Abstract
Background
Many medical schools have incorporated the Stages of Change Model into their curricula with specific application to tobacco cessation.
Objective
This study examined the extent to which medical students were prepared to provide stage-based interventions to treat nicotine dependence.
Design
Using a quasi-experimental design, medical students’ counseling interactions were evaluated with a standardized patient portraying a smoker in either the precontemplation or preparation stage of change.
Participants
Participants were 147 third-year medical students at the University of California, San Francisco.
Measurements
Checklists completed by standardized patients evaluated students’ clinical performance. Surveys administered before and after the encounters assessed students’ knowledge, attitudes, confidence and previous experience with treating smoking.
Results
Most students asked about tobacco use (89%), advised patients of the health benefits of quitting (74%), and assessed the patient’s readiness to quit (76%). The students were more likely to prescribe medications and offer referrals to patients in the preparation than in the precontemplation stage of change (P < 0.001); however, many students had difficulty identifying patients ready to quit, and few encouraged patients to set a quit date or arranged follow-up to assess progress. Students’ tobacco-related knowledge, but not their attitudes, confidence, or previous experience predicted their clinical performance.
Conclusions
The findings indicated evidence of students tailoring their counseling strategies to the patients’ stage of change; however, they still could do more to assist their patients in quitting. Additional training and integration of cessation counseling into clinical rotations are needed.
Key words: tobacco treatment, smoking cessation, medical education, training, standardized patients, stages of change model
Cigarette smoking accounts for 440,000 deaths in the US each year and is the leading preventable cause of morbidity and mortality.1 Physician advice doubles the likelihood of patients quitting, and tobacco treatment guidelines recommend that health care providers screen all patients for tobacco use, advise smokers to quit, assess their readiness to quit, and offer appropriate interventions.2–4
Although an estimated 80% of smokers visit a physician annually, most smokers are neither advised to quit nor provided with tobacco cessation treatment.2 Most smokers do not intend to quit in the next month, and it may take several visits for a physician to help a patient through the change process.5
Cessation counseling based on the Stages of Change Model has demonstrated efficacy in helping patients at all stages of change to quit smoking.6–9 The model defines a 5-stage smoking cessation process. Each stage is characterized by a patient’s short and long-term intentions and behaviors, and the model suggests interventions appropriate to each stage.10 In precontemplation, the smoker has no intention to quit in the next 6 months. Recommended interventions include encouraging greater awareness of tobacco use and the benefits of quitting. Contemplators intend to quit, but not in the next 30 days. For these patients, physicians are advised to address barriers and resistance to quitting. Smokers in preparation plan to quit in the next 30 days and report a quit attempt in the past year. For smokers in preparation, clinical strategies are more action-oriented and include setting a quit date, prescribing cessation medications, or recommending participation in a cessation program. Relapse prevention strategies are advised for individuals in the action (smoke-free for less than 6 months) and maintenance (smoke-free for greater than 6 months) stages.
Tobacco cessation training has been shown to increase physician attention to patients’ tobacco use.11 A recent randomized controlled trial of stage-based tobacco training for practicing physicians reported significant improvements in the quality of physicians’ counseling and increases in smokers’ motivation to quit and abstinence rates at one year.12 Many medical schools have incorporated the Stages of Change Model into their curricula with specific application to tobacco cessation; however, students’ ability to apply stage-based strategies in patient encounters has not been studied. Furthermore, in their review of the undergraduate medical education literature, Spangler and colleagues identified the need for studies that evaluate the degree to which tobacco cessation training is retained long-term.13
The purpose of the current study was to evaluate medical students’ skills in providing stage-appropriate smoking cessation counseling to standardized patients representing two different stages of change. We hypothesized that students’ counseling strategies would vary according to the Stages of Change Model, specifically that more action-oriented strategies would be recommended for patients in preparation versus precontemplation. By focusing on third-year medical students, who received stage-based tobacco treatment training in their first year of medical school, we were able to evaluate the degree to which such training was retained. In addition, students’ self-appraisals of their experience, confidence, knowledge, and attitudes were assessed and examined as predictors of counseling performance.
Methods
Setting The study was conducted at the University of California, San Francisco (UCSF) School of Medicine, which uses components of the evidence-based Rx for Change tobacco treatment curriculum and teaches the Stages of Change Model for counseling patients on a variety of health behaviors, including smoking cessation.14 In their first year, the medical students received 2 hours of didactic instruction on stage-based behavioral and pharmacological treatments for nicotine dependence. The lecture was followed by a 2-hour small group session, during which the students role-played counseling interventions in pairs with a variety of patient cases representing different stages of change. In addition, 36% of the students received a 1-hour tobacco treatment review during their third-year family medicine clerkship. This session was offered at only one of the clerkship’s multiple sites. Site assignment was based on random lottery and student preference.
Procedures The study was conducted in December 2005 as part of the mini-clinical performance examination (mini-CPX), a required, formative standardized patient assessment conducted midway through the third year. Standardized patients can simulate clinical situations in a realistic and consistent fashion and have been employed in many medical schools to teach and evaluate students’ clinical skills.13,15During the mini-CPX, each student saw three patients in 17-minute encounters and completed a 10-minute interstation exercise immediately after each encounter. One of the three cases, a patient with a cough, presented the students with an opportunity to offer smoking cessation counseling. Figure 1 provides a brief description of the two versions of the case used in the study. In one version, the patient was not motivated to quit in the next 6 months (stage of change: precontemplation). In the other, the patient was motivated to quit in the next month (stage of change: preparation). We selected these two stages because they are most distinct from each other. Students were randomly assigned by examination day to one or the other version of the case and were not informed that two versions of the case were in use or that the case centered on smoking cessation. The three female actors portraying the case received 15 hours of training that addressed case presentation, checklist completion, and the Stages of Change Model. Because of scheduling conflicts, one actor played only the precontemplation role, while the other two actors played both roles.
Figure 1.
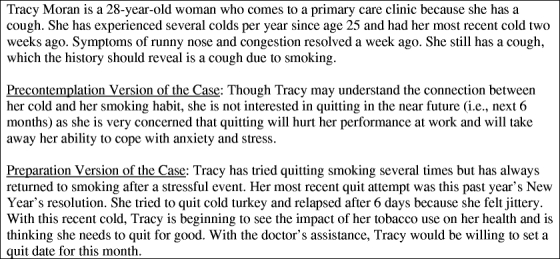
Standardized patient case profile.
Participants Third-year medical students (N = 147), midway through their core clerkships, participated in the study. During the orientation to the mini-CPX, the students were informed of the study described as an examination of student performance with disease assessment and prevention. The study was approved by the UCSF Institutional Review Board.
Measures Three surveys assessed students’ confidence and experience, knowledge and attitudes, and clinical performance in the mini-CPX.Confidence and experience with clinical skills and preventive health counseling were assessed with a 22-item survey, based on work by Wilkerson and Geller, and completed by students before the first mini-CPX clinical station.16,17 Two tobacco-specific items were embedded within the longer questionnaire. The items assessed students’ confidence in providing smoking cessation counseling, with responses ranging from 1 = “not at all confident” to 5 = “extremely confident” and the number of times they had counseled patients about smoking cessation, with responses ranging from 1 = “never” to 5 = “more than 25 times.” The two items correlated (r = .35, p < 0.001) in the current sample.Knowledge and attitudes related to smoking cessation counseling were assessed with a 13-item survey completed by students after the tobacco standardized patient station. Six items assessed students’ tobacco-related knowledge, including their understanding of the Stages of Change Model. An additional item, not included in the knowledge score, asked students to identify the stage of change for quitting smoking of the patient they interviewed. Five items assessed students’ attitudes towards smoking cessation counseling including beliefs that patients are unable to quit or may become angry if asked about their tobacco use and that smoking cessation is not a priority for medicine. Ratings ranged from 1 = “strongly disagree” to 5 = “strongly agree.” The knowledge and attitudinal items were drawn from measures evaluated previously as part of the Rx for Change curriculum.14 A final item assessed students’ readiness to engage in cancer prevention and detection practices.Clinical performance was evaluated with a 46-item checklist completed by the standardized patients after the clinical encounter. The patient/physician interaction was rated using an adaptation of the Common Ground Rating Form.18 The standardized patients used a 6-point rating scale, where 100% = “outstanding” and 0% = “unacceptable,” to evaluate students’ demonstrated competence, information gathering, active listening, exploration of the patient’s perspective, development of personal rapport, and meeting of the patient’s needs. Internal consistency of the total scale score for the current sample was Cronbach alpha = 0.78.Students’ attention to tobacco use was assessed by the standardized patient via checklist items based on the National Cancer Institute’s 5-A’s tobacco treatment framework.3 Points were credited if the student: (1) asked about tobacco use; (2) advised the patient of the health benefits of quitting; (3) assessed the patient’s readiness to quit; (4) assisted with cessation; and (5) arranged a follow-up visit. Points also were gained if the student asked about previous quit attempts and linked the patient’s cough to tobacco use. Assistance with cessation was meant to vary by the patient’s stage of change. For patients in precontemplation, points were given for encouraging the patient to become more aware of her smoking habit and develop coping strategies other than smoking for dealing with stress and anxiety. For patients in preparation, additional points were given for working with the patient to set a quit date, referring the patient to a smoking cessation program or recommending smoking cessation medications. Total possible points for tobacco treatment interventions were 8 for the precontemplation case and 11 for the preparation case. Internal consistency of the total tobacco treatment score was Cronbach alpha = 0.85 and 0.86 for precontemplation and preparation, respectively. The percentage of total possible points attained was calculated to yield a common metric across the two cases.
Analyses Descriptive analyses summarized survey responses. Correlations, paired sample t-tests, and univariate analysis of variance (ANOVAs) tests examined associations among the constructs. Differences in student performance were examined by the stage of change of the standardized patient. The effect of an additional hour of didactic instruction provided during the clerkship year on student performance and survey response also was examined.
Results
Sample Descriptives Data were collected from all 147 students. One of the students, however, did not complete the pre-survey on confidence and experience. The sample was 56% female. Seventy-five students (51%) interviewed the patient in precontemplation, and 72 (49%) interviewed the patient in preparation. There were no differences in student reported confidence, experience, knowledge, or attitudes by patient case version (all P-values > 0.05).
Pre-Survey: Confidence and Experience Eighty-two percent of students reported moderate to extreme confidence in their ability to provide smoking cessation counseling. The mean confidence rating of 3.16 (SD = 0.80) for smoking cessation ranked it sixth among a list of 10 common clinical practices. In paired sample t-tests, students’ confidence ratings for counseling patients about a diagnostic plan, a new medication, an acute problem, or behavior change, in general, were significantly higher than reported confidence for smoking cessation counseling (all P’s < 0.05). The number of times students counseled actual patients for smoking cessation was never (9% of students), 1 to 3 times (40%), 4 to 9 times (34%), 10 to 25 times (14%), and more than 25 times (3%).
Post-Survey: Knowledge and Attitudes The students averaged 72% correct (SD = 17; range: 17% to 100%) on the tobacco-related knowledge items. Most students (74%) underestimated the percentage of smokers who see a physician annually. Nearly all students (97%) correctly identified the Stages of Change Model as providing a framework for understanding patients’ readiness to quit smoking; however, only 50% correctly identified their patient’s stage of change. Correct stage identification differed significantly by the patient’s readiness to quit with 71% of students correctly identifying the patient in precontemplation compared to 28% for the patient in preparation (χ2 = 27.03, df = 1, P < 0.001). Fifty-seven percent of students who saw the patient in preparation staged the patient in the earlier stage of contemplation.All students (100%) reported actively engaging in cancer prevention and detection practices during actual patient encounters. On the attitudinal items, only 2 students (1%) reported not asking about smoking because they believed patients would not be able to quit; 6 (4%) reported reluctance to take away an enjoyable and rewarding activity from their patients; and 4 (3%) believed smoking cessation is not a priority for medicine. Twenty-six percent expressed concern that asking about smoking might make patients angry or defensive. Most students (69%) believed patients would probably follow their recommendations to quit smoking.
Counseling Interaction Table 1 summarizes combined and stage-specific performance on the mini-CPX smoking cessation case. Most students asked about tobacco use (89%), advised patients of the health benefits of quitting (74%), and assessed the patient’s readiness to quit smoking (76%), with no difference by case version. A few students assisted patients in precontemplation by encouraging them to become more aware of their smoking (14%) or by encouraging coping strategies to manage stress and anxiety without smoking (14%). As hypothesized, and consistent with the Stages of Change Model, students who saw patients in the preparation stage were more likely to recommend pharmacotherapy for quitting smoking (P < 0.001) and refer patients to a quit smoking program (P < 0.001). A few students (18%), however, encouraged patients in preparation to set a quit date. Only 13% of students who saw the patient in preparation set a quit date, recommended medications, and provided treatment referrals; 47% engaged in at least two of the practices, 14% engaged in one, and 26% engaged in none.Students obtained a mean of 55% (SD = 0.28) of the possible points for tobacco treatment strategies with no difference by the stage of change of the patient case: precontemplation = 55% (SD = 0.28) and preparation = 56% (SD = 0.27). Higher tobacco treatment total scores were associated with greater knowledge (r = 0.19, P = 0.02), but not confidence (r = 0.05) or experience (r = 0.07). Lower tobacco treatment scores were associated with beliefs that asking about smoking might make patients angry or defensive (r = −0.17), that smoking is an enjoyable and rewarding activity for patients (r = −0.17), and that smoking cessation is not a priority for medicine (r = −0.19; all P’s < 0.05).Students averaged 76% (SD = 0.09) on the patient/physician interaction total score, scoring lowest on personal rapport (M = 72%, SD = 0.16) and highest on professional competence (M = 80%, SD = 0.13). The patient/physician interaction score may be influenced by the actor who rated the case. Controlling for the patient–actor, performance in the mini-CPX as assessed with the patient/physician interaction total score was unrelated to students’ tobacco-related confidence (partial r = 0.10), experience (partial r = 0.12), or knowledge (partial r = 0.13) (all P-values > 0.10) but was significantly correlated with the tobacco treatment interventions provided (partial r = 0.21, P < 0.01). That is, students who more comprehensively addressed patients’ tobacco use achieved higher clinical performance scores.
Table 1.
Combined and Stage-Specific Scoring for Tobacco-Related Standardized Patient Exam
| Precontemplation (n = 75) (%) | Preparation (n = 72) (%) | Overall (N = 147) (%) | |
|---|---|---|---|
| Asked patient about tobacco use | 87 | 92 | 89 |
| Asked patient about prior quit attempts | 68 | 72 | 70 |
| Assessed patient’s readiness to quit | 77 | 74 | 76 |
| Linked patient’s cough to tobacco use | 80 | 81 | 80 |
| Advised patient of health benefits of quitting | 72 | 76 | 74 |
| Encouraged patient to become more aware of smoking behavior and triggers to smoke | 9 | 19 | 14 |
| Addressed coping strategies for patient’s stress and anxiety alternative to smoking | 9 | 18 | 14 |
| Encouraged patient to set a quit date* | 17 | 18 | 18 |
| Recommended medications for quitting*† | 37 | 69 | 53 |
| Referred patient to a quit smoking program*† | 17 | 58 | 37 |
| Scheduled a follow up visit to re-evaluate patient’s tobacco use/quit attempt | 40 | 33 | 37 |
*Stage-appropriate for preparation case, but not precontemplation case.
†Indicates P < 0.05 for group comparison by patient version (precontemplation or preparation).
Clerkship Training Students who received the additional 1-hour didactic tobacco review during their family medicine clerkship reported greater experience with tobacco treatment (M = 2.9, SD = 1.0) compared to those who did not receive the review (M = 2.4, SD = 0.8; P = 0.002 for mean difference), and were significantly more likely to assess patients’ readiness to quit smoking (85% vs 70%), encourage patients to become more aware of their smoking behavior (23% vs 10%), set a quit date (26% vs 13%), and schedule a follow-up visit (47% vs 31%) (all P’s < 0.05). There were no differences in identification of patient’s tobacco use or correct stage of change, recommendation of medications or referrals, knowledge of tobacco treatment, confidence level, or tobacco-related attitudes.
Discussion
In a standardized patient evaluation, most medical students assessed tobacco use, advised patients of the health benefits of quitting smoking, and assessed their readiness to quit—all activities that should be incorporated in treating tobacco-dependent patients. Furthermore, as hypothesized, the students tailored their cessation strategies based on the patient’s stage of change. Specifically, the students were more likely to prescribe medications and provide cessation referrals to patients in the preparation stage of change. Seventy-four percent of students who saw the patient in preparation offered some type of active intervention, compared to 47% of those who saw the patient in precontemplation.
The medical students were trained to provide smoking cessation counseling based on the Stages of Change Model, and they demonstrated knowledge of the model. Most of the students who saw the patient in precontemplation correctly identified her stage. However, for the patient in preparation, many of the students had difficulty identifying that she was ready to quit in the next 30 days, and instead, staged her in contemplation. This mis-staging may have contributed to the finding that only 18% worked with the patient to set a quit date. Correct identification of the immediacy with which patients intend to quit smoking would likely increase the provision of active interventions. Our results indicate that students may be less skilled in identifying and treating a patient who is in preparation. The study findings parallel those of Parish and colleagues’ study with standardized patients for assessment of stage-based substance abuse counseling, which found that internal and family medicine residents performed better in general communication than in assessment or clinical management of patients’ drug abuse.19
A recent survey of 12 U.S. medical schools reported that 11 included training on the Stages of Change Model, and 10 believed that their graduating students knew how to intervene with patients at various stages.20 Such perceptions can be verified by incorporating cases that assess stage-based tobacco treatment skills into existing standardized patient exercises.
In the current study, students with greater tobacco-related knowledge addressed patients’ smoking more comprehensively supporting the value of didactic instruction. Students who received the additional tobacco review during their family medicine clerkship reported more experience and engaged in more tobacco treatment strategies. The clerkship didactic occurred 1 to 28 weeks before the mini-CPX. Informal inquiry with the other UCSF third-year clerkship directors indicated no other formal tobacco treatment training activities. Greater attention to tobacco treatment during third-year clerkship clinical rotations would likely expand students’ repertoires of tobacco treatment strategies. Recent studies indicate success in increasing medical students’ actual treatment of tobacco dependence when cessation counseling protocols are integrated into clinical training.21 To be successful, clerkship preceptors, who themselves may lack adequate preparation to treat tobacco dependence, also may require additional training.22
While endorsed by a few students, negative attitudes towards tobacco treatment were associated with less attention to tobacco use in the clinical encounter, indicating that negative attitudes likely serve as barriers to treatment. Modeling from faculty members may play an important role in increasing the perceived priority of tobacco cessation in medicine and decreasing student concerns that clinical rapport will be harmed if patients’ tobacco use is addressed.
The current study is limited to one training site, with a single standardized patient encounter, and may not generalize to other programs. Strengths of the study include the 100% student participation rate, examination of retention of tobacco training, and use of standardized patients, which allow for assessment of skills in a clinically realistic and standardized manner.
The findings demonstrate that after a tobacco curriculum based on the Stages of Change paradigm, medical students identified patients’ tobacco use and were able to tailor their treatment strategies to patients’ readiness to quit. Greater integration of tobacco treatment into clerkship rotations may serve to further reinforce the value and importance of treating patients’ tobacco use and increase students’ expertise with treating this deadly addiction.
Acknowledgements
This work was supported by the National Cancer Institute (#R25 CA96975), the National Institute on Drug Abuse (#K23 DA018691 and #P50 DA09253), the State of California Tobacco-Related Disease Research Program (#13KT-0152), Haile T. Debas Curriculum Innovations Award (UCSF School of Medicine), and the Health Resources and Services Administration (#D56HP00042). We thank Bernie Miller, Jewel Smally, and Ann Magdalen for overseeing the patient–actors and survey data collection; LuAnn Wilkerson, MD for commenting on an earlier version of this manuscript; and Kathleen Kerr for editorial assistance.
Potential Financial Conflicts of Interest None disclosed.
References
- 1.Centers for Disease Control. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States, 1995–1999. MMWR. 2002;51:300–3. [PubMed]
- 2.Silagy C, Stead LF. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2001(2):CD000165. [DOI] [PubMed]
- 3.Glynn TJ, Manley MW. How to help your patients stop smoking: a National Cancer Institute manual for physicians: USDHHS, Public Health Service, NIH, National Cancer Institute, 1990.
- 4.U.S. Public Health Service. A clinical practice guideline for treating tobacco use and dependence. J Am Med Assoc. 2000;283:3244–54. [DOI] [PubMed]
- 5.Velicer WF, Fava JL, Prochaska JO, Abrams DB, Emmons KM, Pierce JP. Distribution of smokers by stage in three representative samples. Prev Med. 1995;24:401–411. [DOI] [PubMed]
- 6.Pieterse ME, Seydel ER, De Vries H, et al. Effectiveness of a minimal contact smoking cessation program for Dutch general practitioners: a randomized controlled trial. Prev Med. 2001;32:182–190. [DOI] [PubMed]
- 7.Prochaska JO, Velicer WF, Redding C, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med. 2005;41:406–16. [DOI] [PubMed]
- 8.Prochaska JO, Velicer WF, Fava JL, et al. Counselor and stimulus control enhancements of a stage-matched expert system intervention for smokers in a managed care setting. Prev Med. 2001;32:23–32. [DOI] [PubMed]
- 9.Valanis B, Lichtenstein E, Mullooly JP, et al. Maternal smoking cessation and relapse prevention during health care visits. Am J Prev Med. 2001;20:1–8. [DOI] [PubMed]
- 10.Prochaska JO, DiClemente CC. Stages and processes of selfchange of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. [DOI] [PubMed]
- 11.Lancaster T, Silagy C, Fowler G. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2000:CD000214. [DOI] [PubMed]
- 12.Cornuz J, Humair J-P, Seematter L, et al. Efficacy of resident training in smoking cessation: a randomized, controlled trial of a program based on application of behavioral theory and practice with standardized patients. Ann Intern Med. 2002;136:429–37. [DOI] [PubMed]
- 13.Spangler J, George G, Foley K, Crandall S. Tobacco intervention training: current efforts and gaps in US medical schools. J Am Med Assoc. 2002;288:1102–9. [DOI] [PubMed]
- 14.Hudmon KS, Corelli RL, Chung E, et al. Development and implementation of a tobacco cessation training program for students in the health professions. J Cancer Educ. 2003;18:142–9. [DOI] [PubMed]
- 15.Ferry LH. Overcoming barriers to nicotine dependence treatment. Primary Care. 1999;26:707–46. [DOI] [PubMed]
- 16.Wilkerson L, Lee M, Hodgson CS. Evaluating curricular effects on medical students’ knowledge and self-perceived skills in cancer prevention. Acad Med. 2002;77(10 Suppl):S51–3. [DOI] [PubMed]
- 17.Geller AC, Prout MN, Miller DR, et al. Evaluation of a cancer prevention and detection curriculum for medical students. Prev Med. 2002;35:78–86. [DOI] [PubMed]
- 18.Lang F, McCord R, Harvill L, Anderson DS. Communication assessment using the common ground instrument: psychometric properties. Fam Med. 2004;36:189–98. [PubMed]
- 19.Parish SJ, Ramaswamy M, Stein MR, Kachur EK, Arnsten JH. Teaching about substance abuse with objective structured clinical exams. J Gen Intern Med. 2006;21:453–9. [DOI] [PMC free article] [PubMed]
- 20.Powers CA, Zapka JG, Bognar B, et al. Evaluation of current tobacco curriculum at 12 US medical schools. J Cancer Educ. 2004;19:212–9. [DOI] [PubMed]
- 21.Nieman LZ, Velasquez MM, Groff JY, Cheng L, Foxhall LE. Implementation of a smoking cessation counseling module in a preceptorship program. Fam Med. 2005;37:105–11. [PubMed]
- 22.Slatt LM, Frasier PY, Strayhorn G, Kowlowitz V. Prevention practices of family medicine clerkship preceptors in North Carolina. Acad Med. 2001;76:722–6. [DOI] [PubMed]


