Abstract
Background
International medical graduates (IMGs) have been a valuable resource for the United States physician workforce, and their contribution to the United States workforce is likely to increase.
Objective
To describe the historical trends and compare the characteristics of IMGs to United States medical graduates (USMGs) in the United States.
Design
Longitudinal analysis of the American Medical Association Physicians’ Professional Data (AMA-PPD) database using the 1978–2004 files and a comparative analysis of the characteristics of a random sample of 1,000 IMGs and a random sample of 1,000 USMGs using the 2004 file.
Measurements
Historical trends and characteristics of IMGs in the United States.
Results
Over the last 26 years, the number of IMGs in the United States grew by 4,873 per year reaching a total of 215,576 in 2004, about 2.4 times its size in 1978. The proportion of IMGs increased 0.12% per year, from 22.2% in 1978 to 25.6% in 2004. In 2004, compared with USMGs, IMGs were older, less likely to be board certified [Odds ratio (OR), 0.68; 95% CI, 0.53 to 0.86], less likely to work in group practice (OR, 0.60; 95% CI, 0.37 to 0.98), more likely to have Internal Medicine as practice specialty (OR, 2.10; 95% CI, 1.62 to 2.71) and more likely to be residents (OR, 1.52; 95% CI, 1.07 to 2.16).
Conclusions
Over the last quarter century, the IMGs provided a significant and steady supply for the United States physician workforce that continues to grow. Policymakers should consider the consequences for both the United States and source countries.
Key words: foreign medical graduates, health manpower, internship and residency
BACKGROUND
In the 1980s and 1990s, health care planners in the United States projected physician surpluses by the beginning of the 21st Century.1 In 1981, the Graduate Medical Education National Advisory Committee (GMENAC) predicted a surplus of 145,000 physicians by the year 2000.2 GMENAC recommended restricting both the number of positions in United States medical schools and the number of international medical graduates (IMGs) training in the United States. In 1997, a consortium of major organizations declared that there is “compelling evidence that the United States is on the verge of a serious oversupply of physicians.”3 The consortium recommended limiting federal funding of residency training positions.
Contrary to these projections, more recent evidence suggests that the United States is actually experiencing an increasing physician shortage.4 Eighty-five percent of officials of United States state medical societies and deans of United States medical schools perceived shortages of physicians in a number of specialties.5 Several reports have confirmed these perceptions for specialties such as radiology,6 anesthesiology,7 cardiology,8 rheumatology,9 and pulmonary and critical care.10 The American College of Physicians (ACP) recently expressed its concerns about “the adequacy of the supply of General Internists who provide care in outpatient settings.”11 There are reports that these shortages are negatively affecting the mission of many medical schools, particularly in the areas of clinical teaching and patient care.5 Leading authorities are projecting deficits by 2020 or 2025 as great as 200,000 physicians, 20% of the needed workforce.4
Despite few alternative predictions of no physician shortage,12,13 most organizations are alarmed and have revised their previous positions and policies. The American Medical Association’s (AMA) current policy emphasizes physician shortages and that “evidence exists for additional shortages in the future.”14 Both the Association of American Medical Colleges (AAMC) and the Council on Graduate Medical Education (COGME) recently recommended increasing the number of United States medical graduates (USMGs) by increasing enrollment in United States medical schools by 15% over the next 10 years.15,16 They also recommended that residency programs increase the number of training positions without recommending increasing or decreasing the number of IMGs in these positions.
Increasing the number of USMGs is challenging and might not suffice the projected needs in the United States if changes are not instituted on a large scale.17,18 The COGME report highlights that the recommended increase of 15% in medical school enrollment will have only a limited impact on the total supply of physicians in 2020.16 Furthermore, a more realistic estimate of the potential expansion of medical school training is thought to be only 7.6%.5 In addition, recent analyses show that the projected growth in the number of applicants to United States medical schools will not parallel the suggested expansion of medical school seats or the projected physician shortage.19
IMGs have been a valuable resource for the United States physician workforce.11 The AMA Physicians’ Professional Data (AMA-PPD) file indicates that 215,928 IMGs were active physicians in the United States in 2004, constituting 23.7% of the total physician workforce.20 Given the projected shortages and the challenges to increasing the number of USMGs, IMGs will likely remain a valuable resource for the United States physician workforce in the future. In fact, the ACP position is that a national health care workforce policy should address the contributions of IMGs in meeting current and anticipated needs of the patient population.11
Because of the current size and potential future growth of IMGs as part of the United States physician workforce, a better understanding of their historical trends and characteristics is essential in setting future policies. Indeed, the AAMC has called for research to understand the role of IMGs in the United States health care system.15 The objective of this study is to describe the historical trends of the number of IMGs who are active physicians in the United States and to compare their characteristics to those of USMGs.
METHODS
We conducted an observational study using the American Medical Association Physicians’ Professional Data (AMA-PPD) as our sampling frame.21 This dataset contains detailed information on all physicians who reside in the United States and who have met the educational and credentialing requirements necessary for recognition as physicians in the United States. A record is created when an individual enters a medical school accredited by the Liaison Committee on Medical Education (LCME), or in the case of IMGs, upon entry into ACGME-accredited programs. Physicians are classified as active unless they are retired, semiretired, working part-time, temporarily not in practice, or not active for other reasons. Active physicians include both physicians in practice and physicians in training who we will refer to as practicing physicians and residents, respectively. We analyzed data from both the historical and the current AMA-PPD files. The historical files were available for the years 1978–2004 except for 1984 and 1990. The most current file available as of November 2005 was the 2004 AMA-PPD.
First, we evaluated the 1978–2004 trends of the number of IMGs who are active physicians in the United States. We evaluated these trends for the following three groups: resident IMGs, practicing physician IMGs, and total IMGs. We then expressed these numbers as proportions (relatively to all residents, all practicing physicians, and all active physicians in the United States, respectively). In a post hoc analysis, we used linear and polynomial models to depict the long-term time trends of numbers and proportions for each of the three groups over the last quarter of the century.
Second, using the 2044 AMA-PPD file, we analyzed and compared the characteristics of a random sample of 1,000 IMGs (sampling rate of 0.46%) to those of a random sample of 1,000 USMGs (sampling rate of 0.16%). These characteristics included age, gender, number of years since graduation from medical school, board certification, practice specialty, practice type, practice location, and primary employer. We omitted the country of birth variable from our analysis because it was missing for about 25% of individuals (of whom 90% were IMGs). We characterized the practice location by linking its zip code to a four-category, rural-to-urban status and taxonomy, a condensed version of the Rural–Urban Commuting Area (RUCA) codes.22 Before purchasing the data, we calculated the sample size required to detect a 5% difference between the 2 groups in the percentage of board certified physicians with a power of 0.80, and a sample size of 1,000 in each group would allow us to detect a difference of 5%.
We conducted univariate analyses using Student’s t-test and the chi-square test, when appropriate. In a first multivariable analysis, we used practice specialty as dependent variable and age, gender, country of graduation, and residency status (yes/no) as independent variables. We then conducted multivariable analyses using board certification, practice type, practice location, and primary employer as dependent variables and age, gender, country of graduation, residency status (yes/no), and practice specialty as consecutive independent variables. We excluded residents from analyses of board certification, but otherwise, adjusted for the same covariates in all models. We did not use the number of years since graduation as an independent variable in the main analyses because it was highly correlated with age (Pearson correlation coefficient 0.9; P < .001). However, we used years since graduation instead of age in secondary analyses to check the stability of the inferences. Multinomial logistic regression models were used for all analyses except board certification for which we used a binary logistic model. We considered two-sided P values and P < .05 as statistically significant and used Microsoft Excel 2005 for data management and SPSS, version 13.0 (SPSS, Inc., Chicago, Illinois), for data analysis.
RESULTS
Historical Trends of IMGs
Between 1978 and 2004, the numbers of resident IMGs, practicing physician IMGs and total IMGs showed consistent upward trends that were more prominent for the latter 2 groups (Fig. 1). The yearly number for each of the three groups fitted simple linear regression models, and the addition of polynomial terms did not significantly improve curve estimation. The respective slopes and P values for the linear models were: β = 702, P < .001; β = 4,171, P < .001; β = 4,873, P < .001. These results suggest that the total number of residents IMGs, practicing physician IMGs, and total IMGs increased, respectively, by 702, 4,171, and 4,873 each year. In 2004, 31,147 resident IMGs, 184,429 practicing physician IMGs and 215,576 total IMGs were active in the United States. These numbers reflect respective increases of 19,310, 107,510, and 126,820 individuals over a 26-year period (relative increases of 163.1%, 139.8% and 142.9%).
Figure 1.
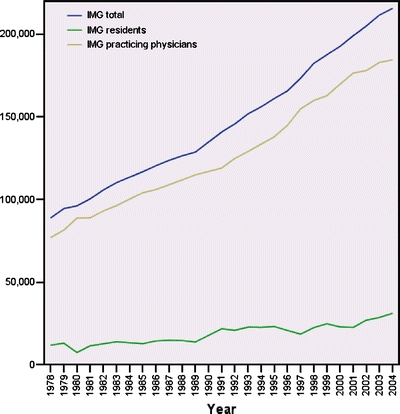
Time trends (1978–2004) of the numbers of residents, practicing physicians, and total IMGs in the United States. Data for 1984 and 1990 are missing. We used straight interpolation in drawing the trends. The total number of physicians in the United State in 2004 was 843,248.
The trends of the proportions of resident IMGs to all residents, of practicing physician IMGs to all practicing physicians, and of total IMGs to all active physicians were also upward (Fig. 2). The yearly proportion for each of the three groups also fit simple linear regression models, and the addition of polynomial terms did not significantly improve curve estimation. The respective slopes and P values of the linear models were β = 0.38%, P < .001; β = 0.08%, P < .001; β = 0.12%, P < .001. These results suggest that the proportion of resident IMGs relative to all residents, for example, increased by 0.38% each year. Accordingly, in 2004, 28.4% of residents, 25.2% of practicing physicians, and 25.6% of total physicians active in the United States were IMGs. These proportions reflect increases of 8.8%, 2.5%, and 3.4% of the respective proportions over the 26-year period.
Figure 2.

Time trends (1978–2004) of the proportions of residents, practicing physicians, and total IMGs in the United States. Data for 1984 and 1990 are missing. We used straight interpolation in drawing the trend.
Characteristics of IMGs Compared to USMGs
Table 1 displays the characteristics of IMGs and compares them to those of USMGs. In the univariate analyses, compared to USMGs, IMGs were on average older (by about 3 years) and had a higher number of years since graduation from medical school (by about 5 years). They were also less likely to be board certified (P < .001) and more likely to have Internal Medicine as a practice specialty (P < .001) and work in solo practice (P < .001).
Table 1.
Characteristics of IMGs and USMGs practicing in the United States
| IMGs | USMGs | P value* | |
|---|---|---|---|
| (n = 1,000) | (n = 1,000) | ||
| Age, mean (SD) | 50.5 (13.3) | 47.6 (13.4) | <.001 |
| Years since graduation, mean (SD) | 23.4 (13.0) | 18.2 (13.0) | <.001 |
| Gender | |||
| Female (%) | 30.0 | 26.1 | .05 |
| Practice specialty† | |||
| Family Practice (%) | 8.3 | 12.1 | <.001 |
| Internal Medicine (%) | 21.9 | 12.0 | |
| Pediatrics (%) | 8.7 | 7.5 | |
| OBGYN (%) | 4.1 | 5.5 | |
| General surgery (%) | 3.3 | 4.6 | |
| Board certification‡ (%) | 72.6 | 81.1 | <.001 |
| Practice type§ | |||
| Resident (%) | 13.4 | 13.8 | .72 |
| Direct patient care (%) | 83.2 | 79.6 | |
| Administration (%) | 1.0 | 1.6 | |
| Medical teaching (%) | 1.3 | 1.2 | |
| Medical research (%) | 1.2 | 1.1 | |
| Practice locationΓ | |||
| Urban (%) | 89.2 | 88.0 | .60 |
| Large rural (%) | 5.6 | 6.8 | |
| Small rural (%) | 1.7 | 2.2 | |
| Isolated small rural (%) | 0.8 | 0.8 | |
| Primary employer¶ | |||
| Governmental (%) | 6.4 | 4.6 | <.001 |
| Solo practice (%) | 19.9 | 13.4 | |
| 2 Physician practice (%) | 2.6 | 3.3 | |
| Group practice (%) | 20.8 | 31.2 | |
| HMO (%) | 0.5 | 0.3 | |
| Medical school (%) | 2.9 | 2.8 | |
| Non- governmental hosp (%) | 16.3 | 17.2 | |
*Based on t-tests for interval variables (age, years since graduation) and chi-square tests for categorical variables.
†Only primary care specialties are listed.
‡Residents excluded from denominator.
§Only relevant categories are listed; data missing for n = 91.
ΓData missing for n = 49.
¶Only relevant categories are listed.
Multivariable analyses confirmed that compared with USMGs, IMGs were less likely to be board certified [Odds ratio (OR) 0.68; 95% CI, 0.53 to 0.86] and work in group practices (OR, 0.60; 95% CI, 0.37 to 0.98). IMGs were more likely to be residents (OR, 1.52; 95% CI, 1.07 to 2.16) and have Internal Medicine as a practice specialty. In the secondary analyses (years since graduation replacing age as an independent variable), the results did not change significantly except for the odds ratio for IMGs being residents (OR, 6.03; 95% CI, 3.75 to 9.7).
DISCUSSION
Over the last quarter century, the number of IMGs in the United States grew on average by 4,873 per year reaching a total of 215,576 in 2004, about 2.4 times its 1978 size. The 2 subgroups of resident IMGs and practicing physician IMGs showed similar increases. In 2004, compared with USMGs, IMGs were older, less likely to be board certified, less likely to work in group practice, more likely to have Internal Medicine as practice specialty, and more likely to be residents.
This study has two major strengths. First, we used a dataset that is compiled using a systematic and comprehensive methodology and accounts for all active physicians licensed to practice medicine in the United States.21 Second, while other studies have provided a cross-sectional analysis of the reliance of the United States physician workforce on IMGs, we were able to describe the historical trends of IMGs in the United States over a period of more than 26 years. While the longitudinal analysis is unique to date, our analysis also reduces the possibility of chance findings that cross-sectional analysis are prone to, and more importantly, enables policymakers to make better future predictions.
The study has some limitations. We did not have the full population data available for analyzing physicians’ characteristics, and used instead, 2 samples of 1,000 records each based on a priori power calculations. IMGs include the two distinct subgroups of United States citizens who trained abroad and non-U.S. citizens. We did not describe the historical trends for the two aforementioned subgroups nor did we compare their characteristics. We did, however, adjust for U.S. citizenship status in comparing the characteristics of IMGs and USMGs. The linear models we used to depict the time trends of numbers and proportions might not be as strong as methods such as piecewise linear regression models or smooth spline models particularly for short-term fluctuations. However, the models we used are appropriate for the purpose of detecting long-term trends especially because they appear to be reasonably approximated by straight lines.
There are a number of interesting observations related to these historical trends. First, the actual numbers of IMGs show higher growth rates than their proportions (Figs. 1 and 2). This is explained by the fact that the growth in numbers is mainly related to the growth of the total population of active physicians in the United States (i.e., even if the proportions of IMGs remained constant, their number will still grow with the growth of the total population of physicians). Second, while the growth in the proportion of IMGs is greater for residents than for practicing physicians (0.38% vs 0.08%, respectively), the growth in the number of IMG residents is lower than for practicing physician IMGs (702 vs 4171, respectively). This is because of the fact that the total population of residents is much smaller than that of practicing physicians. The slower growth in the number of resident IMGs is also related to the fact that individuals joining the resident IMGs group will leave it after a few years (e.g., 3 years for Internal Medicine training) while individuals joining the practicing physician IMG group will leave it after many years of practice.
The comparisons of the characteristics of IMGs and USMGs are consistent with the published literature. In terms of board certification, Benson et al. found that among physicians who graduated between 1975 and 1980 and applied for the certifying examination of the American Board of Internal Medicine, USMGs had higher passing rates than IMGs.23 Among IMGs, non-U.S. citizens had higher passing rates than U.S. citizens. Norcini et al. showed similar results among 1958–1994 medical graduates, regardless of specialty.24 In terms of primary employer, Freshnok et al. also found in the early 1980s that physicians in group practice were predominantly USMGs.25 In terms of practice location, both a 1995 study and a 2003 study indicated that patterns of location of IMGs mirrored those of USMGs.26,27 Our findings relating to practice specialty differ from the findings by Mullan in 1995 that IMGs had similar specialty patterns to USMGs. The reasons for these differences are unclear.
Our analysis shows that over the last quarter century, the IMGs provided a significant and steady supply for the United States physician workforce. Based on the regression model, and assuming demand and supply factors remain the same, the number of IMGs would increase about 102,000 by 2025. In formulating policies to address the projected physician shortage, U.S. and foreign policymakers need to consider whether IMGs could sustain such supply. In fact, a number of high income countries are trying to address their own physician shortages by recruiting from the same pool of English-speaking IMGs as the United States.28 This competition could potentially complicate the recruitment of IMGs into the United States physician workforce and affect the quality of care delivered by those who are ultimately recruited.
In addition, the United States and foreign policymakers should consider the implications of the global physician migration for the ‘source countries’ that are mainly low income countries.29 These countries benefit financially through remittances, skills transfer, and possible investment upon migrants’ return.30 They suffer, however, from a ‘brain drain’ resulting in loss of educational investment, loss of intellectual capital, reduced range of available services, and chronic understaffing of health care facilities.31 This dilemma has indirect impact on high income countries such as the United States because of the increased threat of global pandemics. Public health in high-income countries increasingly depends on the effectiveness of health care systems in the low income countries.18
In summary, this study shows that the United States physician workforce increasingly consists of IMGs and that their characteristics differ from those of USMGs. Future studies should quantify the needs of the United States physician workforce for IMGs and determine how to meet those needs in view of the source countries’ requirements and the expected toll of the brain drain. Studies should also compare the quality of care provided by IMGs to that of USMGs and how the differences in certain characteristics of IMGs and USMGs (e.g., specialty and primary employer) affect clinical practice patterns.
Acknowledgments
Acknowledgments We thank Dr. Gordon Guyatt and Dr. Peter Tugwell for their comments and suggestions. Research for Health in Erie County, Inc. funded this work and was not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Investigators received salary support from institutional sources. This study was presented as a poster during the SGIM 29th annual meeting (Apr 28 2006).
Potential Financial Conflicts of Interest None disclosed.
References
- 1.Grumbach K, Lee PR. How many physicians can we afford? JAMA. 1991;265:2369–72. [DOI] [PubMed]
- 2.Graduate Medical Education National Advisory Committee. Summary report of the Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services. Washington, D.C. April 1981.
- 3.American Association of Colleges of Osteopathic Medicine, American Medical Association, American Osteopathic Association, Association of Academic Health Centers, Association of American Medical Colleges, National Medical Association. Consensus Statement on Physician Workforce. Washington, DC; 1997.
- 4.Cooper RA. Weighing the evidence for expanding physician supply. Ann Intern Med. 2004;141:705–14. [DOI] [PubMed]
- 5.Cooper RA, Stoflet SJ, Wartman SA. Perceptions of medical school deans and state medical society executives about physician supply. JAMA. 2003;290:2992–5. [DOI] [PubMed]
- 6.Sunshine J. Overview and Analysis of Information Regarding the Shortage. Chicago, IL: American College of Radiology; 2001.
- 7.Schubert A, Eckhout G, Tremper K. An updated view of national anesthesia personnel shortfall. Anesth Analg. 2003;96:207–14. [DOI] [PubMed]
- 8.Foot DK, Lewis RP, Pearson TA, Beller GA. Demographics and cardiology, 1950–2050. J Am Coll Cardiol. 2000;35:1067–81. [DOI] [PubMed]
- 9.Boyce ST. The Rochester Community Physician Workforce: Factors Affecting Recruitment and Retention. Rochester, NY: CGR; 2003.
- 10.Angus DC, Kelly MA, Schmitz RJ, White A, Popovich J. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284:2070–762. [DOI] [PubMed]
- 11.Zerehi, R. For the Health and Public Policy Committee of the American College of Physicians. Creating a New National Workforce for Internal Medicine. A Position Paper: American College of Physicians; 2006.
- 12.Weiner JP. Prepaid group practice staffing and U.S. physician supply: lessons for workforce policy. Health Aff. 2004;Suppl Web Exclusives:W4-43–59. [DOI] [PubMed]
- 13.Lurie JD, Goodman DC, Wennberg JE. Benchmarking the future generalist workforce. Eff Clin Pract. 2002; 5:58–66 [PubMed]
- 14.American Medical Association. H-200.953 The Physician Workforce: Recommendations for Policy Implementation. 2003 January 18, Available at: http://web.archive.org/web/20040207002827/http://www.ama-assn.org/ama/pub/article/print/1616-8229.html. Accessed January 23, 2006.
- 15.Association of American Medical Colleges. The physician workforce: position statement. February 2005. Available at: http://www.aamc.org/workforce/12704workforce.pdf. Accessed January 23, 2006.
- 16.Council on Graduate Medical Education. Physician Workforce Policy Guidelines for the United States, 2000–2020. Rockville, MD: Health Resources and Services Administration, 2005.
- 17.Cooper RA. Medical schools and their applicants—an analysis: if more physicians are required, can medical schools fill the gap? Health Aff. 2003;22:71–84. [DOI] [PubMed]
- 18.Blumenthal D. New steam from an old cauldron—the physician-supply debate. N Engl J Med. 2004;350:1780–7. [DOI] [PubMed]
- 19.Cooper RA. Impact of trends in primary, secondary, and postsecondary education on applications to medical school. I: Gender considerations. Acad Med 2003;78:855–63. [DOI] [PubMed]
- 20.American Medical Association. International Medical Graduates. 2005 Available at: http://www.ama-assn.org/ama/pub/category/1550.html. Accessed January 23, 2006.
- 21.American Medical Association. AMA Physicians’ Professional Data. 2004. Available at: http://www.ama-assn.org/ama/pub/category/2673.html. Accessed January 23, 2006.
- 22.U.S. Department of Agriculture. RUCA Codes. Available at: http://www.ers.usda.gov/Briefing/Rurality/RuralUrbanCommutingAreas/. Accessed January 23, 2006.
- 23.Benson JA, Jr., Meskauskas JA, Grosso LJ. Performance of U.S. citizen–foreign medical graduates on certifying examinations in internal medicine. Am J Med. 1981;71:270–3. [DOI] [PubMed]
- 24.Norcini JJ, Boulet JR, Whelan GP, McKinley DW. Specialty board certification among U.S. Citizen and non-U.S. Citizen graduates of International Medical Schools. Acad Med. 2005;80:S42–5. [DOI] [PubMed]
- 25.Freshnock LJ, Goodman LJ. The organization of physician services in solo and group medical practice. Med Care. 1980;18:17–29. [DOI] [PubMed]
- 26.Mullan F, Politzer RM, Davis CH. Medical migration and the physician workforce. International medical graduates and American medicine. JAMA. 1995;273:1521–7. [DOI] [PubMed]
- 27.Fink KS, Phillips RL, Jr., Fryer GE, Koehn N. International medical graduates and the primary care workforce for rural underserved areas. Health Aff. 2003;22:255–62. [DOI] [PubMed]
- 28.Mullan F. The metrics of the physician brain drain. N Engl J Med. 2005;353:1810–8. [DOI] [PubMed]
- 29.Hallock JA, Seeling SS, Norcini JJ. The international medical graduate pipeline. Health Aff. 2003;22:94–6. [DOI] [PubMed]
- 30.Regets MC. Research and Policy Issues in High-skilled International Migration: a Perspective with Data from the United States. Arlington VG: National Science Foundation; 2001. Discussion paper 366.
- 31.Adams O, Kinnon C. A Public Health Perspective. International Trade in Health Services: a Developmental Perspective. Geneva: World Health Organization; 1998.


