Abstract
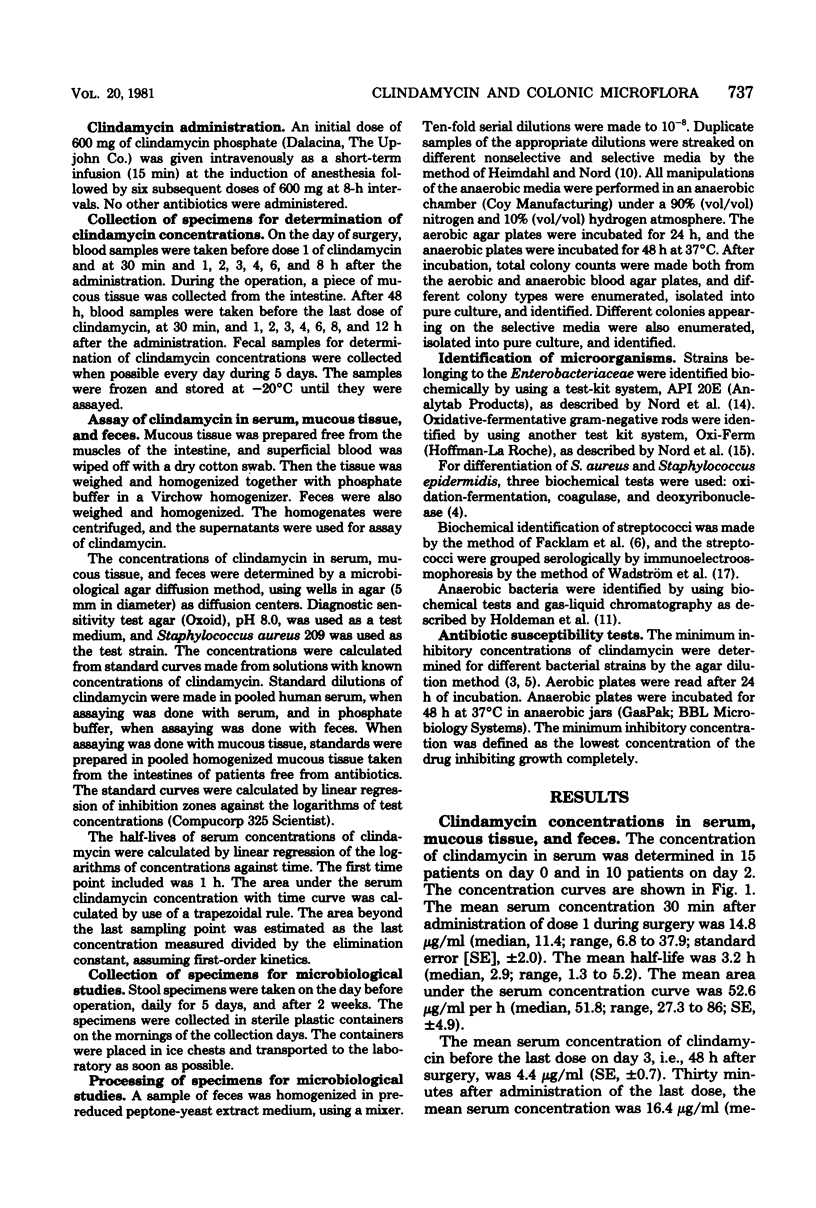
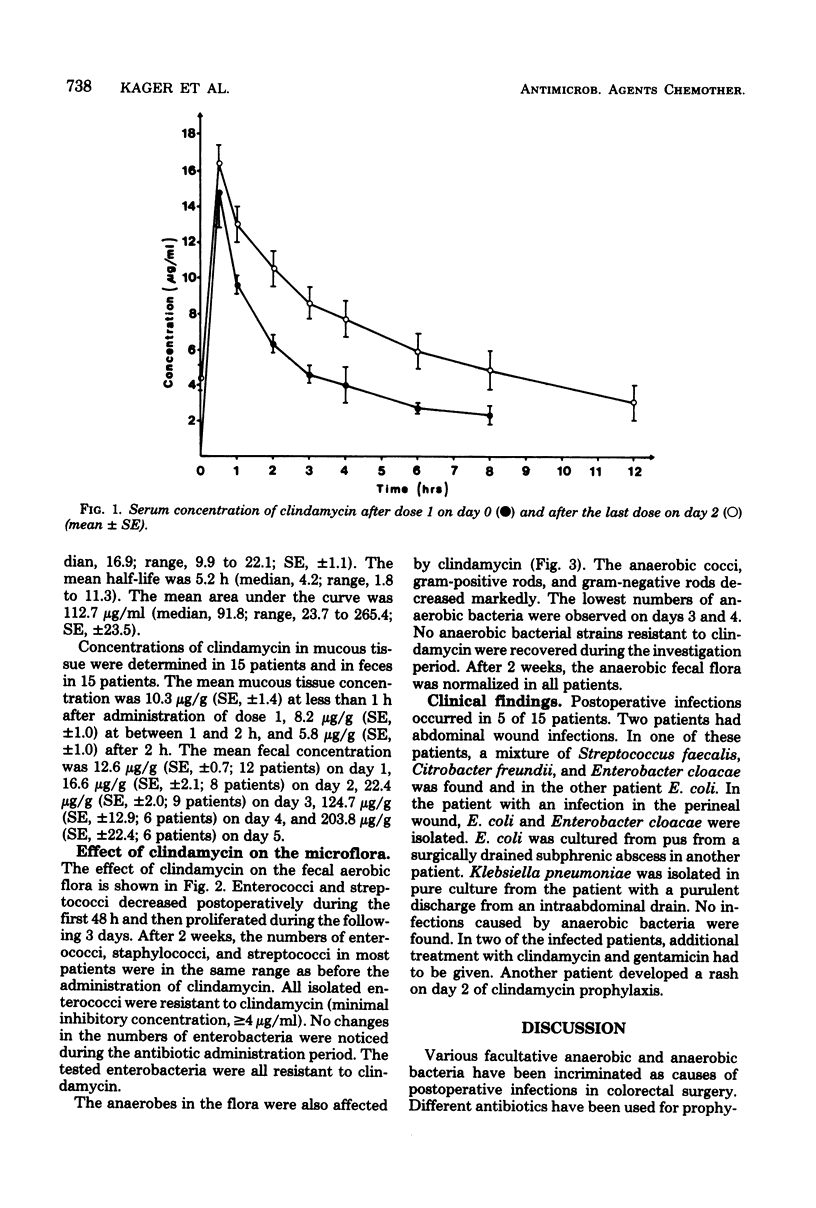
Clindamycin was given intravenously to 15 patients undergoing colorectal surgery in an initial dose of 600 mg, given at induction of anesthesia followed by 6 doses of 600 mg at 8-h intervals. Series of serum samples and fecal specimens were taken for analysis of clindamycin concentrations. Tissue samples from the gut wall were taken at surgery. The highest serum concentrations observed occurred 30 min after administration of clindamycin and varied between 6.8 and 37.9 microgram/ml (mean, 14.8 +/- 2.0 [standard error] microgram/ml). The clindamycin concentrations in the tissue samples were between 1.8 and 13.0 microgram/g. Clindamycin concentration in the fecal samples varied between 2.1 and 460 microgram/g. Fecal samples were also collected during the investigation period for cultivation of aerobic and anaerobic bacteria. Among the aerobic bacteria, enterococci and streptococci decreased during the prophylaxis period. Anaerobic bacteria also decreased significantly during the same period. After the clindamycin administration period, enterococci, streptococci and anaerobic bacteria proliferated. No anaerobic strains resistant to clindamycin were isolated. Postoperative infections due to Streptococcus faecalis and different enterobacteria such as Escherichia coli, Enterobacter cloacae, Citrobacter freundii, and Klebsiella occurred in five patients.
Full text
PDF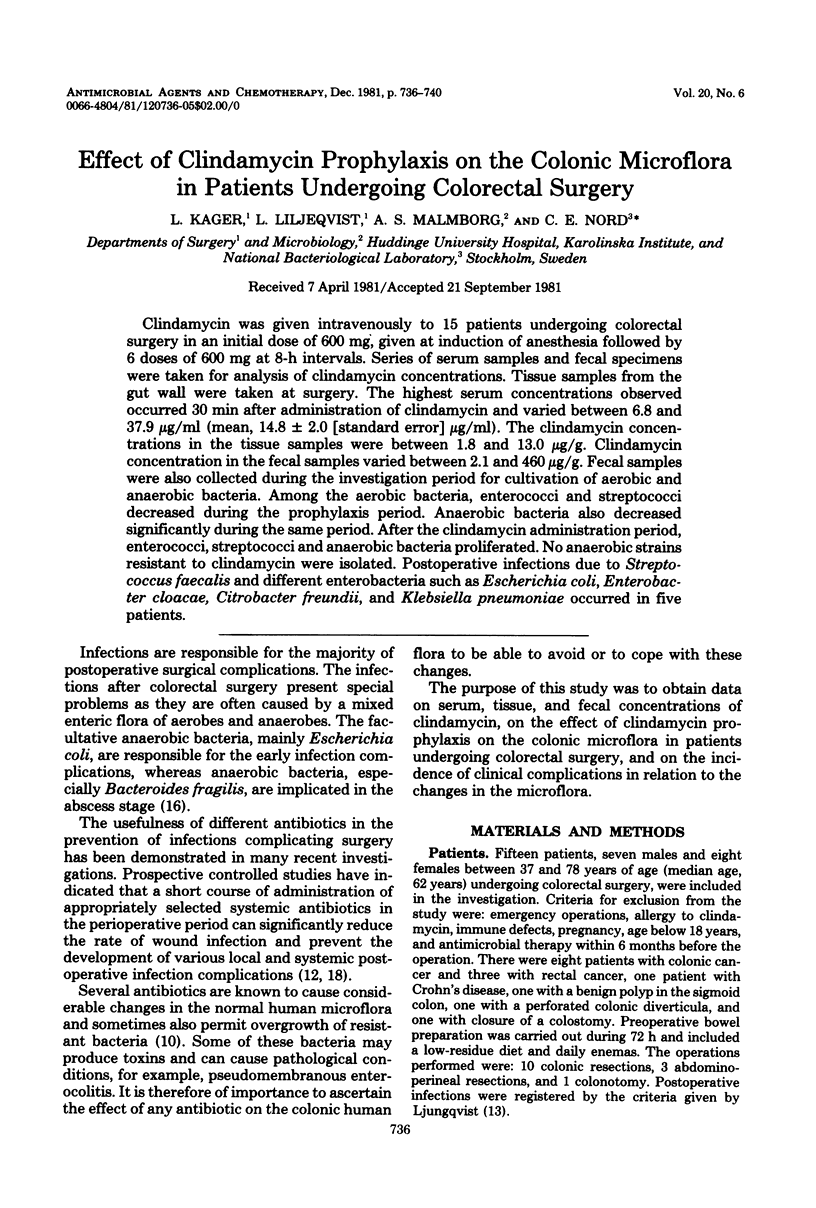
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bartlett J. G., Condon R. E., Gorbach S. L., Clarke J. S., Nichols R. L., Ochi S. Veterans Administration Cooperative Study on Bowel Preparation for Elective Colorectal Operations: impact of oral antibiotic regimen on colonic flora, wound irrigation cultures and bacteriology of septic complications. Ann Surg. 1978 Aug;188(2):249–254. doi: 10.1097/00000658-197808000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeHaan R. M., Metzler C. M., Schellenberg D., Vandenbosch W. D. Pharmacokinetic studies of clindamycin phosphate. J Clin Pharmacol. 1973 May-Jun;13(5):190–209. doi: 10.1002/j.1552-4604.1973.tb00208.x. [DOI] [PubMed] [Google Scholar]
- Dornbusch K., Nord C. E., Olsson B., Wadström T. Some properties of coagulase-negative deoxyribonuclease-producing strains of staphylococci from human infections. Med Microbiol Immunol. 1976 Jun 1;162(2):143–152. doi: 10.1007/BF02121324. [DOI] [PubMed] [Google Scholar]
- Dornbusch K., Nord C. E., Wadström T. Biochemical characterization and in vitro determination of antibiotic susceptibility of clinical isolates of Bacteroides fragilis. Scand J Infect Dis. 1974;6(3):253–258. doi: 10.3109/inf.1974.6.issue-3.08. [DOI] [PubMed] [Google Scholar]
- Ericsson H. M., Sherris J. C. Antibiotic sensitivity testing. Report of an international collaborative study. Acta Pathol Microbiol Scand B Microbiol Immunol. 1971;217(Suppl):1+–1+. [PubMed] [Google Scholar]
- Facklam R. R., Padula J. F., Thacker L. G., Wortham E. C., Sconyers B. J. Presumptive identification of group A, B, and D streptococci. Appl Microbiol. 1974 Jan;27(1):107–113. doi: 10.1128/am.27.1.107-113.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fass R. J., Saslaw S. Clindamycin: clinical and laboratory evaluation of parenteral therapy. Am J Med Sci. 1972 May;263(5):368–382. [PubMed] [Google Scholar]
- Fass R. J., Scholand J. F., Hodges G. R., Saslaw S. Clindamycin in the treatment of serious anaerobic infections. Ann Intern Med. 1973 Jun;78(6):853–859. doi: 10.7326/0003-4819-78-6-853. [DOI] [PubMed] [Google Scholar]
- Hanel K. C., King D. W., McAllister E. T., Reiss-Levy E. Single-dose parenteral antibiotics as prophylaxis against wound infections in colonic operations. Dis Colon Rectum. 1980 Mar;23(2):98–101. doi: 10.1007/BF02587603. [DOI] [PubMed] [Google Scholar]
- Heimdahl A., Nord C. E. Effect of phenoxymethylpenicillin and clindamycin on the oral, throat and faecal microflora of man. Scand J Infect Dis. 1979;11(3):233–242. doi: 10.3109/inf.1979.11.issue-3.11. [DOI] [PubMed] [Google Scholar]
- Kager L., Ljungdahl I., Malmborg A. S., Nord C. E., Pieper R., Dahlgren P. Antibiotic prophylaxis with cefoxitin in colorectal surgery: effect on the colon microflora and septic complications--a clinical model for prediction of the benefit and risks in using a new antibiotic in prophylaxis. Ann Surg. 1981 Mar;193(3):277–282. doi: 10.1097/00000658-198103000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LJUNGQVIST U. WOUND SEPSIS AFTER CLEAN OPERATIONS. Lancet. 1964 May 16;1(7342):1095–1097. doi: 10.1016/s0140-6736(64)91291-7. [DOI] [PubMed] [Google Scholar]
- Nord C. E., Lindberg A. A., Dahlbäck A. Evaluation of five test-kits-API, AuxoTab, Enterotube, PathoTec and R-B-for identification of Enterobacteriaceae. Med Microbiol Immunol. 1974 Mar 22;159(3):211–220. doi: 10.1007/BF02121337. [DOI] [PubMed] [Google Scholar]
- Nord C. E., Wretlind B., Dahlbäck A. Evaluation of two test-kits--API and Oxi Ferm tube--for identification of oxidative-fermentative Gram-negative rods. Med Microbiol Immunol. 1977 Jul 18;163(2):93–97. doi: 10.1007/BF02121824. [DOI] [PubMed] [Google Scholar]
- Onderdonk A. B., Bartlett J. G., Louie T., Sullivan-Seigler N., Gorbach S. L. Microbial synergy in experimental intra-abdominal abscess. Infect Immun. 1976 Jan;13(1):22–26. doi: 10.1128/iai.13.1.22-26.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadström T., Nord C. E., Lindberg A. A., Möllby R. Rapid grouping of streptococci by immunoelectroosmophoresis. Med Microbiol Immunol. 1974 Mar 22;159(3):191–200. doi: 10.1007/BF02121335. [DOI] [PubMed] [Google Scholar]
- Washington J. A., 2nd, Dearing W. H., Judd E. S., Elveback L. R. Effect of preoperative antibiotic regimen on development of infection after intestinal surgery: Prospective, randomized, double-blind study. Ann Surg. 1974 Oct;180(4):567–572. doi: 10.1097/00000658-197410000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]



