Abstract
Poly(ADP-ribose)polymerase (PARP) is a nuclear enzyme which plays an important role in regulating cell death and cellular responses to DNA repair. Pharmacological inhibitors of PARP are being considered as treatment for cancer both in monotherapy as well as in combination with chemotherapeutic agents and radiation, and were also reported to be protective against untoward effects exerted by certain anticancer drugs.
Here we show that pharmacological inhibition of PARP with 3-aminobenzamide or PJ-34 dose-dependently reduces VEGF-induced proliferation, migration and tube formation of human umbilical vein endothelial cells in vitro.
These results suggest that treatment with PARP inhibitors may exert additional benefits in various cancers and retinopathies by decreasing angiogenesis.
Keywords: Poly(ADP-ribose)polymerase (PARP), angiogenesis, proliferation, migration, tube formation, HUVEC, 3-AB, PJ-34
Introduction
Poly(ADP ribose) polymerase (PARP), also known as poly(ADP ribose) synthetase (PARS), is a family of abundant nuclear enzymes of eukaryotic cells that participates in the regulation of DNA repair, gene transcription, cell cycle progression, chromatin function, genomic stability and cell death [1; 2]. Pharmacological inhibitors of PARP are recently being considered as treatment for cancer both in monotherapy as well as in combination with chemotherapeutic agents and radiation [2; 3; 4; 5; 6; 7] and entering clinical development as cytoprotective agents in cardiovascular diseases [2; 4; 8]. Angiogenesis is very important in the growth and metastasis formation of a variety of tumors, and increased angiogenesis also contributes to the development of blindness associated with diabetic retinopathy. In the present study we studied the effects of PARP inhibition with 3-AB and PJ-34 on VEGF-induced proliferation, migration and tube formation of human umbilical vein endothelial cells in vitro.
Materials and Methods
Reagents
Human recombinant VEGF165 was purchased from R&D systems (Minneapolis, MN). PARP inhibitor 3-aminobenzamide was obtained from Sigma, and PJ-34 was from Inotek Pharmaceuticals (Boston, MA).
Cell Culture
Human umbilical vein endothelial cells (HUVEC) and endothelial cells growth medium EGM™ were purchased from Cambrex, (Walkersville, MD) and cells were cultured in EGM™ medium according to manufacture’s instruction. Cells were grown in either 100 mm dishes or 6 well multi-dish chambers coated with 0.2 % gelatin. Cells were used within passages 3 to 7. Prior to treatment, cells were acclimatized in endothelial basal medium containing 1% FBS (Invitrogen, CA) 6 hrs and then treated.
Cell viability assays
Cells were grown in 96 well plates and treated with either aminobenzamide (3-AB) or PJ 34 with varying concentrations for 6 hrs in growth factor free medium containing 1 % FBS. Then effects of the PARP inhibitors on cell viability were determined using commercially available MTT assay (Promega, WI). Each experiment was repeated in triplicate and the entire set of experiments was repeated three times.
Proliferation assay
Endothelial cells (5 X 103 ) cells were suspended in 100 μl of growth factor free medium containing 1 % FBS and then treated with either VEGF 20 ng/ml alone or PARP inhibitors 3-AB (0.5–6 mM) and PJ 34 (0.5–6 μM) and seeded on to 0.2 % gelatin coated 96 well plates and allowed to proliferate for 24 hrs. Then BrdU labeling solution was added and incubated further for 12 hrs. After the incubation, the effect of PARP inhibitors on VEGF induced proliferation of the HUVECs was determined by the extent of BrdU incorporation using ELISA kit following the protocol supplied by the manufacturer (Roche Diagnostics, IN). In brief, after the incubation of cells with BrdU labeling solution, the medium was aspirated and the cells were fixed and incubated with anti-BrdU antibody. After washing, the cells were incubated with secondary antibody conjugated with horse radish peroxidase. Finally, the extent of BrdU incorporation was determined colorimetrically at 450 nm. The treatments were performed in triplicate and the experiment was repeated at least three times.
Migration assay
The migration assays were performed in a 24–well modified Boyden chamber as described earlier [9]. In brief, 8 μm cell culture inserts (BD Biosciences) coated with 0.2 % gelatin (Sigma) were placed over the bottom chamber containing 20 ng/ml VEGF as the chemo-attractant. Growth factor free medium containing 1% FBS served as negative control. 3 X 104 cells were suspended in 150 μl in growth factor free medium containing 1% FBS. Then the cells were pretreated with PARP inhibitors, for 30 min at 37°C in 5% CO2 incubator. Then the HUVECs cell suspension was added to the upper chamber. After 8 hrs of incubation at 37°C, the non-migrated cells on the upper surface of the filter were removed by gentle swabbing with cotton tipped applicators. The cells that had migrated to the lower side of the chamber were fixed with 100 % methanol for 15 min at room temperature. After complete drying, the cells were stained with 0.5 % Giemsa stain (Sigma). 3–4 fields per insert were counted using 10X objective using Olympus IX81 microscope. The assays were performed in triplicate.
In vitro angiogenesis assay
The effect of PARP inhibits on inhibiting the formation of tube-like structures on growth factor reduced Matrigel (BD Biosciences) were performed as described earlier [9; 10]. In brief, 96 well plates were coated with 50 μl of growth factor reduced Matrigel and allowed to solidify at 37°C in 5% CO2. During the incubation for the solidification of Matrigel, the cells were treated exactly as described as above and seeded on to the solidified matrix. After 12 hrs of incubation at 37°C in 5% CO2, the medium was carefully aspirated and the cells were fixed with 4% formaldehyde and the images were captured using Olympus IX81 microscope. The tube length was quantified using the NIH Image J software. Results are represented as total tube length (μm) for three photographic fields per experimental condition. Each treatment was performed in duplicate and the set of experiment was independently repeated three times.
Statistical analysis
Values are represented as mean ± SD. The statistical significance of the data was analyzed using students ‘t’ test. P < 0.05 was considered as significant.
Results
PARP inhibitors did not affect cell viability in HUVECs
As shown in Fig.1, and consistently with results of numerous previous studies ( [11; 12; 13]; reviewed in [1]) 3-AB (0.5–6 mM) and PJ-34 (0.5–6 μM) did not decrease cell viability in HUVECs.
Fig.1. PARP inhibitors did not affect cell viability of HUVECs.
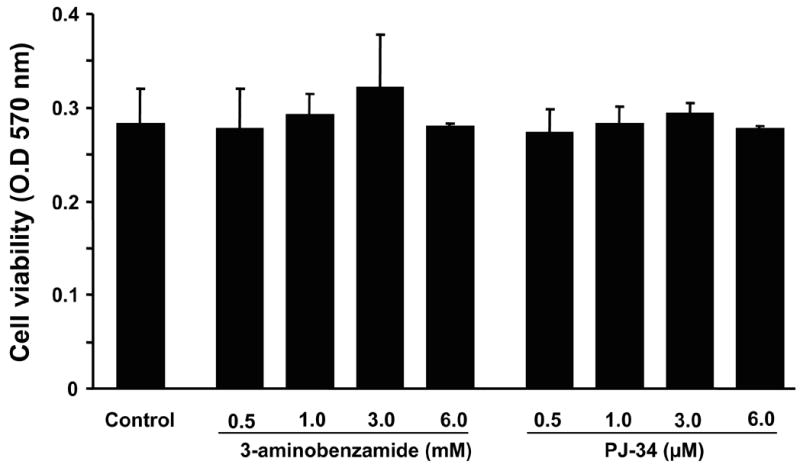
Cells were grown in 96 well plates and treated with either aminobenzamide (3-AB) or PJ-34 with varying concentrations as indicated for 6 hrs. Then the cytotoxic effects of the PARP inhibitors were determined using commercially available MTT assay, n = 3.
PARP inhibitors decrease VEGF- induced proliferation of HUVECs
As shown in Fig.2., VEGF enhanced the proliferation of HUVECs (measured by BrdU incorporation assay) by 4 fold (P<0001 vs. control) and both 3-AB and PJ-34 significantly inhibited the HUVECs proliferation in a dose dependent manner (P < 0.001 vs. VEGF). 3-AB or PJ-34 alone had no effect on the proliferation of HUVECs (data not shown).
Fig.2. PARP inhibitors decrease VEGF-induced proliferation of HUVECs.
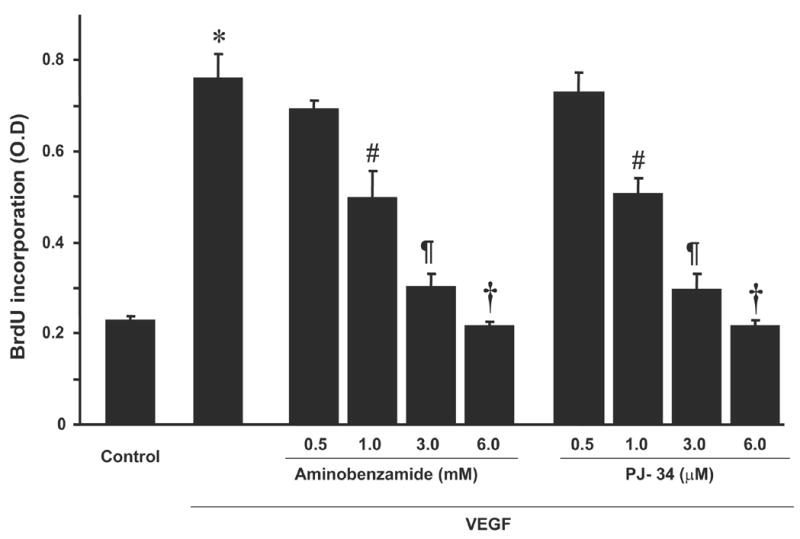
HUVECs were treated with either VEGF alone or with PARP inhibitors as indicated and the proliferation of HUVECs were assed by measuring the rate of BrdU incorporation by ELISA kit colorimetricaly at 450 nm. * P < 0.001 vs. control ; # P < 0.001 vs. VEGF ; ¶ P < 0.001 vs. VEGF ; † P < 0.001 vs. VEGF ; n =3.
PARP inhibitors decrease VEGF- induced migration of HUVECs
As shown in Fig. 3, VEGF significantly enhanced the migration of HUVECs in the order of ~3 fold (P < 0.001 vs. control). 3-AB and PJ-34 elicited concentration dependent inhibition in VEGF induced migration of HUVECs (Fig. 3A and B, P<0.001 vs. VEGF). On the other hand, 3-AB or PJ-34 by itself had no effect on migration and the results were comparable to that of vehicle control (data not shown).
Fig.3. PARP inhibitors attenuate VEGF-induced migration of HUVECs.

Cells were treated with either VEGF or PARP inhibitors as indicated and migration assays were performed using Boyden chamber.
(A) Depicts the representative images of HUVECs migrated in response to treatment with either vehicle control, 20 ng/ml VEGF alone, 6 mM 3-AB + VEGF or 6 μM PJ–34 respectively.
(B) Shows the quantification of data for cell migration in response to treatments. * P < 0.001 vs. control; # P < 0.001 vs. VEGF ; ¶ P < 0.001 vs. VEGF ; † P < 0.001 vs. VEGF ; n =3.
PARP inhibitors decrease VEGF-induced tube formation in vitro in HUVECs
When HUVECs were placed on growth factor reduced Matrigel, in the presence of VEGF 20 ng/ml, endothelial cells differentiate in to tube- like structures mimicking the neoangiogenesis process in vivo (Fig. 4, P < 0.001 vs. control). When HUVECs were pretreated with 3-AB (0.5 – 6 mM) or PJ-34 (0.5 – 6.0 μM) and plated on to polymerized Matrigel, in the presence of VEGF (20 ng/ml), both 3-AB and PJ-34 dose-dependently inhibited the tube formation of HUVECs when compared with cells treated with VEGF alone (Fig. 4; P < 0.001 vs. VEGF). Quantification of tube length revealed that VEGF enhanced the tube formation by ~3 fold when compared to control cells and this was decreased by PARP inhibitors in dose-dependent manner. PARP inhibitors alone had no effect on tube formation of HUVECs (data not shown).
Fig.4. PARP inhibitors inhibit VEGF-induced tube formation in vitro.

HUVECs were treated with either VEGF or PARP inhibitors+VEGF and an in vitro angiogenesis assays were performed using growth factor reduced Matrigel as described in the Methods section.
(A) Depicts the representative images of tube formation of cells treated with either VEGF alone or with 3-AB (6 mM) or PJ-34 (6 μM) showing the maximum inhibitory effect.
(B) Shows the quantitative data for the tube lengths in cells treated as indicated in the figure. * P < 0.001 vs. control ; # P < 0.001 vs. VEGF ; ¶ P < 0.001 vs. VEGF ; † P < 0.001 vs. VEGF ; n =3.
Discussion
Pharmacological inhibitors of PARP have been shown to decrease tumor growth and to restore sensitivity of resistant tumors to methylating agents or topoisomerase I inhibitors (drugs recently used for the treatment of various malignancies refractory to conventional chemotherapy), and to increase the sensitivity of cancer cells to radiotherapy [3; 4; 5; 6; 7; 14; 15; 16; 17; 18; 19; 20; 21; 22]. The use of PARP inhibitors as anticancer agents exploits the fact that the repair of certain types of antitumor-agent related cellular damage relies almost exclusively on the functional integrity of PARP [3].
In the present study we demonstrate that pharmacological inhibition of PARP exerts antiangiogenic effects by reducing VEGF-induced proliferation, migration and tube formation of human umbilical vein endothelial cells in vitro. These results suggest that PARP inhibition may exert additional beneficial effects by decreasing angiogenesis-dependent growth in certain types of tumors and by inhibiting tumor metastasis formation. Interestingly, a semisynthetic tetracycline antimicrobial antibiotic minocycline, which has recently been reported to have potent PARP-1 inhibitory effects [23; 24] also inhibits angiogenesis [25].
Antiangiogenetic potential of PARP inhibitors can further be exploited for the treatment of diabetic retinopathy, where the pathologically increased angiogenesis is the major cause of complications and blindness. PARP activation is also involved in the development of various diabetic complications (reviewed in [26]) including retinopathy [27; 28] and PARP inhibitors exert protective effects against these pathologies [26].
Excitingly, PARP inhibitors were also reported to protect against nephrotoxicity of cisplatin [29] and cardiotoxicity of doxorubicin [30; 31], which cause oxidative/nitrosative stress and consequent PARP overactivation and cell death. The cytoprotective effects of PARP inhibitors comprise of inhibition of the pathological overactivation of PARP, and blockade of the cell from entering into necrosis via over-utilization of cellular NAD+ pools and promotion of cellular energetic failure [1; 2].
Collectively, the present results suggest that treatment with PARP inhibitors may exert additional benefits in various cancers and retinopathies by decreasing angiogenesis.
Acknowledgments
This study was supported by the Intramural Research Program of NIH/NIAAA (to P.P.). Dr. Pacher wants to dedicate this work to his beloved mother Iren.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Virag L, Szabo C. The therapeutic potential of poly(ADP-ribose) polymerase inhibitors. Pharmacol Rev. 2002;54:375–429. doi: 10.1124/pr.54.3.375. [DOI] [PubMed] [Google Scholar]
- 2.Jagtap P, Szabo C. Poly(ADP-ribose) polymerase and the therapeutic effects of its inhibitors. Nat Rev Drug Discov. 2005;4:421–40. doi: 10.1038/nrd1718. [DOI] [PubMed] [Google Scholar]
- 3.Graziani G, Battaini F, Zhang J. PARP-1 inhibition to treat cancer, ischemia, inflammation. Pharmacol Res. 2005;52:1–4. doi: 10.1016/j.phrs.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Graziani G, Szabo C. Clinical perspectives of PARP inhibitors. Pharmacol Res. 2005;52:109–18. doi: 10.1016/j.phrs.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Tentori L, Leonetti C, Scarsella M, Muzi A, Mazzon E, Vergati M, Forini O, Lapidus R, Xu W, Dorio AS, Zhang J, Cuzzocrea S, Graziani G. Inhibition of poly(ADP-ribose) polymerase prevents irinotecan-induced intestinal damage and enhances irinotecan/temozolomide efficacy against colon carcinoma. Faseb J. 2006;20:1709–11. doi: 10.1096/fj.06-5916fje. [DOI] [PubMed] [Google Scholar]
- 6.De Soto JA, Wang X, Tominaga Y, Wang RH, Cao L, Qiao W, Li C, Xu X, Skoumbourdis AP, Prindiville SA, Thomas CJ, Deng CX. The Inhibition and Treatment of Breast Cancer with Poly (ADP-ribose) Polymerase (PARP-1) Inhibitors. Int J Biol Sci. 2006;2:179–85. doi: 10.7150/ijbs.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Soto JA, Deng CX. PARP-1 inhibitors: are they the long-sought genetically specific drugs for BRCA1/2-associated breast cancers? Int J Med Sci. 2006;3:117–23. doi: 10.7150/ijms.3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pacher P, Schulz R, Liaudet L, Szabo C. Nitrosative stress and pharmacological modulation of heart failure. Trends Pharmacol Sci. 2005;26:302–10. doi: 10.1016/j.tips.2005.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cattaneo MG, Pola S, Francescato P, Chillemi F, Vicentini LM. Human endostatin-derived synthetic peptides possess potent antiangiogenic properties in vitro and in vivo. Exp Cell Res. 2003;283:230–6. doi: 10.1016/s0014-4827(02)00057-5. [DOI] [PubMed] [Google Scholar]
- 10.Rajesh M, Kolmakova A, Chatterjee S. Novel role of lactosylceramide in vascular endothelial growth factor-mediated angiogenesis in human endothelial cells. Circ Res. 2005;97:796–804. doi: 10.1161/01.RES.0000185327.45463.A8. [DOI] [PubMed] [Google Scholar]
- 11.Garcia Soriano F, Virag L, Jagtap P, Szabo E, Mabley JG, Liaudet L, Marton A, Hoyt DG, Murthy KG, Salzman AL, Southan GJ, Szabo C. Diabetic endothelial dysfunction: the role of poly(ADP-ribose) polymerase activation. Nat Med. 2001;7:108–13. doi: 10.1038/83241. [DOI] [PubMed] [Google Scholar]
- 12.Soriano FG, Pacher P, Mabley J, Liaudet L, Szabo C. Rapid reversal of the diabetic endothelial dysfunction by pharmacological inhibition of poly(ADP-ribose) polymerase. Circ Res. 2001;89:684–91. doi: 10.1161/hh2001.097797. [DOI] [PubMed] [Google Scholar]
- 13.Jagtap P, Soriano FG, Virag L, Liaudet L, Mabley J, Szabo E, Hasko G, Marton A, Lorigados CB, Gallyas F, Jr, Sumegi B, Hoyt DG, Baloglu E, VanDuzer J, Salzman AL, Southan GJ, Szabo C. Novel phenanthridinone inhibitors of poly (adenosine 5′-diphosphate-ribose) synthetase: potent cytoprotective and antishock agents. Crit Care Med. 2002;30:1071–82. doi: 10.1097/00003246-200205000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Delaney CA, Wang LZ, Kyle S, White AW, Calvert AH, Curtin NJ, Durkacz BW, Hostomsky Z, Newell DR. Potentiation of temozolomide and topotecan growth inhibition and cytotoxicity by novel poly(adenosine diphosphoribose) polymerase inhibitors in a panel of human tumor cell lines. Clin Cancer Res. 2000;6:2860–7. [PubMed] [Google Scholar]
- 15.Tentori L, Portarena I, Vernole P, De Fabritiis P, Madaio R, Balduzzi A, Roy R, Bonmassar E, Graziani G. Effects of single or split exposure of leukemic cells to temozolomide, combined with poly(ADP-ribose) polymerase inhibitors on cell growth, chromosomal aberrations and base excision repair components. Cancer Chemother Pharmacol. 2001;47:361–9. doi: 10.1007/s002800000248. [DOI] [PubMed] [Google Scholar]
- 16.Canan Koch SS, LH Thoresen, Tikhe JG, Maegley KA, Almassy RJ, Li J, Yu XH, Zook SE, Kumpf RA, Zhang C, Boritzki TJ, Mansour RN, Zhang KE, Ekker A, Calabrese CR, Curtin NJ, Kyle S, Thomas HD, Wang LZ, Calvert AH, Golding BT, Griffin RJ, Newell DR, Webber SE, Hostomsky Z. Novel tricyclic poly(ADP-ribose) polymerase-1 inhibitors with potent anticancer chemopotentiating activity: design, synthesis, and X-ray cocrystal structure. J Med Chem. 2002;45:4961–74. doi: 10.1021/jm020259n. [DOI] [PubMed] [Google Scholar]
- 17.Tentori L, Portarena I, Bonmassar E, Graziani G. Combined effects of adenovirus-mediated wild-type p53 transduction, temozolomide and poly (ADP-ribose) polymerase inhibitor in mismatch repair deficient and non-proliferating tumor cells. Cell Death Differ. 2001;8:457–69. doi: 10.1038/sj.cdd.4400832. [DOI] [PubMed] [Google Scholar]
- 18.Calabrese CR, Batey MA, Thomas HD, Durkacz BW, Wang LZ, Kyle S, Skalitzky D, Li J, Zhang C, Boritzki T, Maegley K, Calvert AH, Hostomsky Z, Newell DR, Curtin NJ. Identification of potent nontoxic poly(ADP-Ribose) polymerase-1 inhibitors: chemopotentiation and pharmacological studies. Clin Cancer Res. 2003;9:2711–8. [PubMed] [Google Scholar]
- 19.Calabrese CR, Almassy R, Barton S, Batey MA, Calvert AH, Canan-Koch S, Durkacz BW, Hostomsky Z, Kumpf RA, Kyle S, Li J, Maegley K, Newell DR, Notarianni E, Stratford IJ, Skalitzky D, Thomas HD, Wang LZ, Webber SE, Williams KJ, Curtin NJ. Anticancer chemosensitization and radiosensitization by the novel poly(ADP-ribose) polymerase-1 inhibitor AG14361. J Natl Cancer Inst. 2004;96:56–67. doi: 10.1093/jnci/djh005. [DOI] [PubMed] [Google Scholar]
- 20.Curtin NJ, Wang LZ, Yiakouvaki A, Kyle S, Arris CA, Canan-Koch S, Webber SE, Durkacz BW, Calvert HA, Hostomsky Z, Newell DR. Novel poly(ADP-ribose) polymerase-1 inhibitor, AG14361, restores sensitivity to temozolomide in mismatch repair-deficient cells. Clin Cancer Res. 2004;10:881–9. doi: 10.1158/1078-0432.ccr-1144-3. [DOI] [PubMed] [Google Scholar]
- 21.Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, Kyle S, Meuth M, Curtin NJ, Helleday T. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434:913–7. doi: 10.1038/nature03443. [DOI] [PubMed] [Google Scholar]
- 22.Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 23.Alano CC, Kauppinen TM, Valls AV, Swanson RA. Minocycline inhibits poly(ADP-ribose) polymerase-1 at nanomolar concentrations. Proc Natl Acad Sci U S A. 2006;103:9685–90. doi: 10.1073/pnas.0600554103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szabo C, Pacher P, Swanson A. Novel modulators of poly(ADP-ribose) polymerase. Trends in Pharmacological Sciences. 2006 doi: 10.1016/j.tips.2006.10.003. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tamargo RJ, Bok RA, Brem H. Angiogenesis inhibition by minocycline. Cancer Res. 1991;51:672–5. [PubMed] [Google Scholar]
- 26.Pacher P, Szabo C. Role of poly(ADP-ribose) polymerase-1 activation in the pathogenesis of diabetic complications: endothelial dysfunction, as a common underlying theme. Antioxid Redox Signal. 2005;7:1568–80. doi: 10.1089/ars.2005.7.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zheng L, Szabo C, Kern TS. Poly(ADP-ribose) polymerase is involved in the development of diabetic retinopathy via regulation of nuclear factor-kappaB. Diabetes. 2004;53:2960–7. doi: 10.2337/diabetes.53.11.2960. [DOI] [PubMed] [Google Scholar]
- 28.Obrosova IG, Minchenko AG, Frank RN, Seigel GM, Zsengeller Z, Pacher P, Stevens MJ, Szabo C. Poly(ADP-ribose) polymerase inhibitors counteract diabetes- and hypoxia-induced retinal vascular endothelial growth factor overexpression. Int J Mol Med. 2004;14:55–64. [PubMed] [Google Scholar]
- 29.Racz I, Tory K, Gallyas F, Jr, Berente Z, Osz E, Jaszlits L, Bernath S, Sumegi B, Rabloczky G, Literati-Nagy P. BGP-15 - a novel poly(ADP-ribose) polymerase inhibitor - protects against nephrotoxicity of cisplatin without compromising its antitumor activity. Biochem Pharmacol. 2002;63:1099–111. doi: 10.1016/s0006-2952(01)00935-2. [DOI] [PubMed] [Google Scholar]
- 30.Pacher P, Liaudet L, Bai P, Virag L, Mabley JG, Hasko G, Szabo C. Activation of poly(ADP-ribose) polymerase contributes to development of doxorubicin-induced heart failure. J Pharmacol Exp Ther. 2002;300:862–7. doi: 10.1124/jpet.300.3.862. [DOI] [PubMed] [Google Scholar]
- 31.Pacher P, Liaudet L, Mabley JG, Cziraki A, Hasko G, Szabo C. Beneficial effects of a novel ultrapotent poly(ADP-ribose) polymerase inhibitor in murine models of heart failure. Int J Mol Med. 2006;17:369–75. [PMC free article] [PubMed] [Google Scholar]


