Abstract
Physician order entry is a powerful function of a computerized hospital information system. Although designed to be clinician-driven, the imaging section of the order entry system may not be designed optimally to engage the clinician with imaging procedures logically organized for the clinician's typical work patterns. There also may be resistance among overburdened clinicians in having to take the time to learn a new computer system and to assume “clerk's duties” of entering imaging orders. A potential means to address clinician opposition is to cooperatively engage each clinical service in the design of an imaging order entry system with customized menus for each service. This article reports a step-by-step process for the implementation of an imaging order entry system with specialized menus for an orthopedic service. This implementation process includes (1) identification of key personnel, (2) familiarization with the system, (3) discussion and dialogue between key personnel, (4) addressing specific problems, (5) education and orientation of the target group, (6) initial implementation, (7) feedback and improvement, (8) demonstration project (time study) to foster acceptance, and (9) ongoing enhancement.
Many investigators advocate physician order entry (POE) as a desirable component of a computerized health information system (HIS).1,2,3,4 Khorasani5 describes an approach to POE whereby clinicians “choose radiology examinations and their indications from structured menus” as a method to improve quality of care. Yet, POE has been implemented in only about one third of medical sites nationwide and with varied success.6
Imaging order entry is the process by which clinicians order an imaging examination by directly inputting their request in a computerized system, adding relevant history and other data as needed. Radiology departments are dependent on getting accurate information from clinicians so that the correct imaging examination can be performed and interpreted accurately. If an incorrect examination is ordered or there is inappropriate clinical information, radiology personnel often expend time to obtain the correct information. This time spent is not reimbursable.
Veterans Affairs (VA) has been a technology leader in implementation of POE and imaging order entry. Virtually all VA medical centers have physician order entry available, and there is notable clinician usage. For example, in the first quarter of fiscal year 2002, 78% of all inpatient and outpatient medication orders were personally entered by clinicians (Collins B, unpublished data, Veterans Health Administration, 2002). High satisfaction indices are reported.7 Yet, staff clinicians within the VA system also have, at times, expressed frustration in having to assume “clerk's duties” entering the imaging request directly into the HIS. Certainly, administrative mandates and eliminating the option for clerk entry are two methods that can be used to persuade the use of POE. Such directives may create friction, lead to resistance in the proper use of POE, and result in decreased job satisfaction.
Collen1 suggests “…procedures must be developed with and by the users themselves to increase acceptability and decrease required orientation and training. Key physician personnel are required to participate in planning and implementation.” Murff and Kannry7 and Sittig and Stead8 also stress the importance of building order entry menus and procedures with clinician input rather than relying on the input of clerks and other ancillary personnel. Weir et al.9 provide a detailed account of successful global implementation strategies, including physician involvement, an interdisciplinary implementation group, participation of regular staff, proper training and support, and 24-hour assistance.
The above strategies were used at our facility, but there were still resistance and resentment among many clinicians in directly ordering imaging examinations through computerized patient record system (CPRS). We believed that involving clinicians in modifying the off-the-shelf system would serve to encourage the use of imaging order entry. Yet, no standardized method or model was available to facilitate the goal of active clinician input in the construction of imaging order entry. In this article, we describe a strategy used to involve a clinical team in the creation of customized imaging menus and ordering systems. This approach is not intended to replace successful global implementation strategies, but rather to enhance clinician involvement by engendering a sense of ownership.
Background
Hardware
The computer system at the Asheville VA Medical Center is composed of clustered ES-40 PCs (Compaq Computer Corporation, Houston, TX) using the Virtual Memory System (VMS) operating system. Applications for the system are written in the Massachusetts General Hospital Utility Multi-Programming System (MUMPS) language and were created over the past decade by developers at the six VA Regional Software Development Centers. Though our HIS is unique to the VA, the steps described in our implementation strategy could be applied to other systems.
Software
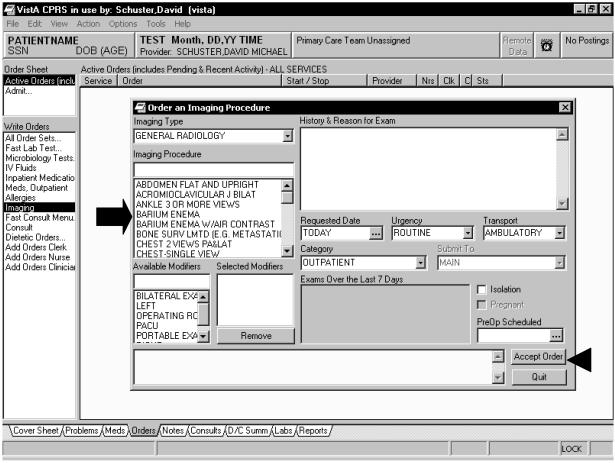
The VA CPRS, which is in use at VA clinics and VA hospitals nationwide, is a client program that interfaces with various clinical components of the VA health information system. A result of the interface is that an electronic patient chart exists for each patient. CPRS is linked to the VA radiology information system version 5.0 (RIS), which includes ordering, tracking, and reporting functionality. The CPRS basic ordering menu is a scroll-down list of all active examinations offered by the imaging service. The examinations are arranged alphabetically by imaging type as shown in ▶. Once an examination is chosen, the clinician types in the history (or copies and pastes from a note) and fills in other relevant information. The order is electronically signed (along with any other orders placed by the clinician), then released to the RIS where it is printed out at a preassigned location and placed in an electronic queue. Once the patient arrives for the examination, the clerk or technologist registers the patient for the requested study.
Figure 1.
An example of the basic imaging order entry screen with a scroll-down alphabetical menu for choosing exams (arrow). The clinician fills in the history and other information as needed, then clicks on “accept order” (arrowhead).
Choice of Clinical Team
Development of POE was a goal of our facility's CPRS task force, established to facilitate the transition from a paper record to a computerized/electronic patient record system. The task force consisted of designated representatives from all clinical and administrative service lines. Clinical representatives included practicing physicians, midlevel practitioners, and nurses. Laboratory, imaging, and pharmacy technicians also were included. Administrative representatives included medical record administration personnel; information management staff; and admission, clinic, and ward clerks.
At the time of implementation, the orthopedic service at the Asheville VA Medical Center consisted of one attending physician who served as the chief of service, two residents, and two physician assistants (PAs). They had approached the task force with feedback about imaging POE, including confusion over the naming of examinations and difficulty in navigating imaging menus to order the appropriate study, especially multipart procedures such as lumbar myelogram with computed tomography (CT) imaging. Although the hectic schedule of this service could be a drawback in learning new technology, the team was highly motivated to improve their efficiency at imaging order entry as a time-saving measure. The authors chose the orthopedic service as a test case because of their initiative in providing feedback and their motivation. We also believed that successful implementation of POE in a demanding clinical service could serve as a positive example for other services in adopting imaging order entry.
The Process
In this section, we outline the process we used to create a menu system for the orthopedic service.
Identification of Key Personnel
To implement modifications within an already established computerized order entry system, it was critical to identify personnel in each service who would be responsible for negotiating, engineering, and implementing these changes. The principal author and the orthopedic attending surgeon agreed to act as clinical champions from their respective services. Clinical champions are physicians who interact daily with patients and use CPRS. They lead specific areas of patient care within the medical center to further electronic implementation, as well as assist in customization and future enhancements of CPRS.
The CPRS clinical applications coordinator (CAC) is a member of the information management staff who interacts with the clinical champion of each service and serves as an ombudsman to information management. Because the CAC is cast in a role of balancing clinical wishes against the practical realities of information management and technology, choosing the right person who has both technology and human relation skills is critical.
Familiarization
The radiologist who initiated the project of POE customization met with the CAC to thoroughly familiarize himself with CPRS, including the capabilities and constraints of the system.
Discussion and Dialogue
The radiologist and the orthopedic surgeon met for three separate 30-minute periods and discussed which elements would be desirable to include in the creation and refinement of an imaging menu tailored for the orthopedic service. The orthopedic surgeon and the radiologist also met with their respective teams in focus sessions to elicit suggestions in the creation of a customized imaging order system for orthopedic surgeons. The radiology focus sessions lasted for approximately 30 to 60 minutes and occurred on two occasions. The orthopedic sessions were performed in various 5- to 10-minute impromptu sessions between surgeries or clinics. Both the radiology service and the orthopedic service gained valuable insights into each other's problems.
Problems Addressed
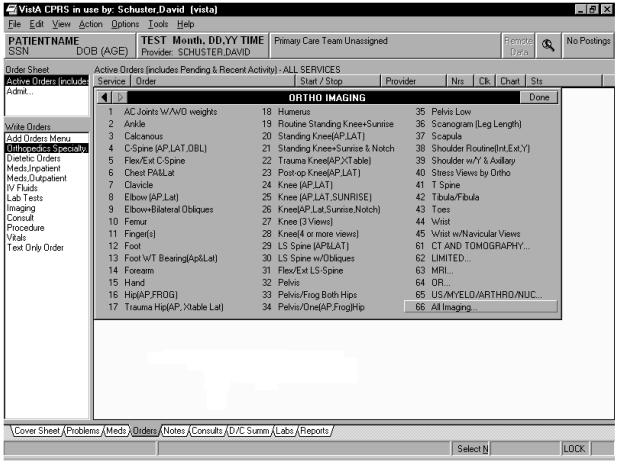
It was noted during a focus group session that clinicians often found it difficult to locate specific imaging examinations among the overwhelming list of formally named studies. Yet, clinicians usually have a core number of examinations that they typically order. It was decided to use a built-in capability of CPRS to depart from the basic menu display as shown in ▶, and use a menu type in which a grouping of imaging examinations and submenu choices could be displayed at once as illustrated in ▶. Use of the latter menu type allowed the orthopedic team to create study names of their choosing, because the menu name merely serves as a pointer to the formally named study within the RIS.
Figure 2.
The ORTHO IMAGING submenu is entered via the main orthopedic specialty menu (not shown). Forty-five plain film examinations chosen by the orthopedic service (choices 1–45) as well as access to other modality submenu screens (choices 61–65) and to the basic à la carte imaging menu (choice 66) are available in this submenu via a mouse click.
Education
Once the clinical champions and the CAC mapped out proposed modifications on paper, members of the orthopedic service were oriented to the new menus with a paper handout. Ideally, this education would be carried out on a mirrored test account, but this option was not available to us as a practical alternative.
Implementation
The new system was inserted within the live CPRS account at a low usage time. The orthopedic surgeon mandated its use by her team at the next outpatient clinic.
Feedback and Real-time Improvement
After the initial implementation, the radiologist and orthopedic surgeon met again and discussed concerns as well as new ideas arising from the use of the modified order entry system. The radiologist in conjunction with the CAC made further revisions to the system. For example, once the orthopedic team understood that the radiologist and CAC were responsive to suggestions, they voiced a long-standing complaint that ordering complex procedures such as myelograms was a time-consuming process that involved searching through the entire imaging menu catalogue for the correct myelogram and CT imaging orders, as well as scheduling, laboratory, and other preparation instructions. This was especially daunting for the residents who were not familiar with the CPRS system. In response, it was decided to take advantage of a built-in functionality of CPRS—the creation of order sets.
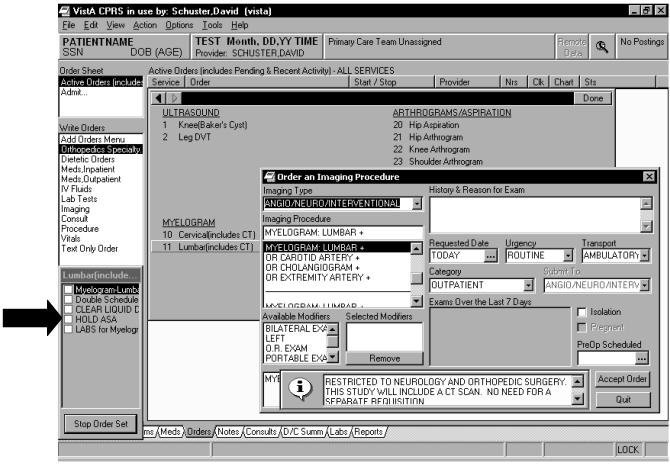
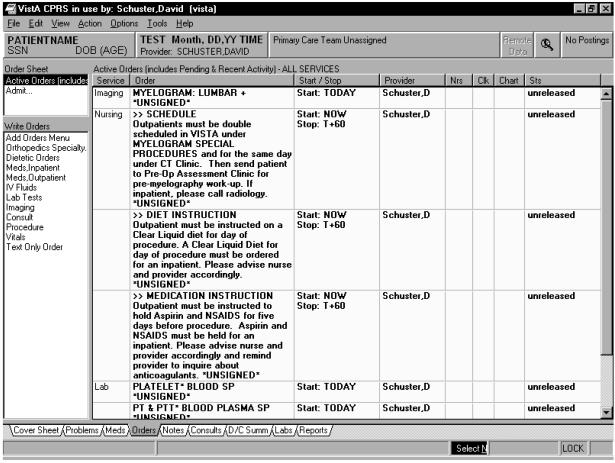
Order sets are a group of predetermined bundled orders that are chosen with a single key click but that can still be modified before final signature. Order sets combine not only groups of imaging orders, but also other types of orders within the electronic medical record system such as nursing, pharmacy, laboratory, and scheduling instructions. Sittig and Stead8 have reviewed the benefit of order sets. Order sets also serve as clinical guidelines checklists for quality assurance, because desired orders are prepackaged without reliance on clinician memory for execution.3 Order sets for myelograms as shown in ▶ and ▶, as well as arthrograms, hip aspirations, and nuclear medicine–labeled white blood cell scans, were formulated by the clinical champions. The CAC created the order sets within CPRS via simple responses to a series of system-prompted questions.
Figure 3.
ULTRASOUND/MYELOGRAM/ARTHROGRAM/NUCLEAR MEDICINE submenu with lumbar myelogram order set chosen. Note order set list in the lower left corner of the screen, which automatically is checked off as each choice is presented (arrow).
Figure 4.
The creation of quick order sets allows preset orders to be defined and generated with a few mouse clicks. The lumbar myelogram order set chosen in ▶ includes scheduling, medication, and laboratory orders.
Demonstration Project (Time Study) to Foster Acceptance
After the above modifications were made to the POE system, a time study was undertaken for the purpose of demonstrating to the members of the orthopedic team the ease of use of the redesigned imaging menu system and the time-saving convenience of the order sets. Because there were only five members of the team, the study was not designed for statistical power. Rather, it was formulated as a method to foster interest in the potential advantages of using the menus and order sets. The orthopedic team was given a series of contrived tasks using the basic imaging menu (old system) versus the specially constructed order screens (new system). This demonstration study presented in ▶ showed impressive overall time savings with the new system, especially for complex tasking and for less-experienced users (the second PA and residents). The results of the time study were shared with the orthopedic team, which elicited enthusiasm.
Table 1.
Task Performance Using New (Custom Menu) versus Old (Basic à la Carte) System
| Attending | PA 1 | PA 2 | Resident 1 | Resident 2 | |
|---|---|---|---|---|---|
| Task 1: Order 5 separate exams | |||||
| Task 1—old | 2:05 | 2:15 | 4:30 | 3:40 | 4:25 |
| Task 1—new | 2:17 | 2:25 | 2:18 | 3:00 | 3:18 |
| Task 1—difference | +:12 | +:10 | −2:12 | −:40 | −1.07 |
| Task 2: Order myelogram and hips aspiration with lab, prep, and scheduling | |||||
| Task 2—old | 4:00 | 5:00 | 5:40 | 9:15 | 6:45 |
| Task 2—new | 1:50 | 1:25 | 1:41 | 1:40 | 1:30 |
| Task 2—difference | −2:10 | −3:35 | −3:59 | −7:35 | −5:15 |
These data were shared with the orthopedic team to generate excitement about the advantages of physician order entry.
NOTE. Average time savings for task 1 = :43; average time savings for task 2 = 4:31 (time is in min:sec). For “difference row”: “+” is increased time with the new system, “−” is time saved.
PA = physician assistant.
Ongoing Enhancement
The process described above is dynamic. Several iterations were required for the final product. Also, as new examinations are developed and Centers for Medicare and Medicaid Services (CMS) rules change, the menu system may have to be modified. The orthopedic service has continued to assess the imaging POE through its clinical experience and can request modifications from radiology and the CAC.
Discussion
In a seminal paper on medical information systems (MIS) published in 1970, Collen1 states: “Physicians should enter their medical orders directly into the computer. The use of clerk technicians to enter into a hospital information system the medical orders handwritten by doctors is merely to mechanize the traditional manual operational mode…. On-line verification of data entered into the patient computer record by the one who generated the data minimizes errors and insures highest quality data.”
Computerized physician order entry has numerous advantages compared with traditional modes of order entry, including decreased medical errors,10 yet at the cost of increased user time.11,12 If computerized medical systems are developed in isolation from day-to-day clinical concerns, they will not likely achieve maximal acceptance despite the provision of adequate training. Including (and empowering) clinicians in design and implementation is a simple yet profound concept that may be overlooked in the desire of administrators to realize perceived cost saving by hastening the implementation of advanced technology.
Khorasani5 states that a well-designed POE is desirable. Yet, technology that is not accepted often is doomed to fail no matter how innovative it may be. Creating a better product by including end users in the software design, development, and improvement process is not a novel idea. Yet, we believe that providing a good product is only part of the approach that will increase clinician “buy-in” of POE. Even when software is implemented after a development process in which clinician input had been sought initially, ongoing feedback is critical. Many investigators have stressed that an interactive and inclusive dialogue between clinicians and developers has value in terms of better acceptance of clinician order entry.1,7,8
The imaging order entry system developed for the orthopedic service as a result of this process is still in use nearly two years postimplementation, and there has been a continuous positive response. The total amount of effort that went into the project (approximately two working days) was small compared with the positive impact of the menu modifications in terms of cumulative time saved for the orthopedic service as well as good will generated for CPRS and POE. In retrospect, it would have been useful to lighten the orthopedic clinic workload on the day of initial implementation and to relieve the radiologist of clinical responsibilities during time spent working on this project. This was not possible at our facility because of clinical volume and shortage of personnel. Yet, because of the motivation on the part of the clinical champions, it was not difficult to involve both services in engineering change. The importance of this motivation and interpersonal cooperation should not be underestimated. In fact, because the radiologist separated from the facility to move to another state, the process has not been repeated with other clinical services.
Conclusion
The capabilities for customization, individualization, and innovation are important considerations when choosing or developing a product for computerized POE. Every health care facility is unique in terms of personnel and politics. We recommend that others adopt the same process but modify it for the individual needs of their particular facility. Furthermore, this process can be applied outside the orthopedic specialty environment. A series of customized imaging order entry menus can be generated for primary care physicians as well as other specialties. Of course, this system does not stop a clinician from erroneously ordering a study. Informed and involved radiologists, technologists, and clerks are still an important line of defense in this regard. This system does allow a clinician who knows what he or she wants to order, to order it swiftly and correctly and to increase his or her enthusiasm toward POE. The interactive model presented above may be useful as a template to increase end-user involvement and to facilitate the development and implementation process of imaging order entry systems.
References
- 1.Collen MF. General requirements for a medical information system (MIS). Comput Biomed Res. 1970:393–406. [DOI] [PubMed]
- 2.Hawkins HH, Hankins RW, Johnson E. A computerized physician order entry system for the promotion of ordering compliance and appropriate test utilization. J Healthcare Inf Manag. 1999:63–72. [PubMed]
- 3.Chin HL, Wallace P. Embedding guidelines into direct physician order entry: simple methods, powerful results. Proc AMIA Symp. 1999:221–5. [PMC free article] [PubMed]
- 4.Shawker TH, Jones BL, Dinberg MD. Computerized ordering of ultrasound examinations. J Ultrasound Med. 1982:37–40. [DOI] [PubMed]
- 5.Khorasani R. Computerized physician order entry and decision support: improving the quality of care. Radiographics. 2001:1015–8. [DOI] [PubMed]
- 6.Ash JS, Gorman PN, Hersh WR. Physician order entry in US hospitals. Proc AMIA Symp. 1998:235–9. [PMC free article] [PubMed]
- 7.Murff HJ, Kannry J. Physician satisfaction with two order entry systems. J Am Med Inform Assoc. 2001:499–511. [DOI] [PMC free article] [PubMed]
- 8.Sittig DF, Stead WW. Computer-based physician order entry: the state of the art. J Am Med Inform Assoc. 1994:108–23. [DOI] [PMC free article] [PubMed]
- 9.Weir C, Lincoln M, Roscoe D, Moreshead G. Successful implementation of an integrated physician order entry application: a systems perspective. Proc Annu Symp Comput Appl Med Care. 1995:790–4. [PMC free article] [PubMed]
- 10.Bates DW, Leape LL, Cullen DJ, et al. Effects of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998:1311–6. [DOI] [PubMed]
- 11.Overhage JM, Perkins S, Tierney WM, McDonald CJ. Controlled trial of direct physician order entry: effects on physician time utilization in ambulatory primary care internal medicine practice. J Am Med Inform Assoc. 2001:361–71. [DOI] [PMC free article] [PubMed]
- 12.Bates DW, Boyle DL, Teich JM. Impact of computerized physician order entry on physician time. Proc Annu Symp Comput Appl Med Care. 1994:996. [PMC free article] [PubMed]