Abstract
The authors implemented an electronic medical record system in a rural Kenyan health center. Visit data are recorded on a paper encounter form, eliminating duplicate documentation in multiple clinic logbooks. Data are entered into an MS-Access database supported by redundant power systems. The system was initiated in February 2001, and 10,000 visit records were entered for 6,190 patients in six months. The authors present a summary of the clinics visited, diagnoses made, drugs prescribed, and tests performed. After system implementation, patient visits were 22% shorter. They spent 58% less time with providers (p < 0.001) and 38% less time waiting (p = 0.06). Clinic personnel spent 50% less time interacting with patients, two thirds less time interacting with each other, and more time in personal activities. This simple electronic medical record system has bridged the “digital divide.” Financial and technical sustainability by Kenyans will be key to its future use and development.
The Institute of Medicine has declared electronic medical records to be an essential technology for health care1 and a necessary tool for improving patient safety2 and the quality of care.3 To date, comprehensive computer-based patient records that serve these functions are uncommonly used in developed countries,4 and are rare to nonexistent in the developing world. This gulf has been termed the digital divide5 and even technological apartheid6 where the simplest technology is not available to promote health care delivery, patient outcomes, and public health.
We have reported previously the conceptualization and initial development of the Mosoriot Medical Record System (MMRS),7 an electronic medical record system supporting a primary care health center in rural Kenya. In this article, we report the implementation of the MMRS within the Mosoriot Rural Health Centre (MRHC) as the sole means for recording clinical data. We emphasize the technical aspects of data capture and storage, describe data from the first 10,000 visit records, and report the results of a formal evaluation of the impact of MMRS on patterns of health care delivery within the MRHC.
Methods
Implementation Site: The Mosoriot Rural Health Centre
This study was approved by Indiana University's Institutional Review Board and the Ethics Committee of the Moi University College of Health Sciences (MUCHS). There is a long-term collaboration between Indiana University and MUCHS.8,9 MUCHS uses a number of rural health centers in western Kenya as part of its medical education and public health research programs. The MRHC is one of these centers, located approximately 25 km (15 miles) southwest of Eldoret, Kenya's fifth largest city. This region is a highland plateau characterized by limited availability of essential resources such as potable water, sewerage, and paper. Electrical power and land-based telephone lines, when available at all, are unreliable. Cellular telephones are widely available and reliable, but they are relatively expensive and, thus, beyond the reach of most Kenyans. The economic infrastructure is mainly subsistence farming with significant poverty and unemployment.
The MRHC is maintained by the Kenyan Ministry of Health to provide primary and emergency care to a surrounding agrarian population of approximately 40,000 persons who mainly live in small villages. Although these villages have traditional (i.e., non-Western) healers and midwives, all state-sponsored health care is delivered in the MRHC. Except for severe emergencies such as major trauma, persons without financial resources who live in the MRHC's catchment area must be referred by the MRHC to receive care elsewhere in the Kenyan health care system. The MRHC contains a number of primary and urgent care clinics: antenatal, child welfare (under 5 years old), pediatric, adult medicine, family planning, and sexually transmitted infections. There also is a small inpatient unit (under 20 beds) in which patients requiring monitoring and more extended care can be hospitalized for brief intervals. Patients needing longer inpatient stays or more sophisticated care are referred to the Moi Teaching and Referral Hospital in Eldoret that is staffed by faculty from MUCHS.
Before the implementation of the MMRS, patients visiting the MRHC stopped at the check-in window where the visit was recorded, and the patient was given a sequential number for that visit that year. There was no permanent patient registry or unique identifier. Then, depending on each patient's age and clinical problem (or prior appointment), the patient was directed to the appropriate clinic. Care at the MRHC is provided by nurses and their assistants with oversight by a single, nonphysician clinical officer. Because the MRHC is a site for education of medical, nursing, and public health students from multiple Kenyan institutions, students often participate in providing care. When diagnostic tests are needed, the patient is directed to a small laboratory where blood smears, urinalyses, and a small number of serologic tests are performed. A basic x-ray unit can take simple chest and bone radiographs. There is a pharmacy that contains bulk quantities of a very small number of drugs, mostly antibiotics and analgesics.
Before installation of the MMRS, records for MRHC visits were kept in logbooks maintained in both the registration office and each clinic. Identical (and duplicative) information for each visit was entered by hand into the logbook of each clinic the patient visited and consisted of the visit number (numbers are recycled at the beginning of each year), the patient's name, the chief complaint, a final diagnosis, and treatment given or prescribed. A single file cabinet holds more than 30 years of medical records for the entire facility (Figure 1, located in an online data supplement at <www.jamia.org>). The nurses and clinical officers record additional clinical notes (diagnoses, test results, etc.) in small booklets that each individual patient is required to purchase each year for $0.25 (US). The patients take these booklets home along with any radiographs that are taken. The patients are expected to bring these booklets to each visit, the value of which is limited by their cost (which can be expensive to the typically large Kenyan families with little or no income) and patients' sometimes forgetting them.
Design of the Mosoriot Medical Record System
Conceptualization and Development
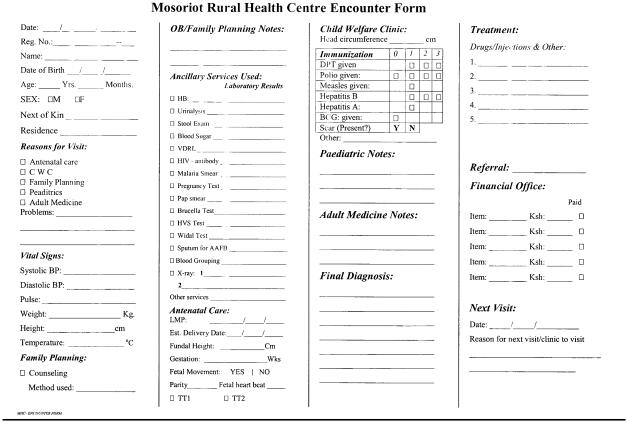
The initial conceptualization and development of the MMRS have been described in detail elsewhere.7 Briefly, it is a modular system comprised of a Registration Module, a paper encounter form, a Data Entry module, a Reporting Module, and a Data Dictionary. When a new patient presents to the check-in window, he or she is registered into the MMRS and given a plastic card on which his or her name and MMRS number are recorded (Figure 2, located in an online data supplement at <www.jamia.org>). Patients proudly carry their cards identifying them as “members” of the MRHC. At all subsequent visits, the patient is expected to present his or her identification (ID) card, and the MMRS number is handwritten on a blank encounter form (▶). If a previously registered patient does not have his or her card, the MMRS registration system provides a name lookup option.
Figure 3.
Paper encounter form on which health care providers enter patient data.
Each patient then is given an encounter form and directed to the appropriate clinic. Nurses in each clinic record clinical information on the encounter form rather than writing it in the clinic or laboratory logbooks or the patients' booklets. Laboratory technicians do the same for patients undergoing diagnostic tests. The encounter form is designed to require minimal writing using check boxes whenever possible. After visits to the clinic(s), laboratory, pharmacy, and financial office, each patient is supposed to return to the check-out window and present the encounter form to the check-out clerk. The clerk then enters encounter form data into the MMRS and returns the encounter form to the patient to take home in lieu of providers' writing in the patient's booklet.
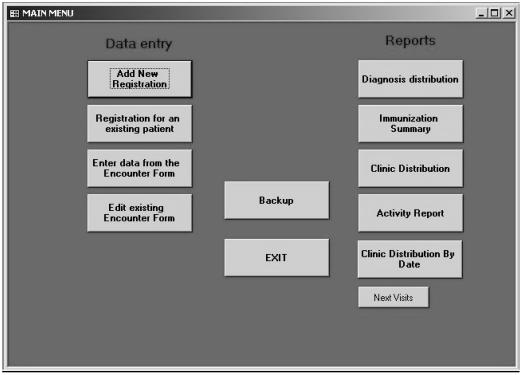
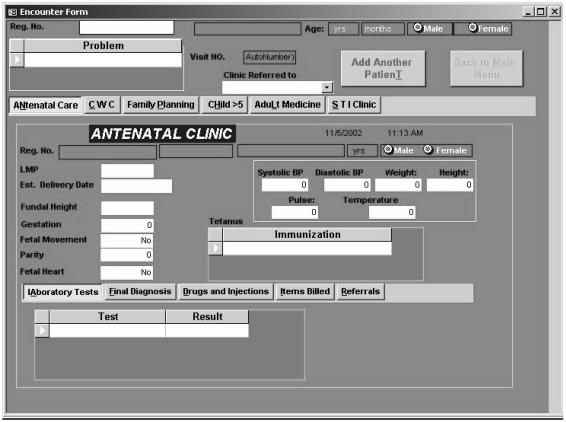
▶ shows the latest version of the MUCHS' main menu screen, and Figure 5 (located in an online data supplement at <www.jamia.org>) shows the registration screen. ▶ shows the encounter form data entry form, with the antenatal clinic screen displayed. The data model uses the patient and date as the unique identifiers of the visit, the basic unit of observation. All clinic, test, pharmacy, and charge data are linked to the visit.
Figure 4.
Main menu screen for the Mosoriot Medical Record System.
Figure 6.
Encounter form data entry screen, with the antenatal clinic tab selected.
Electrical Power
The MRHC gets power from the local electrical grid, which obtains 90% of its power from hydroelectric dams. During dry spells, the water level behind these dams drops drastically, which results in power rationing: certain regions of the country and services are deprived of electric power on a rotating basis so that the reserve can be used for important services such as hospitals and security facilities. The MRHC is in a rural area considered not large enough to warrant receiving continuous power supply. Therefore, to ensure sustainability and continued operation of the MMRS, we provided multiple backup systems:
An uninterruptible power source (UPS) battery
A solar-powered system
A gasoline-powered generator
A paper backup system (paper registration and encounter forms that can be back-entered into the system when power is restored)
With the use of a power inverter (converts DC to AC), the solar system is connected to the main power source via two large batteries so that the system can use either the electric grid or the solar system. The computer system including the identification label printer and the report printer use the above cascade of power sources. Whenever there is main grid failure, the UPS automatically takes over. If the local grid is not restored before the UPS fails (approximately 30 minutes), an alarm sounds, after which a clerk flips a switch, and the system begins drawing power from the solar batteries that last approximately four hours.
The choice of the backup solar power system was made because Kenya has sunlight for more than 90% of the day, which, at Mosoriot (located near the equator), is 12 hours long every day of the year. An exception is during the wet season, which is highly variable, when the amount of sunlight is significantly decreased. Fortunately, these are the seasons when the power rationing is usually not in effect because the water level has increased. The solar system is reasonably inexpensive (approximately $1,000 US). Because the MMRS was turned on in February of 2001, there has been no loss of data because of a lack of electricity. The gasoline-powered generator was never used, so it was removed.
Unique Patient Identifier
There is no Kenyan unique identifier equivalent to the American social security number. Therefore, we had to create an MMRS number for each patient using the smallest number of data fields that uniquely identify Kenyans. After consultation with MUCHS faculty and MRHC staff, we decided on the following fields:
First name (usually Western)
Middle name (usually Kenyan)
Last name (often shared by many persons in one's village)
Mother's first name
Father's first name (not really required technically but required socially to maintain the status of Kenyan men)
Village (whose names are not unique)
Location (equivalent to a US county)
Sublocation (equivalent to a US township)
Data Dictionary
The foundation of the MMRS is the data dictionary. As shown in Figure 7, which is located in an online data supplement at <www.jamia.org>, the dictionary contains a list of terms, reference terms (that allow for multiple synonyms for each term), the term type (diagnosis, test, drug, or treatment), the clinical system to which the term belongs (e.g., organ system, drug class), its ICD-10 code (for diagnoses only), a text description, and a charge for each test and drug. The dictionary has been updated continually as clinicians record new (less common) diagnoses, drugs, and treatments. The data dictionary also has been increased by adding terms the MRHC's managers have requested to generate reports to aid them in their management activities.
Data Security
Before the MMRS could completely replace the MRHC's paper-based record system, the clinicians and staff had to be convinced that the data were secure. Acquiring such trust was particularly difficult in Kenya, where the health care providers and clerks had little or no computer training. But for full implementation to occur, and to realize any time savings that the system might generate, the paper system had to be abandoned, and the MMRS had to become the sole source of medical records for MRHC. In addition to data security, confidentiality is important, but there were no rules governing the use of electronic data in a country with no prior experience with them. We therefore established redundant steps to assure data security and confidentiality:
All accesses to the MMRS are password protected.
Access to data for various users is limited to only those aspects of the MMRS for which they are responsible.
Twice a day, the MMRS automatically backs up its entire database to a Zip disk.
At the end of the day when the MMRS computer is shut down, the entire database is again backed up onto a Zip disk. The backup Zip disk is taken home every night by the MRHC Matron (i.e., Head Nurse).
Once a week, the MMRS' system administrator (JKR) receives a copy of the entire database on a Zip disk and places it on his own computer at MUCHS.
Generating Reports
▶ shows the various standard reports that are built into the MMRS. Most of them are required by the Ministry of Health (e.g., immunizations, distribution of visits by clinic, and an activity report). Additional custom reports can be created at the request of MRHC's Director and Matron to aid in their appealing for funds and managing MRHC. For example, before implementing the MMRS, the MRHC could not document the amount of free care (as required by the Ministry of Health) that is provided to pregnant women, children under 5 years old, and adults with sexually transmitted diseases. The MRHC pharmacist is also using MMRS reports to manage drug inventories.
MMRS Implementation, Evolution, and Problem Solving
Redesigning Data Entry
On February 3, 2002, we installed a fully operational MMRS at MRHC. During the previous eight months, all MRHC clinicians and staff had undergone computer training to familiarize them with keyboarding and to reduce their fears and distrust of computers. On the day that the system was turned on, the local power grid was unavailable because a tree had fallen on the power line during the previous night's thunderstorm. The backup UPS and solar systems performed flawlessly. For the ensuing 20 months, the MMRS has been down for only three days: for a disk crash, failure of a video card, and theft of the solar panel. No data were lost on those days because the paper registration and encounter forms were kept, and data were entered later.
For simplicity and to design a medical record system for the developing world that is relatively inexpensive and most likely to be sustainable, we originally designed the MMRS to exist on a single microcomputer run by the same clerk who had been responsible for check-in and check-out under the paper-based system. However, as patients checked in and were registered into the MMRS, the clerk at the check-in window found that she could not register and check in patients while also entering data from the encounter forms as patients checked out. A single window and clerk could not be used for both check-in and check-out. Therefore, because checking patients in and out and registering them took precedence, encounter forms were not being entered into the system. As time went on, this did not improve, and the stack of used encounter forms grew.
Therefore, we redesigned the system by (1) connecting a second computer to the original MMRS computer using a crossover cable between their network ports, and (2) hiring a dedicated check-out clerk who was solely responsible for entering encounter form data. (In Kenya, such a clerk receives approximately $60 US per month.) The entire MMRS database sits on the “mother” (registration) computer, whereas the “child” (data entry) computer writes to the database on the mother computer, to which the printers and Zip drive are connected.
Redirecting Patient Flow
Under the paper-based record system, the patients would leave after receiving their drugs and/or educational materials and visiting the financial office, taking their patient information booklets with them. During the first several months of MMRS activity, patients often took their encounter forms with them, preventing their data from being entered into the MMRS. Vigilance by the clerks and other clinic staff reduced the number of lost encounter forms dramatically, but the problem persisted. Several additional actions were taken to redirect patient flow toward the check-out window, including closing and locking a gate that allowed them to avoid walking past the check-out window, adding signage in both English and Swahili, and having the check-in clerk keep the patient's MRHC ID card at the time of check-in, to be returned by the check-out clerk after the encounter form is returned.
Redesign of the Data Entry Screen
For various reasons, mostly lack of computer experience, the data entry clerks had difficulty using a mouse to navigate the encounter form data entry screen. Consequently, the data entry screen was redesigned with tabs that reflected the clinic that the patient visited, another site within the MRHC such as the laboratory or pharmacy, or a specific activity (e.g., entering vital signs). Each tab selects a subscreen that contains all of the fields relevant to that site. These tabs can be selected either by hitting control characters (e.g., alt-F for Family Planning clinic) or with a mouse. Using tabs also allows for easy expansion of the MMRS to include new clinics. For example, Figure 5 shows the tab and data entry fields for MRHC's clinic.
In addition, we added partial name lookup for entering data in which the data entered must be a dictionary term. Using partial name lookup and the tabs for navigating the screen has reduced data entry time from encounter forms to 30–90 seconds each.
Impact of the MMRS on Care in the MRHC
An electronic medical record system can affect how health care providers deliver care, which, in turn, can affect whether, and how well, they ultimately accept the system. We evaluated the effects of the MMRS on workflow at the MRHC by performing formal time–motion studies before and after implementation. Implementation was divided into three periods (preimplementation, implementation, and final acceptance of the MMRS as the default medical record). We performed identical time–motion studies during the preimplementation and final acceptance periods. Kenyan research assistants carrying personal digital assistants (PDAs, in this case the Palm Pilot V) unobtrusively followed patients, health care providers, and medical record clerks (including the financial officer). The PDA data-entry program was written in Hand-D-Base. When a research assistant first started following a subject, he or she opened a record. When the subject initiated an action (such as standing up to move), an observation was entered into his or her PDA, which assigned it a beginning time (with precision to the second). When it became clear to the research assistant what the activity was, he or she recorded the activity into one of the preestablished sets of categories. When the next activity began, the research assistant entered a new activity into the PDA, which assigned an ending time to the previous activity and a beginning time to the next activity. No conversations were allowed between the person being observed and the research assistant. For patients, these categories were registration, time with provider, laboratory, pharmacy, cashier, waiting, and miscellaneous. For health care providers, the categories observed were time with patients, time with other staff, searching for information, personal activities (eating, drinking, idle, etc.), and miscellaneous. For clerks, the categories were registering patients, other patient interactions, time with other staff, searching for information, writing reports, walking, personal activities, and miscellaneous.
The goal was to follow a minimum of 100 patients, all nurses and other clinical health care providers for one day, and all medical record technicians for multiple days. Patients were followed from the time they walked into the MRHC gate until they left, and the time in each category of activity (see below) was recorded, along with the total time spent in the MRHC. The research assistant picked up the first patient entering the MRHC gate, followed that patient until he or she left the MRHC, and then picked up the next patient entering the MRHC gate. The health care providers and clerks were usually followed for the entire time they worked in the MRHC on the day of observation. The length of the providers' and clerks' workdays varied between four and eight hours. Clerks were followed for two days each during the preimplementation period and for at least a week during the postimplementation period. For these reasons, the providers' and clerks' activities were expressed as a percent of all activities observed for each person throughout the preimplementation or postimplementation periods. Differences between the pre- and postimplementation periods were compared using nonpaired t-tests (nonpaired because some of the providers and clerks changed between the pre- and postimplementation periods).
Results
The First 10,000 Visits
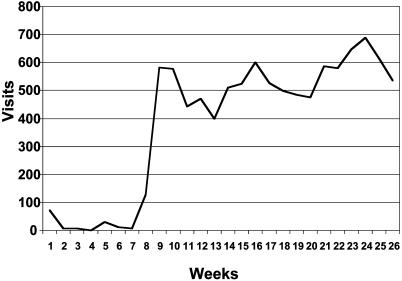
Between February 3 and August 2, 2001, 8,812 individual patients had been registered into the MMRS, of whom 6,190 (70%) visited the MRHC 10,000 times. As shown in ▶, the number of visits with encounter form data rose from just under 100 per week during the first eight weeks to 600 per week by the sixth month of operation. Since August 2001, the data entry clerk has entered encounter form data for more than 95% of all visits. The increase in capture of encounter forms occurred when traffic in the MRHC was rerouted by closing a gate, forcing patients to walk past the check-out window where they turned in their encounter forms, rather than taking them home. During this time, the MRHC staff also used the legacy paper-based system, writing patients' names, diagnoses, and treatments in their logbooks and writing notes in patients' booklets (as described above). In November 2001, the MRHC Director and Matron removed the logbooks from the check-in office and all clinics, after which the MMRS became the MRHC's sole medical record.
Figure 8.
Encounter forms entered into the Mosoriot Medical Record System by week for the first six months.
Of the 6,190 patients making the first 10,000 visits, 57% were female and 33% were male; for 10% the gender was not recorded. Their mean age was 18 ± 16 (SD) years (range newborn to 88 years). The mean age for patients attending the adult medicine clinic was 27 ± 16 years. ▶ shows the clinics visited, with the busiest being adult medicine followed by child welfare (under age 5), pediatrics, and antenatal. ▶ shows the top ten diagnoses and the top ten drugs prescribed, and ▶ shows the tests performed. The predominant problems treated were infections and trauma.
Table 1.
Distribution of Clinics Visited during the First 10,000 Visits with Data Stored in the Mosoriot Medical Record System
| Clinic Visited | No. of Patients | No. of Visits | Mean Age (years) ± SD |
|---|---|---|---|
| Adult medicine | 2,607 | 3,357 | 26 ± 16 |
| Child welfare (age <5 yr) | 962 | 2,254 | 0.8 ± 2.5 |
| Pediatrics (age ≥ 5 yr) | 966 | 1,480 | 3.3 ± 4.2 |
| Antenatal | 504 | 1,192 | 25 ± 6.5 |
| Family planning | 593 | 716 | 28 ± 6.7 |
| Sexually transmitted infections | 16 | 22 | 26 ± 8.2 |
| Not specified* | 544 | 979 | 18 ± 16 |
Most unspecified visits are to the antenatal and family planning clinics, where “diagnoses” are not recorded because there is technically no disease being treated.
Table 2.
Top Ten Primary Visit Diagnoses and Top Ten Drugs Prescribed in the First 10,000 Visits with Data Stored in the Mosoriot Medical Record System
| No. of Visits | |
|---|---|
| Diagnosis | |
| Clinical malaria* | 1,520 |
| Upper respiratory tract infection | 1,161 |
| Malaria | 548 |
| Bronchial pneumonia | 240 |
| Wound, septic | 186 |
| Tonsillitis | 139 |
| Wound, laceration | 116 |
| Myalgia | 108 |
| Gastroenteritis | 105 |
| Conjunctivitis | 98 |
| Drug prescribed* | |
| Acetaminophen | 3,386 |
| Penicillin G injection | 1,506 |
| Sulfadoxine/pyrimethamine | 1,171 |
| Amoxicillin | 994 |
| Tetanus toxoid | 824 |
| Quinine | 1,251 |
| Progesterone injection | 631 |
| Ibuprofen | 486 |
| Chlorpheniramine | 486 |
| Metronidazole | 410 |
Clinical diagnosis of malaria without confirmation by a positive blood smear.
Table 3.
Tests Performed by the Laboratory and Radiology on the First 10,000 Visits with Data Stored in the Mosoriot Medical Record System
| Test Name | Number Performed | Results |
|---|---|---|
| Malaria blood smear | 1,768 | 249 (13%) positive |
| Urinalysis | 335 | Variable |
| Hemoglobin | 322 | 60 (19%) <10 g/dL |
| VDRL* | 296 | 18 (6%) positive |
| Stool examination | 94 | 2 (2%) ova or parasites |
| Widal test† | 88 | 26 (31%) positive |
| Brucella test | 71 | 25 (35%) positive |
| Blood group | 61 | Variable |
Venereal Disease Research Laboratory serologic test for syphilis.
Serologic test for typhoid fever.
Impact of the MMRS
The first time–motion study was performed in January 2001, after pilot testing of the MMRS but before it was used to register patients. The postimplementation time–motion study was performed in January 2002, after the initial implementation of the MMRS and after the paper logbooks had been discontinued for two months. During the preimplementation period, the research assistants recorded 1,142 separate activities for 101 patients, 1,804 activities for 16 health care providers, and 209 activities for five clerks. During the final acceptance period, the research assistants recorded 1,311 activities for 115 patients, 2,258 activities for 14 health care providers, and 3,027 activities for six clerks. As shown in ▶ , during the follow-up period, using the MMRS, patients spent substantially less time with their provider (5 vs. 12 minutes before the MMRS; p < 0.0001) and slightly more time being registered. Overall duration of visits dropped from 41 to 31 minutes, which was not statistically significant.
Table 4.
Results of Formal Time–Motion Study
| Activity | Paper Medical Record System | Electronic Medical Record System | p-value |
|---|---|---|---|
| Patient activities (mean minutes/visit) | 101 Patients | 115 Patients | |
| Waiting | 20.9 | 13.2 | 0.06 |
| Time with provider | 12.2 | 4.9 | <0.0001 |
| Miscellaneous activities | 4.3 | 9.1 | 0.03 |
| Registration | 1.8 | 2.5 | 0.01 |
| Pharmacy | 1.2 | 0.5 | 0.02 |
| Cashier | 0.7 | 0.8 | 0.6 |
| Laboratory | 0.5 | 0.7 | 0.5 |
| Total time per visit | 41.5 | 31.9 | 0.1 |
| Provider activities (% of workday) | 16 Providers | 14 Providers | |
| Time with patients | 33 | 16 | 0.004 |
| Time with other staff | 23 | 8 | 0.0002 |
| Miscellaneous activities | 22 | 26 | 0.6 |
| Personal activities | 15 | 46 | 0.001 |
| Searching for information | 7 | 3 | 0.06 |
| Clerk activities (% of workday) | 5 Clerks | 6 Clerks | |
| Personal activities | 29 | 38 | 0.7 |
| Writing reports | 18 | 2 | 0.2 |
| Time with other staff | 14 | 5 | 0.1 |
| Registering patients | 12 | 22 | 0.1 |
| Other patient interactions | 12 | 15 | 0.7 |
| Miscellaneous activities | 11 | 12 | 0.8 |
| Walking | 2 | 2 | 0.7 |
| Searching for information | 0.5 | 3 | 0.01 |
The reduced time in provider–patient interactions was validated in the observations of the health care providers, where time spent with patients dropped by half: from a third to a sixth of their workday (p = 0.004). Providers also spent two thirds less time interacting with other staff (p = 0.0002) and tripled their time spent in personal activities (15% vs. 46%; p = 0.001). During the postimplementation period, clerks also spent two thirds less time interacting with other staff and almost doubled their time registering patients. They also spent one sixth of the time writing reports (3% vs. 18%) and more time searching for information (3% vs. 0.5%) during the postimplementation period. Because of the small numbers of clerks observed, only this last difference was statistically significant.
There is additional evidence of the impact of the MMRS on care at the MRHC. The paper logbooks shown in Figure 1 have been discarded permanently because they were never referenced. Any needed data concerning MRHC patient care are now obtained from the MMRS. In addition, the MRHC's Matron noticed two patterns of care on MMRS reports: there was a cluster of sexually transmitted diseases in one village. The Matron dispatched a team of nurses to investigate. She also noticed a lack of child immunizations in another village. She dispatched nurses to this village as well, where 20 children were immunized in the primary school and another 40 were immunized in the village (Kalamai I, personal communication, February 2003). In addition, the Director of the MRHC reports that he must send monthly reports to the Kenyan Ministry of Health regarding, for example, the number of patients seen with selected infectious diseases and the number of childhood vaccinations given. Before the MMRS, creating these reports by hand from the MRHC logbooks took a clerk two weeks. Now they take just minutes. This has allowed the Director of the MRHC to reassign two medical records clerks to perform other duties in the MRHC where they are experiencing staff shortages. Finally, in 2002, the Ministry of Health named the MRHC number one among all Kenyan health centers, the first time that this has occurred. Furthermore, the Provincial Minister of Health and the Ministry's information officers have visited the MRHC to study the MMRS, entertaining plans to make it the default information system for all its health centers (Sawe J, personal communication, February 2003).
Discussion
We have shown that the “digital divide” can be bridged by an inexpensive and reliable electronic medical record system. The key to its acceptance and continued use by the MRHC's clinicians, staff, and patients was the authors' sensitivity to local cultures when designing the system. This was accomplished by involving the MRHC clinicians and staff in the initial design and evolution of the MMRS. These Kenyans developed a sense of pride and ownership of their ambulatory electronic medical record system, a system that is unique in Kenya and all of sub-Saharan Africa. Another key to gaining trust, necessary for the initial and sustained success of the MMRS, was the fact that it was developed and maintained mostly by Kenyans—faculty and technicians from MUCHS.
However, implementation of the MMRS was neither simple nor easy. MRHC staff had to be convinced that taking on the additional burden of a new electronic medical record system and the training it required would ultimately result in improvements in the processes and outcomes of care. This burden was especially high during the initial implementation period, when both the electronic and paper record systems were being maintained. We also had to make substantial changes in the design and implementation of the MMRS as early experience did not bear out some of our initial assumptions. For example, we assumed that a single medical record clerk could both register patients and enter data from the encounter forms. This could not be done, so we had to add a second computer and a second data entry clerk. Although this made the system more expensive and may jeopardize its sustainability in MRHC and implementation at other health centers, we had to compromise. Even though the MMRS was conceptualized and developed by an international team of experienced medical informaticians collaborating with Kenyan faculty and staff, it was impossible to predict exactly how the system would be used or what its impact on health care delivery would be. Flexibility and compromise are keys to any attempt to cross the “digital divide.”
The MMRS clearly changed the flow of health care in the MRHC. Patients spent substantially less time interacting with health care providers. After the time–motion study, the providers said that before the MMRS each clinic had a separate logbook in which information identical to that entered into the registration logbook was duplicated. In addition, each patient had a small booklet in which patient notes were written in longhand. With the MMRS, the logbooks and the patient booklets were both replaced by the MMRS encounter form (▶), which used mostly check boxes to store information and which, at the conclusion of the visit, was handed to the patient to take home.
Patients also spent substantially less time waiting, and their total time per visit to the MRHC was marginally shorter after implementation of the MMRS. Health care providers (nurses and clinical officers) also spent less time with patients and other staff and had substantially more time for personal activities. It seems that, for health care providers, the MMRS also saved time, creating a resource that the managers of the MRHC could harness for additional activities (e.g., patient education). Clerks, however, spent additional time registering patients but less time writing reports and interacting with other staff. For them, the MMRS was largely time-neutral for everyday tasks, although it was remarkably timesaving in terms of producing monthly reports for the Kenyan Ministry of Health.
We believe that the MMRS and similar systems can be used to improve health care in developing countries. Such systems can help administrators and managers account for the care they deliver and compete more effectively for scarce medical and financial resources. By identifying patients and problems whose care or outcomes are suboptimal, health centers in developing countries can target limited resources toward specific improvement activities. Despite limited resources, most developing countries have national and international public health initiatives, such as immunizations, that are mostly aimed at disease prevention and health promotion. Electronic medical record systems such as the MMRS can support and enhance these initiatives by helping identify both appropriate targets for these activities and providing outcome data.
A simple, inexpensive, and effective electronic medical record system can be established and work in a resource-poor developing country. The key to its ultimate usefulness will be its sustainability. The more such a system is used to guide care and as a tool for research and development activities, the greater the chance that the costs of implementation and maintenance will be offset by benefits, both financial and in the health of the people served.
Supplementary Material
This study was funded by grant number TW-01082 from the Fogarty International Center of NIH. The opinions expressed herein represent the opinions of the authors and do not necessarily represent their institutions or the funding agency. The authors thank Josephat Sawe, the Director of the Mosoriot Rural Health Centre; Irene Kalamai, the Centre's Matron; and the Centre's clinicians and clerks for their dedication and cooperation. The authors also thank Barasa Otsyula, Dean of the Moi University Faculty for the Health Sciences, and Haroun Mengech, Principal of the Moi University College of Health Sciences, for their energetic and consistent support of this medical informatics program. Thanks also go to George Odhiambo-Otieno, PhD, for his advice and guidance.
References
- 1.Institute of Medicine, Committee on Improving the Medical Record. The Computer-based Patient Record: An Essential Technology for Health Care. Washington, DC: National Academy Press, 1991.
- 2.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press, 1999.
- 3.Institute of Medicine. Crossing the Quality Chasm: A New System for the 21st Century. Washington, DC: National Academy Press, 2001.
- 4.Loomis GA, Ries JS, Saywell RM Jr, Thakker NR. If electronic medical records are so great, why aren't family physicians using them? J Fam Pract. 2002;51:636–41. [PubMed] [Google Scholar]
- 5.Parent F, Coppieters Y, Parent M. Information technologies, health, and “globalization”: anyone excluded? J Med Internet Res. 2001;3:E11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hart DK. Combating technological apartheid in Brazilian Favelas. Available at: <http://www.changemakers.net/journal/00may/hart.cfm>. Accessed May 14, 2002.
- 7.Hannan TJ, Rotich JK, Odero WW, et al. The Mosoriot Medical Record System: design and initial implementation of an outpatient electronic record system in rural Kenya. Int J Med Inform. 2000;60:21–8. [DOI] [PubMed] [Google Scholar]
- 8.Einterz RM, Dittus RS, Mamlin JJ. General internal medicine and technologically less developed countries. J Gen Intern Med. 1990;5:427–30. [DOI] [PubMed] [Google Scholar]
- 9.Einterz RM, Kelley CR, Mamlin JJ, Van Renken DE. Partnerships in international health. The Indiana University–Moi University experience. Infect Dis Clin North Am. 1995;9:453–5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.