Most patients who present with neck pain have “non-specific (simple) neck pain,” where symptoms have a postural or mechanical basis. Aetiological factors are poorly understoodw1 and are usually multifactorial, including poor posture, anxiety, depression, neck strain, and sporting or occupational activities.w2 Neck pain after whiplash injury also fits into this category, provided no bony injury or neurological deficit is present.w3 When mechanical factors are prominent, the condition is often referred to as “cervical spondylosis,” although the term is often applied to all non-specific neck pain. Mechanical and degenerative factors are more likely to be present in chronic neck pain.
In cervical spondylosis, degenerative changes start in the intervertebral discs with osteophyte formation and involvement of adjacent soft tissue structures. Many people over 30 show similar abnormalities on plain radiographs of the cervical spine, however, so the boundary between normal ageing and disease is difficult to define.w4 Even severe degenerative changes are often asymptomatic, but can lead to neck pain, stiffness, or neurological complications.
I will concentrate on the diagnosis of cervical spondylosis and the evidence available for the different treatments. I will also mention some practical measures that are thought to be important but have not yet been studied. Specific conditions like fibromyalgia, disc prolapse, and whiplash will not be considered, although some patients with these conditions may have been included in therapeutic studies.
Summary points
The diagnosis of cervical spondylosis is usually based on clinical symptoms
Patients need detailed neurological assessment of upper and lower limbs as cervical degeneration is often asymptomatic, but can lead to pain, myelopathy, or radiculopathy
“Red flag” symptoms identify the small number of patients who need magnetic resonance imaging, blood tests, and other investigations
The best treatments are exercise, manipulation, and mobilisation, or combinations thereof
Radiculopathy has a good prognosis and may respond to conservative measures
Results of neck surgery for myelopathy or intractable pain are often disappointing
Data sources and selection criteria
I searched Chirolars (now called Mantis), Bioethicsline, Cinahl, Current Contents, and Medline for therapeutic options to treat mechanical neck pain when preparing and updating an article for Clinical Evidence.1 This review is based on that article.
Who gets neck pain?
About two thirds of the population have neck pain at some time in their lives,w5w6 and prevalence is highest in middle age. In a general practice survey of adults in the United Kingdom, 25% of women and 20% of men reported current neck pain.w7 In a Norwegian survey of 10 000 adults, 34% of responders had experienced neck pain in the previous year.w8 After back pain, neck pain is the most frequent musculoskeletal cause of consultation in primary care worldwide. In the UK about 15% of hospital based physiotherapy and in Canada 30% of chiropractic referrals are for neck pain.w9w10 Epidemiological studies of neck pain are mostly based on questionnaire or population surveys and may overestimate the frequency of the condition. Despite these methodological difficulties, they do provide evidence that neck pain places a heavy burden on individuals, employers, and healthcare services.
What is the natural history of neck pain?
The outcome of neck pain depends on the underlying cause, but acute neck pain usually resolves within days or weeks, although it can recur or become chronic (more than three months' duration). A UK survey of 7669 adults found that 18% had neck pain at the time of the survey, and half of those (58% of the symptomatic patients responded) still had pain when asked one year later.w11 Outcome is unpredictable once pain becomes chronic, and prognosis and the factors that influence it vary greatly.w1 Reports on the importance of factors like age, sex, occupation, psychological factors, and radiological findings are conflicting,w1w2 but the quality of most studies is poor. Three recent studies (1535 patients)w11–w13 found that the best predictors of an unfavourable outcome one year after presentation with neck pain were severity of the initial pain and concomitant back pain. At least 10% of affected people develop chronic neck pain,w5 although this figure is much higher in some studies.w11w13 In some industries, neck related disorders account for as much time off work as low back pain.w14 Neck pain causes severe disability in 5% of affected people.w6
How is cervical spondylosis diagnosed?
Cervical spondylosis is usually diagnosed on clinical grounds alone (box 1). Although pain is predominantly in the cervical region, it can be referred to a wide area, and is characteristically exacerbated by neck movement. Neurological change should always be sought in the upper and lower limbs, but objective changes occur only when spondylosis is complicated by myelopathy or radiculopathy, or when unrelated causes like disc prolapse, thoracic outlet obstruction, brachial plexus disease, malignancy, or primary neurological disease are present.
Box 1 Presenting features of cervical spondylosis
Symptoms
Cervical pain aggravated by movement
Referred pain (occiput, between the shoulder blades, upper limbs)
Retro-orbital or temporal pain (from C1 to C2)
Cervical stiffness—reversible or irreversible
Vague numbness, tingling, or weakness in upper limbs
Dizziness or vertigo
Poor balance
Rarely, syncope, triggers migraine, “pseudo-angina”w15
Signs
Poorly localised tenderness
Limited range of movement (forward flexion, backward extension, lateral flexion, and rotation to both sides)
Minor neurological changes like inverted supinator jerks (unless complicated by myelopathy or radiculopathy)
Box 2 Differential diagnosis of cervical spondylosis
Other non-specific neck pain lesions—acute neck strain, postural neck ache, or whiplash
Fibromyalgia and psychogenic neck pain
Mechanical lesions—disc prolapse or diffuse idiopathic skeletal hyperostosis
Inflammatory disease—rheumatoid arthritis, ankylosing spondylitis, or polymyalgia rheumatica
Metabolic diseases—Paget's disease, osteoporosis, gout, or pseudo-gout
Infections—osteomyelitis or tuberculosis
Malignancy—primary tumours, secondary deposits, or myeloma
What conditions need to be differentiated from cervical spondylosis?
Box 2 shows the most important differential diagnoses. Other non-specific neck pain syndromes are not easy to distinguish from cervical spondylosis, but conditions like whiplash have different dynamics, which may greatly influence outcome. Fibromyalgia and related conditions cause more diverse symptoms, with prominent tender “trigger” points around the joints, sleep disturbance, and psychological abnormalities. The other differential diagnoses are usually suggested by “Red flag” symptoms (box 3), which indicate the need for further investigation. Inflammatory changes associated with rheumatoid arthritis affect the atlanto-axial joint and upper cervical spine, where degenerative change is unusual, and in patients with arthritis it may be necessary to determine whether neck pain is due to arthritis or concomitant cervical spondylosis. Disc prolapse, other mechanical lesions, or primary neurological disease are likely to cause objective neurological abnormalities and trigger further investigation.
Box 3 “Red flag” features and the conditions they may suggest
Malignancy, infection, or inflammation
Fever, night sweats
Unexpected weight loss
History of inflammatory arthritis, malignancy, infection, tuberculosis, HIV infection, drug dependency, or immunosuppression
Excruciating pain
Intractable night pain
Cervical lymphadenopathy
Exquisite tenderness over a vertebral body
Myelopathy
Gait disturbance or clumsy hands, or both
Objective neurological deficit—upper motor neurone signs in the legs and lower motor neurone signs in the arms
Sudden onset in a young patient suggests disc prolapse
Other
History of severe osteoporosis
History of neck surgery
Drop attacks, especially when moving the neck, suggest vascular disease
Intractable or increasing pain
How do I investigate patients with suspected cervical spondylosis?
Most patients do not need further investigation, and the diagnosis is made on clinical grounds alone. Plain radiographs of the cervical spine may show a loss of normal cervical lordosis, suggesting muscle spasm, but most other features of degenerative disease (fig 1) are found in asymptomatic peoplew4 and correlate poorly with clinical symptoms. Magnetic resonance imaging of the cervical spine is the investigation of choice if more serious pathology is suspected, as it gives detailed information about the spinal cord, bones, discs, and soft tissue structures (fig 2). However, normal people can show important pathological abnormalities on imaging,w16 so scans need to be interpreted with care. Patients who are systemically ill or have symptoms suggesting more serious pathology (box 3) may need additional investigations such as full blood count, erythrocyte sedimentation rate, C reactive protein, protein electrophoresis, and occasionally electrodiagnostic studies to exclude other pathologies. In patients with rheumatoid arthritis, flexion and extension radiographs of the neck will show whether severe atlanto-axial subluxation is present, but magnetic resonance imaging may be needed to define the severity of inflammatory and degenerative changes.
Fig 1 Oblique radiograph of the cervical spine in a patient with cervical spondylosis showing loss of disc height, anterior osteophytosis, and narrowing of the foramina
Fig 2 Magnetic resonance imaging scan of the cervical spine showing the loss of disc height and signal from several discs with multisegmental spondylotic bars. Protrusion of the C5/6 disc results in compression of the cervical cord, which shows associated myelopathic changes
What are the complications?
Cervical spondylosis can be complicated by myelopathy or radiculopathy, although cervical disc prolapse, plexopathy, motor neurone disease, or other diseases can cause similar symptoms2; magnetic resonance imaging, electrodiagnostic tests, and other investigations may be needed to exclude other diagnoses. Neurological complications can occur in established cervical spondylosis or can be the presenting feature of the disease.
Myelopathy causes clumsiness of the hands or gait disturbance, or both, as a result of sensory ataxia or spastic paraparesis of the lower limbs, with bladder dysfunction being a late symptom. Examination of the upper limbs may show an increase in tone, with a pronator “catch” (C6/C7) or increased tone in finger flexors (C8). Wasting and fasciculation of biceps (C5/C6) or triceps (C7) are occasional findings. The lower limbs usually show an increase in tone with spasticity, but little true weakness. Tendon reflexes are characteristic, with reduced or even inverted biceps or supinator jerks (finger flexion instead of the normal biceps or supinator jerk), and an increase in triceps jerks, finger jerks, and all lower limb reflexes, with upgoing plantar responses. A positive Hoffman's sign (flexion of the terminal phalanx of the thumb and second and third phalanges of the other fingers when one of the middle fingertips is flicked) and ankle clonus are also common findings. Sensory changes vary, but tend to affect vibration and joint position sense in the hands more than the feet.
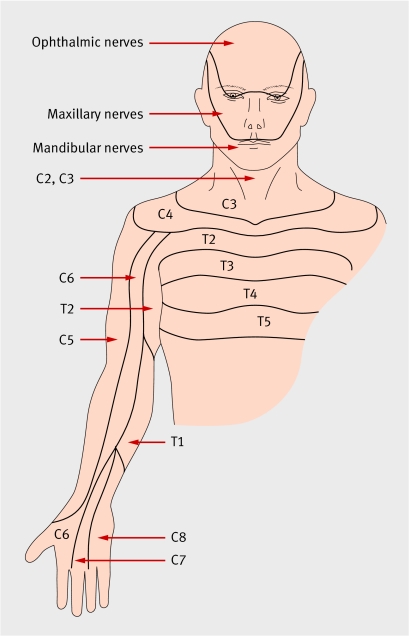
Radiculopathy (nerve root compression) due to cervical spondylosis usually occurs at the C5 to C7 levels, although higher levels can also be affected. Neurological features follow a segmental distribution in the upper limb, with sensory symptoms (shooting pains, numbness, hyperaesthesia) being more common than weakness. Reflexes are usually diminished at the appropriate level (biceps (C5/6), supinator (C5/6), or triceps (C7)). Figure 3 shows the dermatomal distribution of the cervical and upper thoracic nerves.
Fig 3 Dermatomal distribution of cervical and upper thoracic nerves
How do I treat cervical spondylosis?
Most mechanical neck pain will respond to conservative measures, but the optimal treatment for uncomplicated neck pain has yet to be established. Few treatments have been assessed in high quality randomised studies, but I will present the best available evidence for the most commonly used ones.
Pragmatic (unstudied) measures
Currently, a balanced view of the management of neck pain cannot be given by discussing evidence based treatments only. Stress management and postural advice on daily activities, work, and hobbies may be useful in some patients. Patients should be advised to use only one pillow at night. When pain is severe, analgesics and anti-inflammatory agents are widely used, despite the lack of evidence that they work. Low dose tricyclic antidepressants, like amitriptyline 10-30 mg per night, might be more effective. Yoga, pilates, and the Alexander technique all improve neck posture, but their value in treating neck pain is uncertain.
How do I treat acute neck pain to prevent chronic disability?
Most studies of early treatment of acute neck pain are on patients with whiplash injury, and it is unclear whether the data can be generalised to non-traumatic causes. Two systematic reviews of small poor quality studies considered acute neck pain not due to whiplash and found limited evidence of benefit for manipulation or mobilisation therapy.3,4 No evidence exists for the efficacy of non-steroidal anti-inflammatory agents or analgesics. The evidence that muscle relaxants relieve pain more than placebo is weak, and the incidence of side effects like drowsiness is high. Studies of the early treatment of whiplash provide moderate evidence that early mobilisation physiotherapyw17-w20 and advice to “act as usual”w21 are more effective than immobilisation and less active treatments in speeding up recovery and reducing chronic disability. Less evidence exists for the benefit of home exercise regimens,w22 pulsed electromagnetic field therapy,w23 and multimodal therapy.w24
How do I treat chronic cervical spondylosis?
Randomised controlled trials identified by systematic reviews1,5,6,7,8 provide moderate evidence that various exercise regimens—using proprioceptive, strengthening, endurance, or coordination exercises—are more effective than usual care (analgesics, non-steroidal anti-inflammatory drugs, or muscle relaxants)9w25 or stress management,10,11 although not all studies have found exercise beneficial.12 One randomised controlled trial found exercise plus infrared heat no more effective than transcutaneous electrical nerve stimulation plus heat at relieving pain at six weeks and six months, although both were better than heat alone.w26
Randomised controlled trials included in systematic reviews of manual treatments (mobilisation physiotherapy or manipulation)1,4,5,13,14,15,16 provide limited evidence that mobilisation physiotherapy17,18 and manipulation17 are more effective for chronic neck pain than less active treatments (drug treatment, education, counselling). However, manipulation has occasionally been associated with serious neurological complications (around 5-10 per 10 million manipulations).w27
Mobilisation, manipulation, and exercise seem to be equally effective.19,20w28 A study comparing combined exercise and manipulation with either modality alone found the combination to be more effective at three months,21 but no difference was seen compared with exercise alone at one and two years.22 However, another pragmatic study found no advantage at six weeks or six months of adding manual therapy (63% of patients had mobilisation physiotherapy) or heat (shortwave diathermy) to exercise and advice.23
Systematic reviews of weak randomised controlled trials provided no conclusive evidence about the effectiveness of acupuncture24 or traction25 compared with a range of other treatments in patients with chronic neck pain. The addition of psychotherapy techniques like cognitive behavioural therapy also added little to physical or mechanical treatment alone.26
How do I treat cervical spondylosis complicated by neurological abnormality?
Most patients with neurological abnormality will need magnetic resonance imaging of the cervical spine at an early stage, particularly if they have progressive myelopathy, radiculopathy, or intractable pain. Neurosurgical intervention also needs to be considered, but the outcome of decompressive surgery is often disappointing, especially for myelopathy complicating cervical spondylosis. While progression of the neurological deficit may be slowed by surgery, lost function may not recover or symptoms may progress at a later date. Poor outcome after surgery may reflect irreversible damage to the cervical cord (see fig 2) or compromise to the vascular supply to the cord.
Radiculopathy usually has a favourable outcome, so conservative treatments are gaining popularity, especially for patients with comorbidities or those who are unsuitable for general anaesthesia but are neurologically stable. Only a few small poor quality randomised controlled trials have assessed cervical epidural injection27 and other conservative measures28 to treat this condition. Two small studies that compared epidural injection with placebo found epidural injections slightly more effective,w29w30 but the difference was not significant. Epidural injection in the cervical region is more invasive than in the lumbar region, and it should be considered in patients with severe intractable pain or radiculopathy only if surgical intervention is not an option.27 One randomised controlled trial in patients with cervical radiculopathy compared surgical intervention with physiotherapy or immobilisation. While the surgical group had less pain at three to four months, no difference was seen between the three treatment groups at one year.29
What has changed and what needs to be done?
Recently, better quality randomised controlled trials have suggested that exercise, mobilisation physiotherapy, and manipulation are more effective than less active treatments, although their relative cost effectiveness has not been studied.10,19,21 One high quality study21,22 suggested further advantages to combining exercise with mobilisation or manipulation; this approach has been advocated by a Cochrane review group8,15 and warrants further study.
Many commonly used treatments including analgesics, anti-inflammatory agents, tricyclic antidepressants, strategies to improve posture, and stress management are widely used but have not been studied. Other modalities like acupuncture, traction, electrotherapy, and psychotherapy are of uncertain value and need further study.
The lack of consistency in study design, populations studied, outcome measures, and lengths of follow-up make comparisons across studies difficult. Use of multiple interventions in the same study also complicates these analyses. Large well designed randomised studies using standardised study protocols are needed to clarify the efficacy and cost effectiveness of individual treatments.
Supplementary Material
Competing interests: None declared.
References
- 1.Binder AI. Neck pain syndromes. Clinical Evidence. Search date December 2006. www.clinicalevidence.com/ceweb/conditions/msd/1103/1103_updates.jsp
- 2.Binder AI. Cervical pain syndromes. In: Isenberg DA, Maddison PJ, Woo P, Glass DN, Breedveld FC, eds. Oxford textbook of rheumatology. 3rd ed. Oxford: Oxford Medical Publications, 2004:1185-95.
- 3.Vernon HT, Humphreys BK, Hagino CA. A systematic review of conservative treatments for acute neck pain not due to whiplash. J Manipulative Physiol Ther 2005;28:443-8. [DOI] [PubMed] [Google Scholar]
- 4.Canadian Chiropractic Association, Canadian Federation of Chiropractic Regulatory Boards, Clinical Practice Guidelines Development Initiative, Guidelines Development Committee (GDC). Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc 2005;49:158-209. [PMC free article] [PubMed] [Google Scholar]
- 5.Aker PD, Gross AR, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ 1996;313:1291-6. [PMC free article] [PubMed] [Google Scholar]
- 6.Philadelphia Panel. Evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain. Phys Ther 2001;81:1701-17. [PubMed] [Google Scholar]
- 7.Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther 2003;8:10-20. [DOI] [PubMed] [Google Scholar]
- 8.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Brontfort G, et al, Cervical Overview Group. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2005;(3):CD004250. [DOI] [PubMed]
- 9.Ylinen J, Takala E, Nykanen M, Hakknen A, Malkia E, Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA 2003;289:2509-16. [DOI] [PubMed] [Google Scholar]
- 10.Waling K, Sundelin G, Ahlgren C, Jarvholm B. Perceived pain before and after three exercise programs—a controlled clinical trial of women with work-related trapezius myalgia. Pain 2000;85:201-7. [DOI] [PubMed] [Google Scholar]
- 11.Waling K, Jaörvholm B, Sundelin G. Effects of training on female trapezius myalgia: an intervention study with a 3-year follow-up period. Spine 2002;27:789-96. [DOI] [PubMed] [Google Scholar]
- 12.Viljanen M, Malmivaara A, Uitti J, Tinne M, Palmroos P, Laippala P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: randomised controlled trial. BMJ 2003;327:475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine 1996;21:1746-60. [DOI] [PubMed] [Google Scholar]
- 14.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J 2004;4:335-56. [DOI] [PubMed] [Google Scholar]
- 15.Gross AK, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, et al, Cervical Overview Group. Manipulation and mobilisation for mechanical neck disorders. Cochrane Database Syst Rev 2004;(1):CD004249. [DOI] [PubMed]
- 16.Oduneye F. Spinal manipulation for chronic neck pain. In: Bazian Ltd, ed. STEER: Succinct and Timely Evaluated Reviews 2004;4(4). Bazian Ltd and Wessex Institute for Health Research and Development, University of Southampton.
- 17.Koes BW, Bouter LM, van Mameren H, Essers AH, Vestegen GM, Hofhuizen DM, et al. Randomised clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow up. BMJ 1992;304:601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoving J, Koes B, de Vet H, van der Wildt DA, Assendelft WJ, van Mameren H, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med 2002;136:713-22. [DOI] [PubMed] [Google Scholar]
- 19.Jordan A, Bendix T, Nielsen H, Hansen ER, Host D, Winkel A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain. A prospective, single-blinded, randomized clinical trial. Spine 1998;23:311-9. [DOI] [PubMed] [Google Scholar]
- 20.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain study. Am J Public Health 2002;92:1634-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine 2001;26:788-97. [DOI] [PubMed] [Google Scholar]
- 22.Evans R, Bronfort G, Nelson B, Goldsmith CH. Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 2002;27:2383-9. [DOI] [PubMed] [Google Scholar]
- 23.Dziedzic K, Hill J, Lewis M, Sim J, Daniels J, Hay EM. Effectiveness of manual therapy or pulsed shortwave diathermy in addition to advice and exercise for neck disorders: a pragmatic randomized controlled trial in physical therapy clinics. Arthritis Care Res 2005;53:214-22. [DOI] [PubMed] [Google Scholar]
- 24.White AR, Ernst E. A systematic review of randomized controlled trials of acupuncture for neck pain. Rheumatology 1999;38:143-7. [DOI] [PubMed] [Google Scholar]
- 25.Van der Heijden GJ, Beurskens AJ, Koes BW, Assendelft WJ, de Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther 1995;75:93-104. [DOI] [PubMed] [Google Scholar]
- 26.Karjalainen K, Malmivaara A, Van Tulder M, Roine R, Jauhianen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev 2002;(3):CD002194. [DOI] [PubMed]
- 27.Boswell MV, Hansen HC, Trescot AM, Hirsch JA. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician 2003;6:319-34. [PubMed] [Google Scholar]
- 28.Fouyas IP, Statham PF, Sandercock PA. Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy. Spine 2002;27:736-47. [DOI] [PubMed] [Google Scholar]
- 29.Persson LC, Carlsson CA, Carlsson JY. Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar: a prospective randomised study. Spine 1997;22:751-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.