Diabetes mellitus (type 2 diabetes, T2D) is one of the main threats to human health in this century.1 The drastic increase in incidence of diabetes worldwide has been attributed to distinct changes in human behavior and lifestyle during the last century, conditions collectively termed as the “metabolic syndrome.”2 Parallel with globalization, pronounced changes in the human environment and in human behavior and lifestyle have resulted in escalating rates of both obesity and diabetes.3 Diabetes mellitus today also means a significantly reduced life expectancy,4 reduced quality of life for the patient, and a significant burden for society due to increased health care cost.5 A recent large meta-analysis of population-based data shows that more than half of the European and probably the same or an even higher proportion of the Asian population will suffer from hyperglycaemia during their lifetime.6 Furthermore, diabetes and impairment of glucose tolerance are appearing increasingly in younger people, with a most sudden increase in the age group younger than 30 years.7 Unfortunately, people with diabetes are diagnosed in the professional medical system too late, often with a diagnose-free interval up to 15 years.8,9 This interval is the major metabolic burden for the disease, because during this time vascular and cellular lesions are set which will lead decades later to the severe disease-associated complications.10
The most efficient way to manage T2D is to prevent diabetes from developing. Also, complications of T2D can best be postponed by delaying the onset of the primary disease itself. The efforts to prevent the disease need to start as early as possible and address all susceptibility factors.11 Fortunately, recent studies have convincingly demonstrated that prevention of T2D is possible12–15 by showing that lifestyle intervention addressing diet and exercise reduces the risk of progressing from impaired glucose tolerance (IGT) to diabetes by 47% and 58%, respectively. Furthermore, it was shown that the drugs metformin,12 acarbose,14 and orlistat16 significantly decreased the progression from impaired glucose tolerance to diabetes.
While these findings offer the evidence base for the development of community-based prevention strategies,17 it is necessary to develop and implement prevention programs into clinical practice, considering scientific aspects and practical requirements during implementation.18 The study interventions followed a very intensive intervention program. There is a good chance that less intensive lifestyle programs are also effective in changing lifestyle.19 In this article, we present a diabetes prevention management concept which can be implemented in clinical practice.
DESIGN
In 2003, an expert team from the German Ministry of Health with representatives from different professions defined health-related aims for diabetes prevention.20 This workgroup extracted the essential intervention strategies from known prevention studies and focused on establishing management aims for primary diabetes prevention in response to the large social and economic burden caused by the late diagnosis of the disease. It also was based on the fact that the secondary and tertiary prevention of diabetes are already mostly covered by diagnostic and treatment regulations. As a result, the workgroup composed three diabetes-related health aims:
Individuals with increased diabetes risk are found before disease onset;
Individuals at risk for diabetes are getting an intervention to prevent diabetes; and
These individuals will not develop diabetes or, if they do develop the disease, it is detected early and treated with adequate therapy (secondary prevention).
To achieve these goals it is necessary to answer the following questions: (1) Who is at risk for diabetes? (2) How do people at risk receive the necessary information and motivation to change their lifestyle, and what intervention is the best one? (3) What is the best way to maintain lifestyle changes over a long time?
The prevention studies known today12–15 were performed with different study designs, intervention procedures, and different observation times; also, the initial hypothesis followed different hypothetical action models. The objective in the TUMAINI concept was to also include normoglycaemic individuals who are at risk to develop diabetes and not only people with impaired glucose tolerance/impaired fasting glucose (IGT/IFG). (TUMAINI is the Swahili word for “hope”—it is our hope to prevent diabetes.) We defined a model of action as a program that over time achieves a proportional slower diabetes incidence increase with the intervention, with the metabolic changes maintained after discontinuation of the intervention.21 In addition, the management concept should be accessible on a national level, reaching people at risk for diabetes in the general population with acceptable effort. Furthermore, it was necessary to take into consideration the reimbursement system in Germany and issues of professionalism—to decide who is the professional to carry out the lifestyle intervention.21
RESULTS AND DISCUSSION
Program concept for diabetes prevention
For the implementation of a prevention management program it is necessary to find a way to translate the intervention of the prevention studies into general health care. It is also important to establish a management concept that achieves similar efficiency in lifestyle changes as the mentioned studies, while being practical to manage a large number of participants. Knowing these challenges, the TUMAINI-Diabetes Prevention management concept was developed consisting of a three-step intervention:
Identification of the individuals at high risk to develop type 2 diabetes;
Intensive intervention based on individual choice;
Continuous intervention for motivation maintenance and evaluation.
The prevention management program is based on group interventions. The intention is to motivate the person at risk to self-manage the diabetes risk and the lifestyle changes with assistance.
1. Identification of the individuals at high risk to develop diabetes.
Strategies to identify individuals at high risk for type 2 diabetes were controversial issues in the past.22 The identification of subjects who meet inclusion criteria for the larger prevention studies consumes large scale resources and is difficult to realize for a large number of people. Our aim for including individuals with elevated diabetes risk—not just those with IGT/IFG—made it necessary to use a test that identifies individuals at risk for the disease. An efficient test should also recognize individuals having a predictive diabetes risk with a good ratio between specificity and sensitivity, should be simple to handle, transparent to both sides (physician and the affected person), widely accessible, and basically cost-free. Furthermore, the test should intend to empower the individual as feeling “at risk” and not “being sick”.
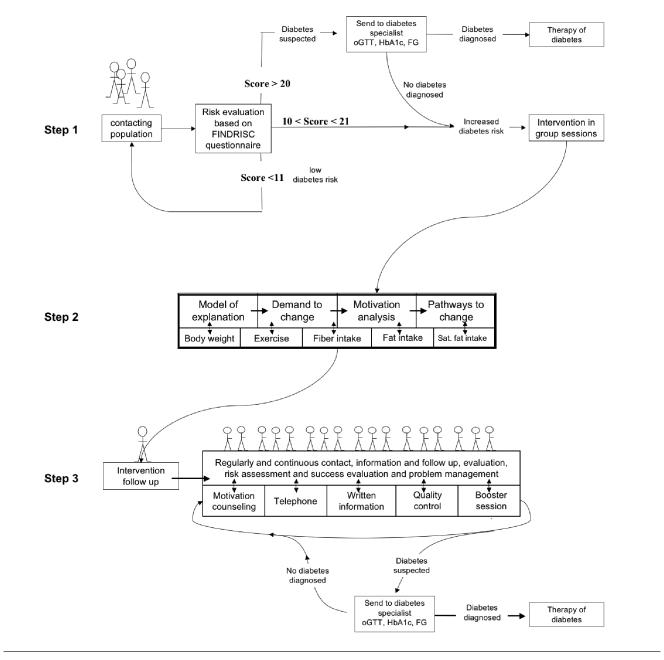
The FINDRISC questionnaire was chosen23 as the first step of the TUMAINI prevention management program to estimate the individual 10-year risk of T2D (Figure 1). This questionnaire is comprised of eight validated items23 and is available via the Internet, information material from the health care and social institution, occupational health care, and public health. People are asked to fill out the questions whenever they have time and interest. At the end of the questionnaire, a local telephone or internet address is available for contacting a prevention manager. The answers of the FINDRISC questionnaire add up to a maximum score of 26 points. Individuals with a low score (below 11) will receive written information about healthy diet and exercise benefits. Those with a high FINDRISC score (11 points or higher) will be offered an opportunity to participate in the intervention program performed in group sessions. Individuals with a very high score (20 and higher) have a high chance of suffering from undiagnosed diabetes. It is suggested that they visit a medical doctor for diabetes diagnosis or exclusion. If diabetes is excluded, these people can participate in the intervention program.
Figure 1.
Steps 1–3 of the TUMAINI prevention management concept
2. Intensive intervention.
People identified with a FINDRISC Score of 11 points or higher and (and no diabetes, if tested) are included in an intensive lifestyle reinforcement program that focuses on empowerment of the participants to change their lifestyle (Figure 1). This program step is time-limited and consists of eight hours of group visits attempting to motivate people at high risk to adopt healthy lifestyles by delivering information about healthy diet and physical activity. Training topics are empowerment and the five core prevention goals learned from the Finnish Diabetes Prevention Study.13 The objectives are to achieve better understanding of the disease risk, and to analyze and build the motivation needed for a commitment to change lifestyle. This protocol is focused on the principle of a self-management intention. In the course, a model of disease risk is developed, the need to change is analyzed, and a motivation analysis is performed. The clients leave the course with individual pathways identified to change their lifestyle. The concept of the disease risk in general and the individual risk in particular form the basis for the demand to change lifestyle.
3. Continuous intervention period for motivation maintenance.
Several investigations in the past have shown that time-limited interventions to change lifestyle fail to reach a continuous lifestyle change. It is typically human to be activated and motivated for a short period of time, but fail to maintain, even with a high personal involvement.21 Establishing a long-term motivation to maintain lifestyle changes to prevent diabetes is the core part of the TUMAINI concept (Figure 1). Therefore, after the initial training step a bundle of regular contact interventions will be established to strengthen the motivation of the participants, including:
A written “newsletter” including repetition of core questions for lifestyle intervention, practical tips addressing physical inactivity and dietary changes, food recipes, and personal self reports from clients (sent every three months).
Telephone hotline with 24-hour assistance.
Active telephone counselling: the participant will be called at regular three-month intervals for problem management and support and to boost motivation.
Continuous multimedia support including web sites and a regular interactive e-mail newsletter.
Optional booster session for those with compliance problems or no successful intervention.
Regular quality control including six monthly measurements of blood pressure and waist circumference as self-reports, followed by a contact for personal feedback.
A contact is made every four to six weeks at a minimum. For subjects with no multimedia access, this contact will be replaced by telephone contact and written information.
The goal is that the telephone contact and face-to-face contact will be performed by the same person who did the initial training (prevention manager, see below) because this person knows the individual situation of the client and can counsel on individual characteristics. The regular personal contact focuses mainly on motivation and problem management; the nonpersonal contact focuses on motivation and information to maintain the motivation for preventive lifestyle changes. The results of the individual risk evaluation and the response to the intervention are given back for personal feedback to stimulate the lifestyle modification. Individuals with no response are eligible for booster intervention.
Professional responsibility
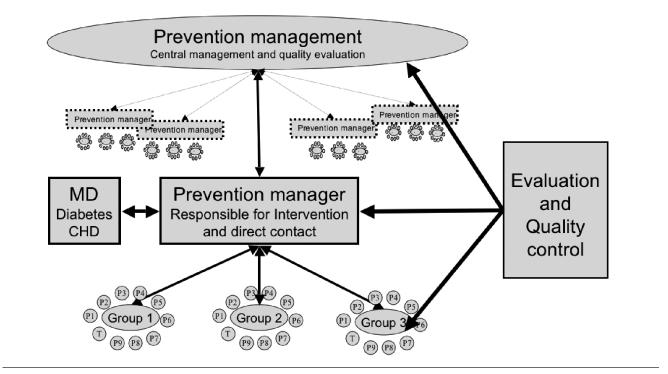
Another key question in the implementation of a nationwide prevention program of type 2 diabetes is: Who should deliver the intervention? Addressing risk factors for a disease such as insulin resistance and obesity is a medical responsibility, but addressing physical inactivity and dietary changes in people who are still “healthy” is not primarily a physician's responsibility.21 Furthermore, even motivated physicians typically have limited experience in training for lifestyle intervention, and often have inadequate access to the resources needed to support lifestyle intervention. Therefore, primary prevention of type 2 diabetes raises several issues related to the integration of lifestyle intervention in clinical or preclinical practice. Luckily, in most countries providers for exercise, nutritional, and motivational counselling exist with high professional standards.19 They can be used to deliver the intervention after a short additional training if adequate quality control and evaluation is established. These professionals are currently established as “prevention managers” and work as providers and coordinators of the intervention.21 The prevention managers can be recruited from existing health care providers including psychologists, dieticians, diabetes educators, physical trainers, physiotherapists, and individuals attending additional training to become a prevention manager if they accept a continuous quality control and evaluation of their work. The advantage is that an existing infrastructure can be used to spread the intervention. This structure is based on a preclinical intervention program together with a supervising role of physicians in the intervention.21 The classic professional responsibility of a physician is the diagnosis of a potential disease and its treatment. Following this concept, the physician is working as a supervising partner of the prevention manager if a professional diagnosis (diabetes, heart disease) is needed. A physician can also become a prevention manager, but this will probably be limited to a small number of highly motivated physicians. The prevention manager will be a new category of health interventionist to deliver and manage long-term lifestyle intervention in the large number of individuals who would be eligible for these services.19 A central institution for prevention management should manage the program and organize the quality control (Figure 2).
Figure 2.
Decentralized implementation model of a national prevention management program
Quality control
The key factors in performing high quality intervention are continuous evaluation and quality control.24 The partners in the prevention management program have a different motivation to deliver or get high quality intervention. The individuals participating in the program want to attend centers where the intervention is of high quality. The prevention manager wants to get information about the individual success of those participating in his center for internal quality control and wants to show a high quality intervention delivery. Both partners are interested in the long-term success of the intervention. Therefore, the long-term measurement of blood pressure and waist circumference are chosen for quality control and a centralized independent evaluation and quality control is established.
Prevention of diabetes and the metabolic syndrome means reduction of metabolic risk factors such as high blood pressure and large waist circumference. In the TUMAINI prevention management plan, these two parameters are measured every six months. Both parameters can give a good evaluation of the risk and lifestyle changes.25 Based on self-reports with random control, this is a low cost strategy for intervention quality control. The data are collected and transferred to a central evaluation center and returned to the participant and the prevention manager for personal feedback and evaluation. With the exception of the evaluating institution, no other infrastructure is needed.
The advantages of quality control based on the intervention effect will be that an individual success evaluation is possible for the participant so that nonresponders who are then eligible for a booster intervention can be identified early. Furthermore, different institutions that provide different lifestyle programs can be compared based on their quality scores, which will lead to a client shift to more quality-oriented centers and, finally, equalization of intervention quality. Representatives from several different professions may become prevention manager if they sign up for evaluation.
CONCLUSION
The only way to reduce the personal and socioeconomic burden of diabetes and its associated complications is the prevention of diabetes. The scientific evidence is compelling supporting primary prevention of diabetes by lifestyle intervention and translations of the study strategies into national prevention programs. The implementation of diabetes prevention programs will require an integrated, international approach if we are to see significant reduction in the premature morbidity and mortality it causes. We must accept that diabetes risk is not a disease; it is a symptom of a much larger problem—the adaptation of our metabolism to sedentary globalization. Diabetes is likely to remain a huge threat to public health in the years to come; affordable strategies and quality controlled programs are needed for primary prevention. The presented TUMAINI concept is a management strategy for a primary diabetes prevention program on a national level. The health intervention may not be limited to diabetes alone, but will have the potential to prevent a great number of health conditions such as cardiovascular disease, certain cancer types, and osteoporosis. Integration of lifestyle intervention into current health care systems will require a simple network of prevention managers and physicians to provide effective programs of lifestyle intervention and to implement quality controlled prevention strategies. An urgent priority is, therefore, to establish guidelines for the prevention of type 2 diabetes, including lifestyle and pharmaco-prevention. Implementing a structured prevention management program will enable implementation of diabetes prevention in clinical practice.
REFERENCES
- 1.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–7. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 2.Alberti KG. Type 2 diabetes: questions of prevention Diabetes Voice; Bulletin of the International Diabetes Federation. 2002;47(4):5. [Google Scholar]
- 3.Zimmet P, Shaw J, Alberti KG. Preventing type 2 diabetes and the dysmetabolic syndrome in the real world: a realistic view. Diabet Med. 2003;20:693–702. doi: 10.1046/j.1464-5491.2003.01052.x. [DOI] [PubMed] [Google Scholar]
- 4.Haffner SM. Can reducing peaks prevent type 2 diabetes: implication from recent diabetes prevention trials. Int J Clin Pract. 2002;129(Suppl):33–9. [PubMed] [Google Scholar]
- 5.Liebl A, Goertz A, Henkel B, Spannheimer A. [Costly type 2 diabetes mellitus Does diabetes cost 20 billion per year?] MMW Fortschr Med. 2000;142(23):39–42. [PubMed] [Google Scholar]
- 6.Valensi P, Schwarz EH, Hall M, Felton AM, Maldonato A, Mathieu C. Pre-diabetes essential action: a European perspective. Diabetes Metab. 2005;31:606–20. doi: 10.1016/s1262-3636(07)70239-2. [DOI] [PubMed] [Google Scholar]
- 7.Nestle M. Preventing childhood diabetes: the need for public health intervention. Am J Public Health. 2005;95:1497–9. doi: 10.2105/AJPH.2005.069120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Prevention of diabetes mellitus: report of a WHO Study Group. WHO Technical Report Series. 1994 WHO Technical Report Series 844(ISBN 9241208449) [PubMed] [Google Scholar]
- 10.Hiltunen LA. Does glucose tolerance affect elderly persons' balance, gait or muscle strength? Cent Eur J Public Health. 2001;9:22–5. [PubMed] [Google Scholar]
- 11.Mayor S. Government publishes strategy to improve diabetes care. BMJ. 2003;326:121. doi: 10.1136/bmj.326.7381.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 14.STOP-NIDDM Trial Research Group. Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359:2072–7. doi: 10.1016/S0140-6736(02)08905-5. [DOI] [PubMed] [Google Scholar]
- 15.Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–44. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 16.Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–61. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- 17.Watts G. Huge numbers must change lifestyle to prevent epidemic of diabetes. BMJ. 2003;327:1365. doi: 10.1136/bmj.327.7428.1365-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Narayan KM, Bowman BA, Engelgau ME. Prevention of type 2 diabetes. BMJ. 2001;323:63–4. doi: 10.1136/bmj.323.7304.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sartorelli DS, Sciarra EC, Franco LJ, Cardoso MA. Primary prevention of type 2 diabetes through nutritional counseling. Diabetes Care. 2004;27:3019. doi: 10.2337/diacare.27.12.3019. [DOI] [PubMed] [Google Scholar]
- 20.Weber I, Brenner G, Schwarz P, Schulze J. Mehr Evidenz - breitere Akzeptanz - erhöhte Chancen auf Umsetzung einer Maβnahme zur Prävention des Typ 2-Diabetes in Deutschland gesundheitsziele.de Berlin: Gesellschaft för Versicherungswissenschaft und-gestaltung e. V., 2005:239–245. [Google Scholar]
- 21.Schwarz P, Schwarz J, Bornstein S, Schulze J. Prevention of type 2 diabetes: what challenges do we have to address. [cited 2006 Dec 21];J Public Health. 2005 2:296–303. Available from: URL: http://www.springerlink.com/content/y8r0453ku55r2800/?p=14d5e26746fa4e1c892616f8e9e7ca87&pi=1. [Google Scholar]
- 22.Schwarz P. [Targeted diabetes prevention in high risk groups: pro] Dtsch Med Wochenschr. 2005;130:1103. doi: 10.1055/s-2005-866795. [DOI] [PubMed] [Google Scholar]
- 23.Lindstrom J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26:725–31. doi: 10.2337/diacare.26.3.725. [DOI] [PubMed] [Google Scholar]
- 24.Roubideaux Y, Buchwald D, Beals J, Middlebrook D, Manson S, Muneta B, et al. Measuring the quality of diabetes care for older American Indians and Alaska natives. Am J Public Health. 2004;94:60–5. doi: 10.2105/ajph.94.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schulze J, Rothe U, Muller G, Kunath H. [Improvement of care for diabetics using the care model from Saxony] Dtsch Med Wochenschr. 2003;128:1161–6. doi: 10.1055/s-2003-39353. [DOI] [PubMed] [Google Scholar]