Abstract
Background
Shared decision making (SDM) involves patients and doctors contributing as partners to treatment decisions. It is not known whether or to what extent SDM contributes to the welfare arising from a consultation, and how important this contribution is relative to other attributes of a consultation.
Aim
To identify patient preferences for SDM relative to other utility bearing attributes of a consultation.
Design of study
In parallel with a randomised trial in training GPs in SDM competencies and risk communication skills, a discrete choice experiment exercise was conducted to assess patients' utilities.
Setting
Twenty general practices in South Wales, UK
Method
Five hundred and eighty-four responders from 747 patients attending the randomised trial (response rate = 78%). All patients had one of four conditions (atrial fibrillation, menorrhagia, menopausal symptoms or prostatism) and attended a consultation with a doctor in their own practice. Patients were randomised to attend a consultation either with a doctor who had received no training in the study or risk communication training alone or SDM training alone, or both combined.
Results
Five key utility bearing attributes of a consultation were identified. All significantly influenced patient's choice of preferred consultation style (P<0.001). Larger increases in utility were associated with changes on ‘doctor listens’ attribute, followed by easily understood information, a shared treatment decision, more information and longer consultation. Utilities were influenced by whether the doctor had received risk communication training alone or SDM training alone, or both combined, prior to the consultations. The randomised trial itself had identified that the communication processes of these consultations changed significantly, with greater patient involvement in decision making, after the training interventions.
Conclusion
Shared treatment decisions were valued less than some other attributes of a consultation. However, patient utilities for such involvement appeared responsive to changes in experiences of consultations. This suggests that SDM may gain greater value among patients once they have experienced it.
Keywords: communication, consultation, discrete choice experiment, patient's ulitity, risk, shared decision making
INTRODUCTION
Evidence of the benefits of greater patient involvement in healthcare decision making is inconsistent.1,2 While some cognitive and affective outcomes can be improved, health gain is usually unaffected.3 This suggests that patient preferences ought to play a major role in determining levels of patent involvement. Shared decision making (SDM) is a consultation model in which patient and professional contribute as partners to the final decision on treatment.4 The extent to which patients want to be involved in treatment decisions and how important they regard such involvement relative to other consultation characteristics remains largely unknown. In health economics, consultations are understood as seeking to maximise patients' welfare (utility).5 Thus, it is important to understand how such utility is generated.
As patients normally have imperfect information,6 they depend on doctors to assist them in their treatment decisions (‘power asymmetry’).7 This doctor–patient relationship has been modelled within the economic theory of ‘agency’8 which at one extreme (paternalism) has the agent (doctor) taking decisions on behalf of the patient. A perfect agent will take the same decision the patient would have taken if he or she had the doctor's medical knowledge, but this requires the doctor to have information on the patient's preferences6 as well as their health. At the other extreme is the informed choice model where the doctor provides information that the patient combines with his or her own preferences to take a decision.4
Gafni et al6 have argued that neither of these models reflects the realities of clinical practice. SDM describes a middle ground where information is exchanged and the nature of the decisional agency negotiated, allowing both patient and professional to decide their degrees of preferred influence on the process.9 SDM also requires the doctor to communicate effectively the treatment options and then portrays the risks and benefits of each option, that is, risk communication.10
There is some evidence to suggest that individuals can vary in the extent to which they wish to be involved in decisions about their health care.2 Previous economic analyses have suggested that patients may experience dis-utility from being involved in such decisions.11 Moreover, actual and preferred degrees of involvement could be context dependent, varying according to the nature, severity and chronicity of their condition.12
The aim of this article is to explore patient preferences using a discrete choice experiment to identify patients' utilities for key characteristics of a ‘successful’ consultation. In particular, we sought to assess if patients' utilities are constant, or whether they change as a result of having experienced a consultation with a doctor who has been trained in SDM, in risk communication or both.
METHOD
The study
An explanatory cluster randomised crossover trial was carried out which involved training GPs in the use of risk communication tools (information aids including numerical formats and charts), SDM competencies, or both. Patients with one of four chronic conditions (menorrhagia, atrial fibrillation, menopausal symptoms or prostatism) were invited by their GP to attend a ‘review consultation’ to discuss their continuing treatment. Decisions taken at these consultations related to previously diagnosed conditions with which the patients were familiar and may have already experienced treatment.
The study was in three phases.13 Twenty GPs from 20 different practices in Gwent, South Wales, UK, were recruited and consenting patients from their practices were invited to review consultations within one of three study phases (Figure 1). Each doctor would consult 48 patients: 12 in phase 1 (pre-training = control group), 24 in phase 2 where half the doctors are trained in risk communication and half trained in SDM, and 12 in phase 3 where all doctors receive the training they did not receive in phase 2 and were thus all now trained in both. The trial assessed the resulting effects on the doctor–patient interaction (level of SDM in consultations14), patient outcomes (SF-12)15 and satisfaction with the decision taken.12 Results of these aspects of the trial are available elsewhere.16,17 Briefly, training produced statistically and clinically significant changes in the process of consultations although patient-based outcomes showed no significant effects. All patients who attended the review consultation were eligible for the discrete choice experiment (Figure 2).
Figure 1.
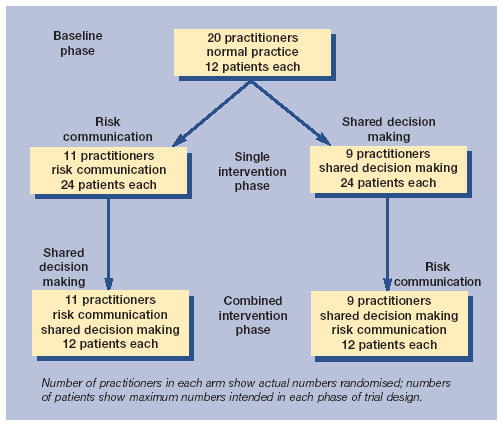
Randomised trial design with crossover.
Figure 2.
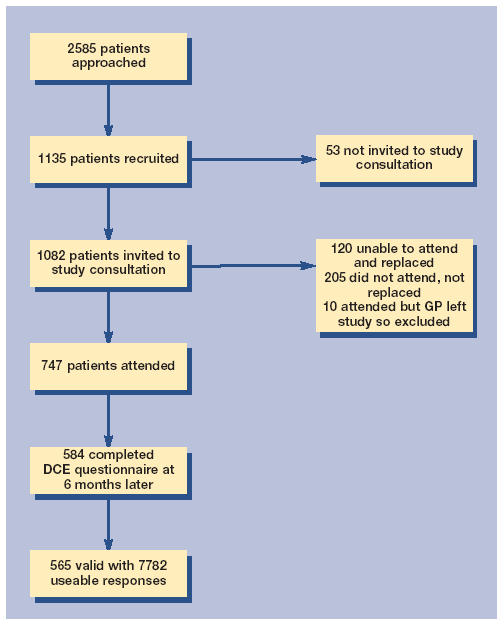
Flow of patients.
The discrete choice experiment
Developed in the early 1980s, discrete choice experiments are increasingly being used by health economists to elicit patient preferences for different forms of healthcare delivery.18 Conventional economic theory asserts that consumers gain ‘utility’ (satisfaction) from consuming goods and services. One formulation of this theory asserts that goods and services can be described in terms of their utility bearing characteristics (attributes) and consumers demand those goods and services whose variations in attributes provide the highest utility.19 In the context of a GP consultation, the relevant (that is, utility bearing) attributes can include the length of the consultation, whether the doctor listens and so on.
How this fits in
Shared decision making (SDM) is widely advocated by health policy makers. This study shows that patients do value this approach, but not as much as other key attributes of consultations such as having a doctor who listens and being provided with easily understood information. In a randomised controlled comparison, the importance that patients attach to SDM increased among the patients who had experienced this approach. This suggests that SDM may gain greater acceptance among patients more widely once they have experienced it.
Discrete choice experiments involves asking patients to choose between pairs of scenarios that differ in terms of these consultation attributes. For example the attribute ‘who makes the treatment decision’ could be described in one scenario including the option ‘doctor decides’ and in the other the option ‘patient decides’. Such stated preference techniques are favoured in health economic analyses because they are grounded in utility theory (responders choose the alternative which give them the highest utility) and they simulate the types of decisions that individuals are accustomed to making in everyday life.20 The five stages of a discrete choice experiment are described below.
Identify attributes. Literature reviews on SDM and risk communication21,22 were used to identify key characteristics of a ‘successful’ consultation (Table 1). ‘Doctor listens’ implies patients want to transmit information to the doctor;23 ‘amount of information’ implies that information from the doctor is valued; ‘information easy to understand’ reflects the doctor's ability to explain health problems and alternative treatments; ‘who chooses your treatment’ reflects the patient's wish to be involved in the decision process;9 and ‘consultation length’ measures patients' preferences for more time with the doctor.
Table 1.
Attributes and options included in the discrete choice experiments.
| Attributes | Options | Coding | |
|---|---|---|---|
| A) Doctor listens: | 1. Doctor does not seem to listen | 0 | |
| 2. Doctor seems to listen | 1 | ||
| B) Amount of information about your health problem and its treatment | 1. A small amount | 0 | 0 |
| 2. A moderate amount | 1 | 0 | |
| 3. A large amount | 0 | 1 | |
| C) How easily the information is understood: | 1. Difficult to understand | 0 | |
| 2. Easy to understand | 1 | ||
| D) Who chooses the treatment: | 1. Doctor chooses | 0 | 0 |
| 2. You choose | 1 | 0 | |
| 3. Both choose | 0 | 1 | |
| E) Length of consultation: | 1. Less than 10 minutes | 0 | |
| 2. More than 10 minutes | 1 | ||
Choosing options for each attribute. The term ‘option’ is used here to reflect the ways that each attribute is described, that is, how the attribute varies. To retain the realistic nature of the comparison between scenarios it is important that the way that the options are described to reflect realistic choices (for example; doctor, patient, both for the attribute ‘who chooses your treatment’). These were informed by the literature reviews (Table 1).
Presenting scenarios. All possible combinations of attributes and options produces 72 scenarios (three attributes with two options plus two attributes with three options = 32 × 23 = 72, the full factorial design). However, evidence shows that responders usually manage between nine and 16 comparisons before losing interest.24 A sub-sample of 27 scenarios was deemed feasible while allowing enough degrees of freedom to perform the required analysis. This gave a relative theoretical D-efficiency of 0.32 compared to the full factorial design, and 1.43 compared to an orthogonal 1/6 fractional design.25
Within discrete choice experiments, one scenario is used in every choice (constant) and all others compared with it. Although the constant can be selected randomly,26 the scenario judged to most closely reflect current practice was chosen as the constant. A scenario assumed to be unambiguously of lower utility24 (‘worst’ scenario) was composed of ‘doctor does not listen’, ‘a small amount of information’, ‘information difficult to understand’, ‘doctor chooses’ and ‘less than 10 minutes’. This was used to assess if responders were making rational choices, such as choosing scenarios yielding more utility over those yielding less. Also, a scenario considered to hold highest utility (‘best’ scenario) was selected (mainly for statistical purposes). It was composed of ‘doctor listens’, ‘a large amount of information’, ‘information easy to understand’, ‘both choose’ and ‘more than 10 minutes’. This is a subjective judgement and responders can legitimately (that is, rationally) have different views of best and worst. In addition to these, 24 other scenarios were chosen to ensure balance between options as well as ‘utility balance’.27
To avoid overburdening patients, two questionnaires were developed. Each included comparison of the constant with ‘best’ and ‘worst’ scenarios with the remaining 24 comparisons randomly divided between the two. Thus, each patient was presented with 14 pair-wise choices; Table 2 shows one pair-wise choice. The scenario on the left represent the constant scenario (that is, current practice) as indicated by the GPs in the research group.
Table 2.
Example of pairwise choice choice used for the discrete choice experiments.
| CHOICE 5 | Scenario Aa | Scenario B |
|---|---|---|
| Doctor listens | Doctor seems to listen | Doctor seems to listen |
| Amount of information about your health problem and its treatment | A moderate amount | A moderate amount |
| How easily the information is understood | Easy to understand | Easy to understand |
| Who chooses the treatment | Doctor chooses | Both choose |
| Length of consultation | Less than 10 minutes | More than 10 minutes |
| What kind of visit would you prefer? (tick one box only) | Prefer visit A ▭ | or Prefer visit B ▭ |
Current practice (used as constant scenario).
The questionnaires explained the aim of the exercises and gave a brief description of the consultation attributes and options attached to them. A ranking exercise, where patients were asked to rank the attributes independently of the scenarios was included. In addition to the pair-wise choices, a series of questions was included to assess the patient's experience at the last consultation, their degree of difficulty in completing the questionnaire (likert scale) and to estimate the time taken to complete the questionnaire.
Administering and piloting the questionnaire. The questionnaire was sent by post to all study patients 6 months after attending the review consultation to allow time for reflection. Reminders were sent to non-responders 2 and 4 weeks after first mailing. The first 72 questionnaires were used for piloting.
Data analysis. Responders and non-responders were compared on the basis of demographic data, clinical condition and SF-12 collected at the review consultation. Patients who always chose the constant scenario were compared with the rest on demographic and clinical variables.
The discrete choice experiment was analysed with a multilevel logistic regression model28,29 using MlWin software. This takes into account correlations at practice level (level 3), individual (level 2) and the multiple responses from within each individual (level 1). The dependent variable was the probability that a patient included the attributes options including whether the doctor had been trained in risk communication, SDM or both, would choose the alternative scenario. The explanatory variables included the attributes and whether the doctor had been trained in risk communication, SDM or both. Dummy variables were used for attributes with three options to avoid assuming that the changes between attributes options were ordinal and that, for instance, little to moderate amount of information gives the same utility gain as moderate to large amounts of information. The main effects in the model described above show the importance that patients place on changing different attribute options of a consultation. To explore whether these remain stable as patients experience consultations with doctors who had been trained, interactions between the attributes and training were examined. It should be noted that patients were randomly allocated to consultations with doctors who had or had not been trained in risk communication, SDM or both and not to a consultation which followed any prescribed model. Nevertheless, within the trial, provision of each form of training significantly increased the level of patient involvement in treatment decisions,14 which suggests that the processes of these consultations were significantly different than in the baseline phase of the trial and specifically manifesting patient involvement competences.
RESULTS
Pilot
Forty of 72 questionnaires were returned (response rate = 58.3%). The only change suggested by the pilot was to alternately place the constant scenario on the right and left side of the paired comparisons on one questionnaire to assess whether patients would become accustomed to seeing the same option on one side and choose it without considering the alternative.
Main study
Five hundred and eighty-four of the 747 questionnaires (including pilot) were returned (response rate = 78%). Data from the pilot was included because the final questionnaire was unchanged. Only 5 responders chose the worst scenario over a better alternative — evidence of irrational economic behaviour24 — and 14 answered only one pair-wise choice. These 19 were excluded from the analysis. Responders and non-responders were comparable (Table 3).
Table 3.
Comparison of respondents versus non-responders.
| Variables | Questionnaires returned (n = 565) | Questionnaires not returned (n = 182) | P-value |
|---|---|---|---|
| Mean age in years (SD) | 59 (10.66) n = 515 | 58.6 (12.65) n = 173 | 0.666a |
| Condition (%) | 0.35b | ||
| Prostatism | 147 (26) | 53 (29) | |
| Atrial fibrillation | 110 (19) | 35 (19) | |
| Menorrhagia | 99 (18) | 39 (21) | |
| Menopausal symptoms | 206 (37) | 58 (31) | |
| Age center school (SD) | 15.7 (1.20) n = 504 | 15.5 (1.20) n = 127 | 0.132a |
| SF12 Physical score (SD) | 42.06 (12.34) n = 470 | 42.45 (12.97) n = 144 | 0.74 |
| SF12 Mental score (SD) | 49.74 (10.53) n = 470 | 48.08 (11.88) n = 144 | 0.108 |
Independent t-test
χ2 test. n refers to usable data for each variable, from 565 returned questionnaires or available data from non-responders. SD = standard deviation.
The questionnaire took on average 15 (SD = 12.1) minutes to complete. Sixty-four per cent found it easy or very easy and 8% difficult or very difficult. There were no differences between the two versions.
One hundred and nine responders (19.3%) always chose the constant scenario over the alternatives, suggesting that many patients have dominant preferences, that is, they were satisfied with what was considered ‘normal practice’. Table 4 compares the two groups.
Table 4.
Comparison of those always choosing the constant scenario versus those whose choices varied.
| Variables | Choice of preferred scenario varied (n = 456) | Always chose constant scenario (n = 109) | P-value |
|---|---|---|---|
| Age; mean (SD) | 57.6 (10.73) n = 418 | 64.8 (8.12) n = 97 | <0.001a |
| Condition (%) | |||
| Prostatism | 103 (23) | 44 (40) | <0.001b |
| Atrial fibrillation | 78 (17) | 32 (29) | |
| Menorrhagia | 93 (20) | 6 (6) | |
| Menopausal symptoms | 179 (40) | 27 (25) | |
| Age left school (SD) | 15.8 (1.2) n = 404 | 15.3 (1.1) n = 100 | <.001a |
| Mean SF12 Physical score (SD) | 42.5 (12.4) n = 378 | 40.1 (12.0) n = 92 | 0.09a |
| Mean SF12 Mental score (SD) | 49.0 (10.7) n = 378 | 52.7 (9.3) n = 92 | 0.003a |
| Type of questionnaire (%) | 0.338b | ||
| Constant scenario changes | 218 (48) | 58 (53) | |
| Constant scenario always on left | 238 (52) | 51 (48) | |
Independent t-test
χ2 test. n refers to usable data for each variable, from 565 returned questionnaires. SD = standard deviation.
Younger (P<0.001) and more educated (P<0.001) patients were more inclined to choose alternatives that differ from current practice. The significance of condition (Table 3) reflects the high correlation between condition and age. There was also a significant difference with respect to mental health (P = 0.003) but not physical health. Those with poorer mental health had a higher tendency to choose alternative scenarios. The position of the constant scenario had no effect suggesting that responders had read the questionnaires.
The 565 questionnaires provided 7782 useable responses. Results of the 3 level logistic model are presented in Table 5, which shows that scenarios involving more of any attribute option increased the probability of choosing the alternative scenarios over current practice, that is, they are associated with higher utility.
Table 5.
Multilevel regression of attributes and study variables on choice made.
| Attributes | B | SE | P-value |
|---|---|---|---|
| Does the doctor listen? | 2.63 | 0.22 | <0.001 |
| How easy is the information to understand? | 2.30 | 0.17 | <0.001 |
| Who chooses your treatment? | |||
| Doctor | 0 | Ref | <0.001 |
| You | 0.10 | 0.13 | |
| Both | 1.38 | 0.12 | |
| Amount of information given | |||
| Small | 0 | Ref | <0.001 |
| Moderate | 0.98 | 0.13 | |
| Large | 1.11 | 0.12 | |
| Length of consultation | 1.05 | 0.10 | <0.001 |
| Training | |||
| RC | 0.56 | 0.32 | 0.08 |
| SDM | −0.609 | 0.33 | 0.063 |
| Interactions | |||
| RC*Doctor listens | −0.18 | 0.26 | 0.486 |
| SDM*Doctor listens | 0.53 | 0.26 | 0.045 |
| RC*Information easy to understand | −0.61 | 0.19 | 0.002 |
| SDM*Information easy to understand | 0.23 | 0.19 | 0.239 |
| Constant terms | −7.24 | ||
| N | 7782 | ||
The B and SE of the level 2 - constant and level 1 - constant were respectively 2.84 (0.24) and 0.89 (0.01). RC = risk communication. SE = standard error. SDM = shared decision making.
Comparison of each attribute's coefficient (B) shows the ordering of the relative importance of a change in option. For each, the extent to which the doctor listens is the most important determinant of improvements in utility, closely followed by information which is easy to understand. Having a shared decision, amount of information and length of consultation were also important but less than the former two attributes.
It is possible that the nature of the review consultation influenced preferences. For example, a patient who experienced a consultation with a doctor trained in risk communication might have different preferences from someone who never experienced such a consultation. The main effects of either form of training are not significant. However, they are kept in the model to explore the interactions.
The interactions show the extent to which the utilities identified in the main effects model are stable. While the strength of this evidence again suggests caution in interpretation, Table 5 shows the presence of interactions between training and the attributes ‘doctor listens’ and ‘information easy to understand’. The positive interaction between SDM and ‘doctor listens’ (0.53) shows that SDM exposure increases the importance of having a listening doctor, but again the overall order of importance of attributes is not changed. The negative interaction between risk communication and ‘information easy to understand’ (−0.61) shows that risk communication exposure decreases the importance of this attribute option. That is, once trained in risk communication, having ‘information easy to understand’ becomes less important to their patients who are now more willing to trade it in exchange for different options of other attributes. This is slightly counter-intuitive and may suggest that the discussions doctors were having with patients covering risks were unhelpful or, alternatively, may reflect that effective risk communication is only the platform for the deeper competencies of SDM.10 Once discussion of risk information has taken place, patients may have focused on, and derived more utility from, the wider aspects of the consultation.
DISCUSSION
Summary of main findings
This study has used a discreet choice experiment to explore the importance that patients place on different attributes options of a consultation (main effects of multilevel model) and whether these remain stable as patients experience different styles of consultation (interactions). It has shown that while all attributes identified from the literature review were significant, having a doctor who listens and who gives information which is easy to understand give greater increases in utility than changing options of other attributes.
The low coefficient for the attribute option ‘you choose’ (0.10) suggests that there is little difference between the paternalistic and informed choice models, that is, there is little extra utility gained from patients making informed choices.12 A consultation in which the patient contributes but does not have sole responsibility for the decision (the SDM model), however, was shown to yield greater utility than either extreme type of consultation.
The interactions (Table 5) showed that for certain attributes training seems to have moderated utilities. It is reasonable to assume that baseline preferences between groups were similar (due to randomisation), which implies that preferences (and utility) are not static, but adapt and change with experience. Owing to the randomised trial design it seems likely that exposure to different models of decision making has resulted in real effects on patient utilities which could be a quantitative shift across the options of the attributes or a reconceptualisation of the attributes themselves.
Strengths and limitations of the study and comparison with existing literature
The use of discreet choice experiments in the study of doctor–patient relationships is not new,23 but the present study had the advantage of using patients with real conditions in real situations. Moreover, delivery of training in phases allowed assessment of the responsiveness of utility to changes in the way that GPs manage consultations after being trained in risk communication and SDM. The response rate was very good compared with analogous studies.18
While such techniques cannot explain what is going on in people's minds when they state their preferences, this study has at least shown that in a randomised comparison the experiences of the patients have resulted in different utilities being expressed. This is not to suggest that changes in preferences following a single consultation 6 months previously are massive, but they are statistically significant, albeit from a large sample size. It is difficult with a concept like utility to specify what would be a clinically significant effect.
Nineteen per cent of responders always chose ‘normal practice’ (the constant scenario) over the alternatives which might overestimate preferences for the status quo as the selected ‘normal practice’ scenario might not reflect everyday life.
Patients who had poorer mental health were more inclined to opt for alternative scenarios. Other studies23 have shown that patients with lower (general) health tend to prefer to leave decision making to the doctor, but we are unaware of any studies that examined willingness to trade separately by mental and physical health status.
Patients with menorrhagia and menopausal problems were less likely to take part in the review appointment,13 which emphasises the fact that the SDM model as currently formulated might be too optimal for certain conditions. Future policy initiatives to promote SDM should take account of this. These data suggest that there could legitimately be some ‘push’ from professionals 30 in addition to the likely ‘pull’ from consumers.31
Comparisons of groups related to whether the GP had been trained in the relevant method and not (necessarily) to the model of consultation that actually took place. Patient preferences are also likely to be influenced by what a patient experiences, as opposed to what training a doctor has or hasn't received.32 This ‘intention-to-treat’ analysis is likely to underestimate the impact of training on utility.
Results of this study are consistent with other work31,32 in that they show that SDM is of lesser priority to patients than other consultation attributes. This suggests that the priority afforded to SDM as a policy objective might be moderated. However, these results also indicate that once patients have been exposed to a consultation with a doctor trained in SDM they place a higher value on such processes, and this change occurred after just one consultation for each patient. While such exposure still did not affect the overall ordering of attributes it is possible that the ordering could change after more repeated exposure.
In addition, there are still considerable ethical justifications for its (cautious) implementation.2 These suggest that it remains important to explore how patient involvement in decisions about their care may be enhanced and these approaches provide a platform for communication skills development for healthcare professionals. The decision-making stage of the consultation — the ‘neglected second half’9 — is also important. Skill acquisition in this area is also beginning to be integrated into professional development programmes. We therefore advocate that skill acquisition for such models of consultations should be included in communication skills training for healthcare professionals.
Implications for clinical practice
This study shows that the use of discrete choice experiments is feasible to ascertain patient's preference of aspects of primary care consultations.
The results indicate that patients are likely to require doctors who listen and give information that is easy to understand as ‘routine’ consultations, before SDM and risk communication approaches are warranted or valuable, that is, the implementation of a SDM or risk communication approach cannot be advocated unless these key attributes are part of a routine consultation.
These findings are important as they suggest that although patient utilities for SDM may be modest to start with, they are responsive to changes in experiences of health care. That is, they suggest that patients' utilities are responsive to their experience, and if healthcare professionals adopt these approaches then patients may come to value the process further. This provides support for advocating SDM skill development in professional training. If implemented in practice, then patients are likely to increasingly value the process as they experience it more.
Acknowledgments
We gratefully acknowledge the commitment of the 20 participating doctors from the general practices across Gwent, South Wales; their practice staff; the 800 participating patients; the secretarial and clerical assistance of Claire Darmanin, Sheila Morris, and Sali Morgan in administering the study; and the guidance of the study Steering Group members.
Funding Body
The UK Department of Health, ‘Health in Partnership’ research programme funding (project no 12)
Ethics Committee
Ethical approval was obtained from the Gwent Health Authority Local Research Ethical Committee (98/2690)
Competing Interests
The authors have stated that there are none
REFERENCES
- 1.Stewart M, Brown JB, Donner A, et al. The impact of patient-centred care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 2.Guadagnoli E, Ward P. Patient participation in decision making. Soc Sci Med. 1998;47:329–339. doi: 10.1016/s0277-9536(98)00059-8. [DOI] [PubMed] [Google Scholar]
- 3.O'Connor AM, Stacey D, Entwistle V, et al. Decision aids for people facing health treatment or screening decision. Issue 2. Update Software: Cochrane Library; 2003. Cochrane Review. [DOI] [PubMed] [Google Scholar]
- 4.Charles C, Gafni A, Whelan T. Shared decision making in the medical encounter: What does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 5.Mooney GH. What else do we want from our health services? Soc Sci Med. 1994;39:151–154. doi: 10.1016/0277-9536(94)90323-9. [DOI] [PubMed] [Google Scholar]
- 6.Gafni A, Charles C, Whelan T. The physician-patient encounter: the physician as perfect agent for the patient versus the informed treatment decision-making model. Soc Sci Med. 1998;47(3):347–354. doi: 10.1016/s0277-9536(98)00091-4. [DOI] [PubMed] [Google Scholar]
- 7.Maynard DW. Interaction and asymmetry in clinical discourse. Am J Sociol. 1991;97:448–495. [Google Scholar]
- 8.Ryan M. Agency in Health Care: lessons for economists from sociologists. Am J Econ Soc. 1994;53(2):207–217. [Google Scholar]
- 9.Elwyn G, Edwards A, Kinnersley P. Shared-decision making: the neglected second half of the consultation. Br J Gen Pract. 1999;49:477–82. [PMC free article] [PubMed] [Google Scholar]
- 10.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision-making and the concept of equipoise: defining the ‘competences’ of involving patients in health care choices. Br J Gen Pract. 2000;50:892–899. [PMC free article] [PubMed] [Google Scholar]
- 11.Shackley P, Ryan M. What is the role of the consumer in health care? J Soc Pol. 1994;23(4):517–514. [Google Scholar]
- 12.Howie JRG, Heaney D, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract. 1998;15:165–71. doi: 10.1093/fampra/15.2.165. [DOI] [PubMed] [Google Scholar]
- 13.Edwards A, Elwyn G, Hood K, et al. The development of COMRADE — a patient-based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Ed and Counselling. 2003;50:311–322. doi: 10.1016/s0738-3991(03)00055-7. [DOI] [PubMed] [Google Scholar]
- 14.Elwyn G, Hutchings H, Edwards A, et al. The OPTION scale: measuring the extend that the clinicians involve patients in decision making tasks. Health Expect. 2005;8(1):34–42. doi: 10.1111/j.1369-7625.2004.00311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ware JE, Kosinski M, Keller S. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Edwards A, Elwyn G, Hood K, et al. Patient-based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21:345–352. doi: 10.1093/fampra/cmh402. [DOI] [PubMed] [Google Scholar]
- 17.Elwyn G, Edwards A, Hood K, et al. Achieving involvement: process outcomes from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21:335–346. doi: 10.1093/fampra/cmh401. [DOI] [PubMed] [Google Scholar]
- 18.Ryan M, Gerard K. Using choice experiment to value health care programmes: current practice and future prospects. Applied Health Economics Policy Annals. 2003;2:55–64. [PubMed] [Google Scholar]
- 19.Lancaster K. A new approach to consumer theory. Journal of Political Economics. 1974;74(1):132–157. [Google Scholar]
- 20.Ryan M. Using conjoint analysis to take account of patient preferences and go beyond health outcomes: an application to in vitro fertilisation. Soc Sci Med. 1999;48:535–546. doi: 10.1016/s0277-9536(98)00374-8. [DOI] [PubMed] [Google Scholar]
- 21.Edwards A, Elwyn G. How should effectiveness of risk communication to aid patients' decisions be judged? A review of the literature. Med Decision Making. 1999;19:428–434. doi: 10.1177/0272989X9901900411. [DOI] [PubMed] [Google Scholar]
- 22.Elwyn G, Edwards A, Mowle S, et al. Measuring the involvement of patients in shared decision-making: a systematic review of instruments. Patient Educ Couns. 2000;43(1):5–22. doi: 10.1016/s0738-3991(00)00149-x. [DOI] [PubMed] [Google Scholar]
- 23.Scott A, Vick S. Patients, doctors and contracts: an application of principal-agent theory to the doctor-patient relationship. Scot J Pol Econ. 1999;46(2):111–134. [Google Scholar]
- 24.Ryan M, Bate A. Testing the assumption of rationality, continuity and symmetry when applying discrete choice experiments in health care. Applied Econ Letters. 2001;8:59–63. [Google Scholar]
- 25.Bunch DS, Louviere JJ, Anderson D. A comparison of experimental design strategies for multinomial logit models: the case of generic attributes. Davis, Ca.: Graduate School of Management, University of California; 1996. Working paper. [Google Scholar]
- 26.Pearmain D, Swanson J, Kroes E, Bradley M. Stated preference techniques: a guide to practice. The Hague: Steer Davis Gleave and Hague Consulting Group; 1991. [Google Scholar]
- 27.Huber J, Zwerma K. The importance of utility balance in efficient choice designs. J Mark Res. 1996;33:307–317. [Google Scholar]
- 28.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. 1998;46(1):97–117. doi: 10.1016/s0277-9536(97)00148-2. [DOI] [PubMed] [Google Scholar]
- 29.Rice N, Jones A. Multilevel models and health economics. Health Econ. 1997;6:561–575. doi: 10.1002/(sici)1099-1050(199711)6:6<561::aid-hec288>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 30.Salkeld G, Ryan M, Short L. The veil of experience: do consumers prefer what they know best? Health Econ Letters. 2000;4(1):4–9. doi: 10.1002/(sici)1099-1050(200004)9:3<267::aid-hec511>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 31.Edwards A, Elwyn G. Developing professional ability to involve patients in their care: pull or push? Qual Health Care. 2001;10:129–130. doi: 10.1136/qhc.0100129... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Little P, Everitt H, Williamson I, Warner G, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–911. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]


