Abstract
General Internal Medicine (GIM) faces a burgeoning crisis in the United States, while patients with chronic illness confront a disintegrating health care system. Reimbursement that rewards using procedures and devices rather than thoughtful examination and management, plus onerous administrative burdens, are prompting physicians to pursue specialties other than GIM. This monograph promotes 9 principles supporting the concept of Coordinated Care—a strategy to sustain quality and enhance the attractiveness and viability of care delivered by highly trained General Internists who specialize in the longitudinal care of adult patients with acute and chronic illness. This approach supplements and extends the concept of the Advanced Medical Home set forth by the American College of Physicians. Specific components of Coordinated Care include clinical support, information management, and access and scheduling. Success of the model will require changes in the payment system that fairly reimburse physicians who provide leadership to teams that deliver high quality, coordinated care.
KEY WORDS: practice model, coordinated care, General Internal Medicine, chronic disease, primary care
A DISINTEGRATING HEALTH SYSTEM FOR PATIENTS WITH CHRONIC ILLNESS
General Internal Medicine (GIM) has entered a challenging period. After several years of national attention and growth, interest has waned. The number of physicians choosing to practice GIM in a primary care setting has decreased by 50% in the past 5 years, and many physicians who have been practicing GIM are now abandoning it. Some academic medical centers are eliminating primary care from their organizations altogether. Why is General Internal Medicine perceived by trainees and experienced by practitioners to be so undesirable? Can anything be done to improve the perception and the Practice of General Internal Medicine?
Paradoxically, this exodus and contraction is occurring at a time when well-trained, well-supported Internists are more essential than ever. Health care has grown more complex: more patients have more chronic illness that requires coordination by a highly trained specialist in adult medicine. In 2005, 133 million Americans (45% of the population) had a chronic condition; approximately 60 million (24% of the population) suffered from multiple chronic conditions, and this number is projected to increase to 81 million (25%) by 2020. 1,2 Care for this type of patient is complex and expensive. Total yearly medical expenditures for a person with a chronic condition ($6,032) are more than 5-fold higher than for a healthy person ($1105) (Fig. 1). 3 From a national perspective, direct medical costs of chronic diseases were $510 billion in 2000 and are expected to rise to more than $1 trillion by 2020, and nearly 80% of this is apt to be spent on patients with chronic illnesses.4 Health care spending for a person with one chronic condition is 2 1/2 times greater than spending for someone without any chronic condition, while spending is almost 15 times greater for someone with 5 or more chronic conditions, translating into more than $15,000 per beneficiary annually (Fig. 3). Thus, care for patients with multiple chronic conditions demands a level of support and a working environment that is vastly different from that required for less complex acute care or prevention.
Figure 1.
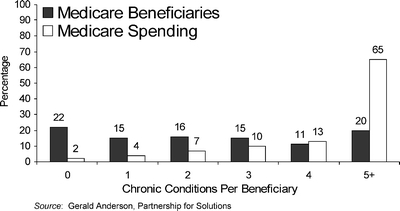
Medicare spending for beneficiaries with chronic conditions.
Figure 3.
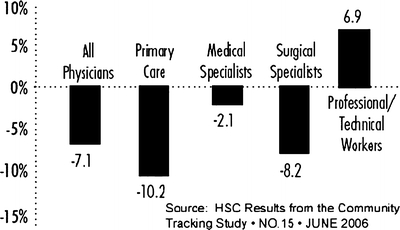
Percent change in the average income of physicians compared with other professional/technical workers, adjusted for inflation, 1996–2000.
The care of such patients has become progressively more fragmented as specialists, who make up the preponderance of the physician workforce, attend to only 1 disease or 1 organ system. Although most General Internists report that demand for their services far outstrips their capacity, decreasing reimbursement for their services coupled with excessive administrative burdens are making this discipline unattractive, if not untenable, for many highly trained physicians.
It is unlikely that this situation can be sustained for many more years before the fabric of health care in the United States begins to rapidly and visibly disintegrate. Health care in the United States is extraordinarily expensive, consuming nearly 15% of the United States gross domestic product in 2002 and projected to grow to more than 18% in 2013, with annual expenditures of $3.4 trillion.5 Despite this vast expenditure, the health care received by most Americans is at best mediocre compared with the rest of the developed world. In a study of approximately 4,600 randomly selected adults from 12 U.S. cities, only slightly more than half received recommended preventive, acute, or chronic care.6 Moreover, these deficiencies respect neither ethnic nor socioeconomic boundaries and are equally pervasive throughout the population. There is substantial evidence that the delivery system is inefficient and wasteful, as illustrated by the fact that 1 in 7 hospital admissions is prompted by poor access to a patient’s medical records, 12% of physicians’ orders are not executed as written, and 20% of laboratory tests are requested because prior results are not readily available.7
Many experts attribute these problems to a fragmented health care system that lacks the structure and tools to genuinely improve quality. Almost all financial incentives favor volume over quality and high-tech procedures over personalized care and prevention.
EFFECT OF THE DYSFUNCTIONAL PAYMENT SYSTEM ON COGNITIVE SPECIALTIES
The care of complex patients with multiple chronic illnesses requires careful management by thoughtful physicians who have the scope of expertise and are able to devote the time to understanding all of the active problems and how they interact and affect the patient. As opposed to physicians who spend most of their time performing procedures, these physicians are often referred to as cognitive specialists because they devote most of their time and effort to interviewing, examining, treating and counseling patients. The environment for these cognitive specialists, who include primary care physicians (General Internal Medicine, Pediatrics, and Family Medicine), non-procedural medical subspecialists (e.g., Endocrinology, Rheumatology, Genetics, and Infectious Diseases), and other medical fields (e.g., Psychiatry), is becoming increasingly hostile. The demands of this type of clinical practice have increased dramatically, while remuneration has steadily declined in relative terms. During the period 1995–2005, physicians spent an increase amount of time on direct patient care, which is defined as face-to-face contact with patients, patient record keeping and office work, travel time connected with seeing patients, and communication with other physicians, hospitals, pharmacies, and others on a patient’s behalf.
As a result, the number of physicians entering these fields has dropped precipitously, and serious shortages of such physicians are predicted (Fig. 2). Conversely, physicians in specialties that entail performance of technical procedures have experienced dramatic improvements in their practice environments and have been able to effectively limit their working hours while incomes have risen more briskly. Correspondingly, procedural specialties are now viewed as more appealing than cognitive specialties and are attracting record numbers of trainees. Even within Internal Medicine, the number of physicians entering the higher paid procedural specialties such as Interventional Cardiology, Gastroenterology, and Nephrology has steadily risen over the past decade, whereas that entering cognitive specialties such as Endocrinology, Infectious Diseases, and Rheumatology that provide long-term care to patients with serious chronic diseases such as diabetes, HIV/AIDS, and rheumatoid arthritis, has been slowly decreasing, as has the number of medical school graduates electing to enter General Internal Medicine.
Figure 2.
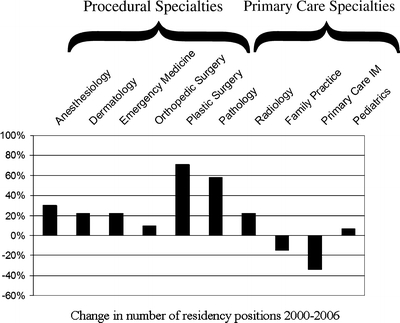
Change in number of residency positions 2000–2006.
The major reason for this shift has been a system of reimbursement that rewards the diagnosis and treatment of disease with procedures and devices rather than primarily with careful examination and management. Between 1999 and 2003, payment for imaging services grew by 45%, and in 2004, the cost of imaging to all payers was approximately $100 billion, equivalent to $350 per person in the United States.8 For reading an ultrasound image, the radiologist, who may never actually see the patient, is paid as much or more than a cognitive specialist who thoughtfully interviews and examines the patient, determines the need for and orders the ultrasound examination, and ultimately, crafts a treatment plan. Although the rationale for this disparity may be that procedures and devices are easily counted and controlled, the net result is increasingly to drive the medical care system toward an impersonal, technological, and expensive approach to care.
General Internal Medicine is a prototypical cognitive specialty with few procedures and has suffered declining fortunes along with the others. Disparities in financial rewards coupled with high levels of indebtedness plus a higher perceived job satisfaction and better lifestyle in other medical specialties are the major factors driving trainees away from primary care. High-tech proceduralists are paid vastly more than physicians whose work is mainly cognitive, and trainees have taken notice. The national average compensation of a Dermatologist is twice that of a General Internist or a Family Physician, while that of an Orthopedic Surgeon is nearly 2 1/2 times higher. In some community settings, the disparity can be much greater, with proceduralists earning up to 6 times as much as a cognitive specialist. This is not necessarily to argue for parity, but to highlight explicitly the power of the incentives that are presently operating in the medical marketplace. Moreover, although in real terms the income of physicians has declined in recent years, that decline has been much more severe for physicians engaged in primary care practice (Fig. 3).
It should be noted that in some countries, England, for example, the incentives are tilted in precisely the opposite direction. Generalist Physicians there are now paid on average more than specialists to attract the best and brightest into general practice and reward efficient, high quality care.
Many cognitive physicians in the United States, such as General Internists, practice in settings in which it is difficult to deliver optimal health care to patients over time. Heavy demands for productivity, micromanagement by insurers, and limited practice support have eroded continuity and opportunities for truly personalized care. Performance of Generalist Physicians is measured in terms of numbers of visits, patients, or relative value units (RVUs), rather than results or quality. Current attempts to address these problems, such as typical disease management programs, that are external to the physician’s practice rather than integrated with it, may produce targeted improvements but also lead to more fragmentation and disease-centric care. These circumstances can easily lead to higher use of medical services (including procedures), lower quality, and higher costs. It is for this reason that every other developed country in the world has a health care system that links each patient to a generalist provider. Accumulating evidence supports the model of care where the patient has a strong relationship with a primary care physician as improving quality of care and lowering costs. Continuity of care is a prime determinant of patient satisfaction.9 Ironically, wealthier patients have recognized these problems and now often seek out “boutique” physicians who have divorced themselves from the systems that pay for disease care and offer a more comprehensive model focused on maintaining health. This reflects the fact that practically no patient wants production line, generic care, and that when substantial economic incentives exist, personalized, continuous care is available. 
The United States has reached a crossroad. Unless the decline in cognitive specialists is reversed and new approaches to care for chronic illness are made readily available to all who need them, our health care system will continue to disintegrate and grow unaffordable to the majority of Americans. Patients will undergo an endlessly growing number of expensive procedures for a diminishing benefit. The elderly, who use most of the health services in this country, will continue to find themselves increasingly adrift in a complex system, required to shuttle on their own between single system specialists, each armed with a procedure. Rather than simply accept this inevitability, the alternative is to create a rational system in which all components of care are sensibly integrated within a highly functional environment that is strongly anchored by a skillful Generalist Physician who is able to match the medical needs and personal preferences of individual patients to the complex array of available tests and therapies. This physician is truly a specialist in managing complex, chronic illness. Although only a limited number of highly integrated systems such as the Veterans Health Administration and group-model health maintenance organizations have begun to move toward this goal, it is possible to envision other settings in which this type of care could readily be provided. Achieving this goal will require vision and commitment by the medical profession and by policy makers as well as a serious restructuring of the current methods of paying for health care.
In the remainder, we highlight principles of effective care for patients with chronic illness and suggest a potential strategy forward. We also address the special role of academic General Internists in addressing this impending crisis.
CREATING A PRACTICE MODEL FOR CHRONIC ILLNESS THAT WORKS—COORDINATED CARE
For the past three decades, the predominant approach to delivery of routine health for most Americans has been a primary care model. Several groups, including the Institute of Medicine, have carefully delineated the essential attributes of effective primary care. Although these remain thoroughly  relevant to the provision of high quality health care, they are general attributes and do not provide detail about how they might be effectively translated into the delivery of care in real world settings such as that described above.
relevant to the provision of high quality health care, they are general attributes and do not provide detail about how they might be effectively translated into the delivery of care in real world settings such as that described above.
More recently, professional organizations such as the American College of Physicians (ACP) and the American Academy of Family Practice (AAFP) have issued very thoughtful and forward thinking position papers that address the current plight of Generalist Physicians. These statements also set forth potential solutions that might help to resurrect the important role of generalists. The ACP has proposed the concept of the Advanced Medical Home consisting of a competent team, including a physician specialist in complex, chronic care management, and coordination and active involvement by informed patients.10 To facilitate this initiative, ACP has called for:
A comprehensive public policy initiative that would fundamentally change the way that care is delivered to patients by linking them to a qualified practice.
Fundamental changes in third party financing, reimbursement, coding, and coverage policies to support practices that qualify as advanced medical homes.
Fundamental changes in workforce and training policies to assure an adequate supply of physicians who are trained to deliver care in this model.
Research and pilot testing on the advanced medical home model and a revised reimbursement system.
AAFP has also issued policy statements supporting the notion of a medical home.11
We applaud and endorse these efforts and hope that the efforts of Society of General Internal Medicine (SGIM) will support and bolster those of our colleagues in those other organizations. We now propose a set of adjunctive principles that are intended to supplement the work of other organizations by establishing an approach that will sustain quality and enhance the attractiveness and viability of care delivered by highly trained General Internists who specialize in the provision of coordinated, longitudinal care of adult patients with acute and chronic illness. These principles address critical components of health care delivery such as clinical support, organization, information management, and access. We discuss the implications for training and for future research.
Primary Care Versus Coordinated Care
In the early 1970s, it was recognized that the rapidly increasing specialization of physicians was leading to care that was fragmented and focused on specific organ systems rather than whole patients. Furthermore, the care was expensive and lacked sufficient emphasis on prevention. The primary care movement was established in response to these circumstances. Over the ensuing three decades, however, the term primary care has come to subsume several types of health care that include:
very basic care provided by allied health professionals who manage relatively simple problems and refer other problems to specialists;
care provided by family physicians that includes components of Pediatrics, Internal Medicine, Obstetrics and Gynecology, Orthopedics, General Surgery, and other disciplines; and
General Internal Medicine which focuses exclusively on acute and chronic medical problems of adults.
Although all of these types of care share certain elements such as a focus on prevention and provision of first contact care, they also differ in important ways. GIM, in particular, focuses on providing care to patients with multiple chronic conditions. For the purposes of this report, we concentrate on the demands of providing effective, high-quality care to adults with multiple chronic conditions. Management of these patients represents a special type of primary care that is very different from the episodic care for acute illness and prevention that otherwise healthy individuals require. Because of these differences, we refer to this type of health care as Coordinated Care as distinct from the more general term, Primary Care. Coordinated Care is also very different from the disease-based approach to care that is encouraged by our present system of payment. Coordinated Care embodies a true system of care in which continuity, coordination, comprehensiveness, and patient-focus, as a whole, are the goals.
PRINCIPLES OF COORDINATED CARE THAT IS EFFECTIVE, EFFICIENT AND REWARDING
-
Coordinated care should be viewed as a process rather than a series of episodes.
The organization and financing of the current health care system is oriented around the notion that certain events, such as scheduled or unscheduled visits, constitute the central activity of health care delivery. This view of health care as episodic for persons with chronic illness should be abandoned. The delivery and payment systems must be reoriented toward supporting longitudinal and continuous care that provides and maintains meaningful improvements in health.
-
Patients value and benefit from a longitudinal relationship with a highly trained physician who understands the context of all their conditions and personal circumstances.
Patients’ satisfaction is directly related to continuity of care, yet little noticed over the past decade has been the disintegration of the fundamental value of a long-standing relationship between a capable physician and a patient. Propelled by frequently changing insurance coverage, constant changes in benefits and eligibility for covered services, complex physician coverage systems, confusing procedures for access, and a piecework mentality toward measuring productivity, any semblance of continuity of care has evaporated for many patients. Not only has this produced frustration and dissatisfaction on the part of both the providers and recipients of health care, but has also caused fragmentation and unnecessary health services. Patients with sufficient financial means have sought to recover continuity with their physician in expensive “boutique” practices seeking the undivided attention of their personal physician.
-
A well-organized team of capable health care providers, coordinated by a knowledgeable and well-trained General Internist is optimally suited to providing Coordinated Care. Described in greater detail below, the composition of the team comprised of medical and nonmedical personnel working closely together to assure accessibility, continuity, and high quality care that includes effective communication with, education of, and outreach to patients.
The current primary care practice model is inefficient for patients with chronic illness and is economically unsustainable. Ultimately, providing care efficiently and satisfying both patients and providers will depend upon delegating and matching the manifold tasks of patient care to members of an integrated team, according to their individual competencies. Long-held traditions, limitations of information systems, and restrictions imposed by the reimbursement system are presently barriers to developing more efficient and effective approaches to longitudinal care. In a few other sectors of the economy is the highest level professional responsible for the majority of production, customer service, and clerical work. The ever-growing burden of administrative tasks is perceived by established physicians and trainees as a major disincentive to remaining in or entering GIM. Given the expense of training and the impending shortage of qualified physicians, it is not only sensible but essential that the unique competencies of physicians be utilized to their fullest. These include the synthesis of large volumes of complex medical information, estimations of risks and benefits customized to the individual patient, and the recognition of biological, psychosocial, and economic factors in the management of health and disease. Without sacrificing the ability of a physician to establish a long-standing, personal relationship with his or her patients, models of care that provide effective, efficient, and personalized longitudinal care must be created. In some settings, General Internists may have to abandon the ideal of providing all care to their patients (e.g., ordinary acute care and routine follow-up for stable chronic illness). The trade-off for this sacrifice is improved access and greater availability of the physician for complex problems.
-
Capable use of a comprehensive, functional electronic health record (EHR) is critical to high quality practice—especially for care of chronically ill patients.
Central to the concept of providing effective Comprehensive Care is the availability of a full-featured EHR that makes all essential data readily available to the health care team, facilitates communication between team members, and simplifies tasks such as order entry. When properly implemented, EHRs have been shown to reduce errors. In routine practice, most errors are a result not of poor judgment but of deficient management of information such as difficulties with the gathering and display of information, breakdowns in communication among multiple care providers, incomplete data, or failure to act on critical information. Although there are many barriers to full and widespread implementation of the EHR in the outpatient setting, the burgeoning amount and complexity of clinical information facing providers make it essential. Health care systems such as the Veterans Health Administration have demonstrated that a fully deployed and functional EHR can support the delivery of quality less expensively than in most other parts of the health care sector.
For these systems to be embraced by practitioners, however, they must be time-neutral or time-saving. Moreover, they should not be used to add additional clerical duties to already overtaxed physicians. Medical information that is consolidated, concise, standardized in format, contextualized, presented “just-in-time”, and processed only once by the physician facilitates the complex cognitive tasks involved in coordinated care. Information presented in this manner minimizes errors, increases efficiency, and makes the process of care more rewarding for the patient and the providers.
-
Payment mechanisms must be modified to support coordinated care.
Current payment mechanisms for care of chronic illness are woefully inadequate. As noted above, these mechanisms largely pay only for face-to-face visits with a single provider. This type of encounter represents only one aspect of high-quality coordinated care; payment mechanisms focused exclusively on the face-to-face visit do not lend themselves to care by a coordinated team. In some integrated health care systems, up to 25% of patient encounters now occur via secure e-mail systems. Some health care systems are also deploying internet-based applications for managing patients. As advocated by the ACP in its recent position statement, payment should be available for physician services that provide essential oversight and coordination of other practitioners who participate in delivering care. In addition, current payment mechanisms do not account for the fact that much of the important work of patient care occurs outside of face-to-face visits. This includes communication between health care providers and patients and among health care providers. Effective use of staff, educational and community resources, and electronic forms of communication can create an environment in which health problems and concerns are addressed promptly, effectively, and efficiently. These activities have the potential to prevent more serious problems and avert costs related to avoidable visits and hospital admissions. At present, however, there is essentially no mechanism to pay for these activities, which in the long-run, adds to the cost of medical care and detracts from quality.
-
The infrastructure necessary for coordinated care must also support acute symptom evaluation and prevention.
Patients with chronic problems and generally healthy patients who have not yet developed a chronic illness still require prompt evaluation and effective management for acute intercurrent symptoms and comprehensive prevention and health maintenance. Clinical support systems, EHRs, coding schemes, and payment mechanisms should be constructed to accommodate these functions as well. The clinical environment should provide easy and convenient access as patients have made it abundantly clear that they do not want to pay for care that is inconvenient or not perceived to meet their needs.
-
The health care system and physicians must be accountable to patients and payers.
General Internists have led the health professions in defining methods to measure the quality of processes and outcomes of care. In the care of an individual patient with multiple medical problems, however, a new generation of performance measures is necessary to define the outcomes of longitudinal coordinated care. Current measures largely reflect actions taken as part of episodic care and are not geared to long-term coordinated care. General Internists need to provide leadership in establishing a new generation of “tightly linked measures” as described by Kerr and her colleagues.12 These measures should be hierarchical in nature and recognize the competing demands that derive from multiple conditions and need to set priorities.
-
Trainees in Internal Medicine must learn in settings in which high quality coordinated care is practiced.
The basic structure of training in Internal Medicine has been relatively static for several decades and no longer provides much of the knowledge, skills, and attitudes necessary to be a successful General Internist. This has, in part, been responsible for the decreasing attractiveness of Internal Medicine, in general, and GIM specifically. Unless the current generation of physicians is well schooled in not only traditional areas of disease etiology, diagnosis, and treatment, but also use of information systems, care coordination, and quality improvement, they will be doomed to fail in the practice of 21st century medicine. In fact, these reforms must be extended back into medical school before the point when medical students start to make long-term career decisions. To successfully address these deficiencies in training, new mechanisms to fund Graduate Medicine Education will be necessary. So long as essentially the sole source of federal support for training of physicians derives from payment to hospitals, genuine and necessary reforms in medical education will not be possible.
-
Researchers in GIM must aggressively design and test innovative methods for delivering coordinated care.
Academic generalists in many settings have fallen behind forward-thinking community providers in designing new approaches to care. Partnerships between these physicians and other health professionals practicing in academic and community setting need to collaborate to design and test improved system designs. The Centers for Medicare and Medicaid Services (CMS) and other entities have begun to fund pilot projects. But without rigorous evaluation, it may not be possible to generalize the successes and failures of these projects to other settings. This presents an ideal opportunity for collaboration between physicians in private practice and academic setting. Unfortunately, few if any of these demonstration projects are being conducted in academic General Internal Medicine Clinics where residents are being trained. The opportunities to engage trainees in innovative efforts to improve health care for chronic conditions will provide them with a broad set of skills and experiences that will be valuable throughout their careers.
A PROPOSED MODEL FOR PROVIDING COORDINATED CARE
The key to providing high caliber coordinated care by a General Internist will be to create a practice environment that incorporates improvements in workflow and information management, but still retains the essential characteristics of primary care models such as maintaining a trusting, long-term relationship with the patient. In the new model, the pre-appointment, intra-appointment, and post-appointment work are designed to maximize the quality and efficiency of the patient care encounter and to optimize the satisfaction of patients, staff, and physicians. The specific components of the new model are described in terms of clinical support, medical information management, and scheduling. Such seemingly mundane issues are vitally important to provision of excellent health care. It has become increasingly apparent that how systems of care are structured and operated is as or more important than the expertise or decisions of individual physicians. To take good care of patients, General Internists need a viable practice model.
Clinical Support
There are numerous ways in which the office or clinic of a General Internist might be restructured to facilitate coordinated care. The physician might work side-by-side with one or more clinical assistants who are not independent clinicians but have substantial training and experience in clinical settings. For each patient, a clinical assistant completes an initial intake, reviews medical records, assesses the patient’s status, solicits agenda items, obtains vital signs, and performs any necessary point of care testing. The clinical assistant confers with the physician to review this information and joins the physician with the patient. The physician confirms and supplements key aspects of the history in an efficient and directed manner. During this process, the patient, clinical assistant, and physician formulate a plan and the clinical assistant simultaneously completes documentation. The physician then moves on to the next patient while the clinical assistant works with the patient to implement the plan and provides further education/explanation. If the patient calls later in the week with a question, she/he can be confident that this clinical assistant works closely with the physician and is personally familiar with the patient’s situation. The clinical assistant is continually learning in this environment, and like the physician, is rewarded by close interactions with patients.
Alternatively, routine interval visits could be scheduled with a nurse practitioner or physician assistant. The physician could visit briefly with the patient at the end of the encounter. The patient would understand that his or her physician remains firmly engaged and can look forward to a one-on-one appointment with the physician in the future. In larger practices, the services of pharmacists, health educators, nutritionists, and others may be warranted by the size of the patient population. In some clinics, pharmacists now initiate insulin therapy and titrate dosage or adjust antihypertensive medications.
Medical Information Management
The typical Generalist Physician still depends heavily upon paper records and forms that are inefficient to complete, store, access, and transmit. Moreover, it is difficult and expensive to use paper records for effective quality improvement or measurement. EHRs overcome many of these limitations, but despite their increasing adoption, their potential for improving the health of patients remains relatively untapped. Even in settings in which extensive EHRs have been deployed, the system is typically used in the same fashion as a paper record, i.e., simply for documentation, and most of the data are not systematically used for quality improvement. This is not only because of limitations of EHRs themselves, but also to the fact that physicians are too busy and poorly trained for such efforts.
In the setting of high quality coordinated care, the General Internist becomes the expert in the use of the EHR, not only in caring for an individual patient but also in managing a large number of patients within a practice. Moreover, the EHR is specifically designed to support this model of practice. When collecting and compiling clinical data, a clinical assistant is easily able to assemble prespecified reports that display all relevant information about patients, irrespective of the source (e.g., history, laboratory results, procedures, etc.) in a readily understandable, standardized format. This facilitates information exchange and eliminates time that would otherwise be spent searching through multiple sections of a record. Data in the record automatically link to context-sensitive resources such as clinical practice guidelines or alerts about newly recognized drug toxicities. The EHR also automatically links to other useful resources, such as patient education material and community resources. Patients can access and enter relevant information that is then available to the health care team.
The EHR in this setting also supports systematic methods for ensuring that patients receive a consistently high quality of care. The staff routinely devotes time each day to reviewing regular reports that identify patients who are due to receive indicated services such as cancer screening tests. Patients with certain parameters that are out-of-range, such as blood pressure, low-density lipoprotein (LDL)-cholesterol, or creatinine are identified, and plans to address these problems are devised. Patients can be confident that important results and findings do not slip through the cracks.
Because most medical errors reflect problems in information gathering and display, the EHR has the potential to play a critical role in improving efficiency and quality. The EHR should assist the physician in managing and using information. It must support physicians’ “thought-flow” as well as work-flow. To achieve this goal, however, the EHR must meet critical performance standards including:
-
Rapid accessibility and response time
In the outpatient setting, physicians presently spend hours daily using computer systems. A few seconds delay with each transaction accumulates into hours of wasted time. These delays directly reduce efficiency and are a barrier to physicians’ embrace of the EHR.
-
Intelligent and flexible data presentation
The visual interface and format or presentation of information is critical. Key information should be readily accessible with a minimum of “clicks”, and unnecessary clutter should be eliminated from the display field. Because of varied preferences, the interface should be customizable by the user, but should not require the user to reconstruct the desired format with each use. This flexibility should permit a high level of information density that relieves the user of the necessity to page through multiple screens to obtain a particular bit of information.
-
Consistency
Information should be presented in a consistent and familiar format. Inconsistency in display promotes inefficiency and likely contributes to errors. This is particularly useful in settings in which novices such as trainees might be using the system and must learn to do so rapidly.
-
Contextual sensitivity
By and large, EHRs are presently used mainly for storage and retrieval of data. Rarely do these systems have the capacity for awareness of important issues related to the individual patient or the needs of the provider. Although it will require substantially more sophistication than is currently available, an EHR should ultimately maintain awareness of key aspects and issues relevant to an individual patient (e.g., active problems or symptoms). The system should also then actively assist the provider with ready access to resources and decision aids. Providing information in context should promote more effective and efficient medical decisions and reduce errors.
-
Prioritization
The timing and prominence of information presented should be based upon its importance and urgency. The EHR should help protect the physician against information overload and assist in attending to the most important information. Redundancy should be eliminated.
-
Promotion of Quality Improvement
The EHR should be a platform for quality improvement. The possible avenues are limitless but include rule-driven alerts for extreme values and potential clinical problems (e.g., rising creatinine values) and evidence-based clinical reminders. Such alerts need to be judiciously applied to avoid causing information overload or unnecessary distraction, which, in turn, can reduce attention to truly important messages. The EHR should also provide the capability to summarize and analyze data in a relational fashion.
-
Electronic Communication
The EHR is an effective and reliable means of communication among health care providers and patients. Secure messaging provides a fast and inexpensive means for Generalist Physicians to communicate with consultants and support staff as well as patients. Computerized order entry that capably manages consultation requests ensures that these requests are not lost and can be readily tracked.
-
Patient Involvement
Modern EHRs also provide the opportunity for patients to access and supplement their health records. They can verify and amend, when warranted, personal health information. They can also supply records about health habits such as exercise, diet, weight loss or self-monitored disease parameters such as glucose and symptoms. This information can be linked to relevant resources and assist with chronic disease management.
The potential of the EHR to improve the efficiency of longitudinal care and the health of patients has barely been tapped. Realizing this potential, through the design of interfaces, implementation and application of the advanced EHR should become the province of physicians who specialize in coordinated care and assume responsibility for the oversight of patients’ overall health care.
Access and Scheduling
The modern General Internist must simultaneously manage three basic sets of issues: evaluation of acute symptoms, management of chronic illness, and disease prevention. The typical practice relies mainly on routinely scheduled visits plus a variable number of acute or drop-in visits, although some practices are beginning to commit a substantial proportion of visits to open access. Advance planning for either type of visit is often minimal, but in a setting in which coordinated care is practiced, the staff carefully manage schedules to optimize efficiency. In the Coordinated Care model, staff assembles necessary data from other providers or the laboratory before the visit to facilitate management of chronic illnesses and to provide opportunities to enhance preventive health. Many offices would continue to provide same-day access for acute problems, but simultaneously dovetail provision of preventive services to potentially obviate routine scheduled visits in the future. In general, routine tests are ordered according to predetermined protocols and accepted clinical practice guidelines. This process is aided by the EHR, which tracks and recommends indicated tests and procedures and functions to reduce unnecessary or duplicative procedures. In this way patients can be automatically contacted at prescribed intervals for tests and visits.
When preferred by the patient and the physician, preventive care can be provided at a dedicated visit that provides sufficient time for the physician and staff to properly assess and counsel the patient. The intelligent EHR relieves the physician and staff of many routine tracking and scheduling tasks and permits them to focus on gathering critical information directly from the patient. The patient has confidence in the system because she/he has come to expect that necessary tests, and treatments are accomplished in a timely and predictable fashion.
PAYMENT FOR COORDINATED CARE
Implicit in all of the foregoing discussion is that few, if any, of these changes can occur without a change in the method of paying for care. The present evaluation and management system reinforces an inefficient and expensive care delivery system that rewards piecework yet ignores the finished product. Unless and until the payment system is revamped, providers will be motivated to provide high volumes of visits without investing the time, energy, or resources into improved approaches to delivering health care to all people, but especially those who are chronically ill. In particular, there must be a mechanism to fairly reimburse physicians who provide leadership to teams that deliver high quality coordinated care. Payers must recognize that teams can provide better care than individuals and provide a mechanism to reasonably support this type of care. By furnishing a mechanism to provide coordinated, longitudinal care, payers will ultimately reap benefits by avoiding preventable complications and unnecessary care. As advocated by ACP, CMS should fund pilot programs to develop better practice models. Some of these should be conducted in academic settings so that the next generation of physicians can furnish leadership in moving toward coordinated care.
THE SPECIAL ROLE OF SGIM
As the premier organization for academic General Internists, SGIM has a critical role to play in discussions regarding the future of GIM and the role of General Internists in caring for patients in the 21st century. In particular, SGIM must lead the way by:
working in close partnership with other organizations such as ACP to advocate for the importance of concepts such as coordinated care and the “advanced medical home” and by seeking new mechanisms of payment and funding for pilot projects.
seeking to develop coalitions with other cognitive specialists through organizations such as the Association of Specialty Professors (ASP).
creating coalitions with General Internists working in other settings (e.g., Hospitalists and perioperative consultants) to support a coordinated care model that broadly encompasses all of GIM.
seeking to establish the preeminence of General Internists as experts in employing the EHR in the care of individuals with chronic illness.
collaborating with other organizations such as Association of American Medical Colleges (AAMC), ACP, Health Resources and Services Administration (HRSA), and American Board of Internal Medicine (ABIM) to create a database for tracking the number of General Internists in practice (as opposed to those completing residencies).
Acknowledgements
The authors are grateful to Barbara J. Turner, MD, Msc, immediate Past President for initiating this project and providing incisive criticism of the draft report, to Robert Centor, MD, President, for exceptional support and leadership and to the SGIM Council for their thoughtful criticism and feedback.
Potential Financial Conflicts of Interest None disclosed.
Footnotes
This paper was developed by the Blue Ribbon Panel of the Society of General Internal Medicine. Its authors include Stewart F. Babbott, MD; JudyAnn Bigby, MD; Susan C. Day, MD; David C. Dugdale, MD; Stephan D. Fihn, MD (panel chair); Wishwa N. Kapoor, MD; Laurence F. McMahon, Jr., MD; Gary E. Rosenthal, MD; and Christine A. Sinsky, MD. It was approved by the SGIM Council on July 14, 2006.
References
- 1.Anderson G. Chronic conditions. The cost and prevalence of chronic conditions are increasing. A response is overdue. Expert Voices. Issue 4, January 2002. National Institute for Health Care Management. [http://www.nihcm.org/ExpertV4.pdf].
- 2.Wu S-Y, Green A. Projection of Chronic Illness Prevalence and Cost Inflation. RAND Corporation, October 2000.
- 3.Partnership for solutions. Chronic Conditions: Making the Case for Ongoing Care. September 2004 Update. (http://www.partnershipforsolutions.org/DMS/files/chronicbook2004.pdf - last accessed 11/18/2006).
- 4.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;263–70. [DOI] [PMC free article] [PubMed]
- 5.Heffler S, Smith S, Keehan S et al.. Health Spending Projections Through 2013. Health Affairs, Health Tracking Trends Web Exclusive. February 11, 2004. (http://content.healthaffairs.org/cgi/content/full/hlthaff.w4.79v1/DC1 - last accessed 11/18/2006). [DOI] [PubMed]
- 6.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45. [DOI] [PubMed]
- 7.President’s Information Technology Advisory Committee. Health Care Through Information Technology. National Coordination Office for Information Technology Research and Development. Arlington, VA. 22230.
- 8.Iglehart JK. The new era of medical imaging—progress and pitfalls. N Engl J Med. 2006;354:2822–8. [DOI] [PubMed]
- 9.Fan VS, Reiber GE, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20:226–33. [DOI] [PMC free article] [PubMed]
- 10.American College of Physicians. The Advanced Medical Home: A Patient-Centered, Physician-Guided Model of Health Care Policy. Monograph; 2006.
- 11.Phillips RL, Green LA, Fryer GE, McCann J. The New Model of Primary Care: Knowledge Bought Dearly. Presented to the American Academy of Family Physicians Board of Directors. March 2004.
- 12.Kerr EA, Smith DM, Hogan MM, et al. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Med Care. 2003;41:1173–82. [DOI] [PubMed]


