Abstract
Background
A clearly stated clinical decision can induce a cognitive closure in patients and is an important investment in the end of patient–physician communications. Little is known about how often explicit decisions are made in primary care visits.
Objective
To use an innovative videotape analysis approach to assess physicians’ propensity to state decisions explicitly, and to examine the factors influencing decision patterns.
Design
We coded topics discussed in 395 videotapes of primary care visits, noting the number of instances and the length of discussions on each topic, and how discussions ended. A regression analysis tested the relationship between explicit decisions and visit factors such as the nature of topics under discussion, instances of discussion, the amount of time the patient spoke, and competing demands from other topics.
Results
About 77% of topics ended with explicit decisions. Patients spoke for an average of 58 seconds total per topic. Patients spoke more during topics that ended with an explicit decision, (67 seconds), compared with 36 seconds otherwise. The number of instances of a topic was associated with higher odds of having an explicit decision (OR = 1.73, p < 0.01). Increases in the number of topics discussed in visits (OR = 0.95, p < .05), and topics on lifestyle and habits (OR = 0.60, p < .01) were associated with lower odds of explicit decisions.
Conclusions
Although discussions often ended with explicit decisions, there were variations related to the content and dynamics of interactions. We recommend strengthening patients’ voice and developing clinical tools, e.g., an “exit prescription,” to improving decision making.
Key words: physician behavior, primary care, closure of patient–physician communication
Introduction
A clinical decision can be defined as a verbal commitment to an explicit action.1 A clearly stated decision can facilitate a cognitive closure in the minds of the patient and physician that the discussion on a particular topic has reached an end. Closure of conversation is an integral part of investing in the end of a clinical encounter, which can increase the potential for collaboration between patient and physician, influence health outcomes, improve adherence, and reduce unnecessary returns calls and visits.2 Despite increasing interest in decision making, we know surprisingly little about the extent to which patient–physician discussions of clinical topics end with explicitly stated decisions. Researchers have reported a deficit in informed decision making in routine office visits1,3; however, there is a gap in knowledge on how often explicit decisions are actually made.
We aim to take a step back to the basics by examining physicians’ propensity to explicitly state a decision when discussion of a topic ends. We took advantage of a unique data set consisting of 395 videotaped elderly patients’ visits with their primary care physicians. We examined the content of visits in terms of units of clinical decision making we refer to as “topics,” operationalized as clinical issues raised by either participant. We applied the multidimensional interaction analysis (MDIA) system, which codes an interaction directly from an audiotape or video of the visit and the topics sequentially introduced by patient or physician.4 The MDIA lists 36 categories subdivided into 5 major content areas: biomedical, lifestyle and habits, psychosocial, patient–physician relationship, and other.4 We partitioned visits into similar content areas and took a step further by recording how discussion of topics in each content area ended, i.e., with an explicitly stated decision or not. Whereas this is not the first study to use video data to examine patient–physician interaction at the topic level,4 it is the first to use such data to analyze the likelihood of an explicit decision being made during clinical encounters and the factors that affect that outcome.
Data and Methods
The videotapes were collected for another study based on a convenience sample of primary care physicians and their patients in routine office visits.5 The practices included a salaried medical group affiliated with an Academic Medical Center (AMC) in the southwest, a capitated private group practice structured as a managed care group (MCG) in a midwest suburb, and several fee-for-service solo private practices in an inner city (SOL) in the Midwest. These medical practices were chosen to because they represent diverse organizational settings.
Participants
The recruitment effort resulted in a sample of 35 physicians, all of whom had completed their training at the time of the original study. To be eligible for the original study, patients had to be at least 65 years of age, identify the participating physician as their usual source of care, and provide informed consent. Patient participation rates ranged from 61% to 65% at the study sites. Whereas it is unfortunate that data on physician participation rates were not collected in the previous study, a comparison of the sampled physicians with physicians nationwide6 showed that our physician sample was similar in gender composition, but had fewer physicians in the extremes of the age distribution. In addition, African-American physicians were overrepresented in our data (14% compared with 6%, nationally). Our patient sample was similar to national data on elderly patients in age distribution, perceived wealth, and living arrangement,7 but different in having more educated and fewer married patients.8 The final sample contained 395 videotaped visits with good audio and video quality. (Twenty nine visits were excluded because of poor audio or video quality.) Details of participant recruitment have been reported elsewhere.9
Data
Training of video-recording coders involved over 8 hours of initial didactic coaching, and independent coding of a series of visits by each of 5 coders. Coding training entailed having all coders code the same set of 10 and then 5 visits. To measure agreement among coders, we calculated intraclass correlation (ICC) for numerical variables. In light of debates on properties of Cohen’s kappa and its susceptibility to showing low values for uncommon behaviors,10–13 we used both Cohen’s kappa and percent agreement for categorical variables.14 Typically, ICC, Cohen’s kappa or percent agreement values are deemed acceptable if they are >0.7. For uncommon behaviors, if percent agreement is >0.7, the reliability is still acceptable even if the value of Cohen’s kappa is lower than that.10–13 After the second round of training coding, consistency was satisfactory: the ICC for visit length was 0.98; the total amount of time spent on conversation, 0.89; the amount of time patient spent talking, 0.84; and the number of topics, 0.95. The Cohen’s kappa and percent agreement for whether there was an explicit decision was 0.54 and 84%, respectively. The intrarater ICC ranged from 0.84 to 1 and percentage agreement from 93% to 100%. Following convention,1 we ensured interrater reliability by randomly recoding 10% of the visits by a second coder. To ensure intrarater reliability, each coder recoded 5% of the visits he or she had already coded. Coding questions were resolved in weekly team consultations with the lead author.
Coders first carefully reviewed the entire video to determine the nature and number of topics raised during the visit. Following the MDIA grouping,4 a topic was regarded as an issue that required a specific response by the physician or patient, regardless of who initiated the discussion. We identified 36 topics pertaining to 5 major content areas: A) biomedical, B) lifestyle and habits, C) psychosocial issues, D) patient–physician relationship, or E) other topics. Each topic was assigned a number from a predetermined list of 36 topics. For example, biomedical content included discussions on medical history, symptoms, and medical conditions. Lifestyle and habits related to diet, weight, alcohol, and smoking. Figure 1 presents detailed information on the 36 topics. Because only those topics under content areas A–C required clinical decisions, we excluded topics in content areas D (patient–physician relationship) and E (others). The analyses were based on 2,101 topics, totaling about 111 hours of video-recording.
Figure 1.
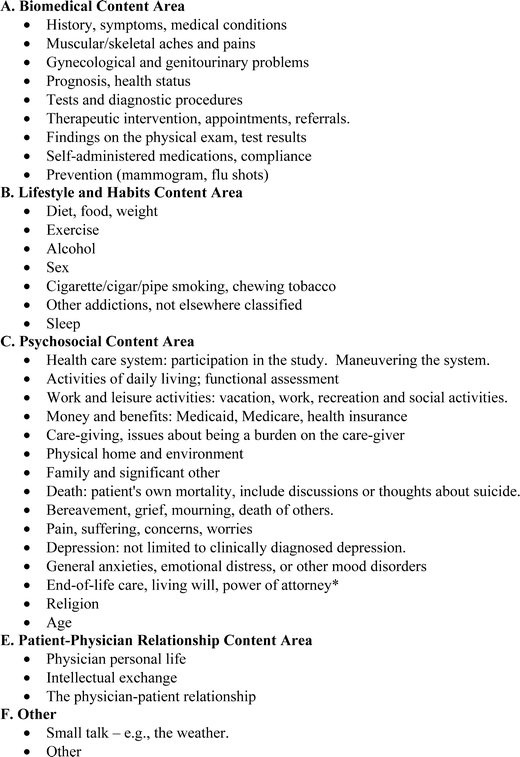
Major content areas and topics. Adopted from the multidimensional interaction analysis (MDIA) system.4
In addition to videotaping, patients were given a brief survey on demographics, whether the physician was their regular source of care, and the purpose of the visit before actually seeing the physician. Immediately after the visit, patients were given another short self-administered survey on health status measured by the SF-36.15 The timing of the second survey was planned to minimize its effect on patient–physician interactions and work flow in clinics. The physician survey provided information on specialization, practice setting, amount of time in practice, and sociodemographic characteristics.
Dependent Variable: Decision Type—Explicitly Stated or Not
The unit of analysis was the topic. A binary variable recorded how discussions on a topic ended: with or without an explicitly stated decision. For example, if the topic was about depression and the physician gave a prescription for an antidepressant and instructed the patient to take it every day, it was coded as an explicit decision. Conversely, if the physician did not discuss what the treatment should be and went on to a different topic without returning to the depression topic later, then it was coded as no decision made.
Explanatory Variables
Explanatory variables contain information about the topic. To capture the phenomenon in which discourse on a topic occurred over several instances and was interspersed by discussion of other topics, we recorded the number of instances contained in a topic. An instance was defined as the exchange between the patient–physician dyad on a particular topic before the subject was changed. For example, when the patient or physician changed subjects during discussion on a particular topic, the interruption point was marked as the end of that instance. If either returned to the same topic later, the second occurrence of discussion on that topic was the second instance, and so on. The total number of instances was recorded.
The length of patient talk time was measured by the number of seconds the patient spent talking before all discussion on the topic concluded. Figure 2 depicts the flow of conversations during 1 office visit and illustrates how they were grouped into topics and how coding was done for the way discussions on each topic ended. This visit took place between a female patient and a male physician who was about to retire. The conversation began with the patient’s complaint about irritable bowel, its negative impact on her social functioning, and her concern about her diet and weight. She also mentioned a family crisis, which the physician responded to only perfunctorily. He redirected the conversation to his retirement and her choosing a new physician. She complained about a cough to which he responded with a token remark: “Oh.” She also complained about heart palpitations. He reassured her about a good cardiac rhythm and stated that a heart monitor could be used if necessary. She complained about her cough the second time, and again received no response. He redirected her back to choosing a new physician; they decided that she would see a female physician. He then prescribed Bentyl®, ordered a colonoscopy, and introduced the patient to her future physician.
Figure 2.
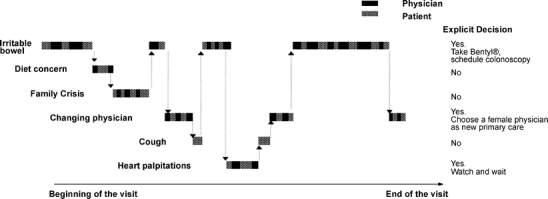
Flow of conversation between a female patient and a male physician during one office visit.
As illustrated in Figure 2, this encounter contained 6 topics: (1) irritable bowel, (2) changing physicians, (3) diet concern, (4) family crisis, (5) cough, and (6) heart palpitations. The first, second, and last topics ended with explicitly stated decisions, whereas the others did not (illustrated in Fig. 2). The frequent changing of topics during the course of a visit is quite common.
Covariates were chosen based on previous research about how patient–physician interaction has been influenced by patient health,16,17 patient gender and ethnicity,18 patients’ perceived wealth,19 physicians’ gender20,21,22 and physicians’ length in practice,23 physicians’ specialty,1 and the continuity of care measured by the number of years the patient has seen the physician.24,25 Patient’s health status was measured by normed SF-36 scores.15,26
Analytic Approach
We used a logit generalized estimating equations (GEE) regression analysis model to identify determinants of explicit decisions. The model accounted for both the clustering of topics within a visit and the clustering of patients within an individual physician. Categorical variables have been “centered” to prevent potential errors in statistical inference.27 All of the analyses were done in STATA 9.0.28
Results
Table 1 displays demographic characteristics of the study participants. In addition to the information provided in Table 1, Table 2 exhibits characteristics of the study sample (topic, visit, patient, physician, and practice setting) divided by whether or not the discussion on a topic ended with an explicit decision. We found that, on average, 77% of discussions on topics ended with an explicit decision. Significant practice site variations were found with respect to physicians’ propensity to provide explicit decisions: 75% at the Academic Medical Center (AMC), 80% in the managed care practice (MCO), and 62% in the inner city private solo practices (SOL; p < .05).
Table 1.
Demographic Characteristics of Study Participants
| Values | |
|---|---|
| Physician characteristics (N = 35) | |
| Age | Mean 49.4 (range 32 to 82) |
| Gender | 27 male, 8 female |
| Race | 29 White, 6 African American |
| Practice setting | 10 in Academic Medical Center, 21 in managed care group, and 4 inner city solo fee-for-service private practitioners |
| Patient characteristics (N = 382) | |
| Age | Mean 74.4 (range 65 to 91) |
| Gender | 125 male, 257 female |
| Race | 310 White, 45 African American, 27 others |
| Marital status | 195 married, 187 not married |
| Education | 168 college or more, 214 less than college |
| Income | 163 more than enough to make ends meet, 143 enough, 76 not enough |
Table 2.
Sample Characteristics by Decision Type
| Decision explicitly stated | ||
|---|---|---|
| Yes | No | |
| All topics (N = 2,101) | 1,625 (77.3%) | 476 (22.7%) |
| Topic characteristics (N = 2101) | ||
| Number of instances of topic, mean | 2.2 | 1.5** |
| Patient talk time (seconds), mean | 66.9 | 35.9** |
| Medical topics, % (control) | 78.8 | |
| Lifestyle and habit topics, % | 72.5** | |
| Psychosocial topics, % | 76.9 | |
| Visit characteristics (N = 382) | ||
| Length of visit (minutes), mean | 19.2 | 19.2 |
| Number of topics raised, mean | 7.4 | 7.8** |
| Patient characteristics (N = 382) | ||
| Age in years, mean | 74.4 | 74.5 |
| Male, % (control) | 75.1 | |
| Female, % | 78.4 | |
| White, % (Control) | 78.4 | |
| African American, % | 72.5* | |
| Education, Less than college, % (control) | 77.5 | |
| College or more, % | 77.2 | |
| Physician characteristics (N = 35) | ||
| Male, % (control) | 76.8 | |
| Female, % | 79.1 | |
| White, % (control) | 78.1 | |
| African American, % | 71.2* | |
| Years in medical practice, mean | 20.4 | 20.4 |
| Internal medicine, % (control) | 80.3 | |
| Family medicine, % | 72.4** | |
| Other specialties, % | 77.7* | |
| Practice setting characteristics (N = 3) | ||
| Academic Medical Center (AMC), % (control) | 75.0 | |
| Managed care organization (MCG), % | 79.6* | |
| Fee-for-service inner city private solo practice (SOL), % | 62.1* | |
| Dyad characteristics (N = 382) | ||
| Year of patient–physician relationship, mean | 6.0 | 6.5 |
*p < 0.05, **p < 0.01
The median number of topics was 6 per visit. The majority of the topics (70%) were biomedical; the second most common were psychosocial matters (12%). Patients spoke for an average of 58 seconds total per topic. Patients at the MCO and SOL spoke less than patients at the AMC (p < .01).
Table 2 shows that the topics with an explicit decision occurred 2.2 times compared with 1.5 instances for topics without an explicit decision (p < .01). Similarly, patients spoke more during topics that ended with an explicit decision (66.9 seconds) compared with significantly shorter time (35.9 seconds) for topics that did not end with an explicit decision. In fact, all of those topics in which patients spoke for at least 5 minutes cumulatively ended with explicit decisions. These patterns were more fully investigated using logit regression analysis where we adjusted for the effects of covariates.
Regression Analysis Results
Odds ratios (OR) based on logit regression model are presented in Table 3. The largest positive effect came from the number of instances of a topic under discussion (OR = 1.73, p < .01). An increase of 1 instance of discussion of a particular topic was associated with a 1.73 times higher odds of the topic ending with an explicitly stated decision. The longer the patient spoke about a topic in total, the more likely the topic would end with an explicit decision, although the magnitude of the effect was relatively small (OR = 1.01, p < .01). In comparison to discussion of biomedical topics, discussions on lifestyle and habits were 0.60 times less likely to receive explicit decisions (p < .05). No differences emerged from comparing biomedical and psychosocial topics. Higher competing demands from other topics discussed during the same visit had an anticipated negative, but relatively small, effect on whether the topic under investigation reached an explicit decision. Each additional topic was 0.95 times less likely to end with an explicit decision (p < .05). Unlike the results of the descriptive analysis, regression analysis showed that the odds of having an explicitly stated decision were similar across the various practice settings, when the effects of other covariates were taken into account. To conserve space, the findings about other covariates are not reported but are available upon request.
Table 3.
Determinants of Making Explicit Decisions
| Determinants | Odds ratio |
|---|---|
| Number of instances in topic | 1.73** |
| Patient talk time | 1.01** |
| Compared to biomedical topics: | |
| Discussion on lifestyle and habits | 0.60* |
| Discussion on psychosocial issues | 0.92 |
| Number of topics in visit | 0.95* |
| Compared to Academic Medical Center: | |
| Inner city solo FFS private practice (SOL) | 0.63 |
| Managed care organization (MCG) | 1.34 |
| N (topics) | 2101 |
| N (visits) | 382 |
| N (physicians) | 35 |
*p < 0.05, **p < 0.01
Regression analysis controlled for covariates (patient age, gender, education, perceived wealth, health status, physician age, physician gender, continuity of care, physician’s years in practice, and physician’s practice setting.)
Discussion
Patient–physician interactions are dynamic and complex conversational exchanges. Whereas the majority of the topics in our sample ended with an explicitly stated decision, the clinical implications of variations in decision making merit further discussion.
Patient Voice and Time Management Challenges
We found that the amount of time a patient spoke was a significant determinant of topics ending with explicit decisions. The more instances there were in a topic, the higher the likelihood of getting an explicit decision. These findings suggest that if patients participate actively in their visits, i.e., making their voice heard, they benefit by expressing their concerns and also improve the chance that the consultation will reach satisfactory closure. Developing a list of concerns (i.e., topics) before the visit may help patients track and return to each concern until there is closure. It would also help the physician to document a brief response or plan for each topic on the list. Patients could present their list and request a brief written plan near the end of the visits—i.e., an “exit prescription”—thereby providing a way to “close the loop” in patient–physician communication.
We also infer that the number of instances in which a topic is discussed may be associated with the complexity of the topic or dissatisfaction by either person as to how the previous instances addressed the topic. For example, if a patient raised a concern about her depressed mood several times in a visit and the physician responded briefly and redirected the discourse to other topics, the large number of instances on mood might suggest the patient’s unmet desire for a more thorough response from the physician. Sociolinguists report that those in subordinate positions are more likely to speak indirectly and, when they do not believe they are heard, may repeatedly call for attention, albeit indirectly.29 Future research could look at the discourse in more depth, taking into consideration the context in which additional instances are introduced to unravel the phenomenon. Future qualitative research could also examine the micro-interactional dynamics that lead to closure. Our preliminary analyses showed that interruptions during a visit (e.g., physicians being paged and leave the room in the middle of a topic, or nurses coming in the room to ask physicians questions about other patients) are not conducive to bringing closure to topics raised. Patients asking questions of clarification, conversely, is conducive to closure. For the time being, we encourage patients to speak out and to continue to bring their physicians’ attention back to issues that are important to them until they reach a satisfactory conclusion. Prioritizing the main concerns is also important because our results suggest that the number of other topics competing for physicians’ attention could reduce the chance of reaching an explicit decision on any given topic being discussed.
Lifestyle and Personal Habits
Counseling patients about lifestyle issues is a complex task.30 The finding that, compared with biomedical topics, topics of lifestyle and habits were less likely to end with explicitly stated decisions further demonstrates difficulties involved in lifestyle counseling. It is widely recognized that physicians should listen to and consider the values of their patients,31 and provide patient-centered counseling to improve compliance with life-enhancing behavior changes. Having explicitly stated decisions that encourage patients to take concrete steps toward lifestyle change is a step in the right direction.
Limitations
This study has several limitations. First, the convenience sample limits the external validity of the findings to other populations beyond the participating elderly patients and physicians. Additional studies are needed to examine whether such patterns of communication exist among other patient and physician populations. Second, we do not have information from the medical records that could provide additional information on the patient’s history, nor do we have data on previous or subsequent visits. These limitations are shared by other studies on patient–physician interactions, however.
Conclusions
Investing in the end of the clinical encounter can ensure patients’ understanding of the decisions, increase potential for collaboration, and improve adherence.2 The complex dynamics of conversations pose a cognitive challenge for physicians to keep track of the discussion. As many patients are reported to leave their visits without having understood what the physician said,32 clearly stating the decision is an important part of informing the patient. Strengthening patients’ voice and developing tools for patients and physicians to meet time management challenges could potentially improve medical decision making. We recommend a written “exit prescription” with a brief plan for each topic addressed to help patients and physicians “close the loop” in their communication. Additional studies are needed to replicate the topic analysis approach on other samples of patients and physicians with more participants. The impact of these findings on clinical practice and policy will be stronger if consistent patterns are identified, using this innovative approach to examine factors influencing clinical decision making and communication of decisions at the topic level.
Acknowledgments
The authors thank Michele Greene for providing the coding guide for the Multidimensional Interaction Analysis (MDIA) system and Thomas McGuire, Charles Huber, Emil Berkanovic, Suojin Wang, three anonymous reviewers, and the Deputy Editor Richard Frankel for helpful comments. Funding from NIMH MH0193, NIA AG 15737, and the Texas A&M Health Science Center School of Rural Public Health and the Scott & White Health Plan Health Services Research Program is gratefully acknowledged.
Potential Financial Conflicts of Interest None disclosed.
References
- 1.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. J Am Med Assoc. 1999;282(24):2313–20. [DOI] [PubMed]
- 2.Frankel R, Stein T. Getting the most out of the clinical encounter: the four habits model. J Med Pract Manage. 2001;16(4):184–91. [PubMed]
- 3.Consensus Development Conference NIH. Diagnosis and treatment of depression in late life. Paper presented at: NIH Consensus Development Conference; 1991.
- 4.Charon R, Greene MG, Adelman RD. Multi-dimensional interaction analysis: a collaborative approach to the study of medical discourse. Soc Sci Med. 1994;39(7):955–65 [DOI] [PubMed]
- 5.Cook M. Final Report: Assessment of Doctor–Elderly Patient Encounters, Grant No. R44 AG5737-S2. Washington, D.C: National Institute of Aging; 2002.
- 6.American Medical Association. Physician Characteristics and Distribution in the US. 2001/2002 Edition ed. Chicago: American Medical Association Press; 2001.
- 7.US Census Bureau. 2001.
- 8.Federal Interagency Forum on Aging Related Statistics. Older Americans 2000: Key Indicators of Well-Being. Hyattsville, MD: National Center for Health Statistics; 2000.
- 9.Tai-Seale M, Bramson R, Drukker D, et al. Understanding primary care physicians’ propensity to assess elderly patients for depression using interaction and survey data. Med Care. 2005;43(12):1217-24. [DOI] [PubMed]
- 10.Feinstien A, Cicchetti D. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543–9. [DOI] [PubMed]
- 11.Cicchetti D, Feinstein A. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43(6):551–8. [DOI] [PubMed]
- 12.Bakeman R, Quera V, McArther D, Robinson BF. Detecting sequential patterns and determining their reliability with fallible observers. Psychol Methods. 1997;2(4):357–70. [DOI]
- 13.Ickes W, Marangoni C, Garcia S. Studying empathic accuracy in a clinically relevant context. In: Ickes W, ed. Empathic Accuracy. New York: Guilford Press; 1997:282–310.
- 14.Eide HQV, Graugaard P, Finset A. Physician–patient dialogue surrounding patients’ expression of concern: applying sequence analysis to RIAS. Soc Sci Med. 2004;59(1):145–55. [DOI] [PubMed]
- 15.Ware JE Jr., Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the medical outcomes study. Med Care. 1995;33(4 Suppl):AS264–79. [PubMed]
- 16.Balsa AI, McGuire TG, Meredith LS. Testing for statistical discrimination in health care. Health Serv Res. 2005;40(1):227–52. [DOI] [PMC free article] [PubMed]
- 17.Bertakis KD, Callahan EJ, Helms LJ, Azari R, Robbins JA. The effect of patient health status on physician practice style. Fam Med. 1993;25(8):530–5. [PubMed]
- 18.Sleath B, Rubin RH. Gender, ethnicity, and physician–patient communication about depression and anxiety in primary care. Patient Educ Couns. 2002;48(3):243–52. [DOI] [PubMed]
- 19.Jacobs LR, Morone JA. Health and Wealth: the American Prospect Online; 2004.
- 20.Phelps CE. The methodologic foundations of studies of the appropriateness of medical care. N Engl J Med. 1993;329(17):1241–5. [DOI] [PubMed]
- 21.Henderson JT, Hudson Scholle S, Weisman CS, Anderson RT. The role of physician gender in the evaluation of the National Centers of Excellence in Women’s Health: test of an alternate hypothesis. Womens Health Issues. 2004;14(4):130–9. [DOI] [PubMed]
- 22.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. J Am Med Assoc. 2002;288(6):756–64. [DOI] [PubMed]
- 23.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–73. [DOI] [PubMed]
- 24.Weiss L, Blustein J. Faithful patients: the effect of long-term physician–patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1998;88(1):135–6. [DOI] [PMC free article] [PubMed]
- 25.Merrill J, Laux L, Thornby J. Troublesome aspects of the patient–physician relationship: a study of human factors. South Med J. 1987;80(10):1211–5. [DOI] [PubMed]
- 26.Ware J, Kosinski M, Dewey J. How to Score Version 2 of the SF-36 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000.
- 27.Kraemer HC, Blasey CM. Centering in regression analyses: a strategy to prevent errors in statistical inference. Int J Methods Psychiatr Res. 2004;13(3):141–51. [DOI] [PMC free article] [PubMed]
- 28.STATACorp. STATA Reference Manual. College Station, TX; 2003.
- 29.Tannen D. The power of talk: who gets heard and why. Harvard Bus Rev. 1995;73(5):138–48.
- 30.Feldman SR, John G, Chen JYH, Fleischer AB. Effects of systematic asymmetric discounting on physician–patient interactions: a theoretical framework to explain poor compliance with lifestyle counseling. BMC Med Inform Decis Mak. 2002;2:8. [DOI] [PMC free article] [PubMed]
- 31.Becker G, Grossman M, Murphy K. Rational addiction and the effect of price on consumption. Am Econ Rev. 1991;81(2):237–41 (May).
- 32.Roter D, Hall J. Studies of doctor–patient interactions. Annu Rev Public Health. 1989;10:163–80. [DOI] [PubMed]


