM, Trombka LH, et al. Alprazolam in the treatment of cardiology patients with atypical chest pain and panic disorder. J Clin Psychopharmacol. 1988;8:127–130. [PubMed] [Google Scholar]
- Wulsin LR, Maddock R, Beitman B, et al. Clonazepam treatment of panic disorder in patients with recurrent chest pain and normal coronary arteries. Int J Psychiatry Med. 1999;29:97–105. doi: 10.2190/X6N2-8HYG-7LLJ-X6U2. [DOI] [PubMed] [Google Scholar]