Abstract
Background
Converging lines of evidence suggest that the hippocampus may be particularly vulnerable to deleterious effects of alcohol and marijuana use, especially during adolescence. The goal of this study was to examine hippocampal volume and asymmetry in adolescent users of alcohol and marijuana.
Methods
Participants were adolescent (aged 15–18) alcohol (ALC) users (n=16), marijuana and alcohol (MJ+ALC) users (n=26), and demographically similar controls (n=21). Extensive exclusionary criteria included prenatal toxic exposure, left handedness, and psychiatric and neurologic disorders. Substance use, cognitive, and anatomical measures were collected after at least 2 days of abstinence from all substances.
Results
Adolescent ALC users demonstrated a significantly different pattern of hippocampal asymmetry (p<.05) and reduced left hippocampal volume (p<.05) compared to MJ+ALC users and non-using controls. Increased alcohol abuse/dependence severity was associated with increased right > left (R>L) asymmetry and smaller left hippocampal volumes while marijuana abuse/dependence was associated with increased L>R asymmetry and larger left hippocampal volumes. Although MJ+ALC users did not differ from controls in asymmetry, functional relationships with verbal learning were found only among controls, among whom greater right than left hippocampal volume was associated with superior performance (p<.05).
Conclusions
Aberrations in hippocampal asymmetry and left hippocampal volumes were found for adolescent heavy drinkers. Further, the functional relationship between hippocampal asymmetry and verbal learning was abnormal among adolescent substance users compared to healthy controls. These findings suggest differential effects of alcohol and combined marijuana and alcohol use on hippocampal morphometry and the relationship between hippocampal asymmetry and verbal learning performance among adolescents.
Keywords: Adolescence, Drug effects, Brain Imaging, Alcohol Abuse, Cannabis Abuse
1. INTRODUCTION
Alcohol is the most widely used intoxicant among adolescents in the U.S. By 12th grade, 77% of students have tried alcohol and 33% reported getting drunk in the past month. Marijuana is the second most used intoxicant, with 20% of 12th graders reporting past month use (Johnston, O'Malley, Bachman, & Schulenberg, 2005). Furthermore, 58% of adolescent drinkers also use marijuana (Martin, Kaczynski, Maisto, & Tarter, 1996), contributing to frequent comorbidity between alcohol and marijuana use disorders (Agosti, Nunes, & Levin, 2002). This prevalence of alcohol and marijuana use during adolescence is of concern because the introduction of toxins may disrupt healthy brain development (Giedd et al., 1996; Sowell, Trauner, Gamst, & Jernigan, 2002). While overall brain size changes little beyond school-age (Giedd, 2004), white matter develops into the 20’s (Jernigan & Gamst, 2005; Pfefferbaum et al., 1994; Sowell, Thompson, Holmes, Jernigan, & Toga, 1999). Gray matter volume peaks around ages 12–14 then decreases, due largely to synaptic pruning (Huttenlocher, 1990). The few studies that examined the hippocampus specifically found increased volume (Giedd et al., 1996; Jernigan & Gamst, 2005; Suzuki et al., 2005) and increasing myelination (Benes et al., 1994) from childhood to adulthood.
Chronic heavy alcohol use is associated with deficits in brain structure and function (Rourke, 1996). Studies of adult alcoholics reveal white matter volume reductions and microstructural abnormalities (Estruch et al., 1997; Hommer et al., 1996; Kril, Halliday, Svoboda, & Cartwright, 1997; Pfefferbaum et al., 1996; Pfefferbaum et al., 2000), and gray matter volume deficits in hippocampal and other brain regions (Gansler et al., 2000; Laakso et al., 2000; Phillips, Harper, & Kril, 1987; Sullivan et al., 2005; Sullivan, et al., 1995). Neuropsychological studies demonstrate deficits in verbal and visual memory, working memory, visuospatial functioning, gait/balance, reasoning, inhibition, and speeded processing (Duka, et al., 2003; Garland, Parsons, & Nixon, 1993; Sullivan, et al., 2002; Sullivan, Rosenbloom, & Pfefferbaum, 2000; Townshend & Duka, 2005).
Adolescents may be particularly vulnerable to the neurotoxic effects of alcohol (see Barron et al., 2005; Monti et al., 2005; Spear, 2000). Animal studies show greater sensitivity during adolescence to the effects of alcohol on spatial working memory (Little, et al., 1996; Silveri & Spear, 1998; Swartzwelder, et al., 1998; White et al., 2002; White, et al., 2000; Yttri, Burk, & Hunt, 2004), social facilitation (Varlinskaya & Spear, 2006), and long-term potentiation (Pyapali, et al., 1999; Swartzwelder, Wilson, & Tayyeb, 1995), as well as greater cortical damage (Crews, et al., 2000; Hollstedt, Olsson, & Rydberg, 1980; Little et al., 1996). In humans, hippocampal (De Bellis et al., 2000; Nagel, et al., 2005) and prefrontal (De Bellis et al., 2005) volumes appear smaller and brain response during spatial working memory is abnormal (Tapert et al., 2004) in adolescents with alcohol use disorders. Heavy alcohol use during adolescence is associated with poorer verbal retrieval (Brown, et al., 2000), attention (Tapert & Brown, 1999), and visuospatial functioning (Giancola, Mezzich, & Tarter, 1998; Tapert, et al., , 2002). Thus, although adolescents have short lifetime drinking durations, heavy alcohol use is associated with abnormalities in brain structure, function, and cognitive performance.
Less is known about the neural consequences of marijuana use. Animal models show changes associated with chronic exposure in prefrontal regions, hippocampus, and cerebellum (Carta et al., 1998; Chan et al., 1998; Childers & Breivogel, 1998; Ghozland et al., 2002; Landfield, et al., 1999; Romero, et al., 1995; Rubino et al., 1997). As with alcohol, cannabinoids appear particularly neurotoxic to hippocampal neurons (Carlson, Wang, & Alger, 2002; Chan et al., 1998; Hoffman & Lupica, 2000; Kim & Thayer, 2001; Landfield, Cadwallader, & Vinsant, 1988). Adult human users (ages 21–35) show decreased gray matter density in the right parahippocampus and bilateral hippocampus compared to controls, but more white matter density in the left parahippocampus gyrus (Matochik, et al., 2005), which could suggest altered adolescent neuromaturational processes. The left hippocampus of marijuana using adults has shown lower regional cerebral blood flow during a verbal memory task (Block et al., 2002). Functional imaging studies have revealed abnormal brain functioning during spatial working memory (Kanayama et al., 2004), inhibitory processing (Gruber & Yurgelun-Todd, 2005), and motor sequencing (Pillay et al., 2004) among heavy marijuana using adults. In terms of neurocognitive effects, a meta-analysis suggested (Grant et al., 2003) that chronic cannabis use was primarily associated with some subtle persistent deficits in learning and memory. Nevertheless, other studies have reported deficits in attention, working memory, time estimation, response perseveration, and processing speed (Ehrenreigh et al., 1999; Bolla et al., 2002; Pope & Yurgelun-Todd, 1996; Solowij et al., 2002). However, neurocognitive deficits may normalize within a month of abstinence among adults (Pope et al., 2001).
Cannabis may differentially affect adolescents compared to adults. CB1 receptor levels peak in early adolescence and decrease thereafter (Belue et al., 1995) and cannabinoid exposed adolescent rats demonstrate more learning impairments compared to exposed mature rats (Cha et al., 2006; Schneider & Koch, 2003; Stiglick & Kalant, 1982, 1985). Wilson and colleagues (2000) retrospectively found that adults who used marijuana before age 17 had smaller gray matter and larger white matter volumes than later-onset users. Further, adults who initiated heavy marijuana use in early adolescence demonstrated poorer attention (Ehrenreich et al., 1999), verbal abilities and short term memory (Pope et al., 2003) compared to those who began use later. Thus far, no published studies have examined brain morphometry in adolescent marijuana users. A preliminary functional magnetic resonance imaging (FMRI) study found that adolescent users of marijuana demonstrate increased right hippocampal response during a 2-back verbal working memory task compared to non-users (Jacobsen et al., 2004), perhaps indicating that marijuana users failed to inhibit hippocampal activity due to cannabis-induced changes in inhibitory neurotransmission or apoptosis in the hippocampus. The few studies that have examined cognitive functioning in heavy marijuana using adolescents report deficits in attention (Tapert et al., 2002) and short-term memory (Schwartz et al., 1989).
In summary, converging lines of evidence suggest that the hippocampus may be particularly vulnerable to structural damage caused by heavy alcohol or marijuana use, especially during adolescence. Hippocampal functioning is associated with learning and memory formation (Eichenbaum, 1999; Squire, 1992). Animal models have demonstrated hippocampal asymmetry (e.g., Diamond et al., 1983), although it has not been examined in developing animals. In healthy adults, hippocampal asymmetry (typically greater right versus left hippocampal volumes; R>L) is often observed (for review see Pedraza, Bowers & Gilmore, 2004), although some studies have found minimal to no asymmetry (Bhatia et al., 1993; Raz et al., 2004). Typical hippocampal asymmetry is theorized to contribute to the functional differences in memory between the two hemispheres (Kawakami et al., 2003; Zaidel et al., 1997). Abnormal hippocampal asymmetry (including exaggerated R>L, L>R, and symmetry) has been associated with multiple clinical conditions, including Alzheimer’s disease (Barnes et al., 2004; Geroldi et al., 2000), schizophrenia (Kim et al., 2005; Zaidel et al., 1997), psychopathy (Raine et al., 2004), violent offending (Chesterman et al., 1994), and prolonged febrile convulsion (Scott et al., 2003). However, due to ongoing gray and white matter development (e.g., Giedd et al., 1996; Nagel et al., 2006; Sowell et al., 2002), results based on adults or children may not generalize to adolescents. Two studies have reported adolescent R>L hippocampal asymmetry; one included youth 4 to 18 years old (Giedd et al., 1996) and the other compared young adolescents (13–14) to young adults (19–21) (Suzuki et al., 2005). Foster and colleagues (1999) reported that during late adolescence, smaller left hippocampal volumes were associated with improved verbal recall. However, the relationship between hippocampal asymmetry and memory functioning in both healthy or substance-using adolescents is unknown.
Further, given the comorbidity of alcohol and marijuana use among adolescents (Agosti, Nunes, & Levin, 2002; Button et al., 2006; Martin, et al., 1996; SAMHSA, 2004), the effects of combined use of marijuana and alcohol use on hippocampal morphometry is also of great interest. Unfortunately, relatively little is known about the neurocognitive consequences of simultaneous use, and previous findings in adults have been conflicting. Some have found no additive acute motor or cognitive effects of combined cannabidiol (CBD) or THC and alcohol use (Belgrave et al., 1979b; Liguori et al., 2002), while others have found cumulative acute effects of THC or CBD and alcohol in perceptual and motor function (Belgrave et al., 1979a; Chait & Perry, 1993; Consroe et al., 1979). Additionally, simultaneous use of CBD and ethanol actually decreased blood alcohol levels (Consroe et al., 1979). Although previous research has shown reduced left hippocampal volumes in adolescent heavy drinkers (Nagel et al., 2005; DeBellis et al., 2000), no studies to date have examined hippocampal volume and asymmetry in adolescents who heavily use both alcohol and marijuana.
One critique of previous research is that hippocampal abnormalities may relate to risk-factors associated with substance use disorders, not to neurotoxic effects of substances. Consequently, this study sought to expand upon previous findings by statistically controlling for or excluding potential preexisting differences, within the limitations of a cross-sectional design, that may affect hippocampal morphometry such as comorbid psychiatric disorders, conduct disorder, or family history of substance use disorders (e.g., Tapert & Brown, 2000; Kruesi et al., 2004). Therefore, the purpose of the present study was to examine hippocampal volume and asymmetry in substance-using and demographically matched adolescents while controlling for potentially confounding factors. Specifically, we compared right and left hippocampal volumes and hippocampal asymmetry (right-left/right+left) in three adolescent groups aged 15–18: 1) alcohol users, 2) alcohol + marijuana users, and 3) non-substance using controls. Relationships between hippocampal morphometry, substance use severity, and verbal memory functioning were also examined.
2. METHODS
2.1 Participants
Adolescents aged 15–18 were recruited via distribution of flyers at local high schools, community colleges, and universities in the greater San Diego area. Flyers described an opportunity for participation in a brain imaging study and included brief eligibility, compensation, and contact information. Newspaper and Internet advertisements supplemented school-based recruitment.
Participants for this study were pooled from two larger projects examining the neural consequences of alcohol and marijuana use in adolescence (Nagel et al., 2005; Schweinsburg et al., 2005; Tapert et al., 2004). Due to high levels of concomitant alcohol and marijuana use during adolescence, we were unable to recruit a large enough group of adolescents who only used marijuana. Both studies were approved by the University of California, San Diego, Human Research Protection Program, and written/verbal consent and assent were obtained from each adolescent and their parent/legal guardian. All teens and parents/guardians were given an extensive screening interview to determine eligibility. Exclusionary criteria were: history of DSM-IV Axis I disorder (other than substance use disorder or conduct disorder due to high co-morbidity with substance use disorders); use of psychotropic medications or any other medication affecting the central nervous system; learning disability or mental retardation; head injury with loss of consciousness >2 minutes; serious medical or neurological problems (e.g. migraines, seizures); prenatal alcohol (maternal intake of ≥4 drinks/day or ≥7 drinks/week) or drug exposure; complicated or premature birth (<33 weeks gestation); parental history of bipolar I or psychotic disorders; left handedness; non-correctable vision or hearing problem; and any MRI contraindications (e.g., claustrophobia, current pregnancy, metal in body).
Eligible participants were classified in three groups based on pattern of substance use: (1) alcohol-only (ALC, n=16), who used alcohol but had limited marijuana experience (<40 lifetime uses; no MJ abuse/dependence diagnosis) or other substance use (≤ 25 lifetime uses); (2) marijuana+alcohol using (MJ+ALC, n=26), who used marijuana and alcohol but had limited other drug use (≤ 25 lifetime uses); (3) controls (n=21), with had limited experience with alcohol (<60 lifetime uses; no ALC abuse/dependence diagnosis) and no experience with any other substance. All participants were requested to abstain from any alcohol or other drug use for 2 days prior to the research session. Any teens unable to remain abstinent (as measured by urine toxicology screening, breathalyzer screening, self-report, and parent report) are not described in this report (see Procedures section).
2.2 Measures
2.2.1 Demographic and Psychiatric Assessment
Screening interviews were completed separately with each adolescent and their parent/guardian to assess for current and past psychiatric conditions and family substance use disorder and psychiatric history. Minor participants (<18 years) were administered the Computerized NIMH Diagnostic Interview Schedule for Children (C-DISC-4.0; Shaffer et al., 2000), and participants over 18 years old who lived independently received the complementary Computerized Diagnostic Interview Schedule (C-DIS-IV; Robins et al., 1996; Shaffer et al., 2000). Parallel modules of the above diagnostic measures assessed for major psychiatric disorders, including DSM-IV Axis I anxiety, mood, conduct, and psychotic disorders. To corroborate this information, parents/guardians (typically biological mothers) of minors were administered the complementary parent version of the DISC.
2.2.2 Alcohol and Substance Use
Current (past 3 month) and lifetime experiences with alcohol, nicotine, and other substances were collected using the Customary Drinking and Drug use Record, assessing DSM-IV abuse and dependence symptoms, symptoms of withdrawal, and substance-related adverse life events (Brown et al, 1998, Stewart and Brown, 1995). In addition, the Time-Line Followback (Sobell and Sobell, 1992) was administered to youth and parents, providing more detailed information in a calendar format about the type, quantity, and frequency of recent use for the past 30 days covering alcohol, marijuana, nicotine, stimulants (e.g., amphetamine, methamphetamine, MDMA/ecstasy, cocaine), opiates (e.g., heroin, Vicodin), hallucinogens, barbiturates, benzodiazepines, and misuse of other prescription and over-the-counter medications.
2.2.3 Cognitive Functioning
As part of a larger neuropsychological testing battery, participants were given the age-appropriate Vocabulary subtests from the Wechsler Intelligence Scales [Wechsler Intelligence Scale for Children-Third Edition (WISC-III; Wechsler, 1993), Wechsler Adult Intelligence Scale-Revised (WAIS-R; Wechsler, 1981), or Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999)], and the California Verbal Learning Test [Children’s Version (CVLT-C, Delis, 1994) or 2nd Edition (CVLT-II, Delis, 2000)]. CVLT-C and CVLT-II measure verbal learning and memory using word lists which include items drawn from semantic categories. The CVLT variables of interest in this study are trial 1 z-score and total recall (across trials 1–5) T-score. The CVLT was chosen because this task has been sensitive to verbal memory deficits in substance abusing populations (e.g., Medina et al., 2006; Medina et al., 2005; Tapert & Brown, 2000) and has been associated with temporal lobe/hippocampal activation (Johnson et al., 2001). All teens were also administered an estimate of premorbid intelligence reflecting quality of education (Wide Range Achievement Test, Reading subtest; Wilkinson, 1993).
2.3 Procedures
Trained research assistants administered screening interviews to adolescents and parents to assess eligibility. If eligible, prospective participants and their parent/guardians were individually administered a detailed interview assessing demographics, psychosocial functioning, and psychiatric history. To facilitate open and honest disclosure, confidentiality of provided information and toxicology results was ensured for youths and parents within ethical and legal guidelines (Winters et al., 1990). Data from adolescents with self-report of drug or alcohol use within two days, or positive urine toxicology screens (all drugs excluding THC) or breath samples (AlcoSensor IV, Intoximeter, Inc., St. Louis, MO) at the time of evaluation were not included in these analyses. Imaging sessions occurred on Thursday evenings to maximize recovery from weekend substance use and to minimize possible circadian influences. Parents and teens received financial compensation for participation upon completion of the study.
2.4 Image Processing
High-resolution MRI data were acquired on a 1.5 Tesla General Electric Signa LX system using a sagittally acquired inversion recovery prepared T1-weighted 3D spiral fast spin echo sequence (TR = 2000 ms, TE = 16 ms, FOV = 240 mm, voxel dimensions = 0.9375 x 0.9375 x 1.328 mm, 128 continuous slices, acquisition time = 8:36) (Wong, 2000). To obtain overall intracranial volume (ICV), a hybrid watershed and deformable surface semi-automated skull-stripping program, followed by manual editing, was utilized to remove non-brain materials from each T1-weighted 3D anatomical dataset (Segonne et al., 2004). All manual editing (ICV and hippocampal tracings) was performed in AFNI (Cox, 1996) by trained research assistants blind to participant characteristics who attained high levels of reliability (intraclass correlation coefficients >.90).
Hippocampal regions of interest were manually traced on contiguous 1.3 mm slices in the coronal plane through the structure (for additional details see Nagel et al., 2005). The stereotactic boundaries were as follows: anterior boundary began at the coronal slice through the fullest portion of the mammillary bodies; superior/lateral boundary was at the temporal horn and alveus; inferior boundary was at the white matter of the parahippocampal gyrus; medial boundary was at the ambient cistern; posterior boundary was where the columns of the fornix are visible. See Figure 1 for sample hippocampal delineation. Left and right hippocampal volumes were each analyzed as ratios to ICV to control for individual variability in brain size (Giedd et al., 1996). The hippocampal asymmetry variable was calculated by subtracting the left hippocampal (LH) volume from the right hippocampal (RH) volume and then diving this by their sum (RH-LH /RH+LH). Positive values reflect R>L and negative values reflect L>R hippocampal asymmetry.
Figure 1.
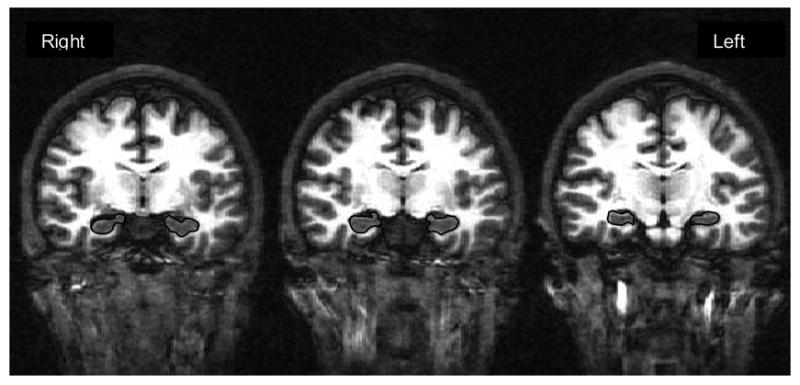
Examples (coronal view) of hippocampal boundary delineation.
2.5 Statistical Analysis
2.5.1. Demographic Information
All statistical analysis was conducted in SPSS 14.0. To explore any potential group differences, ANOVAs and chi-square tests were run to compare groups on important demographic variables such as age, gender composition, ethnic category, parental SES, family history of substance use disorders, prevalence of conduct disorder, verbal intellect, reading ability, and CVLT performance. Differences between the groups in frequency, duration, and severity of drug use and intracranial volumes were also analyzed. If necessary, post-hoc analysis utilizing Tukey’s HSD tests were utilized. Interpretations of statistical significance were made if p< .05.
2.5.2 Hippocampal Volume
In order to examine left and right hippocampal structure, a MANCOVA analyzed whether LH/ICV and RH/ICV volumes differed by group, gender, or conduct disorder diagnosis after controlling for ethnicity and age. To address the primary study aim, a 3X2 repeated measures ANCOVA (Raine et al., 2004; Suzuki et al., 2005) was run to assess whether substance use group (control, ALC users, MJ+ALC users), gender, or conduct disorder diagnosis predicted hippocampal asymmetry after controlling for ethnicity and age (which differed between groups). An interaction between group and gender was also explored. If necessary, post-hoc Tukey’s HSD tests were conducted and interpretations about statistical significance were made if p< .05.
2.5.3 Substance Use & Hippocampal Volume
As a post-hoc analysis, a multiple regression tested the relationship between alcohol and marijuana disorder severity (# of abuse/dependence criteria) and LH/ICV, RH/ICV, and hippocampal asymmetry ratio (RH-LH/RH+LH) after controlling for gender, conduct disorder diagnosis, age, and ethnicity (p< .05).
2.5.4 Hippocampal Volume & Verbal Learning
To evaluate the functional relationship between hippocampal asymmetry and verbal learning and memory, simple bivariate relationships (Pearson’s r) were examined between hippocampal asymmetry and CVLT one-trial learning and total recall, separately for each substance use group. For this preliminary analysis, to decrease Type II error and improve low power due to small n’s, interpretations about statistical significance were made if p< .10 (Cohen, 1988). In addition, Fisher’s z transformations were calculated to compare the magnitude of correlation coefficients between the groups.
3. RESULTS
3.1 Group Comparisons
3.1.1 Demographics/Cognitive Variables/Intracranial Volume
As shown in Table 1, the three groups did not significantly differ in gender composition [x2(2)=0.55, p<.76], family history of substance use disorders (none, mild, positive) [x2(3)=2.96, p<.56], verbal intellectual functioning [F(2,62)=1.15, p<.33], reading ability [F(2,62)=.48, p<.62], CVLT 1st trial performance [F(2,62)=.85, p<.43], CVLT total recall [F(2,62)=1.32, p<.28], parental SES (based on Hollingshead) [F(2,62)=1.15, p<.33], parental income [F(2,62)=0.44, p<.65], or intracranial volume [F(2,62)=1.19, p<.31]. The groups did significantly differ in age (range 15–18) [F(2,62)=3.28, p<.05], prevalence of conduct disorder [x2(2)=7.22, p<.03], and ethnic category [x2(8)=16.29, p<.04].
Table 1.
Demographic, Cognitive Function, Substance Use Characteristics, and Hippocampal Morphometry Information According to Drug Use Group.
| Controls (n=21) M (SD) or % [range] | Alcohol (n=16) M (SD) or % [range] | MJ+Alc (n=26) M (SD) or % [range] | |
|---|---|---|---|
| Age £ | 17.5 (1.1) [15.6 – 18.9] | 16.9 (0.7) [15.2 – 17.7] | 17.6 (0.9) [15.7 – 18.9] |
| % Female | 35% | 33% | 27% |
| % Caucasian£ | 65% | 100% | 85% |
| % Family history negative/mild/positive¥ | 62/10/28% | 43/32/25% | 48/24/28% |
| % Conduct disorder positive£ | 0% | 31% | 16% |
| Parent annual salary (thousands) | 130.3 (60.2) [35 – 275] | 146.3 (64.5) [55 – 280] | 125.8 (72.5) [8 – 275) |
|
| |||
| WRAT-3 Reading Standard Score | 104.6 (8.3) [85 – 116] | 106.6 (7.7) [90 – 120] | 106.5 (6.8) [88 – 116] |
| Vocabulary T-score a | 56.7 (8.6) [39 – 77] | 59.2 (6.4) [47 – 70] | 55.3 (8.5) [37 – 70] |
| CVLT 1st Trial z-score b | 0.0 (0.9) [−1.5 – 2.0] | 0.1 (0.9) [−1.0 – 2.0] | −0.2 (0.8) [−1.5 – 1.5] |
| CVLT Total Recall T-score b | 52.2 (9.1) [36 – 67] | 48.4 (7.1) [30 – 63] | 51.9 (6.9) [41 – 66] |
|
| |||
| Days since last drink * | 521.3 (447.8) [14 – 998] | 16.6 (14.4) [5 – 60] | 20.2 (12.7) [3 – 45] |
| Lifetime alcohol use episodes d,* | 7.9 (15.7) [0 – 57] | 133.6 (139.5) [14 – 505] | 152.3 (185.4) [11 – 900] |
| Drinks/month, past 3 months * | 1.0 (2.4) [0 – 10] | 40.8 (30.3) [3 – 108] | 45.2 (35.4) [4 – 180] |
| Alcohol abuse/dependence criteria, past 3 months e,* | 0.5 (0.2) [0 – 1] | 2.7 (1.6) [1 – 6] | 2.5 (2.2) [0 – 10] |
| Days since last marijuana use c,d,‡ | 951.9 (211.2) [30 – 998] | 419.9 (465.7) [12 – 998] | 31.4 (28.7) [2 – 120] |
| Lifetime marijuana use episodes d,*** | 2.2 (5.7) [0 – 20] | 11.9 (12.7) [0 – 40] | 402.3 (259.7) [60 – 998] |
| Marijuana use/month, past 3 months *** | 0.0 (0.0) | 0.8 (1.4) [0 – 5] | 14.2 (10.6) [1 – 30] |
| Marijuana abuse/dependence criteria, past 3 months e,** | 0.0 (0.0) | 0.9 (1.5) [0 – 4] | 2.2 (3.1) [0 – 12] |
| Smoked cigarettes, past month* | 4% | 50% | 50% |
| Cigarettes per smoking day c | 1.0 (0) [1] | 2.0 (1.7) [1 – 4] | 2.8 (3.0) [1 – 10] |
| Lifetime other drug use episodes *** | 0.0 (0.0) | 0.0 (0.0) | 3.5 (6.8) [0 – 25] |
|
| |||
| Intracranial Volume (ICV) (cc3) | 1566.8 (129.6) [1333 – 1733] | 1627.3 (114.1) [1430 – 1866] | 1569.8 (142.9) [1333 – 1799] |
| Left Hippocampal (LH) Volume (cc3) | 3.26 (0.43) [2.55 – 3.86] | 3.15 (0.36) [2.68 – 3.86] | 3.33 (0.34) [2.69 – 4.01] |
| Right Hippocampal (RH) Volume (cc3) | 3.07 (0.38) [2.48 – 3.56] | 3.17 (0.29) [2.79 – 3.67] | 3.15 (0.33) [2.60 – 3.76] |
| Hippocampal Asymmetry (RH-LH/RH+LH) | −0.0312 (0.0372) [−0.0959 – 0.0534] | 0.0033 (0.0432) [−0.1167 – 0.0551] | −0.0270 (0.0454) [−0.0828 – 0.0747] |
Full sample ANOVA or Chi-Square p<.05. (MJ+ALC differ in age from ALC, p<.10.).
Family history (FH) was calculated as Negative=no FH+ relatives; Mild=one FH+ 2nd degree relative or two FH+ 2nd degree relatives on different sides; Positive= one or more FH+ 1st degree relative or two FH+ 2nd degree relatives on the same side.
Converted T-scores based on Wechsler Intelligence Scale for Children-III (Wechsler, 1997), Wechsler Adult Intelligence Scale-III , or Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999).
Converted standard scores based on the California Verbal Learning Test-Children’s Version or the California Verbal Learning Test-2nd Edition (CVLT-C, Delis, 1994; CVLT-II, Delis, 2000).
Figures include only those who reported use.
The maximum allowed was 998.
Number of abuse/dependent symptoms do not necessarily indicate a positive DSM-IV diagnosis as symptoms may overlap within a criterion.
Post-hoc analysis reveal all groups significantly different (Tukey p < .05).
Post-hoc analysis reveal controls differ from other groups (Tukey p < .05).
Post-hoc analysis reveal controls differ from MJ+ALC teens only (Tukey p < .05).
Post-hoc analysis reveal MJ+ALC differ from other groups (Tukey p < .05).
3.1.2 Substance use
All participants were abstinent from all drugs and alcohol for at least 2 days. As shown in Table 1, user groups reported more recent alcohol and marijuana use than controls, as well as more lifetime alcohol use episodes, drinks per month (past 3 months), alcohol abuse/dependence symptoms, marijuana abuse/dependence symptoms, and likelihood of smoking cigarettes (p values <.05). Importantly, the ALC and MJ+ALC groups did not significantly differ on alcohol use variables or nicotine involvement. As expected, the MJ+ALC users reported more lifetime and past 3-month marijuana use episodes as well as lifetime other drug use, although the latter was relatively low (3.5 times, on average) (p values <.05).
3.2 Hippocampal Volumes
3.2.1 Left & Right Hippocampal Volumes
We examined group and gender differences in LH/ICV and RH/ICV after controlling for age, ethnic group, and conduct disorder. LH/ICV significantly differed between the groups [F(2,62)=3.3, p<.04, see Figure 2]. No LH/ICV gender differences [F(1,62)=1.2, p<.27], RH/ICV group [F(2,62)=1.1, p<.34] or gender differences [F(1,62)=1.1, p<.31] were found. Post-hoc analysis revealed that the ALC users demonstrated significantly smaller left hippocampal volumes compared to the MJ+ALC users (p<.04), but not the control group (p<.17).
Figure 2.
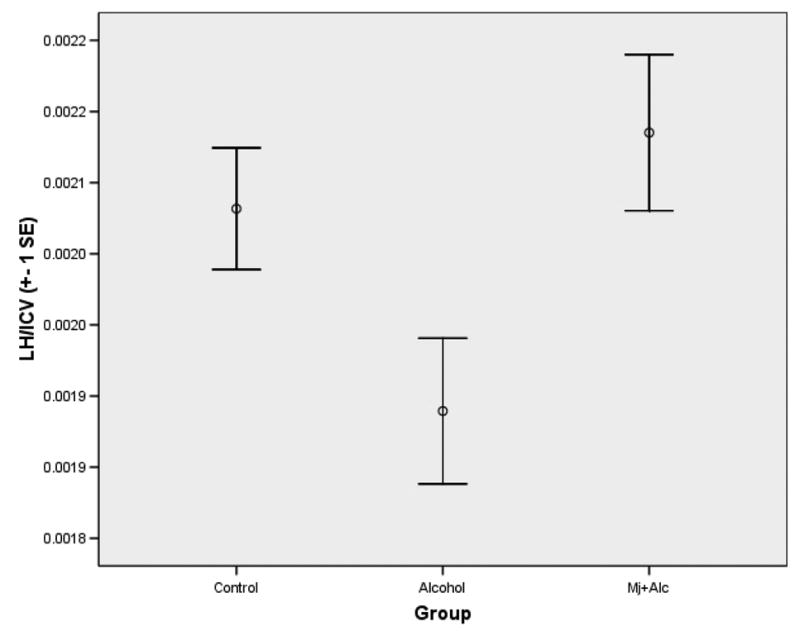
Means (± 1SE) of Left Hippocampal Volume/ICV According to Group
3.2.2 Hippocampal Asymmetry
To test the primary aim of the study, a 3 (group) X 2 (hippocampal hemisphere) repeated measures ANCOVA with gender and conduct disorder as additional independent variables and age and ethnic group as covariates was run. There was no main effect for hippocampal asymmetry [F(1,53)=.11, p<.75], but a significant asymmetry-by-group interaction [F(2,53)=3.24, p<.05] was found, indicating that ALC users had greater R>L hippocampal asymmetry than controls and MJ+ALC users (see Figure 3). No significant hippocampal asymmetry-by-gender interaction [F(1,53)=0.004, p<.95], hippocampal asymmetry-by-gender-by-group interaction [F(2,53)=2.30, p<.11], or hippocampal asymmetry-by-conduct disorder interaction [F(1,53)=2.02, p<.16] was found. (See Table 1 for hippocampal volumes and asymmetry values according to group.)
Figure 3. Means (± 1SE) of Hippocampal Asymmetry (RH-LH /RH+LH) by Group.
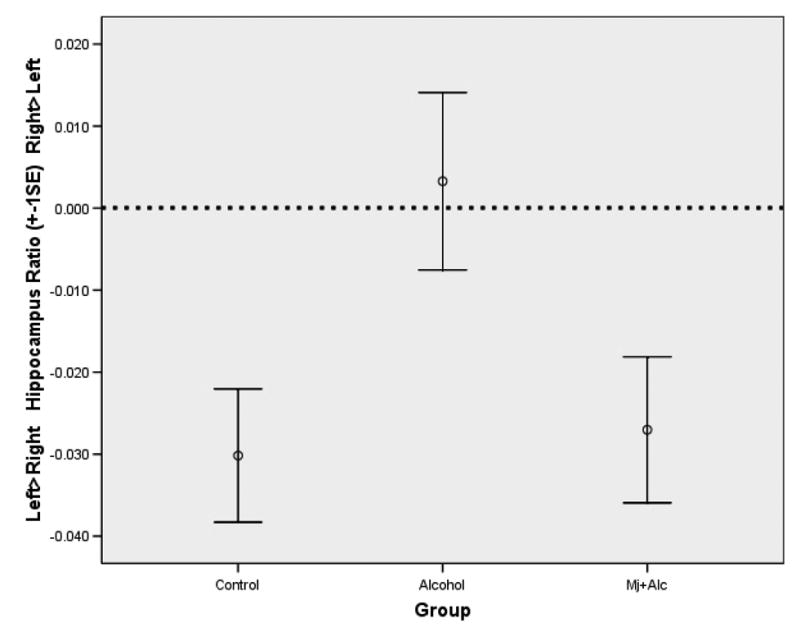
(Note: positive values indicate R>L hippocampal volumes, while negative values indicate L>R.)
3.3 Substance Use & Hippocampal Volume
To assess the relationships between substance use severity (# abuse/dependence symptoms met) and hippocampal morphometry, ordinary least squares multiple regressions were run (N = 63) with the following dependent variables: hippocampal asymmetry (RH–LH /RH+LH), LH/ICV, and RH/ICV. Independent variables were the number of alcohol and marijuana abuse/dependence symptoms endorsed. Covariates were gender, conduct disorder status, ethnic group, and age. After controlling for these covariates, increased alcohol abuse/dependence symptoms were associated with more R>L hippocampal asymmetry [beta =.52, p < .006]. The opposite was found for increased marijuana abuse/dependence symptoms, which were associated with more L>R hippocampal asymmetry [beta = −.40, p < .02]. Smaller left hippocampal volumes (LH/ICV) were associated with more alcohol abuse/dependence symptoms [beta = −.55, p < .004] and fewer marijuana abuse/dependence symptoms [beta = .51, p < .003]. None of the covariates were associated with the hippocampal variables, and abuse/dependence symptoms did not predict right hippocampal volume.
3.4 Hippocampal Volume & Verbal Learning
Table 2 shows correlations between hippocampal variables and CVLT one-trial learning and total recall (standardized scores) as well as Fisher z transformations utilized to compare correlation coefficients between the groups. Among the hippocampal measures, asymmetry was the most robust predictor of verbal memory performance among the healthy non-using control adolescents (p<.06). The controls demonstrated a stronger relationship between hippocampal asymmetry and CVLT trial 1 performance compared to the ALC-users (p<.04) and marginally stronger relationship compared to the MJ+ALC users (p<.09). Controls also demonstrated a stronger relationship between hippocampal asymmetry and CVLT total recall compared to the MJ+ALC group (p < .05). No relationships between LH/ICV, RH/ICV, or asymmetry and memory performance were found among ALC or MJ+ALC using adolescents. Figure 4 displays the bivariate scatterplot between hippocampal asymmetry and CVLT one-trial learning by group.
Table 2.
Bivariate Relationships Between Hippocampal Volumes and California Verbal Learning Test Performance by Group
| LH/ICV | RH/ICV | Hippocampal Asymmetry Ratio | |
| Controls | |||
| CVLT 1st Trial | −.13 | .22 | .42 ± |
| CVLT Total Recall | −.29 | −.02 | .33 |
| ALC Users | |||
| CVLT 1st Trial | −.09 | −.24 | −.20 |
| CVLT Total Recall | −.01 | .18 | .23 |
| MJ+ALC Users | |||
| CVLT 1st Trial | −.10 | −.10 | .004 |
| CVLT Total Recall | .01 | −.09 | −.16 |
| Fisher’s z-score | |||
| LH/ICV | RH/ICV | Hippocampal Asymmetry Ratio | |
| Controls vs. ALC (1st Trial) | −0.11 | 1.29 | 1.75* |
| Controls vs. ALC (Total Recall) | −0.79 | −0.55 | 0.30 |
| Controls vs. MJ+ALC (1st Trial) | −0.10 | 1.03 | 1.37** |
| Controls vs. MJ+ALC (Total Recall) | −0.98 | 0.22 | 1.60* |
| ALC vs. MJ+ALC (1st Trial) | 0.55 | −0.42 | −0.60 |
| ALC vs. MJ+ALC (Total Recall) | −0.06 | 0.78 | 1.14 |
p<.06
p<.10,
p<.05.
Notes: Pearson product moment correlations run separately by group: controls (n=21), alcohol users (n=16), marijuana+alcohol users (n=26). Fisher’s converted z-score measures the differences between correlation coefficients. LH= Left hippocampal volume. RH= Right hippocampal volume. ICV= Intracranial volume. Hippocampal asymmetry was calculated as RH-LH/RH+LH; positive values denote R>L and negative values reflect L>R. CVLT= California Verbal Learning Test (Children’s Version or 2nd Edition) standard score.
Figure 4.
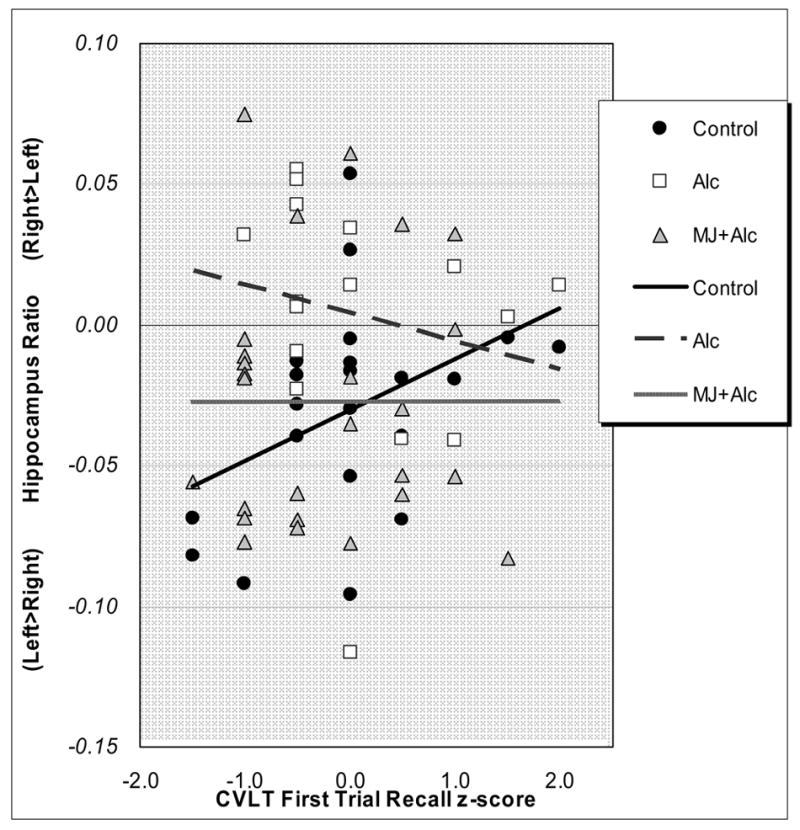
Bivariate Scatterplot Between California Verbal Learning Test (CVLT) Trial 1 (Z-Score) and Hippocampal Asymmetry (RH-LH/RH+LH) According to Group.
4. DISCUSSION
Converging lines of evidence suggest that adolescents are at increased risk for neurocognitive consequences of alcohol and marijuana use. Further, animal, neuroimaging, and neuropsychological data suggest that the hippocampus is particularly sensitive to drug and alcohol neurotoxicity. The present study was designed to examine hippocampal asymmetry, as well as right and left hippocampal volume, among adolescent alcohol (ALC) users, marijuana and alcohol (MJ+ALC) users, and demographically matched healthy controls. The primary findings revealed that adolescent ALC users demonstrated more right>left (R>L) asymmetry than non-using controls and MJ+ALC using teens. This was primarily driven by smaller left hippocampal volumes among alcohol users.
This study did not find R>L asymmetry in the healthy adolescents, which is in conflict with two previous findings (Giedd et al., 1996; Suzuki et al., 2005). However, adolescents the age of our sample (15–18) were not assessed in the latter study (Suzuki et al., 2005), and the former study (Giedd et al., 1996) examined a sample substantially younger (ages 4–18) than the current sample. Visual inspection of the published scatterplots within the age range of 15–18 reveal that males in the study appear to demonstrate symmetrical hippocampal volumes, and R>L asymmetry was found primarily among the females (Giedd et al., 1996). Therefore, the current study findings may have been driven by our higher proportion of males compared to females (65% vs. 35%), and limited power to examine gender effects.
Interestingly, we did observe that more R>L asymmetry was associated with improved verbal learning only among the non-substance using control adolescents in this sample. These results may be driven by individual differences in neuromaturation, which would be consistent with previous findings that smaller left hippocampal volumes are associated with improved verbal memory during adolescence (Foster et al., 1999). Perhaps most importantly, these results highlight the need for further studies specifically examining gender and hippocampal development during the critical period of adolescence.
Expanding on previous findings of reduced hippocampal volumes among adolescent alcohol users (Nagel et al., 2005), we found that R>L asymmetry was significantly associated with alcohol abuse/dependence severity, even after controlling for gender, conduct disorder, ethnic category, and age. Further, compared to controls, ALC users demonstrated a significantly weaker correlation between hippocampal asymmetry and verbal learning. Therefore, in this sample of alcohol-using adolescents, smaller left hippocampal volumes and greater R>L asymmetry likely indicates a small degree of pathological processes, such as alcohol-related neuronal death or atrophy (e.g., Melis et al., 1996), as opposed to normal pruning. There are several possible reasons why left, but not right, hippocampal differences were found among adolescent ALC users. Given that other studies have found reduced left hippocampal and amygdale, but not right, volumes associated with other pathological processes (e.g., Chen et al., 2004; Saylam et al., 2006), there may be neurotoxic or pre-existing developmental trajectory differences between the hemispheres that account for these differences. For example, left versus right hippocampi may differ in drug effects due to gene expression or neurotransmitter receptor discrepancies (e.g., Mostal et al., 2006).
In contrast to the alcohol findings, greater marijuana abuse/dependence severity was associated with larger left hippocampal volumes and greater L>R asymmetry, although as a group MJ+ALC users did not differ from controls in hippocampal asymmetry or volume. Several possible scenarios explain these findings. One possibility is that marijuana use could be neuroprotective in combination with alcohol use. Indeed, among adults, simultaneous use of cannabidiol and alcohol actually reduces blood alcohol levels (Consroe et al., 1979). However, this hypothesis is in conflict with our finding that the MJ+ALC-using adolescents demonstrated significantly weaker correlations between hippocampal asymmetry and verbal learning compared to control adolescents. It is possible that the concomitant use of both substances may create opposing mechanisms so that macromorphometric variables do not differ from those of controls. Microstructural hippocampal changes related to marijuana use may include increased glial proliferation and white matter density as well as reduced gray matter density (Chan et al., 1998; Matochik et al., 1995), which could result in relatively normal hippocampal volumes among MJ+ALC teens despite functional pathology. Alternatively, heavy adolescent marijuana use could subtly interfere with synaptic pruning processes, resulting in larger gray matter volumes, particularly in the left hippocampus. Of course, additional longitudinal studies examining hippocampal morphometry and function among adolescents who use combined MJ+ALC and MJ alone are necessary to test these competing hypotheses.
Some potential limitations warrant consideration. Although comparable to other published neuroimaging studies, the alcohol use group included fewer participants than the other two groups, reducing power to detect bivariate relationships in this group. Further, results may not generalize to substance users with different patterns of use or lengths of abstinence. Without a marijuana-only group, it is difficult to disentangle the effects of alcohol vs. marijuana use alone. It is also possible that the methods to measure the hippocampal volumes could have influenced the measure of asymmetry. By using stereotactic methods to define the anterior hippocampal boundary (the mammillary bodies), the left hippocampus may have been artificially larger than the right because the right hemisphere is typically slightly more anterior compared to the left (Thompson et al., 2005). Although this would not have affected group difference results, it may have slightly underestimated R>L asymmetry for all participants. Lastly, due to the cross-sectional nature of this study, the directional and developmental relationship of hippocampal asymmetry and substance use cannot be clearly ascertained. Although statistically controlled, the groups differed in the frequency of conduct disorder, with more substance-using adolescents meeting criteria. However, there were no group differences in other premorbid variables or risk factors associated with substance use such as family history of substance use disorders, parental SES, verbal intellectual functioning, reading ability, and education. Still, it remains possible that the observed hippocampal differences may be due to preexisting individual differences, and longitudinal studies are required to further examine hippocampal asymmetry in both healthy and substance-using adolescents.
In summary, the present study found that adolescent heavy drinkers demonstrated a significantly different pattern of hippocampal asymmetry compared to marijuana+alcohol users and non-substance using controls. Further, results indicate that the functional relationship between hippocampal asymmetry and verbal learning was abnormal among adolescent alcohol and marijuana+alcohol users compared to healthy controls. Finally, these results highlight the need for additional animal and human research examining the potential interaction of heavy marijuana and alcohol use on neurocognitive functioning, especially among adolescent populations.
Acknowledgments
We would like to express our appreciation to the research participants and their families, the research associates in the Laboratory of Cognitive Imaging (LOCI) in the Department of Psychiatry, UCSD, and the LOCI IT team. Funding was provided by grants from the National Institute on Drug Abuse (PI: Tapert, R21 DA15228 and R01 DA021182; PI: Medina, F32 DA020206), the National Institute on Alcohol Abuse and Alcoholism (PI: Tapert, R21 AA12519 and R01 AA13419), and the UCSD Fellowship in Biological Psychiatry and Neuroscience (Nagel, Cohen-Zion).
Footnotes
Publisher's Disclaimer: This is a PDF le of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its nal citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aasly J, Storsaeter O, Nilsen G, Smevik O, Rinck P. Minor structural brain changes in young drug abusers. Acta Neurologica Scandinavica. 1993;87:210–214. doi: 10.1111/j.1600-0404.1993.tb04103.x. [DOI] [PubMed] [Google Scholar]
- Agosti V, Edward N, Frances L. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse. 2002;28(4):643–652. doi: 10.1081/ada-120015873. [DOI] [PubMed] [Google Scholar]
- Barnes J, Scahill RI, Schott JM, Frost C, Rossor MN, Fox NC. Does Alzheimer's disease affect hippocampal asymmetry: Evidence from a cross-sectional and longitudinal volumetric MRI study. Dementia and Geriatric Cognitive Disorders. 2004;19:338–344. doi: 10.1159/000084560. [DOI] [PubMed] [Google Scholar]
- Barron S, White A, Swartzwelder HS, Bell RL, Rodd ZA, Slawecki CJ, Ehler CL, Levin ED, Rezvani AH, Spear LP. Adolescent vulnerabilities to chronic alcohol or nicotine exposure: findings from rodent models. Alcohol Clin Exp Res. 2005;29(9):1720–1725. doi: 10.1097/01.alc.0000179220.79356.e5. [DOI] [PubMed] [Google Scholar]
- Belue RC, Howlett AC, Westlake TM, Hutchings DE. The ontogeny of cannabinoid receptors in the brain of postnatal and aging rats. Neurotoxicol Teratol. 1995;17(1):25–30. doi: 10.1016/0892-0362(94)00053-g. [DOI] [PubMed] [Google Scholar]
- Benes FM, Turtle M, Khan Y, Farol P. Myelination of a key relay zone in the hippocampal formation occurs in the human brain during childhood, adolescence, and adulthood. Arch Gen Psychiatry. 1994;51:477–484. doi: 10.1001/archpsyc.1994.03950060041004. [DOI] [PubMed] [Google Scholar]
- Belgrave BE, Bird KD, Chesher GB, Jackson DM, Lubbe KE, Starmer GA, Teo RK. The effect of (−) trans-delta9-tetrahydrocannabinol, alone and in combination with ethanol, on human performance. Psychopharmacology (Berl) 1979a;62:53–60. doi: 10.1007/BF00426035. [DOI] [PubMed] [Google Scholar]
- Belgrave BE, Bird KD, Chesher GB, Jackson DM, Lubbe KE, Starmer GA, Teo RK. The effect of cannabidiol, alone and in combination with ethanol, on human performance. Psychopharmacology (Berl) 1979b;64:243–246. doi: 10.1007/BF00496070. [DOI] [PubMed] [Google Scholar]
- Bhatia S, Bookheimer SY, Gaillard WD, Theodore WH. Measurement of whole temporal lobe and hippocampus for MR volumetry: Normative data. Neurology. 1993;43:2006–2010. doi: 10.1212/wnl.43.10.2006. [DOI] [PubMed] [Google Scholar]
- Block RI, O'Leary DS, Hichwa RD, Augustinack JC, Boles Ponto LL, Ghoneim MM, Arndt S, Hurtig RR, Watkins GL, Hall JA, Nathan PE, Andreasen NC. Effects of frequent marijuana use on memory related regional cerebral blood flow. Pharmacol Biochem Behav. 2002;72(1–2):237–250. doi: 10.1016/s0091-3057(01)00771-7. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol 1998. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tapert SF, Granholm E, Delis DC. Neurocognitive functioning of adolescents: Effects of protracted alcohol use. Alcoholism: Clinical and Experimental Research. 2000;24:164–171. [PubMed] [Google Scholar]
- Button TMM, Rhee SH, Hewitt JK, Young SE, Corley RP, Stallings MC. The role of conduct disorder in explaining the comorbidity between alcohol and illicit drug dependence in adolescence. Drug and Alcohol Dependence. 2006 doi: 10.1016/j.drugalcdep.2006.07.012. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Carlson G, Wang Y, Alger BE. Endocannabinoids facilitate the induction of LTP in the hippocampus. Nat Neurosci. 2002;5(8):723–724. doi: 10.1038/nn879. [DOI] [PubMed] [Google Scholar]
- Carta G, Nava F, Gessa GL. Inhibition of hippocampal acetylcholine release after acute and repeated Δ9- tetrahydrocannabinol in rats. Brain Research. 1998;809:1–4. doi: 10.1016/s0006-8993(98)00738-0. [DOI] [PubMed] [Google Scholar]
- Cha YM, White AM, Kuhn CM, Wilson WA, Swartzwelder HS. Differential effects of delta(9)-THC on learning in adolescent and adult rats. Pharmacol Biochem Behav. 2006;83(3):448–455. doi: 10.1016/j.pbb.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Chait LD, Perry JL. Acute and residual effects of alcohol and marijuana, alone and in combination, on mood and performance. Psychopharmacology. 1994;115:340–349. doi: 10.1007/BF02245075. [DOI] [PubMed] [Google Scholar]
- Chan GC, Hinds TR, Impey S, Storm DR. Hippocampal neurotoxicity of Delta9-tetrahydrocannabinol. J Neurosci. 1998;18(14):5322–5332. doi: 10.1523/JNEUROSCI.18-14-05322.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen BK, Sassi R, Axelson D, Hatch JP, Sanches M, Nicoletti M, Brambilla P, Keshavan MS, Ryan ND, Birmaher B, Soares JC. Cross-sectional study of abnormal amygdala development in adolescents and young adults with bipolar disorder. Biological Psychiatry. 2004;56(6):399–405. doi: 10.1016/j.biopsych.2004.06.024. [DOI] [PubMed] [Google Scholar]
- Chesterman LP, Taylor PJ, Cox T, Hill M. Multiple measures of cerebral state in dangerous mentally disordered inpatients. Crim Behav Ment Health. 1994;4:228–239. [Google Scholar]
- Childers SR, Breivogel CS. Cannabis and endogenous cannabinoid systems. Drug and Alcohol Dependence. 1998;51:173–187. doi: 10.1016/s0376-8716(98)00075-1. [DOI] [PubMed] [Google Scholar]
- Crews FT, Braun CJ, Hoplight B, Switzer RC, 3rd, Knapp DJ. Binge ethanol consumption causes differential brain damage in young adolescent rats compared with adult rats. Alcoholism, Clinical and Experimental Research. 2000;24(11):1712–1723. [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Lawrence Erlbaum Associates; Hillsdale, New Jersey: 1988. [Google Scholar]
- Consroe P, Carlini EA, Zwicker AP, Lacerda LA. Interaction of cannabidiol and alcohol in humans. Psychopharmacology (Berl) 1979;66(1):45–50. doi: 10.1007/BF00431988. [DOI] [PubMed] [Google Scholar]
- Cox RW. AFNI: Software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research. 1996;29:162–173. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- Diamond MC, Johnson RE, Young D, Singh SS. Age-related morphologic differences in the rat cerebral cortex and hippocampus: Male-female; right-left. Experimental Neurology. 1983;81:1–13. doi: 10.1016/0014-4886(83)90153-x. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Clark DB, Beers SR, Soloff PH, Boring AM, Hall J, Kersh A, Keshavan MS. Hippocampal volume in adolescent-onset alcohol use disorders. American Journal of Psychiatry. 2000;157(5):737–744. doi: 10.1176/appi.ajp.157.5.737. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Narasimhan A, Thatcher DL, Keshavan MS, Soloff P, Clark DB. Prefrontal cortex, thalamus and cerebellar volumes in adolescents and young adults with adolescent onset alcohol use disorders and co-morbid mental disorders. Alcoholism: Clinical and Experimental Research. 2005 doi: 10.1097/01.alc.0000179368.87886.76. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. Manual for the California Verbal Learning Test-Children's Version. San Antonio, Texas: The Psychological Corporation; 1994. [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test-Second Edition. San Antonio, Texas: The Psychological Corporation; 2001. [Google Scholar]
- Duka T, Townshend JM, Collier K, Stephens DN. Impairment in cognitive functions after multiple detoxifications in alcoholic inpatients. Alcohol Clin Exp Res. 2003;27 (10):1563–1572. doi: 10.1097/01.ALC.0000090142.11260.D7. [DOI] [PubMed] [Google Scholar]
- Ehrenreich H, Rinn T, Kunert HJ, Moeller MR, Poser W, Schilling L, Gigerenzer G, Hoehe MR. Specific attentional dysfunction in adults following early start of cannabis use. Psychopharmacology. 1999;142(3):295–301. doi: 10.1007/s002130050892. [DOI] [PubMed] [Google Scholar]
- Eichenbaum H. The hippocampus and mechanisms of declarative memory. Behavioral Brn Research. 1999;103(2):123–133. doi: 10.1016/s0166-4328(99)00044-3. [DOI] [PubMed] [Google Scholar]
- Estruch R, Nicolás JM, Salamero M, Aragón C, Sacanella E, Fernández-Solà J, Urbano-Márquez A. Atrophy of the corpus callosum in chronic alcoholism. Journal of the Neurological Sciences. 1997;146:145–151. doi: 10.1016/s0022-510x(96)00298-5. [DOI] [PubMed] [Google Scholar]
- Foster JK, Meikle A, Goodson G, Mayes AR, Howard M, Sunram SI, Cezayirli E, Roberts N. The hippocampus and delayed recall: bigger is not necessarily better? Memory. 1999;7(5–6):715–732. doi: 10.1080/096582199387823. [DOI] [PubMed] [Google Scholar]
- Gansler DA, Harris GJ, Oscar Berman M, Streeter C, Lewis RF, Ahmed I, Achong D. Hypoperfusion of inferior frontal brain regions in abstinent alcoholics: a pilot SPECT study. J Stud Alcohol. 2000;61(1):32–37. doi: 10.15288/jsa.2000.61.32. [DOI] [PubMed] [Google Scholar]
- Garland MA, Parsons OA, Nixon SJ. Visual spatial learning in nonalcoholic young adults with and those without a family history of alcoholism. J Stud Alcohol. 1993;54 (2):219–224. doi: 10.15288/jsa.1993.54.219. [DOI] [PubMed] [Google Scholar]
- Geroldi C, Laakso MP, DeCarli C, Beltramello A, Bianchetti A, Soininen H, Trabucchi M, Frisoni GB. Apolioprotein E genotype and hippocampal asymmetry in Alzheimer's disease: a volumetric MRI study. J Neurol Neurosurg Psychiatry. 2000;68:93–96. doi: 10.1136/jnnp.68.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghozland S, Aguado F, Espinosa-Parrilla JF, Soriano E, Maldonado R. Spontaneous network activity of cerebellar granule neurons: impairment by in vivo chronic cannabinoid administration. European Journal of Neuroscience. 2002;16:641–651. doi: 10.1046/j.1460-9568.2002.02112.x. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Mezzich AC, Tarter RE. Disruptive, delinquent and aggressive behavior in female adolescents with a psychoactive substance use disorder: Relation to executive cognitive functioning. Journal of Studies on Alcohol. 1998;59:560–567. doi: 10.15288/jsa.1998.59.560. [DOI] [PubMed] [Google Scholar]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann N Y Acad Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Snell JW, Lange N, Rajapakse JC, Casey BJ, Kozuch PL, Vaituzis AC, Vauss YC, Hamburger SD, Kaysen D, Rapoport JL. Quantitative magnetic resonance imaging of human brain development: ages 4–18. Cereb Cortex. 1996;6(4):551–560. doi: 10.1093/cercor/6.4.551. [DOI] [PubMed] [Google Scholar]
- Grant I, Gonzalez R, Carey CL, Natarajan L, Wolfson T. Non acute (residual) neurocognitive effects of cannabis use: a meta analytic study. J Int Neuropsychol Soc. 2003;9(5):679–689. doi: 10.1017/S1355617703950016. [DOI] [PubMed] [Google Scholar]
- Gruber SA, Yurgelun-Todd DA. Neuroimaging of marijuana smokers during inhibitory processing: A pilot investigation. Cognitive Brain Research. Special Issue: Multiple Perspectives on Decision Making. 2005;(1):107–118. doi: 10.1016/j.cogbrainres.2005.02.016. [DOI] [PubMed] [Google Scholar]
- Hoffman AF, Lupica CR. Mechanisms of cannabinoid inhibition of GABA(A) synaptic transmission in the hippocampus. J Neurosci. 2000;20(7):2470–2479. doi: 10.1523/JNEUROSCI.20-07-02470.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollstedt C, Olsson O, Rydberg U. Effects of ethanol on the developing rat. II. Coordination as measured by the tilting plane test. Med Biol. 1980;58(3):164–168. [PubMed] [Google Scholar]
- Hommer D, Momenan R, Rawlings R, Ragan P, Williams W, Rio D, Eckardt M. Decreased corpus callosum size among alcoholic women. Arch Neurol. 1996;43:359–363. doi: 10.1001/archneur.1996.00550040099019. [DOI] [PubMed] [Google Scholar]
- Huttenlocher PR. Morphometric study of human cerebral cortex development. Neuropsychologia. 1990;28:517–527. doi: 10.1016/0028-3932(90)90031-i. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Mencl WE, Westerveld M, Pugh KR. Impact of cannabis use on brain function in adolescents. Ann N Y Acad Sci. 2004;1021:384–390. doi: 10.1196/annals.1308.053. [DOI] [PubMed] [Google Scholar]
- Jernigan T, Gamst A. Changes in volume with age: Consistency and interpretation of observed effects. Neurobiol Aging. 2005;26(9):1271–1274. doi: 10.1016/j.neurobiolaging.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use, 1975–2004. Vol. 1. Bethesda, MD: National Institute on Drug Abuse; 2005. Secondary school students (NIH Publication No. 05-5727) [Google Scholar]
- Johnson SC, Saykin AJ, Flashman LA, McAllister TW, Sparling MB. Brain activation on fMRI and verbal memory ability: functional neuroanatomic correlates of CVLT performance. J Int Neuropsychol Soc. 2001;7(1):55–62. doi: 10.1017/s135561770171106x. [DOI] [PubMed] [Google Scholar]
- Kanayama G, Rogowska J, Pope HG, Gruber SA, Yurgelun Todd DA. Spatial working memory in heavy cannabis users: A functional magnetic resonance imaging study. Psychopharmacology. 2004;176(3–4):239–247. doi: 10.1007/s00213-004-1885-8. [DOI] [PubMed] [Google Scholar]
- Kawakami R, Shinohara Y, Kato Y, Sugiyama H, Shigemoto R, Ito I. Asymmetrical allocation of NMDA receptor ε2 subunits in hippocampal circuitry. Science. 2003;300:990–994. doi: 10.1126/science.1082609. [DOI] [PubMed] [Google Scholar]
- Kim D, Thayer SA. Cannabinoids inhibit the formation of new synapses between hippocampal neurons in culture. J Neurosci. 2001;21(RC146):1–5. doi: 10.1523/JNEUROSCI.21-10-j0004.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Lee JM, Kim HP, Jang DP, Shin YW, Ha TH, Kim JJ, Kim IY, Kwon JS, Kim SI. Asymmetry analysis of deformable hippocampal model using the principal component in schizophrenia. Human Brain Mapping. 2005;25:361–369. doi: 10.1002/hbm.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kril JJ, Halliday GM, Svoboda MD, Cartwright H. The cerebral cortex is damaged in chronic alcoholics. Neuroscience. 1997;79(4):983–998. doi: 10.1016/s0306-4522(97)00083-3. [DOI] [PubMed] [Google Scholar]
- Kruesi MJ, Casanova MF, Mannheim G, Johnson-Bilder A. Reduced temporal lobe volume in early onset conduct disorder. Psychiatry Research: Neuroimaging. 2004;132(1):1–11. doi: 10.1016/j.pscychresns.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Laakso MP, Vaurio O, Savolainen L, Repo E, Soininen H, Aronen HJ, Tiihonen J. A volumetric MRI study of the hippocampus in type 1 and 2 alcoholism. Behav Brain Res. 2000;109(2):177–186. doi: 10.1016/s0166-4328(99)00172-2. [DOI] [PubMed] [Google Scholar]
- Landfield PW, Cadwallader LB, Vinsant S. Quantitative changes in hippocampal structure following long-term exposure to delta 9-tetrahydrocannabinol: possible mediation by glucocorticoid systems. Brain Res. 1988;443(1–2):47–62. doi: 10.1016/0006-8993(88)91597-1. [DOI] [PubMed] [Google Scholar]
- Liguori A, Gatto CP, Jarrett DB. Separate and combined effects of marijuana and alcohol on mood, equilibrium, and simulated driving. Psychopharmacology. 2002;163:399–405. doi: 10.1007/s00213-002-1124-0. [DOI] [PubMed] [Google Scholar]
- Little PJ, Kuhn CM, Wilson WA, Swartzwelder HS. Differential effects of ethanol in adolescent and adult rats. Alcohol Clin Exp Res. 1996;20(8):1346–1351. doi: 10.1111/j.1530-0277.1996.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Martin CS, Kaczynski NA, Maisto SA, Tarter RE. Polydrug use in adolescent drinkers with and without DSM-IV alcohol abuse and dependence. Alcoholism: Clinical and Experimental Research. 1996;20(6):1099–1108. doi: 10.1111/j.1530-0277.1996.tb01953.x. [DOI] [PubMed] [Google Scholar]
- Matochik JA, Eldreth DA, Cadet JL, Bolla KI. Altered brain tissue composition in heavy marijuana users. Drug Alcohol Depend. 2005;77(1):23–30. doi: 10.1016/j.drugalcdep.2004.06.011. [DOI] [PubMed] [Google Scholar]
- Medina KL, Shear PK, Corcoran K. Ecstasy (MDMA) exposure and neuropsychological functioning: A polydrug perspective. Journal of the International Neuropsychological Society. 2005;11(6):1–13. doi: 10.1017/S1355617705050915. [DOI] [PubMed] [Google Scholar]
- Medina KL, Shear PK, Schafer J. Memory functioning in polysubstance dependent women. Drug and Alcohol Dependence. 2006;84(3):248–55. doi: 10.1016/j.drugalcdep.2006.02.009. [DOI] [PubMed] [Google Scholar]
- Melis F, Stancampiano R, Imperato A, Carta G, Fadda F. Chronic ethanol consumption in rats: correlation between memory performance and hippocampal acetylcholine release in vivo. Neuroscience. 1996;74(1):155–159. doi: 10.1016/0306-4522(96)00109-1. [DOI] [PubMed] [Google Scholar]
- Monti PM, Miranda R, Nixon K, Sher KJ, Swartzwelder HS, Tapert SF, White A, Crews FT. Adolescence: booze, brains, and behavior. Alcohol Clin Exp Res. 2005;29(2):207–220. doi: 10.1097/01.alc.0000153551.11000.f3. [DOI] [PubMed] [Google Scholar]
- Mostal JR, Kroes RA, Otto NJ, Rahimi O, Claiborne BJ. Distinct patterns of gene expression in the left and right hippocampal formation of developing rats. Hippocampus. 2006;16:629–634. doi: 10.1002/hipo.20198. [DOI] [PubMed] [Google Scholar]
- Nagel BJ, Schweinsburg AD, Phan V, Tapert SF. Reduced hippocampal volume among adolescents with alcohol use disorders without psychiatric comorbidity. Psychiatry Research. 2005;139(3):181–190. doi: 10.1016/j.pscychresns.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel BJ, Medina KL, Yoshii J, Schweinsburg AD, Moadab I, Tapert SF. Age related changes in prefrontal white matter volume across adolescence. NeuroReport. 2006;17(13):1427–31. doi: 10.1097/01.wnr.0000233099.97784.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedraza O, Bowers D, Gilmore R. Asymmetry of the hippocampus and amygdala in MRI volumetric measures of normal adults. J Int Neuropsychol Soc. 2004;10:664–678. doi: 10.1017/S1355617704105080. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Lim K, Desmond J, Sullivan E. Thinning of the corpus callosum in older alcoholic men: A magnetic resonance imaging study. Alcohol Clin Exp Res. 1996;20:752–757. doi: 10.1111/j.1530-0277.1996.tb01682.x. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Mathalon DH, Sullivan EV, Rawles JM, Zipursky RB, Lim KO. A quantitative magnetic resonance imaging study of changes in brain morphology from infancy to late adulthood. Arch Neurol. 1994;51(9):874–887. doi: 10.1001/archneur.1994.00540210046012. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Hegehus M, Adalsteinsson E, Lim KL, Moseley M. In vivo detection and functional correlates of white matter microstructural disruption in chronic alcoholism. Alcoholism: Clinical and Experimental Research. 2000;24:1214–1221. [PubMed] [Google Scholar]
- Phillips SC, Harper CG, Kril J. A quantitative histological study of the cerebellar vermis in alcoholic patients. Brain. 1987;110(Pt 2):301–314. doi: 10.1093/brain/110.2.301. [DOI] [PubMed] [Google Scholar]
- Pillay SS, Rogowska J, Kanayama G, Jon DI, Gruber S, Simpson N, Cherayil M, Pope HG, Yurgelun Todd DA. Neurophysiology of motor function following cannabis discontinuation in chronic cannabis smokers: An fMRI study. Drug Alcohol Depend. 2004;76(3):261–271. doi: 10.1016/j.drugalcdep.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Pope HG, Gruber AJ, Hudson JI, Cohane G, Huestis MA, Yurgelun-Todd D. Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug and Alcohol Dependence. 2003;69(3):303–310. doi: 10.1016/s0376-8716(02)00334-4. [DOI] [PubMed] [Google Scholar]
- Pope HG, Gruber AJ, Hudson JI, Huestis MA, Yurgelun Todd D. Neuropsychological performance in long term cannabis users. Arch Gen Psychiatry. 2001;58(10):909–915. doi: 10.1001/archpsyc.58.10.909. [DOI] [PubMed] [Google Scholar]
- Pope HGJ, Yurgelun Todd D. The residual cognitive effects of heavy marijuana use in college students. JAMA. 1996;275(7):521–527. [PubMed] [Google Scholar]
- Pyapali GK, Turner DA, Wilson WA, Swartzwelder HS. Age and dose dependent effects of ethanol on the induction of hippocampal long term potentiation. Alcohol. 1999;19(2):107–111. doi: 10.1016/s0741-8329(99)00021-x. [DOI] [PubMed] [Google Scholar]
- Raine A, Ishikawa SS, Arce E, Lencz T, Knuth KH, Bihrle S, LaCasse L, Colletti P. Hippocampal structural asymmetry in unsuccessful psychopaths. Biol Psychiatry. 2004;55:185–191. doi: 10.1016/s0006-3223(03)00727-3. [DOI] [PubMed] [Google Scholar]
- Raz N, Gunning-Dixon F, Head D, Rodrigue K, Williamson A, Acker JD. Aging, sexual dimorphism, and hemispheric asymmetry of the cerebral cortex: replicability of regional differences in volume. Neurobiol of Aging. 2004;25:377–396. doi: 10.1016/S0197-4580(03)00118-0. [DOI] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, Compton W. The Diagnostic Interview Schedule, Version 4.0 (DIS 4.0) St. Louis, MO: Washington University; 1996. [Google Scholar]
- Romero J, Garcia L, Fernandez-Ruiz JJ, Cebeira J, Ramos JA. Changes in rat brain cannabinoid binding sites after acute or chronic exposure to their endogenous agaonist, anandamide, or to Δ9- Tetrahydrocannabinol. Pharmacology Biochemistry and Behaviora. 1995;51(4):731–737. doi: 10.1016/0091-3057(95)00023-p. [DOI] [PubMed] [Google Scholar]
- Rourke S. Neuropsychological assessment of neuropsychiatric disorders. 2. 1996. Neurobehavioral correlates of alcoholism; pp. 423–485. [Google Scholar]
- Rubino T, Patrini G, Perenti M, Massi P, Paroloro D. Chronic treatment with a synthetic cannabinoid CP-55,940 alters G-protein expression in the rat central nervous system. Molecular Brain Research. 1997;44:191–197. [PubMed] [Google Scholar]
- SAMHSA. Results from the 2003 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, DHHS; 2004. [Google Scholar]
- Saylam C, Ucerler H, Kitis O, Ozand E, Gonul AS. Reduced hippocampal volume in drug-free depressed patients. Surg Radiol Anat. 2006;28(1):82–7. doi: 10.1007/s00276-005-0050-3. [DOI] [PubMed] [Google Scholar]
- Schneider M, Koch M. Chronic pubertal but not adult chronic cannabinoid treatment impairs sensorimotor gating, recognition memory and performance in a progressive ratio task in adult rats. Neuropsychopharm. 2003;28:1760–1790. doi: 10.1038/sj.npp.1300225. [DOI] [PubMed] [Google Scholar]
- Schwartz RH, Gruenewald PJ, Klitzner M, Fedio P. Short-term memory impairment in cannabis-dependent adolescents. American Journal of Diseases in Children. 1989;143(10):1214–1219. doi: 10.1001/archpedi.1989.02150220110030. [DOI] [PubMed] [Google Scholar]
- Schweinsburg AD, Schweinsburg BC, Cheung EH, Brown GG, Brown SA, Tapert SF. fMRI response to spatial working memory in adolescents with comorbid marijuana and alcohol use disorders. Drug & Alcohol Dependence. 2005;79:201–210. doi: 10.1016/j.drugalcdep.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott RC, King MD, Gadian DG, Neville BGR, Connelly A. Hippocampal abnormalities after prolonged febrile convulsion: a longitudinal MRI study. Brain. 2003;126(I):2551–2557. doi: 10.1093/brain/awg262. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliablility of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Silveri MM, Spear LP. Decreased sensitivity to the hypnotic effects of ethanol early in ontogeny. Alcohol Clin Exp Res. 1998;22(3):670–676. doi: 10.1111/j.1530-0277.1998.tb04310.x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Raye Z, Litten JPA, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Humana Press, Inc; Totowa, NJ, US: 1992. [Google Scholar]
- Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post adolescent brain maturation in frontal and striatal regions. Nature Neuroscience. 1999;2(10):859–861. doi: 10.1038/13154. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Trauner DA, Gamst A, Jernigan TL. Development of cortical and subcortical brain structures in childhood and adolescence: a structural MRI study. Dev Med Child Neurol. 2002;44(1):4–16. doi: 10.1017/s0012162201001591. [DOI] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews. 2000;24:417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Squire LR. Memory and the hippocampus: a synthesis from findings with rats, monkeys, and humans. Psychol Rev. 1992;99(2):195–231. doi: 10.1037/0033-295x.99.2.195. [DOI] [PubMed] [Google Scholar]
- Stewart DG, Brown SA. Withdrawal and dependency symptoms among adolescent alcohol and drug abusers. Addiction 1995. 1995;90:627–635. doi: 10.1046/j.1360-0443.1995.9056274.x. [DOI] [PubMed] [Google Scholar]
- Stiglick A, Kalant H. Learning impairment in the radial arm maze following prolonged cannabis treatment in rats. Psychopharmacology. 1982;77(2):117–123. doi: 10.1007/BF00431932. [DOI] [PubMed] [Google Scholar]
- Stiglick A, Kalant H. Residual effects of chronic cannabis treatment on behavior in mature rats. Psychopharmacology. 1985;85(4):436–439. doi: 10.1007/BF00429660. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Deshmukh A, De Rosa E, Rosenbloom MJ, Pfefferbaum A. Striatal and forebrain nuclei volumes: Contribution to motor function and working memory deficits in alcoholism. Biological Psychiatry. 2005;57:768–776. doi: 10.1016/j.biopsych.2004.12.012. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Fama R, Rosenbloom MJ, Pfefferbaum A. A profile of neuropsychological deficits in alcoholic women. Neuropsychology. 2002;16(1):74–83. doi: 10.1037//0894-4105.16.1.74. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Marsh L, Mathalon DH, Lim KO, Pfefferbaum A. Anterior hippocampal volume deficits in nonamnesic, aging chronic alcoholics. Alcohol Clin Exp Res. 1995;19(1):110–122. doi: 10.1111/j.1530-0277.1995.tb01478.x. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Rosenbloom MJ, Pfefferbaum A. Pattern of motor and cognitive deficits in detoxified alcoholic men. Alcoholism: Clinical and Experimental Research. 2000;24 (5):611–621. [PubMed] [Google Scholar]
- Suzuki M, Hagino H, Nohara S, Zhou SY, Kawasaki Y, Takahashi T, Matsui M, Seto H, Ono T, Kurachi M. Male-specific volume expansion of the human hippocampus during adolescence. Cerebral Cortex. 2005;15:187–193. doi: 10.1093/cercor/bhh121. [DOI] [PubMed] [Google Scholar]
- Swartzwelder HS, Richardson RC, Markwiese-Foerch B, Wilson WA, Little PJ. Developmental differences in the acquisition of tolerance to ethanol. Alcohol. 1998;15 (4):311–314. doi: 10.1016/s0741-8329(97)00135-3. [DOI] [PubMed] [Google Scholar]
- Swartzwelder HS, Wilson WA, Tayyeb MI. Age-dependent inhibition of long-term potentiation by ethanol in immature versus mature hippocampus. Alcoholism, Clinical and Experimental Research. 1995;19(6):1480–1485. doi: 10.1111/j.1530-0277.1995.tb01011.x. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown SA. Neuropsychological correlates of adolescent substance abuse: Four year outcomes. J Int Neuropsychol Soc. 1999;5(6):481–493. doi: 10.1017/s1355617799566010. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown SA. Substance dependence, family history of alcohol dependence, and neuropsychological functioning in adolescence. Addiction. 2000;95:1043–1053. doi: 10.1046/j.1360-0443.2000.95710436.x. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Granholm E, Leedy NG, Brown SA. Substance use and withdrawal: Neuropsychological functioning over 8 years in youth. J Int Neuropsychol Soc. 2002;8(7):873–883. doi: 10.1017/s1355617702870011. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Schweinsburg AD, Barlett VC, Brown SA, Frank LR, Brown GG, Meloy MJ. Blood oxygen level dependent response and spatial working memory in adolescents with alcohol use disorders. Alcohol Clin Exp Res. 2004;28(10):1577–1586. doi: 10.1097/01.alc.0000141812.81234.a6. [DOI] [PubMed] [Google Scholar]
- Thompson PM, Sowell ER, Gogtay N, Giedd JN, Vidal CN, Hayashi KM, Leow A, Nicolson R, Rapoport JL, Toga AW. Structural MRI and brain development. Int Rev Neurobiol. 2005;67:285–323. doi: 10.1016/S0074-7742(05)67009-2. [DOI] [PubMed] [Google Scholar]
- Townshend JM, Duka T. Binge drinking, cognitive performance and mood in a population of young social drinkers. Alcohol Clin Exp Res. 2005;29(3):317–325. doi: 10.1097/01.alc.0000156453.05028.f5. [DOI] [PubMed] [Google Scholar]
- Varlinskaya EI, Spear LP. Differences in the social consequences of ethanol emerge during the course of adolescence in rats: social facilitation, social inhibition, and anxiolysis. Dev Psychobiol. 2006;48(2):146–161. doi: 10.1002/dev.20124. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Manual for the Wechsler Adult Intelligence Scale-Revised. The Psych Corp; San Antonio, TX: 1981. [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children-III. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. The Psych Corp; San Antonio, TX: 1999. [Google Scholar]
- White AM, Bae JG, Truesdale MC, Ahmad S, Wilson WA, Swartzwelder HS. Chronic-intermittent ethanol exposure during adolescence prevents normal developmental changes in sensitivity to ethanol-induced motor impairments. Alcohol Clin Exp Res. 2002;26(7):960–968. doi: 10.1097/01.ALC.0000021334.47130.F9. [DOI] [PubMed] [Google Scholar]
- White AM, Ghia AJ, Levin ED, Swartzwelder HS. Binge pattern ethanol exposure in adolescent and adult rats: differential impact on subsequent responsiveness to ethanol. Alcoholism, Clinical and Experimental Research. 2000;24(8):1251–1256. [PubMed] [Google Scholar]
- Wilkinson G. (WRAT-3) Manual. 3. Wilmington, DE: Wide Range, Inc; 1993. Wide Range Achievement Test. [Google Scholar]
- Wilson W, Mathew R, Turkington T, Hawk T, Coleman RE, Provenzale J. Brain morphological changes and early marijuana use: a magnetic resonance and positron emission tomography study. J Addict Dis. 2000;19(1):1–22. doi: 10.1300/J069v19n01_01. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD, Henly GA, Schwartz RH. Validity of adolescent self-report of alcohol and other drug involvement. International Journal of the Addictions. 1990;25:1379–1395. doi: 10.3109/10826089009068469. [DOI] [PubMed] [Google Scholar]
- Wong EC, Luh WM, Buxton RB, Frank RL. Single slab high resolution 3D whole brain imaging using spiral FSE. Proceedings of the International Society of Magnetic Resonance Medicine. 2000;8:683. [Google Scholar]
- Yttri EA, Burk JA, Hunt PS. Intermittent ethanol exposure in adolescent rats: dose dependent impairments in trace conditioning. Alcohol Clin Exp Res. 2004;28(10):1433–1436. doi: 10.1097/01.alc.0000147657.51745.a7. [DOI] [PubMed] [Google Scholar]
- Zaidel DW, Esiri MM, Harrison PJ. The hippocampus in schizophrenia: lateralized increase in neuronal density and altered cytoarchitectural asymmetry. Psychological Medicine. 1997;27:703–713. doi: 10.1017/s0033291796004618. [DOI] [PubMed] [Google Scholar]


