SYNOPSIS
Objectives
The purpose of this study was to describe results from a pilot surveillance system for carbon monoxide poisoning—a significant yet preventable public health issue for which most public health agencies do not conduct routine public health surveillance.
Methods
The authors developed a rate-based statewide surveillance system. Cases were identified using the 1998 Council of State and Territorial Epidemiologists' case definition in hospital discharges, emergency department and hospital outpatient visits, and mortality data. Intentional and fire-related injuries were excluded. The system was supplemented with qualitative information from newspaper articles. Annual, age, and sex-specific incidence rates were estimated. Exposure source/setting was described using E-codes; occupational setting was assessed by combining E-codes and payer code. Cases occurring during a disaster-related power outage in January 1998 were compared with cases identified during routine surveillance from 1999 through 2003.
Results
During the five years of routine surveillance, 740 cases were identified; 47 (6.4%) were hospitalized, 442 (59.7%) were seen in an emergency department, and 251 (34.3%) were seen in another outpatient setting. More cases were observed in fall/winter; 23.1% of patients aged 16 or older were classified as exposed in an occupational setting. Among disaster-related cases, more were older (≥65 years of age; 11.9% vs. 4.2%) and female (61.6% vs. 45.3%); and fewer were in occupational settings (1.8% vs. 23.1%).
Conclusions
Establishing state-based public health surveillance for CO poisoning is feasible and essential for guiding prevention and control efforts. The finding that more than 20% of cases were classified as occupational should be investigated further.
Carbon monoxide (CO) is a colorless, odorless, toxic gas that results from the incomplete combustion of fossil fuels. It is one of the oldest documented poisons. There are potential sources of CO exposure in most homes and workplaces in the United States, including furnaces, motor vehicles, generators, gas heaters, and other small engine-powered appliances such as lawn mowers. The toxic effects of CO exposure are nonspecific; they include headache, dizziness, and nausea. For higher exposures (above 150–200ppm), disorientation, unconsciousness, and death are possible. The symptoms are easily mistaken for alternative causes, such as a viral illness. In addition to acute morbidity and mortality, somewhere from 10%–40% of CO poisoning survivors may have persistent neurological injury.1
Mortality and morbidity from acute, unintentional, non-fire-related CO poisoning is a substantial public health problem in the United States.1 Instances of CO poisoning that are either intentional or fire-related have other public health pathways for prevention and control and will be excluded from further discussion. CO poisoning is increasingly recognized as a public health concern in the wake of large scale disasters.2–9 CO poisoning also occurs as a result of routine domestic, occupational, and recreational activities.
An estimated 15,200 individuals seek medical attention annually in an emergency department (ED) or miss at least one day of work due to exposure to CO.10 The incidence of CO poisoning has remained stable from 1992 to 2002, while mortality rates have declined from 20.1 deaths per million people in 1968 to 8.8 deaths per million in 1998.11 This decline has been largely attributed to the reduction in CO emissions from automobiles, other prevention efforts, and improved treatment.12
CO poisoning is largely preventable by the combination of correct installation, maintenance, and operation of devices that may emit CO, with the appropriate use of CO detectors. CO detectors may prevent at least half of all deaths attributable to CO poisoning.13 Systematic, ongoing national, state, and local public health surveillance systems would be invaluable in the planning of new and the evaluation of existing prevention programs. Public health surveillance is conducted for many health conditions for which there are recognized, evidence-based primary or secondary prevention strategies; however, such systems do not exist for acute CO poisoning.
While no national surveillance system exists for acute CO poisoning, there are recently published national estimates for both mortality and morbidity at the national10,12 and state14–17 levels. There is an extensive body of literature describing excess cases of CO poisoning related to large scale power outages in the aftermath of disasters such as those caused by hurricanes,2–6 floods,7 and winter storms.8,9 Multiple reports also describe exposure from use of gasoline-powered engines and tools in occupational,18–20 residential,15,21 and recreational settings,22–26 some of which were open-air exposures.20,25,26 Historically, data sources for these reports were death certificate files and hospital chart reviews. Innovative combinations of data sources are now being used to investigate post-disaster-related CO poisoning including population-based surveys of risk factors27 and case finding using poison control center reports and reports from hyperbaric chamber treatments.28
We describe the development of a state-based surveillance system for unintentional, non-fire-related CO poisoning using a combination of existing data sources, analyzed using standard public health methodology. The system is largely based on hospital discharge and emergency department data, which are available in most states. We demonstrate how these data sources can infer exposure source and setting as well as help to describe and compare cases that occur subsequent to a natural disaster with those occurring at other times.
Objectives
A state-based public health surveillance system was developed using multiple data sources in order to: (1) Retrospectively estimate the statewide incidence of CO poisoning and related trends over time; (2) Describe the demographic and exposure characteristics of individuals with CO poisoning; (3) Assess our ability to monitor trends in sources of CO exposure over time; (4) Compare demographic and exposure characteristics of individuals with CO poisoning that occurred during a large scale power outage with those occurring at other times; (5) Describe risk factors for CO poisoning; (6) Detect and characterize exposure events; and (7) Use the system for planning and evaluating prevention programs.
METHODS
Data sources
Maine hospital visits and discharge data.
To estimate incidence of CO poisoning as well as to describe case and exposure characteristics, we used three Maine hospital records datasets: inpatient (IP), ED, and outpatient (OP), housed by the Maine Health Data Organization (MHDO). These datasets include record-level information for every patient visit to all non-federal acute care facilities in Maine. IP data include records of patients admitted to the facility by a physician. A patient presenting at an OP setting and then admitted in the course of the same visit will have a record only in the IP dataset. The ED data are a complete subset of the other two data sets; that is, patients seen in the ED and then admitted will have a record in the ED and IP datasets; those discharged will have a record in both the ED and OP datasets.
MHDO records do not include individual identifiers such as name or street address; patients have a unique identification number within any one facility. The datasets include demographic, diagnostic, procedural, payment, and length of stay information. Diagnostic information is coded using the International Classification of Diseases, Version 9—Clinical Modification (ICD-9 CM).29 Each electronic record has a “Principal Diagnosis Field,” which must contain a diagnosis code, and nine other secondary diagnosis fields may or may not be utilized. External cause of injury codes (E-codes) can be used in the secondary diagnosis fields only.
Maine death certificate files.
The Office of Data, Research, and Vital Statistics (ODRVS) maintains Maine electronic death certificate files. The data include an underlying cause of death code and up to 20 additional contributing causes. Cause of death was coded using ICD-10.30
Online newspaper search.
In order to capture additional information on place and type of exposure, particularly regarding occupational exposure, we used an online newspaper search engine, ProQuest Information and Learning Company. 31
Analytical methods
Morbidity and mortality data—case definition.
Records were selected that met the Council of State and Territorial Epidemiologists (CSTE) 1998 definition for public health surveillance for a “confirmed” or “probable” case of acute CO poisoning.32 A record with one or more E-codes indicating the injury was fire-related (E890.0–E899.9, inclusive) or intentional (E950.0–E959.9, inclusive; E962, inclusive; E952, inclusive), as well as those coded for late effects (E929.0–E929.9, inclusive) were excluded.
Statistical analysis—record identification.
Records meeting the case definition were identified from each of the IP, OP, and death certificate data sets from 1999 through 2003; a unique dataset of ED patients was available beginning in 2000 and cases were included through 2003 (previously these patients were categorized only as OP or IP). Records were excluded if the geocode of their residence was not within Maine. Data were de-duplicated within medical facilities.
Distribution by year, age, and sex.
Annual crude rates for the total population, as well as age and sex-specific rates, were estimated. Numerators were constructed using counts of records meeting the case definition from each dataset. The ODRVS updates U.S. Census population figures annually; hence, the ODRVS files were used to construct the denominators. All rates and exact binomial 95% confidence intervals are presented as the rate per 100,000 people.33
Seasonal distribution.
Seasonal trends were assessed visually using a histogram of cases by week over the six-year period from 1999 to 2003. The year was divided into two time periods to further assess seasonal effect: fall/winter (September through February) and spring/summer (March through August). The observed cases during the winter months were compared to the expected cases based on average monthly case counts.
Exposure setting and source.
E-codes were assessed for information on potential sources of exposure to CO. The percent of records with each CO-related E-code was estimated by using the number of records with the E-code as the numerator and the total number of cases of CO poisoning as the denominator, independent of the presence or absence of other E-codes in the same record.
Assessing if exposure occurred in an occupational setting.
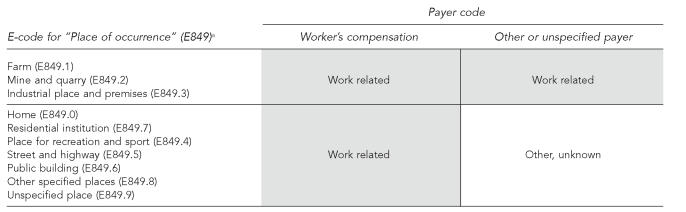
We assessed whether exposure occurred in a place of work using the OP records of patients aged 16 and older. We first used the documented CSTE approach:34 we identified records with the principal payer coded as “Worker's Compensation” and used the count of these records as the numerator and the count of all CO cases (aged 16 and older) as the denominator. We then further assessed place of exposure by using the E-code, “E849, Place of Occurrence,” which includes codes for potential occupational settings (e.g., Farm, E849.1; Mine and quarry, E849.2; Industrial place and premises, E849.3; residential Home, E849.0; Residential institution, E849.7), or other settings. We combined the E-code and payer code in an effort to more accurately describe exposures that occurred in workplaces (Figure 1).
Figure 1.
Information about occupationally related CO poisoning in outpatient hospital visits data
a Department of Health and Human Services (US). International Classification of Diseases, 9th Revision—Clinical Manifestation (ICD-9-CM). Hyattsville (MD): National Center for Health Statistics; 2004.
Analysis comparing disaster-related cases to all other cases.
On January 7, 1998, a catastrophic ice storm struck Maine and left more than half of the state's population without commercially provided electrical power. Large-scale outages continued for the next two to three weeks. In order to compare characteristics of individuals with CO poisoning that occurred during this disaster to those that did not, we defined disaster-related cases as those with onset of CO poisoning during the three-week period from January 7, 1998, to January 27, 1998, and nondisaster cases as those cases identified in 1999 to 2003. We used only the OP dataset for this comparison due to limited sample size in the other two datasets. Thus, we compared demographic characteristics (age and sex) and exposure characteristics (place and type of exposure) between disaster-related and nondisaster cases. Analyses were conducted using CMH chi-square tests to assess the null hypothesis of no difference between groups.
In addition, we estimated the number of excess cases that occurred as a result of the ice storm for both OP and IP datasets by calculating the number of cases expected to occur based on a thirty-day interval and using that number to determine the number of expected cases during the outbreak. We then described the difference between the observed and expected number of cases.
Assessment of ProQuest search results
We queried the ProQuest online search engine for information about usual increases in case counts. We searched the two available Maine newspapers, The Bangor Daily News and The Portland Press Herald, using the following search criteria: any article published from 1999 to 2003 that included the words “carbon monoxide” in the text. All headlines were manually reviewed; articles were retrieved and reviewed if the headline indicated that the article might provide information on multiple-person exposures. If exposures resulting in multiple illnesses were described, the MHDO databases were searched for corresponding records during a five-day window around the reported date of the incident. We summarized demographic and exposure characteristics of patients who corresponded temporally and geographically to the incident (and who were at least 16 years old).
RESULTS
Maine hospital visits and discharge data
Population rates.
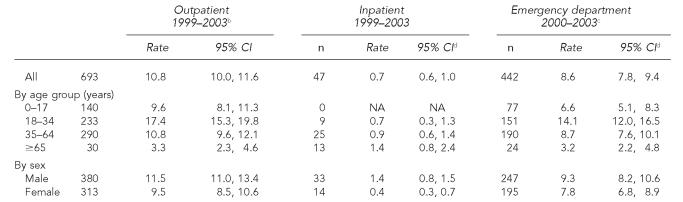
We identified a total of 740 cases; 47 (6.4%) were hospitalized; 442 (59.7%) were seen in an ED; 251 (34.3%) were seen in another outpatient setting. Twenty percent more cases were identified in the OP than by using only the ED (19.5%); the rates did not vary significantly by year (data not shown). In the OP and ED dataset, we observed statistically significant higher rates in the 18–34-year-old age group and lower rates in the 65 years and older group. In the IP setting, rates appeared highest in the older age group and there were no cases admitted among 0–17-year-olds. In all settings, more males than females were identified, with closely overlapping confidence intervals (Table 1).
Table 1.
Cases of CO poisoning in Maine—annual average rates based on hospital visits and hospitalization dataa
Data are housed and managed by Maine Health Data Organization; includes records of visits to any non-federal hospital facility in Maine.
Includes records of all outpatient visits billed through a non-federal hospital in Maine, including emergency department visits.
Includes a record of any visit to a non-federal hospital facility in Maine; emergency department data are a complete subset of the outpatient and inpatient datasets; data not available for 1999.
95% confidence intervals based on the binomial approximation to the Poisson distribution
CI = confidence interval
NA = no rates were calculated because there were no cases
Seasonal distribution.
More cases were observed during the fall and winter seasons, when the monthly average number of cases was 17, compared with the summer and spring seasons, when the average was 12.
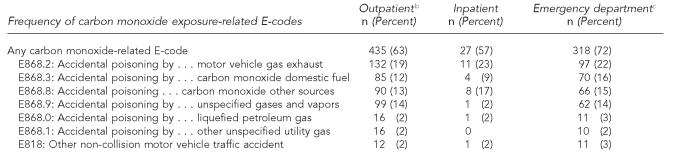
Exposure setting and source.
An E-code that potentially describes the source of CO exposure was present in 57% of IP dataset records and 72% of ED records (Table 2); the most commonly recorded E-code was for accidental poisoning by motor vehicle gas exhaust.
Table 2.
Frequency of E-codes related to carbon monoxide poisoning in Maine hospital discharge and visits data,a 1999–2003
Data are housed and managed by Maine Health Data Organization; include records of visits to any non-federal hospital facility in Maine.
Includes records of all outpatient visits billed through a non-federal hospital in Maine, including emergency department visits.
Includes a record of any visit to a non-federal hospital facility in Maine; emergency department data are a complete subset of the outpatient and inpatient datasets.
Assessment of workplace setting.
Among OP records, 577 were 16 years or older, and so were included in the assessment of workplace exposure (Figure 1). Of these records, 77 (13%) were coded with the principal payer of “Worker's Compensation”; likewise, 77 (13%) records were coded with a Place of Occurrence E-code (all but two were coded to E849.3, “Industrial place and premises”). On limited occasions, the same record had both the payer code and an E-code for place of work (21 records); hence, combining the two identified 133 (23.1%) records as having been exposed in an occupational setting, an increase of 72% over using payer code alone.
Analysis of disaster-related cases to all other cases.
During the three-week disaster period, 193 cases were identified in the OP setting while six cases were expected; 11 cases were identified in the IP setting, while less than one case was expected. Compared to the expected number of monthly cases, an excess of 193 cases per month in the OP setting and 10 excess hospital admissions were observed.
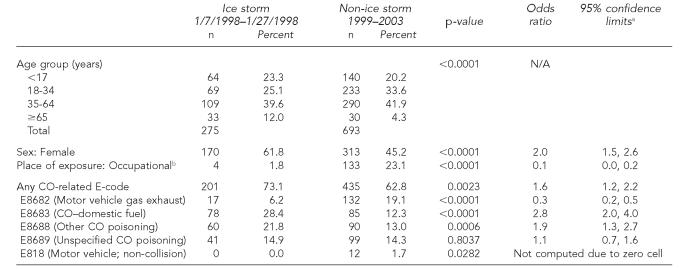
Comparing cases (OP only) that occurred during the three-week disaster period with cases occurring from 1999 through 2003 resulted in the following observations: a significantly higher percentage of disaster-related cases were age 65 or older (12.0% vs. 4.3%) and fewer were aged 18 to 34 (25.1% vs. 33.6%); more were female (61.8% vs. 45.2%) and fewer were classified as occurring at a workplace (1.8% vs. 23.1%); fewer disaster-related cases were coded as accidental exposure to motor vehicle exhaust fuel (6.2% vs. 19.1%) and more as exposure to domestic fuel (28.4% vs. 12.3%) (Table 3).
Table 3.
Person and exposure characteristics of cases occurring during the ice storm with those occurring from 1999–2003
95% confidence intervals based on the normal distribution
Records with age ≤15 excluded; records with the principal payer coded as Worker's Compensation or with a diagnostic code of E849.1 (Farm) or E849.2 (Mine and quarry), or E849.3 (Industrial place and premises)
Mortality data
Two records meeting the case definition for death due to CO poisoning were identified in the death certificate files in 2003; there were none for 1999 through 2002.
ProQuest search results
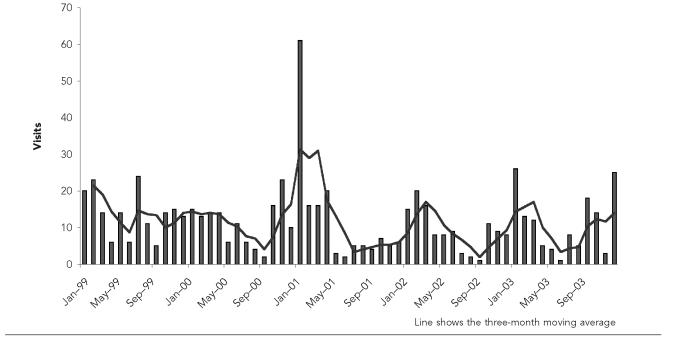
The ProQuest query identified 76 articles matching the search criteria. After reviewing the titles and abstracts, nine were retrieved and the full text was reviewed; six provided information about three separate occupational exposure incidents that resulted in multiple people seeking medical care for CO poisoning. Two of the events, in July 1999 and January 2001, had been observed in the histogram (Figure 2) as unusually high peaks; malfunctioning forklifts (one each in an agricultural and industrial setting) caused these events. The third event (July 2003) occurred in a restaurant kitchen. When these events were matched temporally and spatially with the OP data set, 17, 29, and 7 records were identified respectively for each event. A Principal Payer code for Worker's Compensation was present in 5% to 14% of these records. Conversely, the majority of records associated with each incident had a secondary diagnostic field that was coded with E849.3: Place of occurrence: Industrial place and premises (range: 59% to 96%).
Figure 2.
Outpatient visits for carbon monoxide poisoning by month, Maine 1999–2003
a Data are housed and managed by Maine Health Data Organization; includes records of visits to any non-federal hospital facility in Maine. Includes records of all outpatient visits billed through a non-federal hospital in Maine—including emergency department visits.
DISCUSSION
The need for nationwide public health surveillance of CO poisoning is recognized in the national Healthy People 2010 goal of “increasing the number of Territories, Tribes, and States, and the District of Columbia that monitor carbon monoxide poisoning from 7 to 51.”35 Using multiple data sources, we designed a public heath surveillance system with the ability to retrospectively describe the characteristics of those poisoned, detect and describe the magnitude of exposure events, assess trends in incidence over time, and identify and track risk factors for both disaster-related and routine cases of acute carbon monoxide poisoning. The system is being used to define the magnitude of the problem, as well as the relative contribution of various exposure sources; such a system is not only feasible, but also essential for planning and evaluating prevention efforts.
Thirteen states and New York City currently list acute CO poisoning as a reportable condition.36 Ninety percent of state health departments currently have access to hospitalization (IP) data;37 however, the relatively small magnitude of cases identified in the IP datasets means that, for public health jurisdictions with relatively small populations, a CO surveillance system could not be based solely on IP data. Fortunately, the number of states with access to ED data is rapidly increasing; 25 states currently have access to these data, up from 12 states in 1997.37 Unfortunately, few states currently have access to OP data; in our data, approximately 10%–20% more cases were identified annually in the OP than ED dataset alone. A potential limitation of a system based on ED data alone is that it will not identify individuals with less severe cases who may present to outpatient settings or private clinician offices, call poison control centers, or who simply do not get treated. Poison control center data may be a potential source to identify individuals with CO poisoning who do not present for treatment at a hospital-based setting; however, poison control centers are often unable to confirm the exposure status of the patient.38 In this pilot system, we chose to limit our data sources to those with clinically confirmed diagnosis.
Public health surveillance is dependent upon the establishment and adoption of a clear and reliable case definition. A case definition must include criteria for person, place, and time that should be further characterized by the degree of certainty regarding diagnosis, such as “confirmed” or “suspected.”39 We attempted to limit our case capturing to non-fire-related cases as well as unintentional cases. However, the specificity for doing so in ICD-9 CM datasets is unknown. A systematic study, probably based on chart reviews, should be undertaken to assess the validity of this approach. We also limited cases to residents of Maine. Although that is standard surveillance methodology, the impact on a nationwide system would be that residents of one state who seek care in another would not be included in any system. If multi-jurisdictional surveillance is initiated, agreements for the receipt of data for residents treated elsewhere should be established.
Because the only patient identifier in the MHDO data is a scrambled medical record number, the data could be reliably de-duplicated only within facilities. This could have resulted in counting the same case more than once if a person was transferred to another facility. We attempted to identify transfers from outpatient facilities to the one facility with a hyperbaric chamber by matching cases on date of birth, date of admission/transfer, sex, and residential ZIP code; only two possible transfers were identified based on the limited demographic information available. Because the number was relatively small and identification was not assured, these cases were retained in both the outpatient and inpatient datasets.
While few cases were identified in the death certificate files that met the case definition for CO poisoning, between one and three death certificate file records a year did meet the CSTE case definition for being a suspected case. Information from medical examiners' records may add information that would allow more specificity in case classification. Previous studies have found 12%16 and 15%40 of death certificate records were misclassified as not due to CO poisoning. These studies used a broader case definition than the one we applied and we found no published reports of misclassification of CO poisoning in hospital admissions data. This issue should be investigated as new data sources are identified and used for surveillance.
Our overall ED rates were higher than those from a national review of ED data from the National Electronic Injury Surveillance System All Injury Program (NEISS-AIP), 10 which reported an overall annual rate of 5.3/100,00 from 2001–2003, compared with our overall rate of 8.6/100,000. The demographic characteristics of our cases was also substantially different from those reported; the NEISS-AIP report found the highest rates among the youngest age group with a linear decline to the lowest rates in individuals aged 65 and older and reported a slightly higher rate among women than men; our highest rates were among those aged 18–34, and we observed slightly higher rates among men than women. These differences could be due to the use of different data sources (chart abstraction and billing data, respectively), regional differences in hospital utilization, or in exposure patterns. The latter includes the possibility that there is a higher rate of occupational exposure in Maine than on average nationally. Our findings were consistent with other reports of proportionally more cases in the fall and winter.16,40,41
The MHDO data do not contain information about patient race or ethnicity; non-white race and Hispanic ethnicity have been identified as important risk factors for carbon monoxide poisoning6,8,10,16,40,41 and efforts should be made to collect this valuable information so that prevention programs can be targeted appropriately.
We found that E-codes provided some information about exposure source and setting; however, while approximately two-thirds of records had one or more E-codes describing exposure, the remainder did not. Records may not be E-coded either because the clinician did not record the information in the chart (either the information was not available or an adequate exposure history was not obtained) or because the technician abstracting the chart did not code the exposure (either due to hospital coding guidelines limiting the use of E-codes or due to oversight). Efforts are needed to better understand why some records do not contain E-codes and to both increase their use and ensure consistency of coding practices among facilities.
An important component of a carbon monoxide surveillance system is characterizing sources of exposure, understanding how those sources are changing over time, and identifying new sources as they emerge. However, because of the coding limitations discussed above, data on hospital visits do not provide adequate detail for this purpose. Data from poison control centers may provide more detailed information on exposure source, but these sources are not confirmed and capture a somewhat different patient population.38
Perhaps the best approach for better characterizing exposure sources is making CO poisoning a reportable condition and conducting case identification and follow-back investigations. CO poisoning in Maine is currently reportable only as an occupational condition and rarely reported. To successfully establish CO as a reportable condition, public health agencies will need to dedicate resources to developing and maintaining a system for investigating case reports, educating providers and other reporting sources, and analyzing and disseminating the data.
CSTE indicators estimate occupationally related hospitalizations by using the principal payer field; i.e., a code for “Worker's Compensation” classifies the record as occupational. It is well documented that this approach underestimates cases.34,42 To address this issue, we combined information from the E-code, which describes place of injury, with the payer code, which gives the principal source of reimbursement. This approach substantially increased our estimate of the burden of CO poisoning that may occur in a place of work (from 13% using payer code alone to 23%). Review of newspaper accounts of occupationally-based events involving multiple people provided some validation for this approach; the vast majority of the records related to these events were not coded as Worker's Compensation but did have a place of occurrence E-code that indicated an occupational setting. Maine hospital visit data have a principal diagnosis field and up to nine additional diagnostic fields that may contain E-codes; data formats and coding practices vary considerably among states and this method may not be applicable in all locales.
The newspaper search also provided information about exposure setting and source, as well as confirmed our suspicion that deaths occurring in January 1998 were indeed excess deaths related to the ice storm. Among the cases we classified as ice-storm-related compared with non-ice-storm-related cases, we observed higher rates of CO poisoning among women and individuals aged 65 and older. The 2004 Maine Behavioral Risk Factor Surveillance System survey queried respondents about generator use and placement; female gender was identified as the sole demographic predictor of improper generator placement. While these results may reflect recall or response bias, the consistency of findings across the data sources suggests that education about using alternative fuel sources during or in the aftermath of a power outage should include women and the elderly.
Cases identified during the ice storm were more likely to occur in a residence and less likely to be occupationally related; there were more cases attributable to domestic fuel and fewer to motor vehicle exhaust. These findings are consistent with the higher rates of residential exposure subsequent to a natural disaster. We chose to classify disaster and routine cases by time, without a geographic component. Although the principal impact of the ice storm was in central Maine, power outages occurred throughout the state, and power was restored in a staggered manner to homes throughout the three-week period, during which we classified all cases as “ice storm-related.” Any such geographic and/or temporal misclassification would have resulted in non-disaster-related cases being classified as disaster-related cases; hence, any bias in our findings would be toward the null hypothesis.
CONCLUSIONS AND RECOMMENDATIONS
There are basic gaps in our knowledge of the epidemiology and outcomes of CO poisoning, including the true magnitude of morbidity and mortality, frequency of exposure routes, and the burden and severity of neurological sequelea. An ongoing public health surveillance system is needed to lay the basis to address these issues as well as to guide the development and evaluation of prevention programs.
Acknowledgments
The authors thank Dr. Steven C. Macdonald, Washington State Department of Health, for his thoughtful review of the manuscript and ongoing collaboration and support, as well as the staff of the Maine Health Data Organization and Brenda Corkum of the Office of Data Research and Vital Statistics, Maine Department of Health and Human Services, for facilitating access to their data and assisting with data interpretation.
This work was generously supported by cooperative agreement U50/CCU122452 from the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC.
REFERENCES
- 1.Ernst A, Zibrak JD. Carbon monoxide poisoning. N Engl J Med. 1998;339:1603–8. doi: 10.1056/NEJM199811263392206. [DOI] [PubMed] [Google Scholar]
- 2.Deaths associated with Hurricanes Marilyn and Opal—United States September–October 1995. MMWR Morb Mortal Wkly Rep. 1995;45(2):32–8. [PubMed] [Google Scholar]
- 3.Deaths associated with Hurricane Georges—Puerto Rico, September 1998. MMWR Morb Mortal Wkly Rep. 1998;47(42):897–8. [PubMed] [Google Scholar]
- 4.Preliminary medical examiner reports of mortality associated with Hurricane Charley— Florida 2004. MMWR Morb Mortal Wkly Rep. 2004;53(36):835–7. [PubMed] [Google Scholar]
- 5.Morbidity and mortality associated with Hurricane Floyd—North Carolina, September–October 1999. MMWR Morb Mortal Wkly Rep. 1999;49(17):369–72. [PubMed] [Google Scholar]
- 6.Carbon monoxide poisoning from hurricane-associated use of portable generators—Florida, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(28):697–700. [PubMed] [Google Scholar]
- 7.Public health consequences of a flood disaster. MMWR Morb Mortal Wkly Rep. 1993;42(34):653–6. [PubMed] [Google Scholar]
- 8.Houck PM, Hampson NB. Epidemic carbon monoxide poisoning following a winter storm. J Emerg Med. 1997;15:469–73. doi: 10.1016/s0736-4679(97)00079-6. [DOI] [PubMed] [Google Scholar]
- 9.Daley WR, Smith A, Paz-Argandona E, Malilay J, McGeehin M. An outbreak of carbon monoxide poisoning after a major ice storm in Maine. J Emerg Med. 2000;18:87–93. doi: 10.1016/s0736-4679(99)00184-5. [DOI] [PubMed] [Google Scholar]
- 10.Unintentional non-fire-related carbon monoxide exposures—United States, 2001–2002. MMWR Morb Mortal Wkly Rep. 2005;54(2):36–9. [PubMed] [Google Scholar]
- 11.Hampson NB. Trends in the incidence of carbon monoxide poisoning in the United States. Am J Emerg Med. 2005;23:838–41. doi: 10.1016/j.ajem.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Mott JA, Wolfe MI, Alverson CJ, Macdonald SC, Bailey CR, Ball LB, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288:988–95. doi: 10.1001/jama.288.8.988. [DOI] [PubMed] [Google Scholar]
- 13.Yoon SS, Macdonald SC, Parrish RG. Deaths from unintentional carbon monoxide poisoning and potential for prevention with carbon monoxide detectors. JAMA. 1998;279:685–7. doi: 10.1001/jama.279.9.685. [DOI] [PubMed] [Google Scholar]
- 14.Girman JR, Chang YL, Hayward SB, Liu KS. Causes of unintentional deaths from carbon monoxide poisonings in California. West J Med. 1998;168(3):158–65. [PMC free article] [PubMed] [Google Scholar]
- 15.Unintentional carbon monoxide poisonings in residential settings—Connecticut, November 1993–March 1994. MMWR Morb Mortal Wkly Rep. 1995;44(41):765–7. [PubMed] [Google Scholar]
- 16.Moolenaar RL, Etzel RA, Parrish RG. Unintentional deaths from carbon monoxide poisoning in New Mexico, 1980 to 1988. A comparison of medical examiner and national mortality data. West J Med. 1995;163:431–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Unintentional deaths from carbon monoxide poisoning—Michigan, 1987–1989. MMWR Morb Mortal Wkly Rep. 1992;41(47):881–3. 889. [PubMed] [Google Scholar]
- 18.Unintentional carbon monoxide poisoning from indoor use of pressure washers—Iowa, January 1992–January 1993. MMWR Morb Mortal Wkly Rep. 1993;42(40):777–9. 785. [PubMed] [Google Scholar]
- 19.Carbon monoxide poisoning from use of gasoline-fueled power washers in an underground parking garage—District of Columbia, 1994. MMWR Morb Mortal Wkly Rep. 1995;44(18):356–7. 363–4. [PubMed] [Google Scholar]
- 20.Outdoor carbon monoxide poisoning attributable to tractor exhaust— Kentucky, 1997. MMWR Morb Mortal Wkly Rep. 1997;46(51):1224–7. [PubMed] [Google Scholar]
- 21.Use of unvented residential heating appliances— United States, 1988–1994. MMWR Morb Mortal Wkly Rep. 1997;46(51):1221–4. [PubMed] [Google Scholar]
- 22.Carbon monoxide levels during indoor sporting events— Cincinnati, 1992–1993. MMWR Morb Mortal Wkly Rep. 1994;43(2):21–3. [PubMed] [Google Scholar]
- 23.Carbon monoxide poisoning at an indoor ice arena and bingo hall— Seattle, 1996. MMWR Morb Mortal Wkly Rep. 1996;45(13):265–7. [PubMed] [Google Scholar]
- 24.Carbon monoxide poisoning deaths associated with camping— Georgia March 1999. MMWR Morb Mortal Wkly Rep. 1999;48(32):705–6. [PubMed] [Google Scholar]
- 25.Carbon monoxide poisoning resulting from exposure to ski-boat exhaust— Georgia June 2002. MMWR Morb Mortal Wkly Rep. 2002;51(37):829–30. [PubMed] [Google Scholar]
- 26.Carbon monoxide poisoning resulting from open air exposures to operating motorboats— Lake Havasu City Arizona,2003. MMWR Morb Mortal Wkly Rep. 2004;53(15):314–8. [PubMed] [Google Scholar]
- 27.Epidemiologic assessment of the impact of four hurricanes— Florida, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(28):693–7. [PubMed] [Google Scholar]
- 28.Carbon monoxide poisoning after hurricane Katrina—Alabama, Louisiana and Mississippi August–September 5, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(39):996–8. [PubMed] [Google Scholar]
- 29.Department of Health and Human Services (US) Hyattsville (MD): National Center for Health Statistics; 2004. International Classification of Diseases 9th Revision, Clinical Manifestation (ICD-9-CM) [Google Scholar]
- 30.World Health Organization. Geneva: World Health Organization; 1994. Manual of the international statistical classification of diseases, injuries, and causes of death, based on the recommendations of the Tenth Revision Conference, 1990. [Google Scholar]
- 31.ProQuest Information and Learning Company. ProQuest 2005. Available from: URL: http://proquest.umi.com/login.
- 32.Council of State and Territorial Epidemiologists. Proposal to adopt new or amended surveillance definitions for four environmental conditions. Position statement 1998-EH 1. [cited 2006 Nov 29]. Available from: URL: http://www.cste.org/ps/1998/1998-eh-01.htm.
- 33.Daly L. Simple SAS macros for the calculation of exact binomial and Poisson confidence limits. Comput Biol Med. 1992;22:351–61. doi: 10.1016/0010-4825(92)90023-g. [DOI] [PubMed] [Google Scholar]
- 34.Council of State and Territorial Epidemiologists. Occupational health indicators: a guide for tracking occupational health conditions and their determinants. 2004. Nov, [cited 2006 Nov 29]. Available from: URL: http://www.cste.org/pdffiles/Revised%20Indicators_12.14.04.pdf.
- 35.Department of Health and Human Services (US) Healthy people 2010: understanding and improving health. 2nd ed. [cited 2006 Nov 29]. Available from: URL: http://www.usmc-mccs.org/healthfitness/HealthyPeople2010/tableofcontents.htm.
- 36.Council of State and Territorial Epidemilologists; National Notofiable Disease Surveillance System. Reporting patterns for non-notifiable diseases and conditions. 2005. Available from: URL: http://www.cste.org/nndsssurvey/2004nndss/nndssstatechrreporcondnona2005.asp.
- 37.Abellera J, Annest J, Conn JM, Kohn M Council of State and Territorial Epidemilologists; Data Committee Injury Control and Emergency Health Services Section; American Public Health Association; State and Territorial Injury Prevention Directors Association. How states are collecting and using cause of injury data: 2004 update to the 1997 report. 2005 Mar [Google Scholar]
- 38.Bekkedal M, Sipsma K, Stremski ES, Malecki KC, Anderson HA. Evaluation of five data sources for inclusion in a statewide tracking system for accidental carbon monoxide poisonings. WMJ. 2006;105(2):36–40. [PubMed] [Google Scholar]
- 39.Teutsch SM. Considerations in planning a surveillance system. In: Tuetsch SM, Churchill RE, editors. Principles and practice of public health surveillance. Oxford, New York: Oxford University Press; 2000. [Google Scholar]
- 40.Liu KS, Paz MK, Flessel P, Waldman J, Girman J. Unintentional carbon monoxide deaths in California from residential and other nonvehicular sources. Arch Environ Health. 2000;55:375–81. doi: 10.1080/00039890009604033. [DOI] [PubMed] [Google Scholar]
- 41.Cobb N, Etzel RA. Unintentional carbon monoxide-related deaths in the Unites States 1979 through 1988. JAMA. 1991;266:659–63. [PubMed] [Google Scholar]
- 42.Biddle J, Roberts K, Rosenman KD, Welch EM. What percentage of workers with work-related illnesses receive workers' compensation benefits? J Occup Environ Med. 1998;40:325–31. doi: 10.1097/00043764-199804000-00006. [DOI] [PubMed] [Google Scholar]