Abstract
The quality of diabetes care delivered to patients falls below the expectations of practice guidelines and clinical trial evidence. Studies in many jurisdictions with varying health care systems have shown that recommended processes of care occur less often than they should; hence, outcomes of care are inadequate. Many studies comparing care between specialists and generalists have found that specialists are more likely to implement processes of care. However, this provides little insight into improving quality of care, as the difference between specialists and generalists in these studies is small compared to the overall deficiency in quality. Therefore, future research should instead focus on ways to implement high quality care, regardless of specialty. To date, few methodologically rigorous studies have uncovered interventions that can improve quality of care. The development of such interventions to help all physicians implement better quality care could greatly benefit people with diabetes.
Key words: quality of care, primary care, diabetes mellitus, specialist care
Although many interventions have been shown to reduce complications and improve health for people with diabetes, both the use of these interventions and the achievement of treatment targets are frequently below the expectations of practice guidelines. These deficiencies in quality of care have been documented all too frequently. In response, a growing body of literature has examined whether specialists deliver better quality care than generalists. Since the 1980s, when just four were published, the number of papers published per decade has risen 10-fold (Fig. 1). Most studies suggest that the difference between specialists and generalists is small. In this paper, we suggest that such studies are a distraction from the more important issues of why diabetes care is suboptimal and what can be done to improve diabetes management, regardless of provider specialty.
Figure 1.
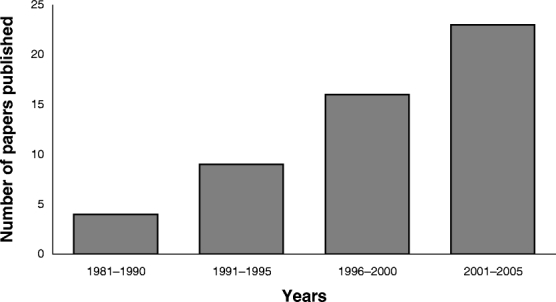
An increasing number of studies have been published comparing specialist and generalist care for diabetes.
OVERALL QUALITY OF CARE
Deficiencies in quality of diabetes care are found in many countries with different health care systems for both process of care measures (such as physical examination maneuvers and the ordering of tests by physicians) and for outcomes of care (the achievement of treatment targets and prevention of complications). In a large study of American patients, fewer than 20% received the recommended two A1c tests, one lipid profile, and one dilated eye exam in 1 year.1 Fewer than half of patients surveyed in Italy reported receiving a foot exam over 1 year,2 and only 11% of Canadian diabetic seniors with established coronary artery disease were prescribed an antiplatelet agent, a statin, and an angiotensin-converting enzyme inhibitor.3 At least partially as a result of these inadequate processes of care, outcomes for patients are often poor. Data from the 1990s using two U.S. health surveys found that 41% of diabetic patients had A1c levels above 8.0%, and 18% had levels over 9.5%. Only 42% of patients had LDL cholesterol levels below 3.4 mmol/L and fewer than two thirds had blood pressure levels below 140/90 mmHg.4 Similar results have been found in countries around the world.5–8 The proportion of patients meeting glycemic, blood pressure and cholesterol targets did not differ between 1988–1994 and 1999–2000,9 and although recent data suggest some small trends toward improvement,10 large numbers of patients remain inadequately treated.
DIFFERENCES IN QUALITY BETWEEN SPECIALIST AND GENERALIST CARE
To address these gaps between evidence and practice, some have speculated that specialists may deliver better chronic disease care than generalists.11 Although many investigators have examined this question in diabetes, few studies accounted for patient clustering within physicians and hence statistical nonindependence. Those that did are summarized below and in Table 1.
Table 1.
A Selection of Studies Comparing Processes of Diabetes Care Between Specialists and Generalists
| Study | Process measure | Performance rate by specialists (%) | Performance rate by generalists (%) |
|---|---|---|---|
| Lafata et al.1 | Measuring lipid profile | 77 | 70 |
| Measuring A1c | 84 | 58 | |
| Eye examination | 51 | 33 | |
| All three | 35 | 16 | |
| Greenfield et al.12 | Measuring lipid profile | 45 | 51 |
| Measuring urine protein | 58 | 42 | |
| Measuring A1c | 90 | 79 | |
| Eye examination | 41 | 34 | |
| Blood glucose self-monitoring | 83 | 73 | |
| De Berardis et al.14 | Measuring total cholesterol | 66 | 66 |
| Measuring microalbuminuria | 53 | 31 | |
| Measuring A1c | 73 | 43 | |
| Eye examination | 55 | 38 | |
| Foot examination | 52 | 40 | |
| Shah et al.15 | Drug escalation in response to poor glycemic control | 45 | 37 |
| Schaars et al.16 | Measuring blood pressure | 73* |
*Indicates the performance rate in the whole study population, as the performance rate by group was not reported separately.
Processes of Care
A study in American ambulatory care clinics found that patients with shared care between endocrinologists and generalists versus generalist-only care received more A1c and lipid tests, and more dilated eye examinations.1 Another smaller study of 1,750 patients across the United States found nonstatistically significant trends favoring specialists for many processes of care.12 An Italian group found that several processes were more common for specialists’ patients compared to general practitioners, including performance of self-monitoring of blood glucose, foot examinations, A1c testing, microalbuminuria testing, and dilated eye exams.2,13,14 A study using large Canadian administrative databases showed that specialists escalated glucose-lowering medications for patients with poor glycemic control more often than generalists,15 and a Dutch study found that specialized diabetes clinics measured patients’ blood pressures more often than generalists did.16 Thus, specialists often do provide better processes of care than generalists, and yet in most cases, the absolute difference is small compared to the deficiency that even specialist care has compared to the ideal performance level of 90% to 100% at which most of these processes ought to be performed (see Table 1).
Outcomes of Care
Because differences between specialists and generalists for many processes are small, it is not surprising that clinical outcomes have not been shown to markedly differ between them. In the Medical Outcomes Study, which prospectively followed 424 diabetic patients in the 1980s, most clinical, functional status and well-being measures did not differ between physician groups; only foot ulcer prevalence showed greater improvement for patients followed by endocrinologists, but their patients had a higher prevalence at baseline.17 The Pittsburgh Epidemiology of Diabetes Complications Study prospectively followed patients with type 1 diabetes for 10 years, and showed that greater time under specialist care during follow-up was associated with a reduced incidence of overt nephropathy, but other micro- and macrovascular complications were not different.18 In Italy, despite small differences in processes between specialists and general practitioners, glycemic, blood pressure, and lipid control did not differ.13,14 Canadian and German studies have also shown only small differences in glycemic control between specialist and generalist care.6,19 Specialist care did not significantly reduce the risk of diabetes-related hospitalizations or emergency department visits.20
A REVISED FOCUS FOR STUDYING QUALITY OF CARE
These observations indicate that the magnitude of the difference between specialist and generalist care is inconsequential compared to the magnitude of the overall deficiency in quality of care. Therefore, research examining differences between types of physicians is asking the wrong question; instead, research should be identifying methods to improve quality of care, regardless of the specialty of the providers.
The Cochrane Collaboration’s Effective Practice and Organisation of Care group has developed a conceptual framework for interventions that improve delivery of care (Fig. 2).21 Several groups have systematically reviewed trials of interventions to improve quality of care, both in general,21–25 and for diabetes care in particular.26,27 The interventions that have been evaluated in diabetes care have included educational materials and meetings, local consensus processes, educational outreach visits, audit and feedback programs, reminder systems, changes to the health care team, formal case management programs, and changes in record keeping and communication between professionals. In addition, because diabetes self-management requires the maintenance of a long-term therapeutic alliance among patients, their family members, and their health care providers,28 successful quality improvement interventions could target patients or their families. Such interventions that have been evaluated include individual- or group-based diabetes education programs delivered by various health professionals, telephone- and computer-based education programs, and written educational material for patients.29–31 Notwithstanding the methodological limitations of many of these trials, most interventions have shown limited ability to change the delivery of care, and many areas of the framework for change remain unstudied. Furthermore, educational interventions appear not to be additive: Multiple interventions do not significantly change behavior beyond what is achieved by a single intervention.25 The enormous gaps that remain in our ability to effectively change the delivery of care underline an urgent need to devise interventions to improve care and to test their effectiveness in heterogeneous real-world populations by using pragmatic trials.32
Figure 2.
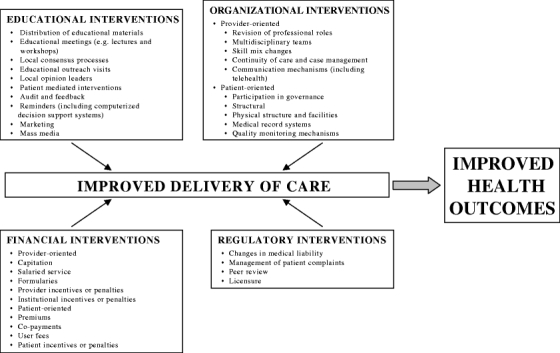
A conceptual framework for interventions to improve quality of care. Adapted from The Cochrane Collaboration’s Effective Practice and Organisation of Care Group.21
However, developing such interventions will not be easy. In 1995, the Veterans Administration (VA) health care system was reengineered by implementing more than 100 interventions to improve quality of care, mostly organizational and educational interventions.33 When compared to the Medicare system, many performance indicators (including annual measurement of A1c and semiannual lipid screening for diabetic patients) improved over the next several years.34 However, many clinical measures continued to have room for improvement; for example, thousands of diabetic patients continued to miss their annual retinal examinations. In decentralized health care systems, such as those available to most patients in most countries, it may be more difficult to apply the comprehensive and resource-intensive interventions that the VA could implement, which would then attenuate any improvement in quality of care that could be achieved. Nonetheless, a recent study did show that halfway through a decade-long government and professional initiative to improve quality of care in the United Kingdom, some improvement in diabetes care was achieved.35
The elusiveness of a “magic bullet” for practice improvement and the systemic barriers to change in many settings should not dissuade efforts to identify interventions, which will produce small but important advances. From the framework for changing practice (Fig. 2), educational interventions to change physician and patient behavior have been studied to some degree, although much more work needs to be done. However, there is a genuine paucity of research examining organizational, financial, and regulatory interventions that change the environment in which care is delivered. Some specific organizational changes that may help improve quality of care include coordinated teams composed of multiple professionals, where each element of care is delivered by the provider with the greatest expertise and experience; information technology to support communication and data transfer within the team of providers and between the team and the patient; and fostering the organizational culture of all stakeholders (providers, institutions, payers, and regulators) to encourage quality through system improvement.36 Financial interventions may include capitation, salary, or pay-for-performance initiatives for primary care physicians,37 while regulatory interventions could include tying licensure to the delivery of quality care.
Ultimately, interventions to improve ambulatory diabetes management will have to meet several objectives to be successful. They will have to be practicable so that they can be implemented within busy clinical practices. Because diabetes is so common, the interventions will need to be affordable to ensure that they can be disseminated widely, and they will have to be generalizable so that they can be used by physicians with different practice styles in different regions and with access to different resources. Finally, to ensure high uptake of the interventions, they will likely need to include some incentives to encourage physicians to use them.
Clinical research continues to find new and better ways of treating diabetes and its complications to reduce the morbidity and mortality for patients with the disease. But the efficacy improvements of these new treatments could be matched by relatively modest increases in the utilization of older, cheaper, and less efficacious predecessor treatments among eligible patients (see Fig. 3). While this calculation may be different were the new treatments vastly more effective than their predecessors, governments are choosing to invest resources in a potentially less efficient way of improving health. The U.S. Congress, for example, budgets just one penny for the Agency for Healthcare Research and Quality to improve quality of care for each dollar budgeted to the National Institutes of Health to fund the development of new treatments, in addition to the billions spent on drug development by the pharmaceutical industry.38 We argue in this paper that no magic bullet for improving quality of care in diabetes has been found, and that attention focused on specialist care is misplaced because of its limited benefits and the financial and human resources implications of increasing specialist care. However, the search for the multiplicity of system and educational, professional, and patient support strategies that will together achieve improved quality surely warrants more investment than the trifling amount it currently receives.
Figure 3.
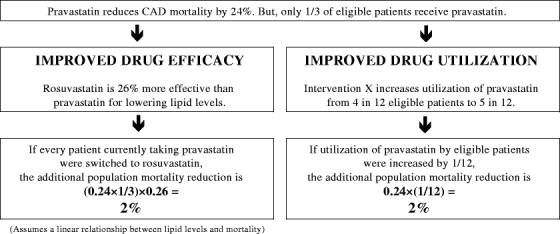
An example from Woolf et al.38 to contrast the impact on population mortality of improving drug efficacy versus improving drug utilization. In this example, developing a new drug, which requires billions of dollars of public and private sector investment, reduces mortality to the same extent as a relatively modest improvement in the utilization of an existing drug might do.
Acknowledgments
Potential Financial Conflicts of Interest: None disclosed.
References
- 1.Lafata JE, Martin S, Morlock R, Divine G, Xi H. Provider type and the receipt of general and diabetes-related preventive health services among patients with diabetes. Med Care. 2001;39:491–9. [DOI] [PubMed]
- 2.De Berardis G, Pellegrini F, Franciosi M, et al. Are type 2 diabetic patients offered adequate foot care? The role of physician and patient characteristics. J Diabetes Complications. 2005;19:319–27. [DOI] [PubMed]
- 3.Brown LC, Johnson JA, Majumdar SR, Tsuyuki RT, McAlister FA. Evidence of suboptimal management of cardiovascular risk in patients with type 2 diabetes mellitus and symptomatic atherosclerosis. CMAJ. 2004;171:1189–92. [DOI] [PMC free article] [PubMed]
- 4.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KMV. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. [DOI] [PubMed]
- 5.Harris SB, Stewart M, Brown JB, et al. Type 2 diabetes in family practice: room for improvement. Can Fam Physician. 2003;49:778–85. [PMC free article] [PubMed]
- 6.Schiel R, Müller UA, Sprott H, et al. The JEVIN trial: a population-based survey on the quality of diabetes care in Germany: 1994/1995 compared to 1989/1990. Diabetologia. 1997;40:1350–7. [DOI] [PubMed]
- 7.Petrelli A, Saitto C, Arca M, Perucci CA. Diabetes management by hospital-affiliated diabetes centres in Lazio, Italy. Eur J Public Health. 2004;14:120–2. [DOI] [PubMed]
- 8.Chuang LM, Tsai ST, Huang BY, Tai TY. The status of diabetes control in Asia: a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabetes Med. 2002;19:978–85. [DOI] [PubMed]
- 9.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–42. [DOI] [PubMed]
- 10.National Committee for Quality Assurance. The State of Health Care Quality: 2005. 2005. Washington, DC, National Committee for Quality Assurance.
- 11.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [DOI] [PubMed]
- 12.Greenfield S, Kaplan SH, Kahn R, Ninomiya J, Griffith JL. Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Ann Intern Med. 2002;136:111–21. [DOI] [PubMed]
- 13.Franciosi M, Pellegrini F, De Berardis G, et al. The QuED Study Group. The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients: an urgent need for better educational strategies. Diabetes Care. 2001;24:1870–7. [DOI] [PubMed]
- 14.De Berardis G, Pellegrini F, Franciosi M, et al. The QuED Study Group. Quality of care and outcomes in type 2 diabetic patients: A comparison between general practice and diabetes clinics. Diabetes Care. 2004;27:398–406. [DOI] [PubMed]
- 15.Shah BR, Hux JE, Laupacis A, Zinman B, van Walraven C. Clinical inertia in response to inadequate glycemic control: Do specialists differ from primary care physicians? Diabetes Care. 2005;28:600–6. [DOI] [PubMed]
- 16.Schaars CF, Denig P, Kasje WN, Stewart RE, Wolffenbuttel BHR, Haaijer-Ruskamp FM. Physician, organizational, and patient factors associated with suboptimal blood pressure management in type 2 diabetic patients in primary care. Diabetes Care. 2004;27:123–8. [DOI] [PubMed]
- 17.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialties. Results from the medical outcomes study. JAMA. 1995;274:1436–44. [DOI] [PubMed]
- 18.Zgibor JC, Songer TJ, Kelsey SF, Drash AL, Orchard TJ. Influence of health care providers on the development of diabetes complications. Diabetes Care. 2002;25:1584–90. [DOI] [PubMed]
- 19.Shah BR, Hux JE, Laupacis A, Zinman B, Austin PC, van Walraven C. Diabetic patients with prior specialist care have better glycaemic control than those with prior primary care. J Eval Clin Pract. 2005;11:568–75. [DOI] [PubMed]
- 20.Huang ES, Gleason S, Gaudette R, et al. Health care resource utilization associated with a diabetes center and a general medicine clinic. J Gen Intern Med. 2004;19:28–35. [DOI] [PMC free article] [PubMed]
- 21.Effective Practice and Organisation of Care Group. [homepage on the internet]. [Accessed 11 January 2006]. Available from: http://www.cochrane.org/reviews/en/topics/61.html.
- 22.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. [DOI] [PubMed]
- 23.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153:1423–31. [PMC free article] [PubMed]
- 24.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003;362:1225–30. [DOI] [PubMed]
- 25.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8. [DOI] [PubMed]
- 26.Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk van JT, Assendelft WJJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001;24:1821–33. [DOI] [PubMed]
- 27.Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427–40. [DOI] [PubMed]
- 28.American Diabetes Association. Standards of medical care in diabetes—2006. Diabetes Care. 2006;29:S4–42. [PubMed]
- 29.Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–87. [DOI] [PubMed]
- 30.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002,25:1159–71. [DOI] [PubMed]
- 31.Deakin T, McShane CE, Cade JE, Williams RDRR. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2005. [DOI] [PubMed]
- 32.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–32. [DOI] [PubMed]
- 33.Kizer KW. The “new VA”: a national laboratory for health care quality management. Am J Med Qual. 1999;14:3–20. [DOI] [PubMed]
- 34.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs health care system on the quality of care. New Engl J Med. 2003;348:2218–27. [DOI] [PubMed]
- 35.Campbell SM, Roland MO, Middleton E, Reeves D. Improvements in quality of clinical care in English general practice 1998–2003: longitudinal observational study. BMJ. 2005;331:1121. [DOI] [PMC free article] [PubMed]
- 36.Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q. 2001;79:281–315. [DOI] [PMC free article] [PubMed]
- 37.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. New Engl J Med. 2006;355:375–84. [DOI] [PubMed]
- 38.Woolf SH, Johnson RE. The break-even point: when medical advances are less important than improving the fidelity with which they are delivered. Ann Fam Med. 2005;3:545–52. [DOI] [PMC free article] [PubMed]


