SYNOPSIS
Objectives
To improve access to prostate cancer treatment for low income uninsured men, California initiated a program called IMPACT: Improving Access, Counseling and Treatment for Californians with Prostate Cancer. The program administered free treatment, case management, counseling, and educational materials to all eligible men until budget cuts led to a state-mandated suspension of enrollment and the establishment of a temporary waitlist in February 2005. To assess the effect of suspension of enrollment on patient outcomes, the authors compared health-related quality of life (HRQOL) in waitlisted and enrolled men.
Methods
Eighty-three men in each group were matched on disease stage, age, and race. HRQOL was captured with the UCLA Prostate Cancer Index short form (PCI-SF), the Medical Outcomes Study Short Form-12 (SF-12), and McCorkle and Young's Symptoms and Degrees of Distress in Patients with Cancer Scale (SDS). Self-efficacy was measured with the Perceived Efficacy in Patient-Physician Interactions (PEPPI) Questionnaire.
Results
At intake, waitlisted men demonstrated significantly more symptom-related distress (2.9; p=0.04) and less perceived self-efficacy (2.5; p=0.005) compared to enrollees. Waitlisted men were significantly less likely to have access to a doctor or nurse case manager, treatment medications, nutrition information, or counseling services (p<0.0001).
Conclusions
Men denied enrollment into the IMPACT program exhibited significantly worse symptom distress and self-efficacy compared to enrolled men at initial assessment. The multivariate model suggests that HRQOL in the waitlisted men may be related to their lack of access to medical services. This data illustrates the importance of ongoing public assistance for low income men with prostate cancer.
Because the primary treatment modalities for early stage prostate cancer appear to be equally effective for most men,1 health-related quality of life (HRQOL) outcomes have become a primary component of medical decision-making.2 However, only recently have researchers begun to explore the effects of access to high quality health care on HRQOL outcomes. Since access to care is influenced by several socioeconomic parameters including income, health insurance status, race/ethnicity, and education level, the relationship between HRQOL and access to care is complex.3,4
Krupski et al. first described the HRQOL of an inadequately insured, multi-ethnic group of prostate cancer patients drawn from a statewide public assistance prostate cancer program, IMPACT: Improving Access, Counseling and Treatment for Californians with Prostate Cancer.2 These subjects represent an extraordinarily impoverished cohort who, without the IMPACT program, would receive either poorly coordinated care or none at all. Both general and disease-specific HRQOL were found to be profoundly worse among low income men than in older men without prostate cancer and in age-matched general population controls.2
A randomized, controlled trial would be the most rigorous way to evaluate the effect of the IMPACT program on HRQOL and clinical outcomes in men with prostate cancer. However, denying access to a public assistance program that provides prostate cancer treatment would be unethical. Nonetheless, in February 2005, the State of California temporarily ceased funding of the IMPACT program; as a direct result, eligible men were no longer enrolled in the program, but placed on a waitlist. We approached the ongoing political process in which reinstatement of program funding is being sought as a rare opportunity to accrue a control group with which to compare outcomes and evaluate the IMPACT program. Hence, to assess the effect of initial suspension of enrollment into a public assistance program for prostate cancer treatment, we compared HRQOL of men enrolled into the IMPACT program with that of men placed on the waitlist.
METHODS
California initiated IMPACT in 2001 to improve access to prostate cancer treatment for low income men. The program administers free prostate cancer treatment to California residents with biopsy-proven prostate cancer who are uninsured or underinsured and whose incomes are below 200% of the federal poverty level.5,6 In addition to primary treatment, IMPACT provides patients with case management; counseling; adjuvant, secondary, and follow-up treatment; and culturally appropriate, literacy-sensitive educational materials. As part of the program's evaluation process, HRQOL, self-efficacy, health behaviors, and satisfaction with care are measured in those who agree to have them tracked.5,6
Upon enrollment in IMPACT, all participants receive a manual that explains the various benefits they receive through the program. Included is an introductory letter from the Program Director and a consent form that explains the risks and benefits of participating in the program's research component, termed the Men's Health Research Survey. Participants are clearly informed that receipt of IMPACT benefits is not contingent upon study participation. Study participation for enrollees involves completing both a telephone interview and mailed questionnaire that ask detailed questions regarding HRQOL. Men complete the combined questionnaire/interview once upon initial enrollment, once after six months of enrollment in the IMPACT program, and once after 18 months of enrollment.
In February 2005, because of state fiscal woes, future funding for the IMPACT program was interrupted and enrollment suspended. At that time a waitlist was created, with plans to enroll these men if funding were reinstated. Men assigned to the waitlist meet the same eligibility criteria as do enrolled men. Those on the waitlist receive the same manual as do enrolled men, and if they consent to participate, they initially complete both the same telephone interview and mailed questionnaires. However, men on the waitlist do not receive any prostate cancer treatment through IMPACT, nor are they assigned a nurse case manager to oversee their care. They do, however, receive the same informational materials, which address the disease and treatment options. The same interview and questionnaires are administered to the waitlist group at three-month intervals until they become enrolled. The baseline survey is taken in both enrolled and waitlisted men after the dissemination of educational materials.
In this study, we specifically evaluated the effect of initial IMPACT enrollment by comparing baseline HRQOL between men enrolled in IMPACT prior to California budget cuts and men placed on the waitlist. We included enrolled men from August of 2004 through February 2005, when the State of California ceased funding the IMPACT program. Men were then waitlisted from February of 2005 until November 2005, when funding was reinstated, at least temporarily. UCLA Institutional Review Board approval was obtained prior to commencing the study.
We assessed general HRQOL with the RAND Medical Outcomes Study Short Form-12 (SF-12, version 2), a 12-item adaptation of the RAND 36-Item Health Survey (SF-36).7,8 The SF-12 quantifies HRQOL into two composite scores, the Physical Component Summary (PCS) and Mental Component Summary (MCS) scales. In addition, the SF-12 quantifies HRQOL into eight multi-item subscales, including physical functioning, emotional well-being, general health, pain, energy, social functioning, and role limitations due to physical or emotional problems. 7,8 The summary scales are scored from 0–100 and converted to a standardized scale with a population mean of 50 and a standard deviation of 10.
We used the Medical Outcomes Study Mental Health Index (MHI-5) to assess emotional well-being. The MHI-5 is comprised of 5 items from the SF-36 that measure emotional well-being,9 and has been validated in diverse populations in detecting major depression, affective disorders, and anxiety disorders.10,11 Responses are scored from 0–100 and then averaged; higher scores indicate better emotional well-being. McCorkle and Young's Symptoms and Degrees of Distress in Patients with Cancer Scale (SDS) was used to measure the degree of distress perceived by patients for ten specific cancer symptoms.12 Responses are scored from 1–5 and summed, with higher scores indicating more symptom-related distress.
We measured perceived self-efficacy in obtaining medical information and physicians' attention to medical concerns with the five-item Perceived Efficacy in Patient-Physician Interactions Questionnaire (PEPPI).13 The PEPPI is a valid and reliable measure of patients' perceived self-efficacy in interacting with physicians. It has been shown to be useful in measuring the impact of empowerment interventions to increase patients' personal sense of effectiveness in obtaining needed health care.13,14 Responses from each item are scored from 1–5 and summed together, with a higher score reflecting lower self-efficacy. We evaluated prostate-specific HRQOL using the UCLA Prostate Cancer Index Short Form (PCI-SF), a 15-item survey that measures urinary, bowel, and sexual function and bother.15,16 The function scales assess incontinence, proctitis, and erectile difficulties, while bother scales measure how troubled the subject is by such symptoms. The PCI-SF scales are scored from 0–100, with higher scores indicating better outcomes.
The telephone interview included the SF-12 and the MHI-5, and the mailed written questionnaire contained the PCI-SF, SDS, and PEPPI. Also, as part of the written questionnaire, subjects were asked several questions regarding access to medical services. These included whether they had a doctor or nurse case manager, whether they were able to go to a hospital or treatment center, and whether they had access to treatment medications, understandable educational materials, nutrition information, and counseling services.
Waitlisted men were matched to a sample of enrolled men on clinical stage, age, and race. Given that detailed clinical information was available only once men became enrolled in the IMPACT Program, clinical data on waitlisted men was usually limited in comparison. However, because a positive biopsy is an eligibility requirement for either the waitlist or the program, pathologic data from diagnostic biopsy results were available. Pretreatment prostate-specific antigen (PSA) and other clinical and pathologic staging information were available for the majority of subjects. In order to best match enrolled and waitlisted men, three staging categories were used: local, local-regional, and metastatic.2 Localized disease included men with a clinical or pathologic stage ≤T2b, Gleason sum ≤7, and an initial PSA of ≤10 (or a post-treatment PSA demonstrating no evidence of recurrence). Local-regional disease included men with a clinical stage T2c, a pathologic stage ≥T3, a Gleason sum >7, and a pretreatment PSA of >10 or a rising PSA following primary treatment.2 Patients were considered to have metastatic disease if they had either a PSA $50 at any time, or any other clinical or pathologic evidence of metastatic disease.
For purposes of matching, age was stratified into categories (<50, 50–59, 60–65, 66–70, and >70 years old). Race was divided into white, Hispanic, African American, and other. Baseline characteristics between the two groups were compared by chi-square tests or, when appropriate, Fisher's exact tests. Multivariate modeling was conducted to compare the scores on the various surveys of men enrolled in IMPACT with the scores of men placed on the waitlist, controlling for clinical stage, age, and race. From the model results, we calculated adjusted means for both enrolled and waitlisted men. All tests were two-sided and were considered statistically significant at p<0.05. All analyses were performed with SAS version 9.1.17
RESULTS
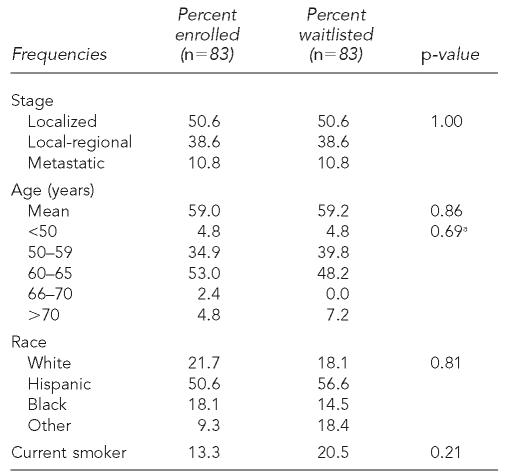
Seventy-nine percent of enrolled men and 74% of waitlisted men participated in the Men's Health Survey. Waitlisted men were matched by stage, age, and race to men from a group of 120 enrollees. After matching, 83 men were available in each of the two groups. For analysis, there were a total of 83 telephone interviews from both the enrolled and waitlisted groups; seventy enrolled men and fifty waitlisted men also completed the written questionnaires. The clinical stage, age, and racial distribution of each group were nearly identical (Table 1). The majority of men in both groups had localized or local-regional disease. The mean age of enrolled men was 59.0 years and 59.2 years for waitlisted men. The majority of men in both groups were Hispanic.
Table 1.
Baseline characteristics of IMPACT enrolled and waitlisted men
Frequency noted with Fisher's exact test.
NOTE: Frequencies were evaluated by chi-square tests.
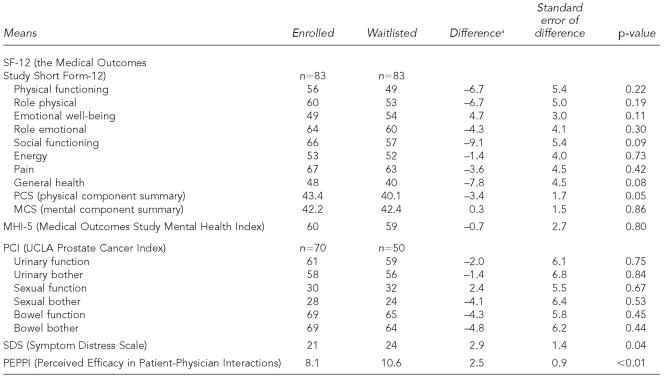
At intake, waitlisted men had significantly more cancer-related symptom distress (as measured by the SDS) compared to enrollees (Table 2). Waitlisted men also demonstrated significantly less perceived self-efficacy on the PEPPI (2.5; p=0.005). Although waitlisted men scored lower on the SF-12 physical component summary, this finding did not reach statistical significance (–3.4; p=0.05). There were no other significant differences in mental health between groups as measured by the Medical Outcomes Study Mental Health Index (MHI-5) and the SF-12 mental component summary (MCS). There were no significant differences in the other SF-12 subscales, including physical functioning, role physical (problems with work or other daily activities as a result of physical health), emotional well-being, role emotional (problems with work or other daily activities as a result of emotional problems), social functioning, energy, pain, and general health. There were no significant differences between enrolled and waitlisted men in any of the six urinary, sexual, or bowel function and bother domains of prostate-specific HRQOL as measured by the PCI-SF.
Table 2.
Adjusted baseline HRQOL mean scores for IMPACT waitlisted and enrolled men (controlling for stage, age, and race)
Calculated prior to rounding.
HRQOL=health-related quality of life
IMPACT=Improving Access, Counseling and Treatment for Californians with Prostate Cancer.
Waitlisted men were significantly (p<0.0001) less likely to have access to a doctor or nurse case manager (14% vs. 83%), treatment medications (44% vs. 83%), nutrition information (60% vs. 91%), or counseling services (46% vs. 86%), compared with enrollees (data not shown). They also considered themselves less likely to have access to understandable educational materials compared with enrolled men (68% vs. 93%; p<0.01). Although waitlisted men considered themselves less able to go to a hospital/treatment center (68% vs. 83%; p=0.06) and less able to go to quality doctors (62% vs. 77%; p=0.07) compared to enrolled men, these analyses did not reach statistical significance.
DISCUSSION
The control group in this evaluation, a group of men placed on a waitlist for public assistance, resulted from a very unusual political and financial situation that is expected to be temporary. Measuring HRQOL in the waitlisted group is an ethical way to make use of an unenrolled group with whom to compare outcomes over time. In this study, we exclusively compared HRQOL at initial intake between men enrolled in the IMPACT program and men placed on a waitlist. We found that men enrolled in the program had less symptom-related distress and better self-efficacy than did men assigned to the waitlist. One might assume that these findings resulted from the waitlisted group having worse disease, but we purposely matched by disease burden.
Men placed on the waitlist differed from men enrolled in the IMPACT program in one major way: they did not receive access to a public assistance prostate cancer program. Rather, they were placed on a waitlist with no guarantee that they would become enrolled in the assistance program; they remained uninsured. Penson et al. previously found that men with prostate cancer who lacked health insurance had significantly worse HRQOL scores over time compared with insured men.4 We attribute the worse HRQOL in the waitlisted group to a lack of access to the care that would have been provided by the public assistance program.
Although it might be expected that placement on the waitlist would have a negative impact on patients' emotional well-being and mental health, we found instead a negative effect on symptom-related distress. This might be explained, at least in part, by unmet expectations among men on the waitlist compared with enrolled men and by less availability of resources for learning and health care management. In an outpatient questionnaire study of adults reporting a health concern to one of several family practice, internal medicine, and cardiology physicians, patients who perceived an unmet expectation for care reported less satisfaction with their visits and less improvement in their condition compared with patients whose expectations for care were met.18 Being placed on a waitlist, rather than provided with treatment, clearly fails to meet the expectations of uninsured men with prostate cancer who otherwise cannot pay for care. It is not surprising, therefore, that waitlisted men were found to have worse symptom-related distress. We speculate that this was a direct result of having unmet expectations; that is, their hopes for care were dashed.
We also found that waitlisted men had lower perceived self-efficacy in interacting with physicians compared with enrolled men. In a previous study of perceived self-efficacy among low income men with prostate cancer enrolled in the IMPACT program, Maliski et al. found that men were more likely to have low self-efficacy if they had diminished overall satisfaction with their care, if they lacked confidence in their providers, or if they had more symptom distress.14 Based on questionnaire responses, waitlisted men were significantly less likely to have access to a doctor or other medical treatments and services compared with enrollees. This lack of access to care among waitlisted men is an obvious source of dissatisfaction with care that may have resulted in lower confidence in their ability to interact with physicians. Maly et al. similarly demonstrated a positive relationship between patient-physician interactions and patient self-reported health, physical function, and satisfaction with care.19 As expected, men on the IMPACT waitlist claimed to have less access to a doctor than did enrollees. Less access to a physician would prevent the development of a stable physician-patient relationship, and therefore might further contribute to poorer self-reported health status and physical function.
Finally, even though the waitlisted men received the same culturally appropriate, literacy-sensitive educational materials as enrolled men, they nonetheless reported substantially worse access to educational materials. It may be that receiving written materials alone, without the coordinated care provided by the physicians and nurse case managers of IMPACT, is insufficient for these men to feel that they fully comprehend their disease. Our findings provide an avenue for further research on how best to educate underserved men with prostate cancer.
This study has several limitations. Because randomization is not ethical in such circumstances, we used matching to control for other variables that could account for the baseline differences in HRQOL between these groups. However, our matching was not exact in any category. Staging categories made use of the limited clinical data available in the waitlisted group and may not reflect the true pathologic stage of disease for all men. However, it is difficult to postulate any reason that in February 2005 this underinsured population would suddenly present with higher stage disease. In addition, since the initial intake for the enrolled men in this study began in August 2004, approximately six months prior to that for men on the waitlist, history represents a threat to internal validity of this study.20 Since the control (waitlist) and intervention (enrolled) groups were staggered in time, it is possible that external change-producing events occurred in one group only (such as a new treatment program for prostate cancer affecting one of the two groups), affecting measured outcomes. It is also possible that the measured differences in QOL between the two groups were due to other internal factors, such as the waitlist group being generally more desperate. Also, the outcomes between groups may have been different based on chance alone, given that we tested multiple outcomes but set the p-value to 0.05.
We compared HRQOL between the groups only at the time of enrollment or waitlist assignment. Ideally, assessing the effect of the IMPACT program on HRQOL would best be performed by comparing HRQOL in enrolled and waitlisted men longitudinally. Although repeat surveys are currently being performed at designated intervals in the waitlisted men, the profoundly worse HRQOL in waitlisted men at initial intake, which we attribute to the uncertainty of receiving IMPACT services, warranted reporting of these early findings. The negative impact on HRQOL in men with prostate cancer denied access to a statewide public assistance program supports our position that ongoing and continuous financial support is crucial for public health care assistance programs. Although cyclical budget cuts are often necessary for the economic stability of any municipal entity, prioritizing early treatment for prostate cancer in low income, uninsured men who otherwise might not receive timely treatment is ultimately a more humane course of action and one that Hippocratic principles compel us to seek.
Underserved men with prostate cancer placed on the waitlist for a public assistance program exhibited significantly worse symptom-related distress and lower self-efficacy compared with men enrolled into the program. Our multivariate model suggests that HRQOL in the waitlisted men may be associated with their lack of access to medical services. These data illustrate the importance of ongoing public assistance for low income, uninsured men with prostate cancer.
Footnotes
The analyses, interpretations and conclusions in this manuscript are those of the authors, not the State of California.
REFERENCES
- 1.D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–74. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 2.Krupski Tl, Fink A, Kwan L, Maliski S, Connor SE, Clerkin B, Litwin MS. Health-related quality-of-life in low income, uninsured men with prostate cancer. J Health Care Poor Underserved. 2005;16:375–90. doi: 10.1353/hpu.2005.0037. [DOI] [PubMed] [Google Scholar]
- 3.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS. The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol. 2001;54:350–8. doi: 10.1016/s0895-4356(00)00312-7. [DOI] [PubMed] [Google Scholar]
- 5.Gore JL, Krupski T, Kwan L, Fink A, Litwin MS. Mental health of low income uninsured men with prostate cancer. J Urol. 2005;173:1323–6. doi: 10.1097/01.ju.0000152312.28002.ad. [DOI] [PubMed] [Google Scholar]
- 6.Maliski SL, Clerkin B, Letwin MS. Describing a nurse case manager intervention to empower low income men with prostate cancer. Oncol Nurs Forum. 2004;31:57–64. doi: 10.1188/04.ONF.57-64. [DOI] [PubMed] [Google Scholar]
- 7.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Ware J, Jr, Kosinski M, Keller SD. Boston: The Health Institute, New England Medical Center; 1995. SF-12: how to score the SF-12 physical and mental health summary scales. [Google Scholar]
- 9.Revick DA, Sorensen S, Wu AW. Reliability and validity of physical and mental health summary scores from the Medical Outcomes Study HIV Health Survey. Med Care. 1998;36:126–37. doi: 10.1097/00005650-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29:169–76. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Gresenz CR, Sturm R, Tang L. Income and mental health: unraveling community and individual level relationships. J Ment Health Policy Econ. 2001;4:197–203. [PubMed] [Google Scholar]
- 12.McCorkle R, Young K. Development of a symptom distress scale. Cancer Nurs. 1978;1:373–8. [PubMed] [Google Scholar]
- 13.Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46:889–94. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 14.Maliski SL, Kwan L, Kurpski T, Fink A, Orecklin JR, Litwin MS. Confidence in the ability to communicate with physicians among low income patients with prostate cancer. Urology. 2004;64:329–34. doi: 10.1016/j.urology.2004.03.042. [DOI] [PubMed] [Google Scholar]
- 15.Litwin MS, McGuigan KA. Accuracy of recall in health-related quality-of-life assessment among men treated for prostate cancer. J Clin Oncol. 1999;17:2882–8. doi: 10.1200/JCO.1999.17.9.2882. [DOI] [PubMed] [Google Scholar]
- 16.Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002–12. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 17.SAS Institute, Inc. SAS v. 9.1. Carey (NC): 2003. [Google Scholar]
- 18.Bell RA, Kravitz RL, Thom D, Krupat E, Azari E. Unmet expectations for care and the patient-physician relationship. J Gen Intern Med. 2002;17:817–24. doi: 10.1046/j.1525-1497.2002.10319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maly RC, Bourque LB, Engelhardt RF. A randomized controlled trial of facilitating information giving to patients with chronic medical conditions: effects on outcomes of care. J Fam Pract. 1999;48:356–63. [PubMed] [Google Scholar]
- 20.Campbell DT, Stanley JC. Experimental and quasi-experimental designs for research. Chicago: R. McNally; 1966. [Google Scholar]