Carbon monoxide is a common, potentially lethal gas produced by the incomplete combustion of fossil fuels such as natural or liquefied petroleum gas, oil, wood, and coal. It is one of the oldest documented toxicants. Mortality and morbidity from acute, unintentional, non-fire-related carbon monoxide poisoning is a substantial, but often unrecognized, public health problem in the United States. (Intentional and fire-related carbon monoxide poisoning have other public health pathways for surveillance, prevention, and control; these events are, therefore, not addressed in this article.) It is estimated that each year in the United States at least 15,200 individuals seek medical attention in an emergency department or miss at least one day of work due to carbon monoxide poisoning.1 However, this estimate does not account for the full burden of illness; the toxic effects of carbon monoxide exposure are nonspecific and easily misdiagnosed. Symptoms may include headache, dizziness and nausea, and—at higher levels of exposure—disorientation, unconsciousness, and death. The estimate also does not account for those directly admitted to a hospital, those presenting to other types of outpatient clinics, who call poison control centers, who do not seek care, or those who die immediately from carbon monoxide exposure and receive no medical care.
Carbon monoxide poisoning occurs both as the result of routine domestic, occupational, and recreational activities, and in the wake of large-scale disasters such as those caused by hurricanes,2,3 floods,4 and winter storms.5,6 It is almost entirely preventable by the correct installation, maintenance, and operation of devices that may emit carbon monoxide, combined with the appropriate use of carbon monoxide detectors (also called carbon monoxide alarms). It has been estimated that carbon monoxide detectors could prevent at least half of all deaths attributable to nondisaster-related carbon monoxide poisoning.7 In 2004, six states (Alaska, Delaware, Florida, Maine, Mississippi, and Montana) included a question about the presence of a carbon monoxide detector in homes on their Behavioral Risk Factor Surveillance System (BRFSS) questionnaires. (The BRFSS is an ongoing random telephone survey of adult, noninstitutionalized state residents conducted by the 50 state health departments as well as those in the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands with support from the U.S. Centers for Disease Control and Prevention [CDC].) The household prevalence of detectors ranged from 19.6% in Florida (Personal communication, Melissa R. Murray, MS, BRFSS Florida Behavioral Risk Factor Surveillance System, Florida Department of Health, January 6, 2006) to 53.0% in Alaska (Personal communication, Rebecca S. Wells, SM, Health Survey Lab Manager, Alaska Department of Health and Social Services, December 2, 2005), dramatically lower than the prevalence of smoke alarms in homes; the 1995 BRFSS estimated that 94% of homes in the United States had at least one smoke alarm.8 While mortality related to carbon monoxide poisoning appears to have declined over the past two decades,9,10 the incidence of carbon monoxide poisoning as measured by related calls to poison control centers and treatment with hyperbaric oxygen appears to have remained stable from 1992 to 2002.11
THE CASE FOR PUBLIC HEATH SURVEILLANCE OF CARBON MONOXIDE POISONING
Surveillance for carbon monoxide poisoning is needed to support public health prevention and intervention activities. The need for nationwide surveillance is recognized in the Healthy People 2010 goal for the United States of “increasing the number of Territories, Tribes, and States, and the District of Columbia that monitor carbon monoxide poisoning from 7 to 51.”12 Currently, carbon monoxide poisoning is reportable in 15 states or territories.13 One-time reports of morbidity and mortality have been published at the state14–17 and national1,9–11 levels, but few describe ongoing public health surveillance of carbon monoxide.
Public health surveillance systems are established and conducted using a case-based and/or rate-based approach;18 either of these methods may lay the basis for public health intervention. Case-based surveillance is a system where information is brought in initially by case reports. Data may be entered and analyzed on an ongoing basis, often within hours or days of the case occurrence. Case reports that are received may need follow-back to obtain more complete information. When such investigations are conducted, this constitutes a “gold standard” for surveillance. Follow-back is resource intensive, however, so the number of case investigations selected is often limited. Cases are typically selected for follow-back based on predetermined criteria that identify cases where further public health action may be warranted. For a case-based carbon monoxide surveillance system, such criteria might include investigating cases where there is the possibility of ongoing exposure, that exceed a predefined carboxyhemoglobin level, and/or that may point to a novel source of hazard. Investigation may also lead to the identification of other environmental hazards, including housing disrepair, poor ventilation, and other events that may lead to adverse health outcomes. Investigating a subset of cases based on predetermined criteria, however, may result in assessing cases with the highest level of acute exposure; investigators may therefore miss important prevention opportunities and lessons from other exposure scenarios.
Rate-based surveillance involves aggregating data and normalizing them across populations and/or time; data are often collected for other purposes, such as hospital discharge and mortality data. Rate-based systems have the benefit of being less resource intensive than the case-based approach; the principal disadvantages are the lag between case occurrence and data evaluation and the absence of detailed case information that constitutes the gold standard for surveillance.
A case- or rate-based surveillance system for carbon monoxide could be used to:
Measure and track the burden of carbon monoxide poisoning over time;
Identify high-risk groups and modifiable factors, including describing demographic and regional variation;
Examine the epidemiology of the occurrence of carbon monoxide poisoning during a disaster and at other times;
Understand the relative contribution of exposure sources (motor vehicles, furnaces, gas-powered appliances) to the burden of carbon monoxide poisoning, as well as describe the settings in which exposures occur (occupational, residential, or recreational); and,
Guide the planning and evaluating of public health prevention and control interventions.
Surveillance for carbon monoxide poisoning is also needed to support research to address some of the unresolved public health issues about carbon monoxide poisoning. One such issue is the long-term sequelea of carbon monoxide poisoning; although a significant proportion of survivors of acute carbon monoxide poisoning may have persistent serious neurological injury,19 little is known about its prevalence or associated risk factors. Additionally, chronic high and moderate levels of exposures to carbon monoxide have been associated with excess cardiovascular disease (CVD)-related mortality,20 but the effects of chronic low level exposures, particularly in regard to occupational settings, are less well understood. A surveillance system could support research into these important questions by providing information with which to generate hypotheses as well as by providing the basis to establish exposure registries.
THE NEED TO ESTABLISH ENVIRONMENTAL PUBLIC HEALTH SURVEILLANCE OF CARBON MONOXIDE
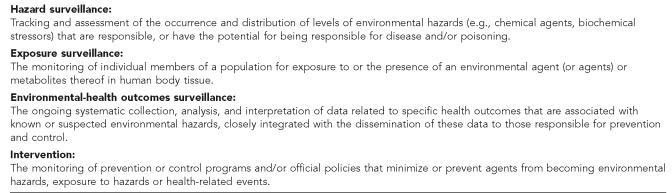
To be most useful for developing interventions for the prevention of carbon monoxide poisoning, surveillance for carbon monoxide should go beyond collecting information on the health outcomes. An ideal environmental public health surveillance system captures, characterizes, and disseminates information on a population's status in regard to the environmental hazard, exposure, health effects, and interventions in addition to health effects (see Figure 1).21 This comprehensive model, being promoted by the CDC's Environmental Public Health Tracking Program (EPHTP), among others, aims to provide the specificity of surveillance data required for designing interventions that can be focused on the appropriate hazards and populations. By tracking hazard, exposure, and intervention information in addition to health effects, carbon monoxide surveillance systems may yield data that make the case for the installation of carbon monoxide detectors, improvements in the installation, operation, and maintenance of gas furnaces and generators, or for outreach to medical care providers or specific population groups.
Figure 1.
Definitions for the components of an environmental public health surveillance system
SOURCE: Thacker SB, Stroup DF, Parrish RG, Anderson HA. Surveillance in environmental public health: issues, systems, and sources. Am J Public Health 1996;86:633-8.
There are a number of available data sources that may prove useful for hazard surveillance of carbon monoxide in ambient air. Carbon monoxide emissions data that are available from the U.S. Environmental Protection Agency (EPA) National Emission Inventory database and concentrations from air monitoring station data that are available from the EPA Air Quality System database are readily available. There is a growing body of literature that shows an ecological association between increased levels of ambient air carbon monoxide and adverse CVD,22,23 stroke,24 and birth outcomes25,26 that supports the need to investigate long-term effects of chronic low dose exposures. Few areas in the United States, however, do not attain federal ambient air standards for carbon monoxide levels.27 Two sources of potential hazard data on carbon monoxide levels in indoor environments, currently largely untapped, are data obtained by utility companies and fire departments. Utility companies are required, in most states, to take and investigate calls about potential gas leaks in homes, communities, and workplaces, and they frequently conduct environmental sampling for carbon monoxide. Fire departments respond to similar calls as well as to carbon monoxide detector alarms and also take carbon monoxide measurements. While these data may represent a rich source of hazard information, their availability is often limited by the absence of electronic data systems and/or the willingness of the data owners to share information with health departments. Hazard surveillance can also be conducted on known risk factors for carbon monoxide exposures. For example, population-based surveys of housing and housing conditions may identify geographic areas and demographic characteristics of residents experiencing heating and electricity loss and who are dependent upon supplemental heating sources.28,29
Exposure surveillance for carbon monoxide can be conducted using data from laboratory tests for elevated carboxyhemoglobin in blood, often conducted in emergency rooms and hospitals. The development and recent U.S. Federal Drug Administration approval of a pulse-oximeter,30 allowing for rapid noninvasive measurement of carboxyhemoglobin, may facilitate more timely exposure monitoring and may therefore increase the availability and the accuracy of these data. This tracking could parallel the use of electronic laboratory reporting infrastructure for lead exposure test results. Such surveillance could be conducted using electronic laboratory reporting infrastructure established by the Public Health Information Network–National Electronic Disease Surveillance System (PHIN–NEDSS). Another source of these data may be poison control centers, which may receive physician reports following confirmed exposures.
Multiple data sources exist for conducting rate-based health outcome surveillance of carbon monoxide poisoning. Data available in all or most states and territories include: hospital discharge data, available in 90% of states; emergency department data, available in 50% of states;31 mortality data; poison control center call data; and the Behavioral Risk Factor Surveillance System. In many jurisdictions, case-based surveillance requires a legislative or regulatory mandate designating carbon monoxide poisoning as a reportable condition. Once so designated, surveillance systems for carbon monoxide poisoning can be designed to identify and collect information on cases based on those processes established for other reportable conditions that are detected through reports from medical care providers, laboratories, and hospitals. Patient identification should also be conducted with facilities that house and operate hyperbaric chambers.
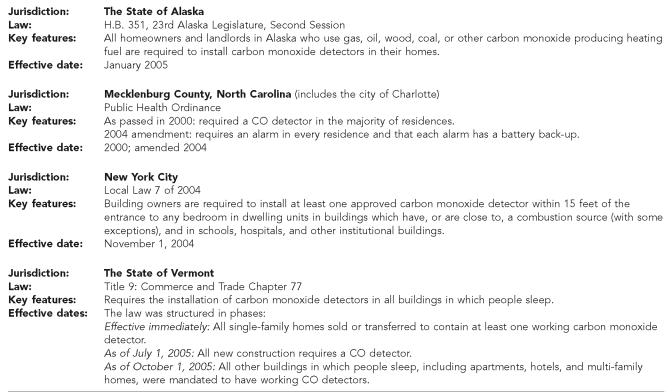
Surveillance on the delivery and effects of interventions can be conducted using surveys such as the BRFSS to assess the prevalence of carbon monoxide detectors in homes, or can be based upon the evaluation of state and local programs or policies to reduce carbon monoxide exposure, such as legislation mandating carbon monoxide detectors in residential settings (see Figure 2).
Figure 2.
Highlights of selected state and local legislative mandates requiring the use of carbon monoxide detectors
Establishing a fully integrated environmental public health surveillance system for carbon monoxide will offer the potential for linking health effects, exposure, and hazard information. These linkages could be used to explore the adverse effects of both indoor and outdoor air quality. Such projects could investigate: the impact of the volume of portable generator sales and the frequency of carbon monoxide poisoning in the context of decreasing generator prices, and increasing promotion of ownership/use as part of emergency preparedness; the effectiveness of marketing strategies data (for example, the co-sale of outdoor extension cords) for prevention, by linking health outcome data with marketing data; or linkage of carbon monoxide poisoning health outcome data with housing data to understand the role of housing age and condition.
THE NEED TO ESTABLISH A NATIONAL SYSTEM FOR ENVIRONMENTAL PUBLIC HEALTH SURVEILLANCE OF CARBON MONOXIDE IN THE UNITED STATES
A coordinated national approach to developing carbon monoxide surveillance is needed. Environmental public health surveillance systems should be sustainable, built on evidence-based standards, and able to collect and integrate scientifically valid data on environmental hazards, exposures, related health outcomes, and interventions. A system that is coordinated nationally would provide the basis to develop and apply these standards as well as the resources, expertise, and the incentive to conduct surveillance. Such a surveillance system, comprised of a central repository of either raw or aggregated data, could bring together state and local data to better evaluate state, regional, urban/rural, and other geographic and demographic variability in carbon monoxide-related hazards, exposures, and health outcomes. Currently, there is neither a national approach nor a national system.
The lack of a coherent nationwide system to track carbon monoxide poisoning has contributed to gaps in local, state, and national capacity to conduct and evaluate public health practice activities for the prevention of carbon monoxide poisoning. National promotion and coordination of developing state and local carbon monoxide surveillance systems would enhance capacity in the basic public health function of building and maintaining surveillance systems; increase staff knowledge about the occurrence, sources, and prevention of carbon monoxide poisoning; support related ongoing public health efforts such as the BRFSS; and potentially increase technical capacity to develop an integrated environmental public health surveillance system.
Other benefits of increasing public health capacity to conduct surveillance for carbon monoxide include: improving environmental public health preparedness for emergency response, improving the ability to plan and evaluate prevention programs, advancing environmental public health science and research, and fostering collaboration among health and environmental programs.
Improving public health preparedness and emergency response
There is a growing recognition of the need to develop systems to begin carbon monoxide surveillance in the wake of large scale disasters, where the use of alternative fuel and cooking sources can lead to carbon monoxide-related morbidity and mortality. Recent experience with the post-hurricane Katrina and Rita public health responses demonstrated the need to use novel data sources and data collection techniques.2 Protocols need to be developed for putting these systems in place in the absence of a pre-existing system, or to quickly and seamlessly transition from an existing system for routine surveillance (whether passive or active) to conducting active surveillance in the wake of large scale power outages and/or disasters. In addition, a national system would provide a platform for planning and coordinating action with other public health responses.
Improving capacity to plan and evaluate prevention actions
A number of jurisdictions have mandated the placement of carbon monoxide detectors (Figure 2); some have conducted one-time evaluations of these laws. For example, in 2000, the county of Mecklenburg, North Carolina (which includes the city of Charlotte), adopted a public health ordinance requiring a carbon monoxide detector in the majority of residences; an evaluation of the effectiveness of the ordinance was conducted following an ice storm that caused 78.9% of houses in the county to be without electricity. The investigation found that 96% of the severe cases of carbon monoxide poisoning occurred in homes without a functioning carbon monoxide detector. As a result of the evaluation, the ordinance was amended to require an alarm in every residence, and that each alarm has a battery backup.32 Surveillance systems would provide the data that are needed to monitor and to evaluate the ongoing effectiveness of such legislative mandates.
Fostering collaboration among health and environmental programs
Public health agencies conducting carbon monoxide surveillance could provide a forum to bring diverse stakeholders together in order to coordinate prevention activities as well as share experiences and lessons learned. Efforts are underway in such diverse jurisdictions as Maine, Washington, Wisconsin, and the City of New York to bring together a variety of interested parties including public and not-for-profit injury prevention programs, emergency room clinicians, first-responders such as emergency medical services and firefighters, the Consumer Product Safety Commission, academicians, poison control centers, and citizen groups to evaluate data and coordinate prevention activities.
PROGRESS TOWARD COORDINATION OF A NATIONWIDE CARBON MONOXIDE SURVEILLANCE SYSTEM
CDC has recently designated a home for carbon monoxide surveillance in their National Center for Environmental Health, Division of Environmental Hazards and Health Effects (DEHHE). Recognizing that carbon monoxide poisoning crosses many public health jurisdictions other than environmental health, including injury, occupational health, and emergency response, DEHHE has begun coordinating carbon monoxide surveillance efforts with many partners. There is also ongoing coordination among the programs within DEHHE that work most closely with carbon monoxide surveillance, the Air Pollution and Respiratory Health and EPHTP. These programs are collaborating with several state and local health departments participating in a National Workgroup for Carbon Monoxide Surveillance. The workgroup's goals include developing national standards for carbon monoxide poisoning surveillance; they have undertaken an assessment of the usefulness of two disparate case definitions for public health surveillance of carbon monoxide poisoning (Personal communication, Allison Stock, PhD, Epidemiologist, Centers for Disease Control and Prevention, National Center for Environmental Health, Environmental Hazards and Health Effects, Air Pollution and Respiratory Effects Branch, March 15, 2006)—the definition adopted by the Council of State and Territorial Epidemiologists in 199833 and the more conservative definition for injuries used by The State and Territorial Injury Prevention Directors Association.34 This coordinated national approach is vital to establishing a nationwide public health surveillance system for carbon monoxide poisoning.
CONCLUSION
The challenges to establishing a nationwide system for public health surveillance are formidable and include the need to standardize data collection, analysis, and dissemination methodologies and the need for resources at the national, state, and local levels. Carbon monoxide surveillance is technically feasible; the data sources and the technical expertise to gather, analyze, and disseminate them exist in the current public health infrastructure. The leading challenges are the need for the recognition of carbon monoxide poisoning as a significant public health issue by public health practitioners, clinicians, and policy makers, and the subsequent identification and dedication of the necessary resources.
Acknowledgments
The authors thank the National Workgroup on Carbon Monoxide Poisoning, which produced the White Paper on Carbon Monoxide Surveillance, from which this commentary evolved.
This work was generously supported in part by grants from the Environmental Public Health Tracking Branch, National Center for Environmental Health (NCEH), Centers for Disease Control and Prevention to the Maine Department of Health and Human Services, the Washington State Department of Health, the New York City Department of Health and Mental Hygiene, and the Wisconsin Division of Public Health (U50/CCU122452; U50/CCU022438; U50/CCJU222455 and U50/CCU223290; and U38 000192-01, respectively).
While this article was supported by an environmental public health tracking cooperative agreement from CDC, its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1.Unintentional non-fire-related carbon monoxide exposures—United States, 2001–2002. MMWR Morb Mortal Wkly Rep. 2005;54(02):36–9. [PubMed] [Google Scholar]
- 2.Carbon monoxide poisoning after hurricane Katrina—Alabama, Louisiana, and Mississippi, August–September 2005. MMWR Morb Mortal Wkly Rep. 2005;54(39):996–1000. [PubMed] [Google Scholar]
- 3.Carbon monoxide poisonings after two major hurricanes—Alabama and Texas, August–October 2005. MMWR Morb Mortal Wkly Rep. 2006;55(09):236–9. [PubMed] [Google Scholar]
- 4.Public health consequences of a flood disaster. MMWR Morb Mortal Wkly Rep. 1993;42(34):653–6. [PubMed] [Google Scholar]
- 5.Houck PM, Hampson NB. Epidemic carbon monoxide poisoning following a winter storm. J Emerg Med. 1997;15:469–73. doi: 10.1016/s0736-4679(97)00079-6. [DOI] [PubMed] [Google Scholar]
- 6.Daley RW, Smith AE, Paz-Argandona E, Malilay J, McGeehin M. An outbreak of carbon monoxide poisoning after a major ice storm in Maine. J Emerg Med. 2000;18:87–93. doi: 10.1016/s0736-4679(99)00184-5. [DOI] [PubMed] [Google Scholar]
- 7.Yoon SS, Macdonald SC, Parrish RG. Deaths from unintentional carbon monoxide poisoning and potential for prevention with carbon monoxide detectors. JAMA. 1998;279:685–7. doi: 10.1001/jama.279.9.685. [DOI] [PubMed] [Google Scholar]
- 8.Deaths resulting from residential fires and the prevalence of smoke alarms—United States, 1991–1995. MMWR Morb Mortal Wkly Rep. 1998;47(38):803–6. [PubMed] [Google Scholar]
- 9.Mott JA, Wolfe MI, Alverson CJ, Macdonald SC, Bailey CR, Ball LB, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288:988–95. doi: 10.1001/jama.288.8.988. [DOI] [PubMed] [Google Scholar]
- 10.Cobb N, Etzel RA. Unintentional carbon monoxide-related deaths in the United States, 1979 through 1988. JAMA. 1991;266:659–63. [PubMed] [Google Scholar]
- 11.Hampson NB. Trends in the incidence of carbon monoxide poisoning in the United States. Am J Emerg Med. 2005;23:838–41. doi: 10.1016/j.ajem.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health and Human Services (US) 2nd ed. Washington: U.S. Government Printing Office; 2000. Nov, [cited 2006 Feb]. Healthy People 2010: understanding and improving health. Available from: URL: http://www.usmc-mccs.org/healthfitness/HealthyPeople2010/tableofcontents.htm. [Google Scholar]
- 13.Council of State and Territorial Epidemiologists. National Notifiable Disease Surveillance System. Reporting patterns of non-notifiable diseases and conditions. 2005. [cited 2006 Feb]. Available from: URL: http://www.cste.org/nndsssurvey/2004nndss/nndssstatechrreporcondnona2005.asp.
- 14.Unintentional carbon monoxide poisonings in residential settings—November 1993–March 1994. MMWR Morb Mortal Wkly Rep. 1995;44(41):765–7. [PubMed] [Google Scholar]
- 15.Girman JR, Chang YL, Hayward SB, Liu KS. Causes of unintentional deaths from carbon monoxide poisonings in California. West J Med. 1998;168:158–65. [PMC free article] [PubMed] [Google Scholar]
- 16.Moolenaar RL, Etzel RA, Parrish RG. Unintentional deaths from carbon monoxide poisoning in New Mexico, 1980 to 1988. A comparison of medical examiner and national mortality data. West J Med. 1995;163:431–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Unintentional deaths from carbon monoxide poisoning—Michigan, 1987–1989. MMWR Morb Mortal Wkly Rep. 1992;41(47):881–3. 889. [PubMed] [Google Scholar]
- 18.Seligman PJ, Frazier TM. Surveillance: the sentinel health event approach. In: Halperin W, Baker EL Jr, Monson RR, editors. Public health surveillance. New York: Van Nostrand Reinhold; 1992. [Google Scholar]
- 19.Jasper BW, Hopkins RO, Duker HV, Weaver LK. Affective outcome following carbon monoxide poisoning: a prospective, longitudinal study. Cogn Behav Neurol. 2005;18:127–34. doi: 10.1097/01.wnn.0000160820.07836.cf. [DOI] [PubMed] [Google Scholar]
- 20.Henry CR, Satran D, Lindgren B, Adkinson C, Nicholson CI, Henry TD. Myocardial injury and long-term mortality following moderate to severe carbon monoxide poisoning. JAMA. 2006;295:398–402. doi: 10.1001/jama.295.4.398. [DOI] [PubMed] [Google Scholar]
- 21.Thacker SB, Stroup DF, Parrish RG, Anderson HA. Surveillance in environmental public health: issues, systems, and sources. Am J Public Health. 1996;86:633–8. doi: 10.2105/ajph.86.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang CC, Tsai SS, Ho SC, Yang CY. Air pollution and hospital admissions for cardiovascular disease in Taipei, Taiwan. Environ Res. 2005;98:114–9. doi: 10.1016/j.envres.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Yang CY, Chen YS, Yang CH, Ho SC. Relationship between ambient air pollution and hospital admissions for cardiovascular diseases in Kaohsiung, Taiwan. J Toxicol Environ Health A. 2004;67:483–93. doi: 10.1080/15287390490276502. [DOI] [PubMed] [Google Scholar]
- 24.Tsai SS, Goggins WB, Chiu HF, Yang CY. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke. 2003;34:2612–6. doi: 10.1161/01.STR.0000095564.33543.64. Epub 2003 Oct 9. [DOI] [PubMed] [Google Scholar]
- 25.Salam MT, Millstein J, Li YF, Lurmann FW, Margolis HG, Gilliland FD. Birth outcomes and prenatal exposure to ozone, carbon monoxide, and particulate matter: results from the Children's Health Study. Environ Health Perspect. 2005;113:1638–44. doi: 10.1289/ehp.8111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilhelm M, Ritz B. Local variations in CO and particulate air pollution and adverse birth outcomes in Los Angeles County, California, USA. Environ Health Perspect. 2005;113:1212–21. doi: 10.1289/ehp.7751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Environmental Protection Agency (US) More details on carbon monoxide—based on data through 2002. [cited 2006 Mar]. Available from: URL: http://www.epa.gov/air/oaqps/greenbk/cindex.html.
- 28.Bhalla CK, Voicu I, Meltzer R, Ellen IG, Been V. New York: Furman Center for Real Estate and Policy, New York University; [cited 2006 Mar]. State of New York City's housing and neighborhoods 2004. Available from: URL: http://furmancenter.nyu.edu/CREUP_Papers/state_of_the_city/intro_material.pdf. [Google Scholar]
- 29.Housing and Urban Development (US) American housing survey 2004 metropolitan sample-items booklet. [cited 2006 Mar]. Available from: URL: http://www.huduser.org/datasets/ahs/AHS2004InstBook.zip.
- 30.Food and Drug Administration (US) Regulation number: 21 CFR 870.2700. [cited 2006 Sep]. Available from: URL: http://www.fda.gov/cdrh/pdf6/K061204.pdf.
- 31.Abellera J, Annest J, Conn JM, Kohn M Council of State and Territorial Epidemilologists; Data Committee Injury Control and Emergency Health Services Section; American Public Health Association; State and Territorial Injury Prevention Directors Association. How states are collecting and using cause of injury data: 2004 update to the 1997 report. 2005. Mar, Available from: URL: http://www.cste.org/pdffiles/newpdffiles/ECodeFinal3705.pdf.
- 32.Use of carbon monoxide alarms to prevent poisonings during a power outage—North Carolina, December 2002. MMWR Morb Mortal Wkly Rep. 2004;53(09):189–92. [PubMed] [Google Scholar]
- 33.Council of State and Territorial Epidemiologists. Position statement 1998-EH 1. Proposal to adopt new or amended surveillance definitions for four environmental conditions. [cited 2006 Mar]. Available from: URL: http://www.cste.org/ps/1998/1998-eh-01.htm.
- 34.Injury Surveillance Workgroup. Consensus recommendations for using hospital discharge data for injury surveillance. [cited 2006 Feb]. Available from URL: http://www.nahdo.org/documents/hdd.pdf.