SYNOPSIS
Objectives
This study was conducted to describe the national magnitude and characteristics of acute pesticide poisoning among workers and customers in retail establishments.
Methods
Analyses included retail employees 15–64 years of age and customers with acute pesticide poisoning identified from the Sentinel Event Notification System for Occupational Risks-Pesticides (SENSOR-Pesticides) and California Department of Pesticide Regulation from 1998 to 2004. Pesticide poisoning incidence rates and incidence rate ratios (IRR) were calculated.
Results
A total of 325 cases of acute pesticide poisoning were identified. Of these cases, 287 (88%) were retail employees and 38 (12%) were customers. Overall, retail employees had a significantly lower acute pesticide poisoning incidence rate compared with non-agricultural, non-retail employees (IRR=0.53; 95% confidence interval 0.47, 0.59). However, significantly elevated pesticide poisoning incidence rates were observed for four retail occupations (janitors, stock handlers/baggers, bakery/deli clerks, and shipping/receiving handlers). In addition, workers employed in two retail industry sectors (farm supply stores and hardware stores) had significantly elevated acute pesticide poisoning incidence rates. Incidence rates among the retail employees demonstrated a quadratic trend, monotonically decreasing from 1998 to 2000 and monotonically increasing from 2000 to 2003. The rates appear to have leveled off in 2003 and 2004.
Conclusions
Preventive measures to decrease acute pesticide poisoning incidence in the retail sector include adoption of unbreakable and tear-resistant container requirements, increased utilization of integrated pest management strategies, and advisement to store managers, employees, and customers about poisoning prevention.
Many retail establishments sell pesticides such as insecticides, herbicides, and disinfectants for home and garden use. In the U.S. from 1982 to 2001, the total annual expenditure of home and garden pesticides increased from $1.2 billion to $2.2 billion.1 Excluding chlorine and hypochlorites, the home and garden expenditure in 2001 accounted for 19% of the total pesticide market and consisted mostly of insecticides/miticides ($1.3 billion) and herbicides/plant growth regulators ($631 million).
Retail employees may come into contact with these potentially hazardous chemicals while performing routine occupational activities. In addition, some retail employees may be required to handle, mix, and apply pesticides. Furthermore, retail employees and customers may be directly exposed to pesticides through spills, sprays, drift, and damaged pesticide containers, or indirectly exposed to residues left by these exposure scenarios.
Since large quantities of pesticides are sold at retail stores and since there is currently a lack of information regarding the risk of pesticide poisoning in the retail industry, we sought to address this topic. In order to estimate the national magnitude and describe the characteristics of acute pesticide-related illnesses associated with retail pesticide exposures, we examined acute pesticide poisoning surveillance data from U.S. state-based agencies for the years 1998 through 2004. This article also proposes recommendations to reduce the risk of pesticide poisoning in the retail industry. To our knowledge, this is the first comprehensive paper to describe pesticide-related illnesses among retail workers and customers.
METHODS
We obtained surveillance data for retail workers 15–64 years of age and all customers who developed an acute pesticide-related illness resulting from exposure at a retail establishment from 1998 to 2004. This analysis excluded exposures that were intentional, asymptomatic, agriculturally-related, volunteer cases (i.e., non-paid workers), or a result of drift from a nearby non-retail establishment application. The cases included retail workers exposed during routine work activities, retail workers exposed while applying or handling pesticides, and non-working individuals (i.e., customers) exposed in a retail establishment. The age range for cases was chosen a priori and should generally have captured most retail workers.
State agencies that contributed data to this project include the California Department of Pesticide Regulation (CDPR) and the following Sentinel Event Notification System for Occupational Risks-Pesticides (SENSOR-Pesticides) programs: the California Department of Health Services (CDHS), the Texas Department of State Health Services, the Washington State Department of Health, the Florida Department of Health, the Oregon Department of Human Services, the Michigan Department of Community Health, the New York State Department of Health, and the Louisiana Department of Health and Hospitals. There were no reported cases that met the inclusion criteria from the Arizona Department of Health Services, which also has a SENSOR-Pesticides program. The principal sources of cases used by these state agencies are poison control centers, workers' compensation agencies, and the state agencies responsible for pesticide regulation. SENSOR-Pesticides is a program through which the National Institute for Occupational Safety and Health (NIOSH) provides technical and funding support to state health departments to conduct acute pesticide poisoning surveillance.2 The U.S. Environmental Protection Agency (EPA) also provides funding support to SENSOR-Pesticides. Data aggregation for the program began in 1998 when the case definition was finalized,2 and the most recent year of available data is 2004.
The time period for data collection of acute pesticide poisoning varied by state agency. SENSOR-Pesticides programs in California, Florida, New York, Oregon, Texas, and Washington, in addition to CDPR, provided data for the entire study period. Data were available for the following SENSOR-Pesticides programs for the given years: Arizona, 1998–2001; Louisiana, 2000–2004; and Michigan, 2000–2004.
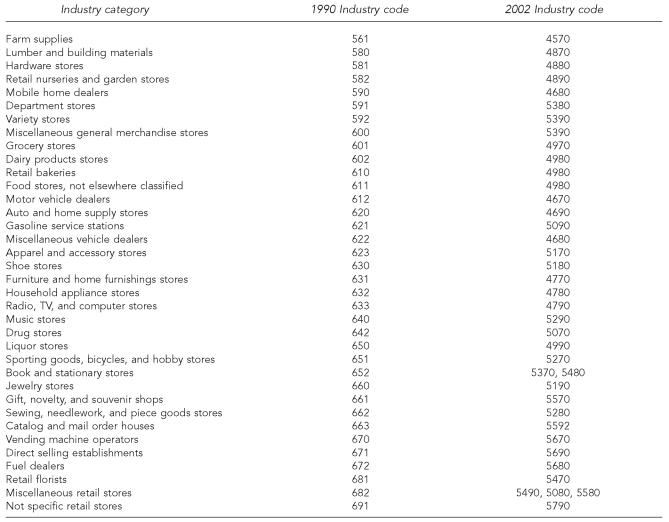
The 1990 and 2002 Bureau of the Census (BOC) industry codes (BOCIC) were used to define the retail industry categories.3,4 Figure 1 displays the BOCIC codes included in the paper.
Figure 1.
The 1990 and 2002 Bureau of the Census Industry Codes (BOCIC) used to define the retail industry categoriesa
a Additional information on the BOCIC is available in references 3 and 4 of this article.
Data collected by the state surveillance systems included date of exposure, case information (age, gender, state of residence, signs, symptoms, illness severity, and category according to the case definition), industry, occupation, activity at time of exposure, pesticide acute toxicity category, pesticide functional and chemical class, and active ingredient. Cases from CDHS and CDPR were cross-referenced based on age, sex, month and year of exposure, and pesticide active ingredient to check for duplicates. Any matching cases were assumed to be the same individual and were counted only once. Additionally, state agencies provided the surveillance data to NIOSH without personal identifiers, thus exempting this work from review by the human subjects review board.
Illness severity was assigned to all cases using standardized criteria.5 The severity index is based on signs and symptoms, medical care received, and lost time from work or normal activities. Low severity illness or injury typically consists of health effects that may not require treatment, with minimal time (<3 days) lost from work or normal daily activities. Moderate severity illness or injury consists of non-life-threatening health effects that generally receive treatment, and normal functioning returns without risk of disability. Time lost from work or activities is generally less than five days. High severity illness or injury consists of life-threatening health effects that usually require hospitalization and may result in permanent disability. Considerable time (more than five days) is often lost from work or activities. Death is the severity category assigned to fatalities resulting from pesticide exposure.
The pesticide acute toxicity category, as defined by the U.S. EPA, was acquired for all pesticide products that resulted in illness or injury from exposure. The U.S. EPA classifies all pesticide products into one of four acute toxicity categories based on established criteria.6 The most toxic products are classified in category I, while the least toxic are classified in category IV. State-based surveillance programs provided most of the data for the acute toxicity category. For cases without this information, the toxicity category was obtained from a dataset provided by the U.S. EPA.
Case definition
The SENSOR-Pesticides program utilizes a standardized case definition.7 Cases were classified into one of the following categories: definite, probable, possible, or suspicious. Classification was conducted by state-based surveillance experts, and was dependent upon the strength of evidence for pesticide exposure and whether heath effects were reported as signs by a health care professional or as symptoms by the exposed case. Cases classified as definite, probable, or possible had to have health effects that were consistent with the current toxicological literature on the given pesticide. Cases were classified as suspicious when limited toxicological data was available on the pesticide. The CDPR uses a similar case definition.8
Data analysis
SAS Version 9.1 was used to perform data management and statistical analysis.9 Chi-square analysis was performed to determine whether case definition category, age, sex, year, work-related category, pesticide toxicity category, or pesticide functional class were associated with differences in illness severity.
We calculated the incidence rates among retail workers by year, occupation, and industry. For each rate, the numerator was the number of acute pesticide-related illnesses for the category of interest, and the denominator was calculated using full-time equivalent (FTE) estimates from the 1998–2004 Current Population Survey (CPS).10 The comparison group consisted of workers employed in non-agricultural, non-retail industries (these industries include construction, manufacturing, services, transportation, communication, utilities, and public administration, and account for approximately 43% of the pesticide poisoning cases identified by the SENSOR-Pesticides program).2 The incidence rates for workers in non-agricultural, non-retail industries were similarly calculated; SENSOR-Pesticides and CDPR provided the numerator data and CPS the denominator data for these workers. We excluded agricultural workers from the comparison group, as previous work has indicated that they have a much greater incidence rate of pesticide poisoning than non-agricultural workers.2 (From 1998 through 1999, the SENSOR-Pesticides program reported an incidence rate among agricultural workers of 182/million FTEs as compared to 13/million FTEs among non-agricultural workers.) Poisson regression was used to test for trends of incidence rates of illness among retail and non-agricultural, non-retail workers from 1998 to 2004. Non-occupational cases (i.e., customers) were excluded from these rate analyses.
Incidence rate ratios (IRRs) were calculated to determine the risk of acute pesticide poisoning while working in a retail establishment. To calculate this ratio, we divided the incidence rate of acute pesticide-related illness among retail workers by the incidence rate among workers in non-agricultural, non-retail industries. A ratio greater than one implied that retail workers had a greater risk of acute pesticide poisoning compared with workers in non-agricultural, non-retail industries, while a ratio less than one suggested a decreased risk. Confidence intervals (95% CIs) were calculated for each rate ratio as described by Rothman.11
RESULTS
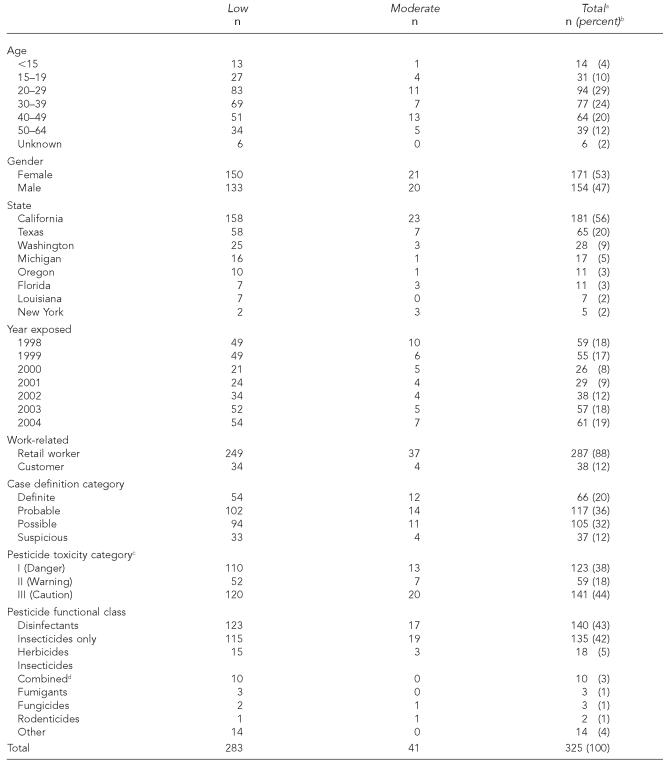
From 1998 through 2004, a total of 325 cases of acute pesticide poisoning associated with pesticide exposure at retail establishments were identified (Table 1). Of these cases, 287 (88%) were retail employees and 38 (12%) were customers. One hundred sixty-seven cases (51%) were obtained from SENSOR-Pesticides and 158 (49%) from CDPR. (Three cases were identified by both SENSOR and CDPR and were excluded from the CDPR total.) The median age was 33 years (range: 2–64 years), 171 cases (53%) were female, and 181 (56%) were from California.
Table 1.
Demographic data, pesticide toxicity, and functional class for 325 cases of acute pesticide poisoning in retail settings by severity category, 1998–2004
One case was classified as a death. This case is found only in the Total column.
Some percentages do not total 100 due to rounding.
Acute pesticide toxicity category as defined by the U.S. EPA. Data was missing for two cases.
Cases exposed to a combination of insecticides and other pesticides.
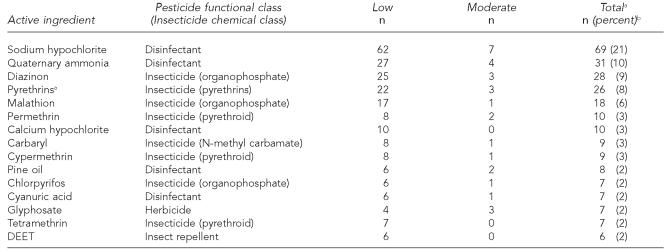
Tables 1 and 2 display the pesticides and active ingredients involved in the pesticide-related illnesses. The pesticide functional classes responsible for the largest proportions of cases were insecticides alone or combined with other pesticides (n=140; 44%), and disinfectants (n=136; 43%). Organophosphorous compounds were responsible for the largest proportion of insecticide cases (n=54; 37%), and the most commonly observed organophosphorous active ingredients were diazinon (n=28) and malathion (n=18). Other commonly involved insecticide chemical classes were pyrethroids (n=28; 19%), pyrethrins (n=26; 18%), N-methyl carbamates (n=13; 9%), and organochlorine compounds (n=5; 4%). All five of the organochlorine cases were associated with one event involving chlordane. Although all approved uses of chlordane in the U.S. were cancelled in 1988,12 these five cases occurred in 1999 at a charity thrift store during the cleanup of a donated bottle of chlordane that broke while workers sorted through donations. The most frequently reported disinfectant active ingredients were sodium hypochlorite (n=69), and quaternary ammonia (n=31).
Table 2.
List of the 15 pesticide active ingredients most commonly associated with acute pesticide poisoning among retail workers and customers, by severity category, 1998–2004
One case was classified as a death. This case is found only in the Total column.
This table does not include all cases so the percents do not sum to 100.
Illness severity is presented in Table 1. Overall, severity was low for 283 (87%) of the cases and moderate for 41 (13%). One death was also identified. The distribution of low and moderate severity did not differ by case definition category (p=0.49), age (p=0.47), sex (p=0.83), year (p=0.78), work-related category (p=0.67), pesticide toxicity category (p=0.65), or pesticide functional class (p=0.61).
The fatal case was a 35-year-old man with a history of asthma who worked as a tire shop service manager. This worker turned on the air conditioner in the tire shop and was exposed to Ditrac® rodenticide (toxicity category = III, chemical class = indandiones, and active ingredient = diphacinone) and Drione® insecticide (toxicity category = III, chemical class = multiple ingredients, and active ingredients = silica gel, piperonyl butoxide, and pyrethrins). These chemicals had been applied the previous night to treat a rat infestation and had leaked into the establishment's ventilation system. The man inhaled the chemicals, and approximately 10–15 minutes later he was coughing, had chest tightness, difficulty breathing, watery eyes, and turned red. He was taken to the hospital and then discharged the same day. This exposure exacerbated a pre-existing asthma condition and required management with large doses of steroidal anti-inflammatory agents. After nearly one month, the steroidal treatment led to a bleeding duodenal ulcer complication with extensive blood loss. Death ensued after the gastrointestinal hemorrhage could not be controlled, despite massive transfusions and surgical intervention.
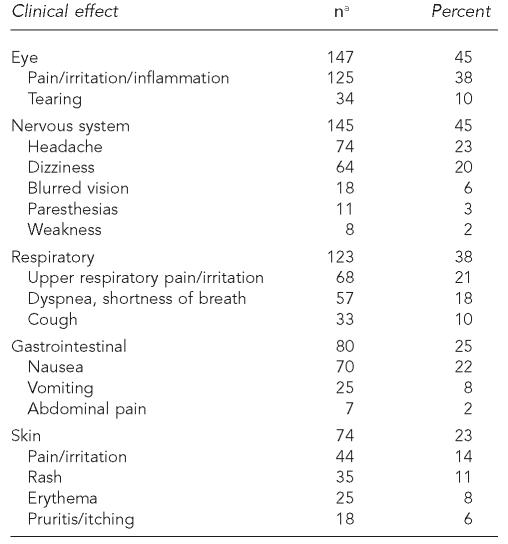
Signs and symptoms observed among the cases were related to the eye (n=147; 45%), nervous system (n=145; 45%), respiratory system (n=123; 38%), gastrointestinal system (n=80; 25%), and skin (n=74; 23%) (Table 3). Specific health effects most commonly experienced by the cases included the following: eye pain/irritation/inflammation (n=125; 38%), headache (n=74; 23%), nausea (n=70; 22%), upper respiratory pain/irritation (n=68; 21%), dizziness (n=64; 20%), and dyspnea (n=57; 18%).
Table 3.
Clinical signs and symptoms of acute pesticide poisoning among retail workers and customers, 1998–2004 (N=325)
The sum of the specific clinical effects do not total the number reported for the system because more than one symptom may have been reported in some cases.
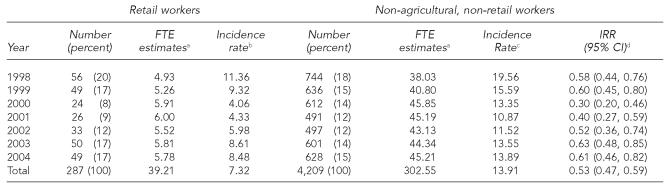
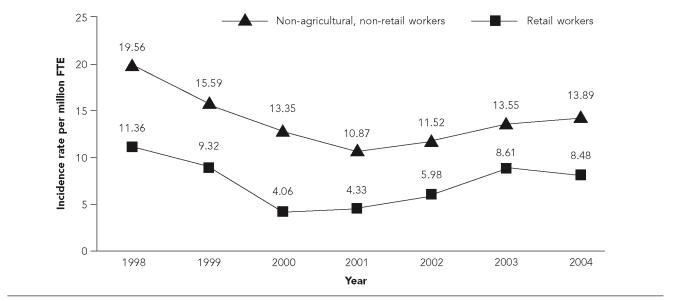
Table 4 and Figure 2 display the incidence rates for the retail and non-agricultural, non-retail workers from 1998 through 2004. For retail workers, the rates demonstrated a quadratic trend, monotonically decreasing from 1998 (when they were the highest at 11.36/million FTEs) through 2000 and monotonically increasing from 2000 to 2003. The rates appear to have leveled off in 2003 and 2004. A similar trend was observed for non-agricultural, non-retail workers. For each year, the incidence rates were significantly reduced among the retail workers compared with workers employed in non-agricultural, non-retail industries. Incidence rates were also calculated by U.S. region (West, South, and East) (Table 5). The western region had the highest incidence rate (13.32/million FTEs), and retail workers in each of the regions had a lower incidence rate compared with workers in non-agricultural, non-retail industries.
Table 4.
Number of acute pesticide poisoning cases among retail and non-agricultural, non-retail workers 15–64 years of age, full-time equivalent estimates, incidence rates, and incidence rate ratios, by year, 1998–2004 (N=287)
FTE = full-time equivalent, in millions.
Incidence rates per million FTEs. Includes only retail workers in Arizona, California, Florida, Louisiana, Michigan, New York, Oregon, Texas, and Washington.
Incidence rates per million FTEs. Includes only non-agricultural, non-retail workers in Arizona, California, Florida, Louisiana, Michigan, New York, Oregon, Texas, and Washington.
Compares the rate of acute pesticide poisoning among retail workers for a given year with non-agricultural, non-retail workers. Cases are those identified by participating SENSOR-Pesticides states.
IRR = incidence rate ratios
Figure 2.
Incidence rates for acute pesticide poisoning among U.S. retail (N=287) and non-agricultural, non-retail workers (N=4,209), 15–64 years, 1998–2004
FTE=full-time equivalent
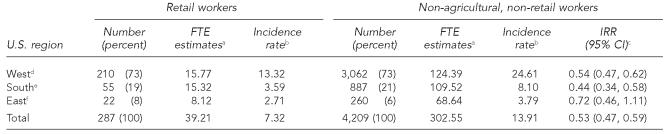
Table 5.
Number of acute pesticide poisoning cases among retail workers 15–64 years of age, full-time equivalent estimates, incidence rates, and incidence rate ratios, by state, 1998–2004 (N=287)
Full-time equivalent, in millions
Incidence rates per million FTEs.
Compares the rate of acute pesticide poisoning among retail workers in a given region with non-agricultural, non-retail workers.
Arizona, California, Oregon, and Washington
Florida, Louisiana, and Texas
Michigan and New York
IRR = incidence rate ratios
CI = confidence interval
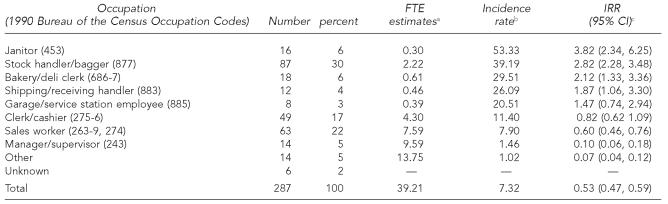
Four occupations in the retail industry were found to have a significantly elevated acute pesticide poisoning incidence rate compared with workers employed in non-agricultural, non-retail industries: janitors (n=16, incidence rate = 53.33/million FTEs; stock handlers/baggers (n=87, incidence rate = 39.19/million FTEs); bakery/deli clerks (n=18, incidence rate = 29.51/million FTEs); and, shipping/receiving handlers (n=12, incidence rate = 26.09/million FTEs) (Table 6). Sales workers (n=63) and clerks/cashiers (n=49) also accounted for a large number of cases; however, their incidence rate of acute pesticide poisoning was not elevated.
Table 6.
Number of acute pesticide poisoning cases among retail workiers 15–64 years of age, full-time equivalent estimates, incidence rates, and incidence rate ratios, by occupation, 1998–2004 (N=287)
Full-time equivalent, in millions
Incidence rates per million FTEs. Includes retail workers in Arizona, California, Florida, Louisiana, Michigan, New York, Oregon, Texas, and Washington.
Compares the rate of acute pesticide poisoning among specific occupations with non-agricultural, non-retail workers. Cases are identified by participating SENSOR-Pesticides states. The incidence rate among non-agricultural, non-retail workers in SENSOR-Pesticides states was 13.91 per million FTEs from 1998–2004.
IRR = incidence rate ratios
CI = confidence interval
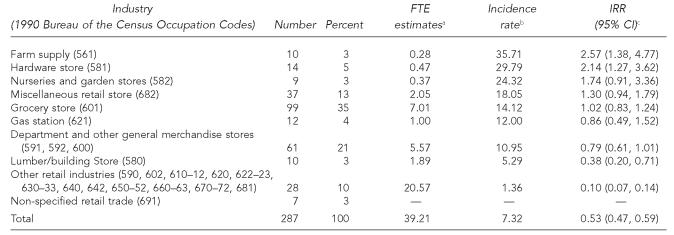
The retail industry sectors with the highest acute pesticide poisoning incidence rates were farm supply stores (n=10; incidence rate = 35.71/million FTEs), hardware stores (n=14; incidence rate = 29.79/million FTEs), and nurseries and garden stores (n=9; incidence rate = 24.32/million FTEs) (Table 7). Two of these sectors had significantly elevated incidence rates: farm supply stores and hardware stores. Grocery stores (n=99) and department and other general merchandise stores (n=61) accounted for a large number of cases; however, the incidence rates in these sectors (14.12/million FTEs and 10.95/million FTEs, respectively) were equivalent to the rate among workers employed in non-agricultural, non-retail industries. Department and other general merchandise stores includes superstores, warehouse clubs, and other department stores that sell a wide range of new products with no one merchandise line predominating.
Table 7.
Number of acute pesticide poisoning cases among retail workers 15–64 years of age, full-time equivalent estimates, incidence rates, and incidence rate ratios, by industry, 1998–2004 (N=287)
Full-time equivalent, in millions
Incidence rates per million FTEs. Includes retail workers in Arizona, California, Florida, Louisiana, Michigan, New York, Oregon, Texas, and Washington.
Compares rate of acute pesticide poisoning among specific industries with non-agricultural, non-retail workers. Cases are identified by participating SENSOR-Pesticides states. The incidence rate among non-agricultural, non-retail workers in SENSOR-Pesticides states was 13.91 per million FTEs from 1998–2004.
IRR = incidence rate ratios
CI = confidence interval
We identified the activities of the 287 retail workers that resulted in pesticide exposure. The majority of workers were exposed while performing routine work activities that did not involve mixing, loading, applying, or disposing of pesticides (n=195; 68%). These routine work activities included: direct contact with spills and/or splashes caused by damaged or dropped pesticide containers (n=44; 23%); bystander exposure involving inhalation from a pesticide application within the retail establishment (n=32; 16%); direct pesticide contact while stocking shelves (n=25; 13%); exposure during checkout (e.g., dropping bottles while scanning or bagging products) (n=22; 11%); and cleaning incidents (i.e., direct contact or splash from disinfecting agents among bakery and deli clerks while cleaning dishes or work surfaces) (n=18; 10%). The remaining occupational activities associated with exposure included: applying pesticides (n=57; 20%); mixing/loading pesticides (n=18; 6%); and transportation/disposal of pesticides (n=15; 5%).
Among the 212 cases with personal protection equipment (PPE) usage information, only 28 individuals (13%) wore PPE. Of these 28 cases, 25 (89%) used disposable or chemical resistant gloves (seven of these 25 individuals reported dermatologic effects), five (18%) used goggles (only one of these five had eye symptoms), four (14%) used chemical resistant clothing (e.g., chemical resistant apron), and three (11%) used cloth/leather gloves.
Non-occupational cases accounted for only 12% of the total cases (n=38). The median age for customers was 28 years (range: 2–64 years) and 53% were female. Insecticides accounted for 21 cases (55%), insect repellents for eight (21%), disinfectants for four (11%), herbicides for three (8%), and other pesticides for two (7%). Exposure scenarios among customers included: direct contact from spills and/or splashes caused by damaged or dropped pesticide containers (n=13; 34%), children spraying themselves in the face with a pesticide (n=11; 29%), bystander exposure following a nearby insecticide application (n=5; 13%), and adults inadvertently spraying themselves in the face with a pesticide (n=3; 8%). Incidence rates for pesticide poisoning among retail customers were not calculated.
Case reports
Two occupational cases and one customer case are described below to illustrate the types of exposures that were detected.
Case 1.
A 20-year-old female stock handler at a retail garden store was stocking shelves above her head; the cap of an insecticide container was loose and the liquid (active ingredient = diazinon, toxicity category III) splashed into her eyes. She sought medical attention at an emergency room, where she was diagnosed with lacrimation and chemical conjunctivitis, which resulted in her missing one day from work. The case definition category was definite, severity was low, and PPE use was unknown.
Case 2.
A 50-year-old male, working as a janitor at a retail produce store, was assisting with the unloading of pesticide boxes; a box was open and insecticide dust (active ingredient = acephate, toxicity category III) fell all over his shirt. The janitor washed himself, began to feel ill, and reported muscle weakness, abdominal pain and cramping, nausea, and diarrhea. The man was admitted to the hospital where he stayed for three days and lost one day from work. The case definition category was possible, severity was moderate, and PPE use was unknown.
Case 3.
In 2004, while shopping at a large department store with one of her parents, a 2-year-old girl grabbed a squirt bottle of DEET (toxicity category III) that was on display in the checkout line. The girl then proceeded to spray herself in the eyes. She immediately developed eye pain, irritation, and lacrimation bilaterally. The parent called poison control for management advice. The case definition category was possible and severity was low.
DISCUSSION
The pesticide poisoning incidence rate for all retail workers combined was significantly lower compared with workers in non-agricultural, non-retail industries. However, several retail occupations (janitors, stock handlers/baggers, bakery/deli clerks, and shipping/receiving handlers), and two retail industry sectors (farm supply stores and hardware stores) had significantly elevated rates of acute pesticide poisoning compared with workers in non-agricultural, non-retail industries.
One reason that stock handlers/baggers and shipping/receiving handlers were at risk is that they may often handle individual pesticide containers and would be the workers most likely exposed to containers damaged in transit. These occupations may also drop and inadvertently damage containers while stocking shelves. Baggers can be exposed at customer checkouts, especially from spills and splashes when pesticide containers are dropped or damaged. Janitors are the workers typically required to clean pesticide spills, and our findings suggest that these workers may not always be adequately trained and equipped to perform this work safely. All of the poisoned bakery/deli clerks were exposed to disinfectants used for cleaning dishes and surfaces. These workers need improved training and provision of PPE. Additionally, farm supply and hardware stores typically sell several varieties of insecticides, herbicides, and disinfectants. The large number of pesticide products sold at these stores may place workers at increased risk of pesticide poisoning compared with workers employed in other retail industry sectors.
Overall, the incidence rates of acute occupational pesticide poisoning in the retail industry showed a quadratic trend, monotonically decreasing from 1998 to 2000 and monotonically increasing from 2000 to 2003. The reasons for the quadratic trend are not clear; however, a similar time trend was observed for some common case characteristics. For example, disinfectants or insecticides were responsible for 91% of the occupational retail cases identified in this report and a similar quadratic trend was observed for cases exposed to each of these pesticide functional classes. In addition, most cases were identified from California, and these cases were also found to have a similar quadratic trend. Finally, a similar quadratic trend was observed for all non-agricultural, non-retail workers.
It should be noted that there has been a shift in the chemical classes responsible for illness among those exposed to insecticides. From 1998 through 2001, the organophosphates were involved in 54% of the insecticide cases, whereas from 2002 through 2004, the pyrethrins and/or pyrethriods were responsible for the largest proportion of insecticide cases (49%). The Food Quality Protection Act (FQPA) may be responsible, at least in part, for this trend. In 1996, the FQPA established a new standard for regulating pesticides, in which “reasonable certainty of no harm to infants and children” was used to assess pesticide safety.13 In response to the FQPA, pesticides that may be found on foods are being reassessed by the EPA to assure compliance with this new standard. As a result, uses of several organophosphates have been cancelled.14 For example, almost all residential uses of chlorpyrifos, a previously popular organophosphate insecticide, were cancelled or phased out in 2001, and retailers were prohibited from selling chlorpyrifos-containing products after December 31, 2001 (with the exception of ant and roach bait products in child-resistant packaging).15 Among the seven cases that involved exposure to chlorpyrifos identified in this paper, four were exposed in 2001 or earlier. Among the three exposed after 2001, two were cashiers employed at a large hardware store where, in July 2002, while placing returned merchandise on the shelves, a chlorpyrifos-containing crack and crevice spray can ruptured and sprayed them in the face. In addition, one customer was exposed in 2004 at an unspecified retail establishment when a chlorpyrifos-containing flea and tick spray spilled on her. The products involved in these two post-2001 events had been cancelled and should have been removed from store shelves in 2001.
As for incidence rate by geographic location, states in the western U.S. had the highest incidence compared with the other SENSOR-Pesticides states. While it is possible that western states such as California and Washington may genuinely have a greater rate of illness, these higher rates are more likely due to the fact that these two states have the oldest and most experienced state-based pesticide poisoning surveillance programs in the U.S., and have more staff workers compared with SENSOR-Pesticides programs in the other states.2
A variety of interventions are available to decrease the risk of acute pesticide poisoning among retail workers and customers. Inexpensive efforts include advising store management and employees about the increased risk of illness among janitors, stock handlers/baggers, bakery/deli clerks, and shipping/receiving handlers. Janitors and other workers involved with cleaning pesticide spills need to be taught to consult the pesticide label, the pesticide manufacturer, or the National Pesticide Information Center (1-800-858-7378) to obtain advice on safely managing pesticide spills. The Occupational Safety and Health Administration (OSHA) has established a hazard communication standard that was amended in 1994 that requires employers to provide their workers with information about any chemical hazard exposures present in the workplace.16 This includes providing employees with pesticide labels, material safety data sheets, and training programs. Employees have the right to know the hazards and identities of the chemicals at their worksite, as well as the appropriate preventive measures to protect themselves. Retail establishments also need to provide appropriate PPE that may be needed to clean pesticide spills, including goggles and chemically protective gloves and clothing. Workers need to be trained on how to use the PPE equipment correctly. Workers handling disinfectants need to be trained in their safe use, and chemical resistant gloves should be available and their use encouraged. Many exposures involved leaking, torn, or ruptured pesticide containers. To prevent similar illnesses, pesticide products should be packaged in non-slip, non-breakable and tear-resistant containers. In addition, integrated pest management (IPM) is an intervention to reduce pesticide usage through utilization of effective and environmentally friendly pest control procedures based on knowledge of pest life cycles and their interaction with the environment.17 Greater adoption of IPM among retail stores and the public can decrease the number of pesticide exposures, thereby reducing the risk of pesticide poisoning among retail employees. As for treatments in and around retail establishments, only trained and qualified workers should handle and apply pesticides, and appropriate safety equipment must be available and should be worn.
Some states have programs to promote pesticide safety in the retail environment and at home. For example, the Pesticide Consultants Registration Rule (357 IAC 1-9) was established in Indiana.18 This rule requires that retail stores with employees who assist customers with pesticide selection and provide use information must ensure that these employees complete pesticide consultant training. Only trained employees are permitted to instruct customers about pesticide labels, safe handling methods, the importance of identifying target pest organisms, and pesticide storage and disposal.18 Improving Kids' Environment, a non-profit advocacy coalition, supported the adoption of these regulations through the Indy Urban Pesticides Initiative,19 and periodically releases reports on retail store compliance.20
Prior research concerning pesticide exposures in retail stores is limited. Maddy and Edmiston collected occupational and non-occupational incidents of illnesses and injuries related to pesticide exposures as reported by California physicians in 1986, and some of these involved retail workers.21 Case selection was based upon death, hospitalization of one or more individuals for more than 24 hours with treatment, or five or more people with symptoms seeking medical care as a result of the same incident. The researchers found a total of four events involving 33 cases resulting from spills in retail establishments. Workers in all four incidents were exposed while cleaning spills without wearing PPE. Pesticides involved were malathion (two events), oxydemeton-methyl and karathane (one event), and acephate and dicofol (one event). We are aware of no other published reports that described pesticide poisoning among retail workers.
There are several limitations present in this analysis. These results should be considered low estimates of the magnitude of the problem because individuals who neither sought medical attention nor contact with a poison control center would likely not be captured in the data. Furthermore, due to the uncommon nature of treating pesticide-related poisonings, health care professionals may not collect a pesticide exposure history, which may result in failure to attribute the illness to pesticide exposure. In addition, some correctly diagnosed cases may not have been reported to public health authorities, despite the fact that 30 states have mandatory reporting of occupationally related pesticide poisoning.8 Another reason that rates may be underestimated is that limited resources preclude some state agencies from tracking all disinfectant cases. Although disinfectants accounted for 43% of all reported cases, three states (Louisiana, New York, and Washington) identified no cases associated with retail disinfectant exposures. The number of customer incidents is also likely to be underestimated. With the exception of Michigan, which tracked only occupational cases, all other states reported both occupational and non-occupational cases. However, many non-occupational cases may have been missed due to limited resources forcing some states to place emphasis on tracking occupational cases and/or limited access to poison control center data, an important source of non-occupational cases. In addition, information was incomplete for some cases. For example, 26% of the occupational cases were missing PPE usage information, and misclassification of severity may be present if all signs or symptoms were not reported. Finally, there may be imprecision in the denominator estimates due to the inherent limitations in the CPS survey design,22 and because the BOC industry and occupation codes used by the Current Population Survey changed in 2003. The change in BOC codes may have caused some retail establishments to be coded into one retail sector before 2003 and into another beginning in 2003.
In conclusion, the findings presented in this analysis emphasize the risk of acute pesticide poisoning among retail workers. Interventions such as implementing educational and training efforts, providing appropriate PPE, adopting unbreakable and tear-resistant container requirements, and utilization of IPM techniques can reduce the incidence of acute pesticide poisoning among retail workers and customers.
Acknowledgments
The authors thank Jia Li, MS, and Marty Petersen, PhD, for their contributions to the statistical analysis, and Walter Alarcon, MD, for his contribution to the methods.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
REFERENCES
- 1.Kiely T, Donaldson D, Grube A. Pesticide industry sales and usage: 2000 and 2001 market estimates. Washington: U.S. EPA; 2004. [Google Scholar]
- 2.Calvert GM, Plate DK, Das R, Rosales R, Shafey O, Thomson C, et al. Acute occupational pesticide-related illness in the U.S., 1998–1999: surveillance findings from the SENSOR-Pesticides program. Am J Ind Med. 2004;45:14–23. doi: 10.1002/ajim.10309. [DOI] [PubMed] [Google Scholar]
- 3.Census Bureau (US) Washington: U.S. Department of Commerce, Bureau of the Census; 1992. 1990 census of population and housing. Alphabetical index of industries and occupations. [Google Scholar]
- 4.Bureau of Labor Statistics (US) Washington: U.S. Department of Labor, Bureau of Labor Statistics; 2004. [cited 2006 Jul 26]. Basic CPS public use file data dictionary. Available from: URL: http://www.bls.census.gov/cps/basic/may04datadic.htm. [Google Scholar]
- 5.Centers for Disease Control and Prevention (US) Cincinnati: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2001. [cited 2006 Jul 26]. Severity index for use in state-based surveillance of acute pesticide-related illness and injury. Available from: URL: http://www.cdc.gov/niosh/topics/pesticides/ [Google Scholar]
- 6.Environmental Protection Agency (US) Washington: EPA; 1975. [cited 2006 Jul 26]. General provisions. Labeling requirements. Available from: URL: http://a275.g.akamaitech.net/7/257/2422/14mar20010800/edocket.access.gpo.gov/cfr_2002/julqtr/pdf/40cfr156.10.pdf. 40CFR156.10(h) [Google Scholar]
- 7.Barnett M, Calvert GM. Cincinnati: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2005. [cited 2006 Jul 26]. Pesticide-related illness and injury surveillance: a how-to guide for state based programs. DHHS (NIOSH) Publication No:2006-102. Available from: URL: http://www.cdc.gov/niosh/docs/2006-102/pdfs/2006-102r.pdf. [Google Scholar]
- 8.Calvert GM, Sanderson WT, Barnett M, Blondell JM, Mehler LN. Surveillance of pesticide-related illness and injury in humans. In: Krieger RI, editor. Handbook of pesticide toxicology. 2nd edition. San Diego: Academic Press; 2001. pp. 603–41. [Google Scholar]
- 9.SAS Institute. Inc. SAS: version 9.1 for Windows. Cary (NC): SAS Institute, Inc; 2003. [Google Scholar]
- 10.Bureau of Labor Statistics (US) Washington: U.S. Department of Labor, Bureau of Labor Statistics; 2004. Current population survey 1998–2002 microdata files. [Google Scholar]
- 11.Rothman KJ. Boston: Little, Brown; 1986. Modern epidemiology; pp. 164–72. [Google Scholar]
- 12.Agency for Toxic Substances and Disease Registry. Atlanta: U.S. Department of Health and Human Services, Public Health Service; 1994. Toxicological profile for chlordane (update) [Google Scholar]
- 13.Environmental Protection Agency (US) Washington: EPA; 2004a. [cited 2006 Jul 26]. Food Quality Protection Act (FQPA) Available from: URL: http://www.epa.gov/pesticides/regulating/laws/fqpa/ [Google Scholar]
- 14.Environmental Protection Agency (US) Washington: EPA; 2005. [cited 2006 Jul 26]. Pesticide reregistration status. (update). Available from: URL: http://www.epa.gov/pesticides/reregistration/status.htm. [Google Scholar]
- 15.Environmental Protection Agency (US) Washington: EPA; 2000. [cited 2006 Jul 26]. Chlorpyrifos revised risk assessment and agreement with registrants. Available from: URL: http://www.epa.gov/pesticides/op/chlorpyrifos/agreement.pdf. [Google Scholar]
- 16.Occupational Safety and Health Administration (US) Washington: OSHA; 1994. [cited 2006 Jul 26]. Hazard communication. 29 CFR 1910.1200. Available from: URL: http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10099. [Google Scholar]
- 17.Environmental Protection Agency (US) Washington: EPA; 2004b. [cited 2006 Jul26]. Integrated pest management (IPM) and food production. Available from: URL: http://www.epa.gov/pesticides/factsheets/ipm.htm. [Google Scholar]
- 18.Office of Indiana State Chemist (OISC) Consultant rule requirements – procedures, 2000. [cited 2006 Jul 26]. Available from: URL: http://www.isco.purdue.edu/pesticide/consultant_rules.html.
- 19.Improving Kid's Environment (IKE) Update on children's environmental health issues in Indiana. Improving Kid's Environment Newsletter. 2002. Dec, [cited 2006 Jul 26]. Available from: URL: http://www.ikecoalition.org/IKE_Newsletter/IKE_12-02_newsletter.htm.
- 20.Improving Kid's Environment (IKE) Your kid's health: can you trust the advice from retail stores selling paint and pesticides. IKE 2005 retail store survey. 2005. [cited 2006 Jul 26?]. Available from: URL: http://www.ikecoalition.org/Stores/2005_Survey.htm.
- 21.Maddy KT, Edmiston S. Selected incidents of illnesses and injuries related to exposure to pesticides reported by physicians in California in 1986. Vet Hum Toxicol. 1988;30:246–54. [PubMed] [Google Scholar]
- 22.Bureau of Labor Statistics (US) Technical paper 63RV. Washington: U.S. Department of Labor, Bureau of Labor Statistics; 2002. [cited 2006 Jul 26]. Current population survey design and methodology. Available from: URL: http://www.census.gov/prod/2002pubs/tp63rv.pdf. [Google Scholar]