Abstract
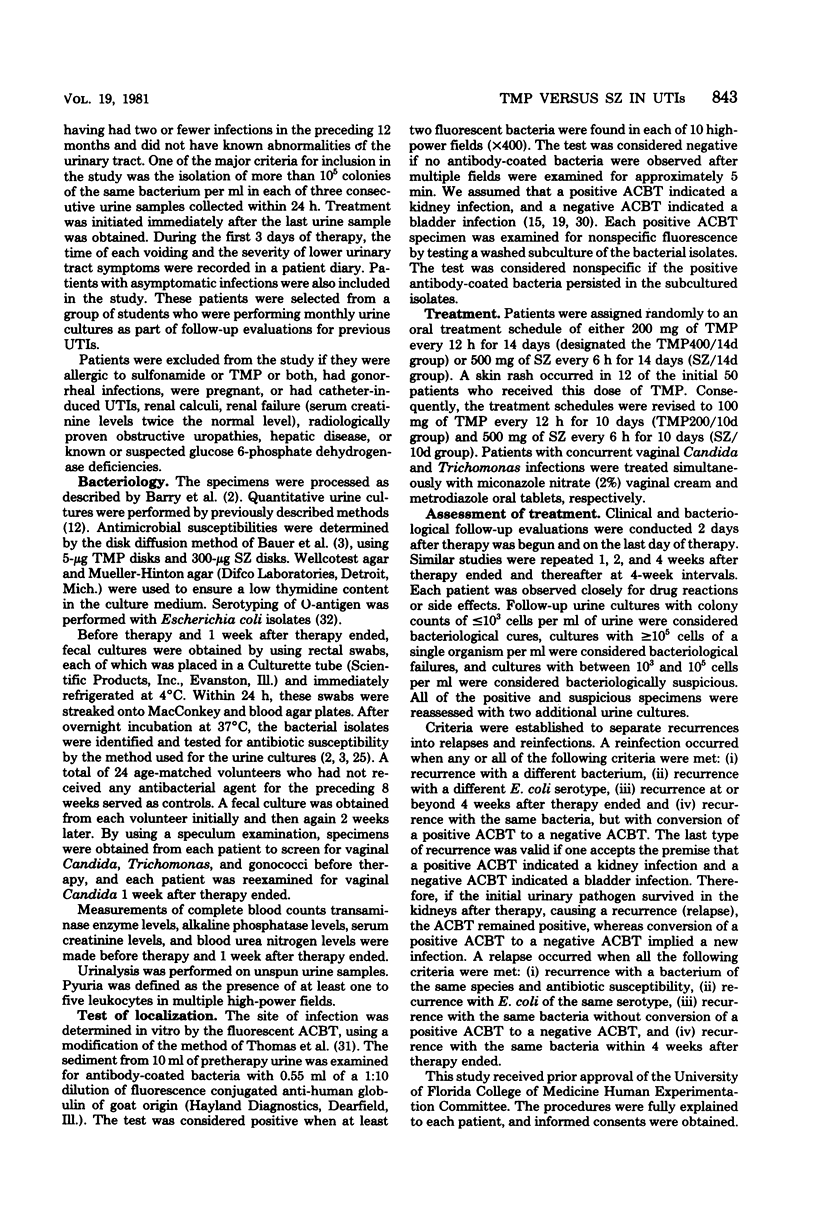
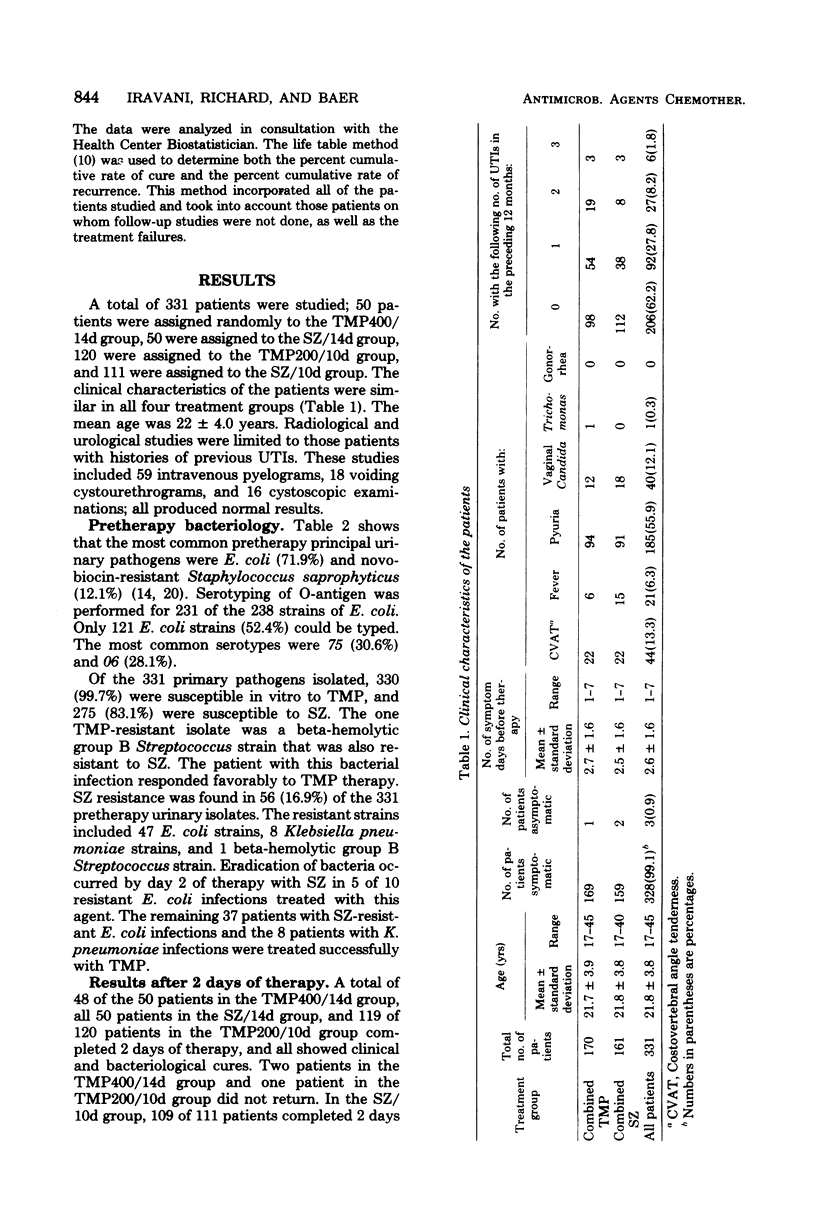
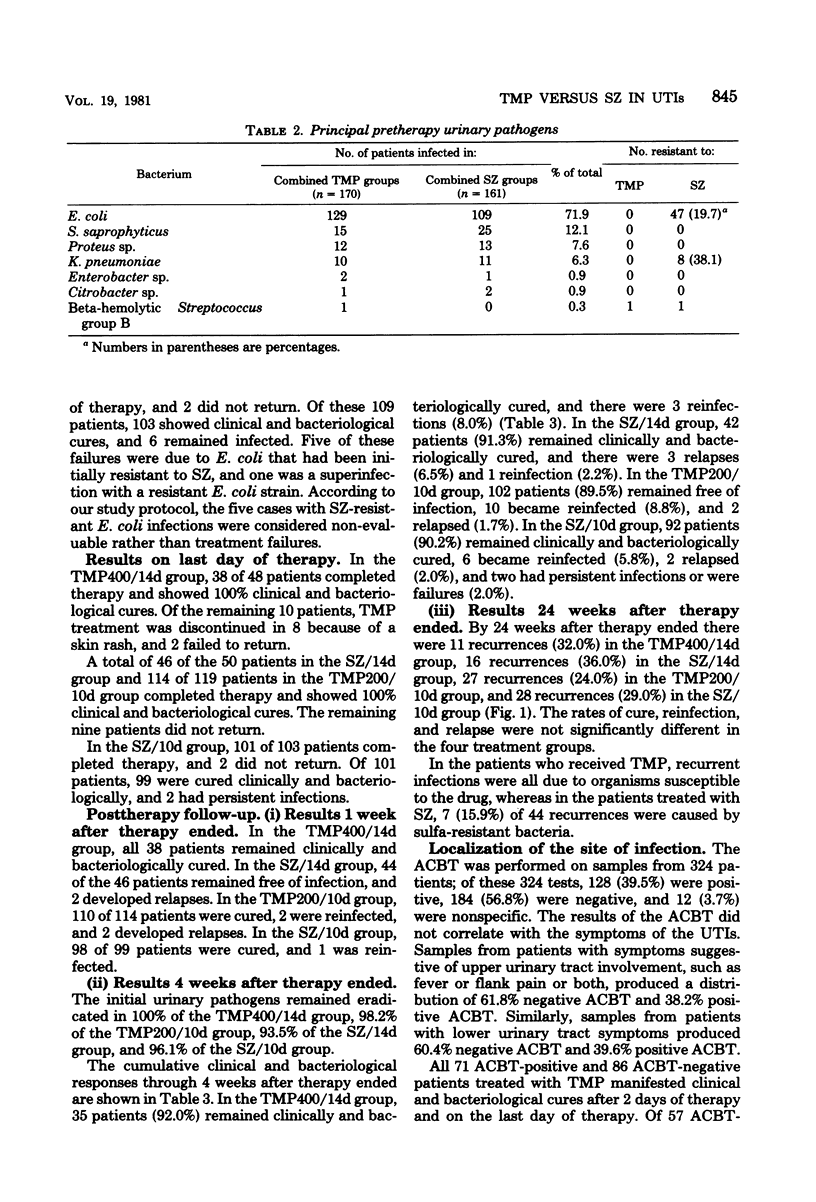
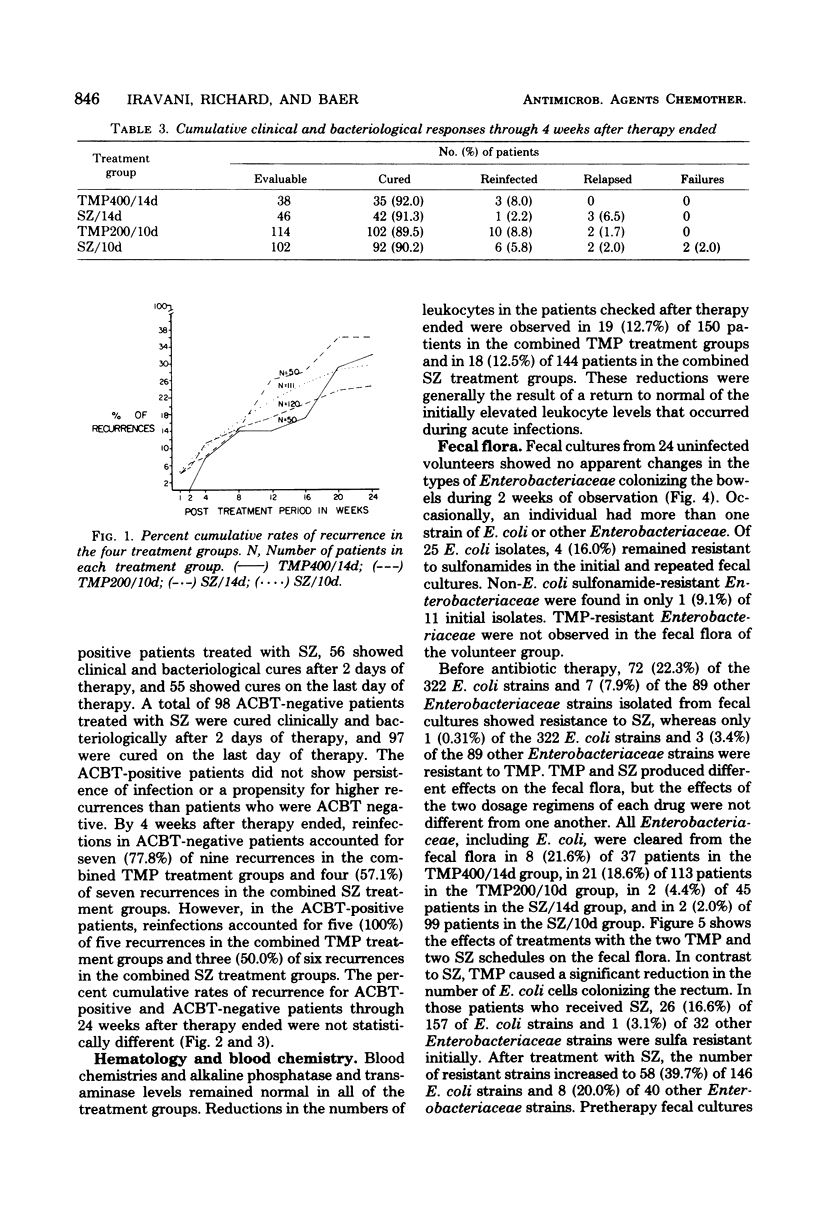
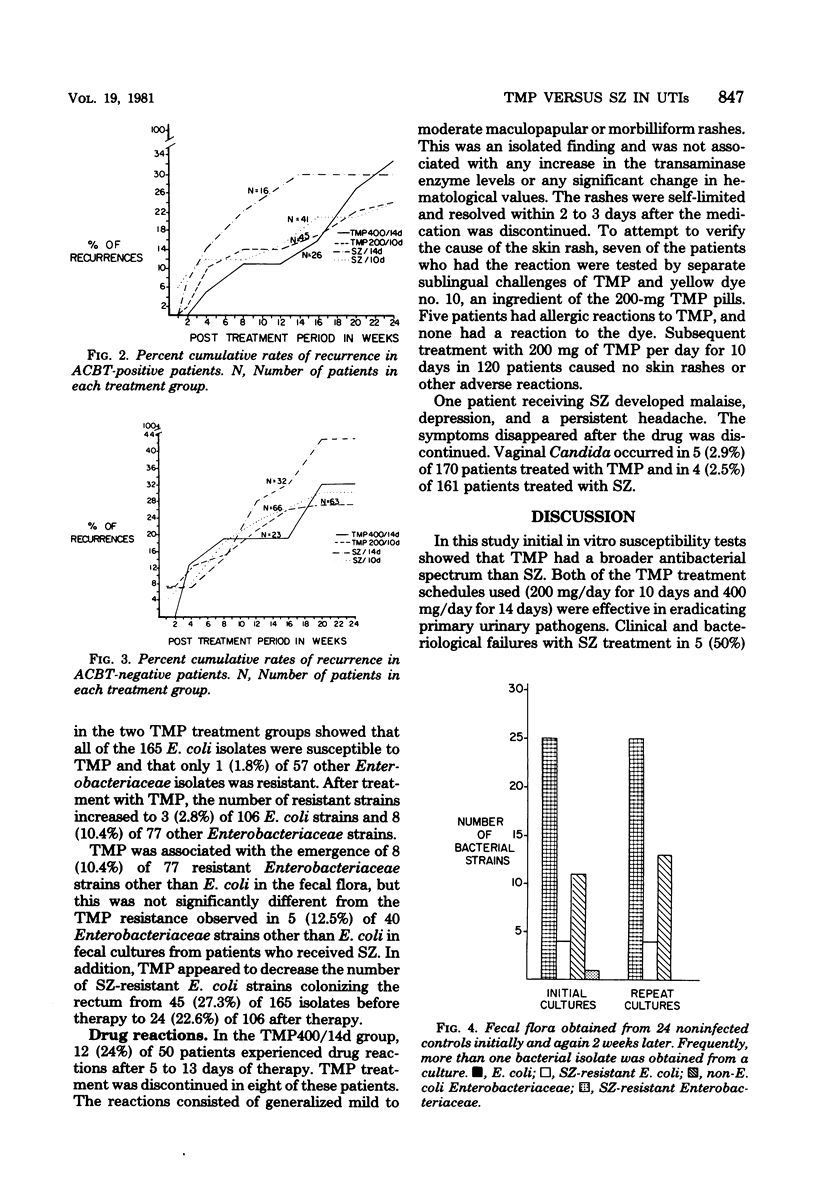
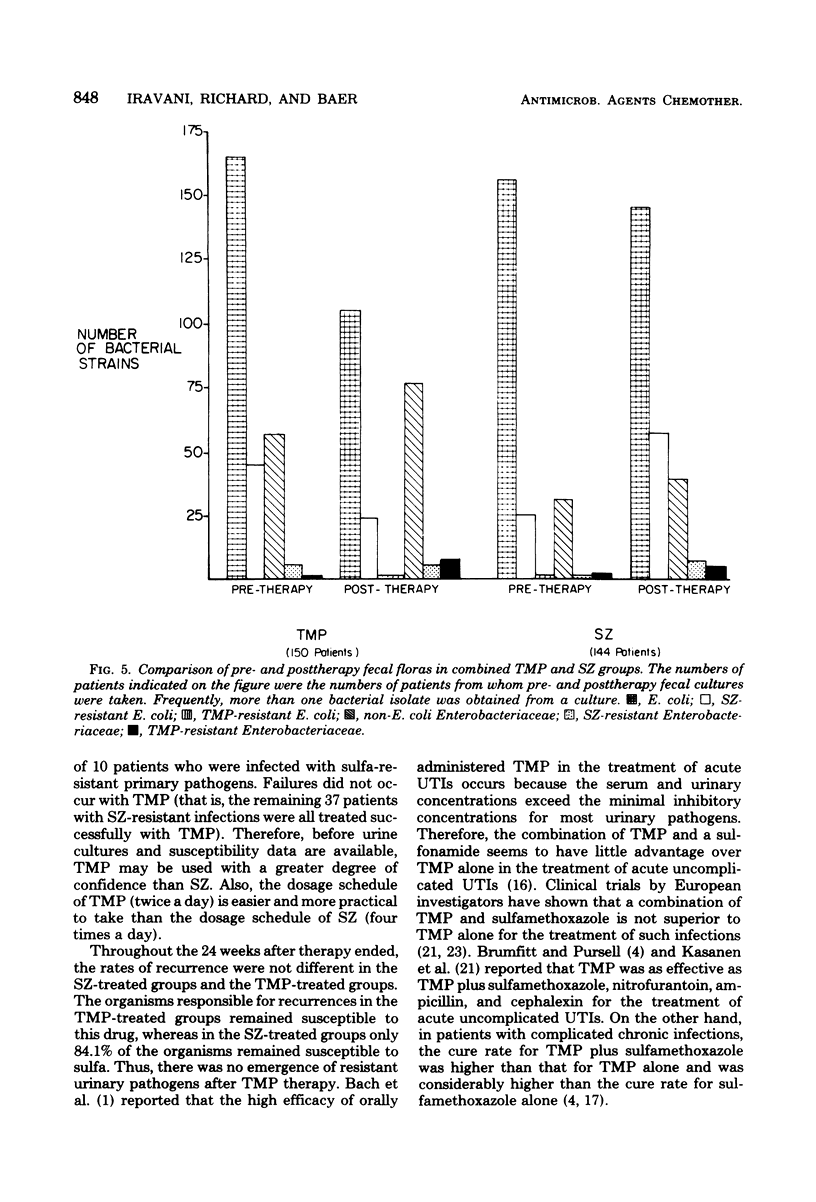
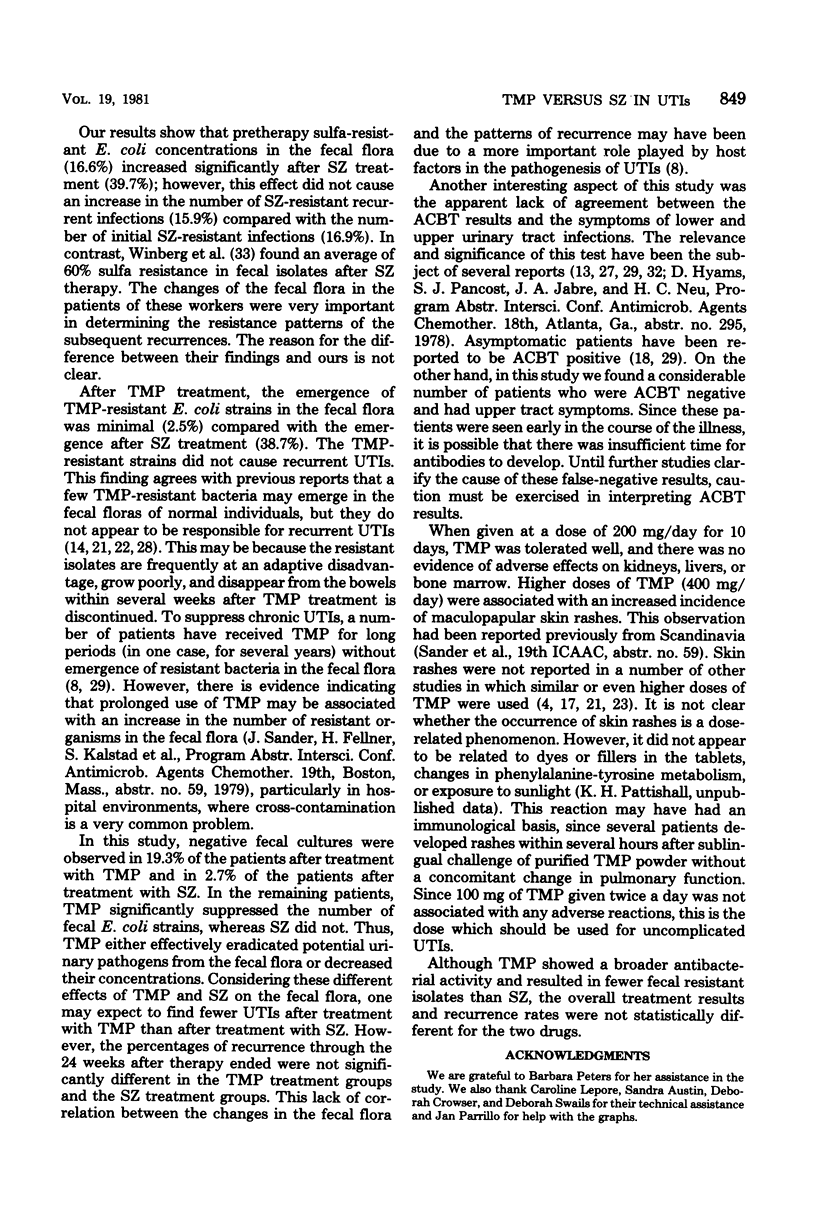
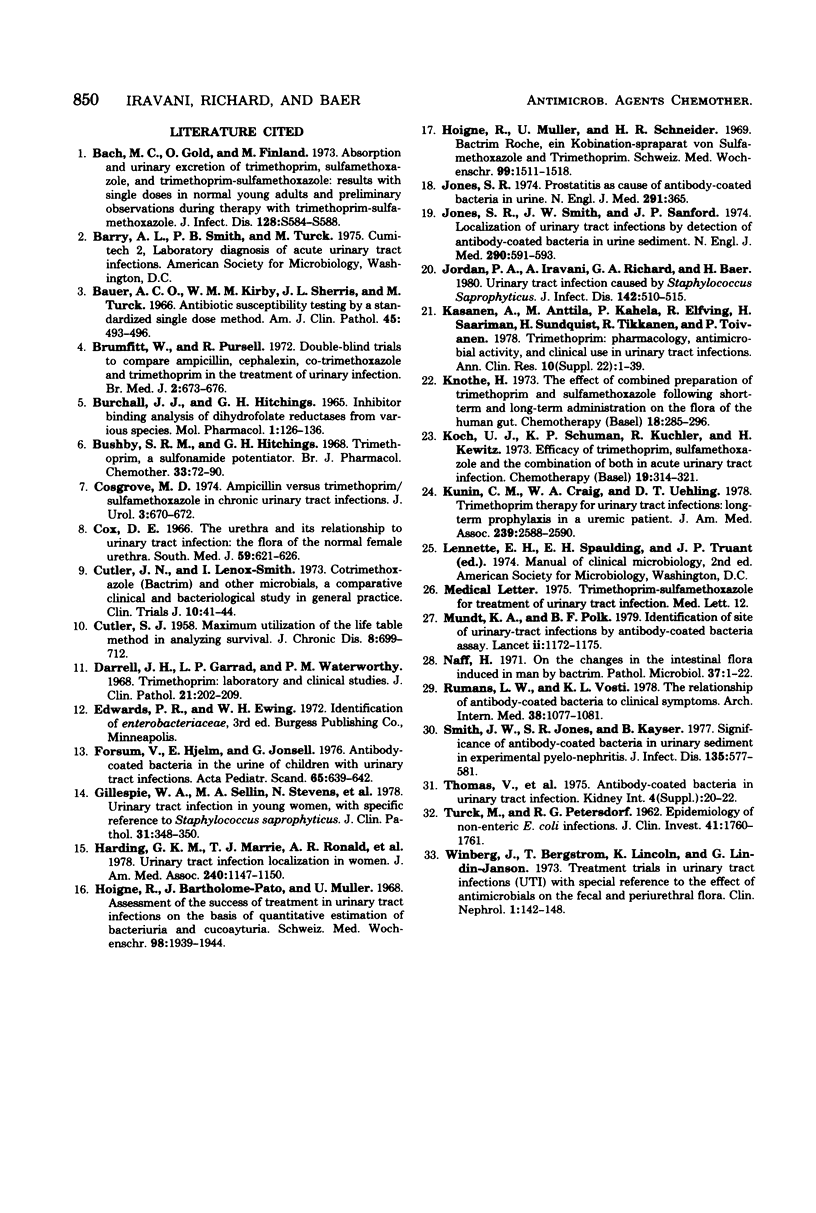
A total of 331 college-age women with urinary tract infections were studied. These women were assigned randomly to the following groups: 50 patients treated with 400 mg of trimethoprim (TMP) per day for 14 days (designated the TMP400/14d group); 50 treated with 2.0 g of sulfisoxazole (SZ) per day for 14 days (SZ/14d group); 120 treated with 200 mg of TMP per day for 10 days (TMP200/10d group); and 111 treated with 2.0 g of SZ per day for 10 days (SZ/10d group). By the last day of therapy, clinical and bacteriological cure rates were 100% in the TMP400/14d, SZ/14d, and TMP200/10d groups and 97.1% in SZ/10d group. At 1 week after therapy ended, the initial urinary pathogens remained eradicated in 100% of the TMP400/14d group, 98.2% of the TMP200/10d group, 95.6% of the SZ/14d group, and 98.0% of the SZ/10d group at 4 weeks after therapy ended, the clinical cure rates were 92.0% in the TMP400/14d group, 92.0% in the SZ/14d group, 89.0% in the TMP200/10d group, and 90.0% in the SZ/10d group. At 4 and 24 weeks after therapy ended, the recurrence rates in the four treatment groups did not differ significantly. The antibody-coated bacteria test localized 39.5% of the infections to kidneys and 56.8% of the infections to bladders. Neither symptoms nor responses to therapy were correlated with the antibody-coated bacteria test results. Both TMP at a dose of 200 mg/day and SZ were tolerated well. TMP at a dose of 400 mg/day was associated with a skin rash in 24% of the patients receiving this therapy. TMP suppressed fecal Escherichia coli. SZ increased the number of sulfa-resistant fecal isolates; however, this phenomenon did not affect the rate of sulfa-resistant recurrences.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Brumfitt W., Pursell R. Double-blind trial to compare ampicillin, cephalexin, co-trimoxazole, and trimethoprim in treatment of urinary infection. Br Med J. 1972 Jun 17;2(5815):673–676. doi: 10.1136/bmj.2.5815.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burchall J. J., Hitchings G. H. Inhibitor binding analysis of dihydrofolate reductases from various species. Mol Pharmacol. 1965 Sep;1(2):126–136. [PubMed] [Google Scholar]
- Bushby S. R., Hitchings G. H. Trimethoprim, a sulphonamide potentiator. Br J Pharmacol Chemother. 1968 May;33(1):72–90. doi: 10.1111/j.1476-5381.1968.tb00475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CUTLER S. J., EDERER F. Maximum utilization of the life table method in analyzing survival. J Chronic Dis. 1958 Dec;8(6):699–712. doi: 10.1016/0021-9681(58)90126-7. [DOI] [PubMed] [Google Scholar]
- Cosgrove M. D., Morrow J. W. Ampicillin versus trimethoprim sulfamethoxazole in chronic urinary tract infection. J Urol. 1974 May;111(5):670–672. doi: 10.1016/s0022-5347(17)60042-9. [DOI] [PubMed] [Google Scholar]
- Cox C. E. The urethra and its relationship to urinary tract infection: the flora of the normal female urethra. South Med J. 1966 May;59(5):621–626. doi: 10.1097/00007611-196605000-00027. [DOI] [PubMed] [Google Scholar]
- Darrell J. H., Garrod L. P., Waterworth P. M. Trimethoprim: laboratory and clinical studies. J Clin Pathol. 1968 Mar;21(2):202–209. doi: 10.1136/jcp.21.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsum U., Hjelm E., Jonsell G. Antibody-coated bacteria in the urine of children with urinary tract infections. Acta Paediatr Scand. 1976 Sep;65(5):639–642. doi: 10.1111/j.1651-2227.1976.tb04944.x. [DOI] [PubMed] [Google Scholar]
- Gillespie W. A., Sellin M. A., Gill P., Stephens M., Tuckwell L. A., Hilton A. L. Urinary tract infection in young women, with special reference to Staphylococcus saprophyticus. J Clin Pathol. 1978 Apr;31(4):348–350. doi: 10.1136/jcp.31.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding G. K., Marrie T. J., Ronald A. R., Hoban S., Muir P. Urinary tract infection localization in women. JAMA. 1978 Sep 8;240(11):1147–1151. [PubMed] [Google Scholar]
- Hoigné R., Bartholomé-Pató J., Müller U. Die Beurteilung des Behandlungserfolgs bei Harnweginfektionen auf Grund quantitativer Bestimmung von Bakterurie und Leukocyturie. Schweiz Med Wochenschr. 1968 Dec 7;98(49):1939–1944. [PubMed] [Google Scholar]
- Hoigné R., Müller U., Schneider H. R. Bactrim Roche, ein Kombinationspräparat von Sulfamethoxazol und Trimethoprim. Schweiz Med Wochenschr. 1969 Oct 18;99(42):1511–1518. [PubMed] [Google Scholar]
- Jones S. R. Letter: Prostatitis as cause of antibody-coated bacteria in urine. N Engl J Med. 1974 Aug 15;291(7):365–365. doi: 10.1056/NEJM197408152910714. [DOI] [PubMed] [Google Scholar]
- Jones S. R., Smith J. W., Sanford J. P. Localization of urinary-tract infections by detection of antibody-coated bacteria in urine sediment. N Engl J Med. 1974 Mar 14;290(11):591–593. doi: 10.1056/NEJM197403142901103. [DOI] [PubMed] [Google Scholar]
- Jordan P. A., Iravani A., Richard G. A., Baer H. Urinary tract infection caused by Staphylococcus saprophyticus. J Infect Dis. 1980 Oct;142(4):510–515. doi: 10.1093/infdis/142.4.510. [DOI] [PubMed] [Google Scholar]
- Kasanen A., Anttila M., Elfving R., Kahela P., Saarimaa H., Sundquist H., Tikkanen R., Toivanen P. Trimethoprim. Pharmacology, antimicrobial activity and clinical use in urinary tract infections. Ann Clin Res. 1978;10 (Suppl 22):1–39. [PubMed] [Google Scholar]
- Knothe H. The effect of a combined preparation of trimethoprim and sulphamethoxazole following short-term and long-term administration on the flora of the human gut. Chemotherapy. 1973;18(5):285–296. doi: 10.1159/000221273. [DOI] [PubMed] [Google Scholar]
- Koch U. J., Schumann K. P., Küchler R., Kewitz H. Efficacy of trimethoprim, sulfamethoxazole and the combination of both in acute urinary tract infection. Clinical and pharmacokinetical studies. Chemotherapy. 1973;19(5):314–321. doi: 10.1159/000221470. [DOI] [PubMed] [Google Scholar]
- Kunin C. M., Craig W. A., Uehling D. T. Trimethoprim therapy for urinary tract infection. Long-term prophylaxis in a uremic patient. JAMA. 1978 Jun 16;239(24):2588–2590. doi: 10.1001/jama.239.24.2588. [DOI] [PubMed] [Google Scholar]
- Mundt K. A., Polk B. F. Identification of site of urinary-tract infections by antibody-coated bacteria assay. Lancet. 1979 Dec 1;2(8153):1172–1175. doi: 10.1016/s0140-6736(79)92396-1. [DOI] [PubMed] [Google Scholar]
- Näff H. Uber die Veränderungen der normalen Darmflora des Menschen durch Bactrim. Pathol Microbiol (Basel) 1971;37(1):1–22. [PubMed] [Google Scholar]
- Rumans L. W., Vosti K. L. The relationship of antibody-coated bacteria to clinical syndromes as found in unselected populations with bacteriuria. Arch Intern Med. 1978 Jul;138(7):1077–1081. [PubMed] [Google Scholar]
- Smith J. W., Jones S. R., Kaijser B. Significance of antibody-coated bacteria in urinary sediment in experimental pyelonephritis. J Infect Dis. 1977 Apr;135(4):577–581. doi: 10.1093/infdis/135.4.577. [DOI] [PubMed] [Google Scholar]
- TURCK M., PETERSDORF R. G. The epidemiology of nonenteric Escherichia coli infections: prevalence of serological groups. J Clin Invest. 1962 Sep;41:1760–1765. doi: 10.1172/JCI104635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winberg J., Bergström T., Lincoln K., Lidin-Janson G. Treatment trials in urinary tract infection (UTI) with special reference to the effect of antimicrobials on the fecal and periurethral flora. Clin Nephrol. 1973 May-Jun;1(3):142–148. [PubMed] [Google Scholar]



