Abstract
Background
Increasing complexity of medical care, coupled with limits on resident work hours, has prompted consideration of extending Internal Medicine training. It is unclear whether further hour reductions and extension of training beyond the current duration of 3 years would be accepted by trainees.
Objective
We aimed to determine if further work-hour reductions and extension of training would be accepted by trainees and whether resident burnout affects their opinions.
Design
A postal survey was sent to all 143 Internal Medicine residents at the University of Colorado School of Medicine in May 2004.
Measurements
The survey contained questions related to opinions on work-hour limits using a 5-point Likert scale ranging from strongly agree to strongly disagree. Burnout was measured using the Maslach Burnout Inventory, organized into three subscales: emotional exhaustion (EE), depersonalization (DP), and personal accomplishment, with burnout defined as high EE or DP.
Results
Seventy-four percent (106/143) of residents returned the survey. The vast majority (84%) of residents disagreed or strongly disagreed with extending training to 4 or 5 years. Burnout residents were less averse to extending training (strongly agree or agree, 18.9% vs 4.3%, P = .04). The majority of residents (68.9%) disagreed or strongly disagreed with establishing a 60-hour/week limit. Residents who met the criteria for burnout were more likely to agree that a 60-hour limit would be better than an 80-hour limit (strongly agree or agree, 22% vs 8%, P = .02).
Conclusions
In this program, most Internal Medicine residents are strongly opposed to extending their training to 4 or 5 years and would prefer the current 80 hours/week cap. A longer, less intense pace of Internal Medicine training seems to be less attractive in the eyes of current trainees.
Key words: residency training, burnout, education, work-hour restriction, Maslach
Background
Medicine residency training is in a state of transition. Spurred by the death of Libby Zion in March 1984 and the grand jury finding fault with the system of residency training and physician staffing, work-hour restrictions were implemented in New York State. In July 2003, the Accreditation Council for Graduate Medical Education (ACGME) mandated that all residents work no more than 24 consecutive hours with an additional 6 hours for educational and administrative activities with no more than 80 hours/week averaged over 4 weeks.1
Internal Medicine residents are at high risk for burnout.2 Burnout originates from frequent intense interactions with patients with complex problems.3 Residents work in an environment with high demands and lack of autonomy. They may not have yet acquired all the knowledge and abilities to care for their patients, causing internal stress and strife leading to burnout.4–7 The hallmark features of burnout are a combination of emotional exhaustion (EE), depersonalization (DP), and a reduced sense of personal accomplishment (PA).8
The depth and breath of knowledge needed to practice adequately in today’s modern medical field continues to expand. In 2003, the Society of General Internal Medicine released a task force report on the future of Internal Medicine.9 They expressed pessimism with the current training system, stating that “only a truly exceptional resident would be able to finish a three-year program capable of practicing in health promotion, in ambulatory and hospital settings, competent in geriatrics and chronic disease management, and with enough medical and management expertise to lead a team of providers in the care of a population, in a rural or urban center.”
Objective
Our objective was to determine University of Colorado’s Internal Medicine residents’ opinions on work-hour restrictions, education, and duration of training. We also evaluated how resident burnout affects the desired intensity and length of training.
Design
We developed an 82-question self-administered postal survey.10 Surveys were mailed to each resident’s home in May 2004, nearly 1 year after the new work schedule was implemented. Residents were asked to answer questions in reference to their previous month’s rotation. Colorado Multiple Institutional Review Board approved the research protocol.
Participants
All University of Colorado Health Science Center (UCHSC) Internal Medicine residents were eligible to participate in the study. The UCHSC Internal Medicine training program includes residents distributed across 3 postgraduate years (PGY) and 3 tracks; preliminary (6 total), primary care (10/PGY class), and categorical (36/PGY class). Before the 2004 academic year, changes were made to ensure that no resident worked more than 30 continuous hours and 80 hours/week on average as mandated by new ACGME regulations.
Measurements
The Maslach Burnout Inventory (MBI) consists of a 22-item self-administered 7-point Likert scale questionnaire organized into three subscales: 9 questions on EE, 5 questions on DP, and 8 questions on PA.3 Based on a normative sample of 1,104 medical workers, responders in the upper third were considered a high scorer for each subscale, EE ≥27, DP ≥10, and PA ≤33.3 Burnout was defined as high EE or DP.3,4,11 PA is not included because it correlates less with measures of psychiatric and physiologic strain.3 We also assessed the resident’s opinions on residency training, using a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.”
Statistical Analysis
We compared attitudes between burned-out and not burned-out residents using Fisher’s exact test. A P value of <.05 was considered to be statistically significant.
Results
The response rate was 74% (106/143) with slightly less second-year residents responding (Table 1). The distribution of respondents by training track mirrors the program as a whole. Two thirds of the respondents were in the 26- to 30-year-old age group. Fifty-eight percent of respondents were women. Fifty-eight of residents met the criteria for burnout.
Table 1.
Demographics of the 106 Responding Residents
| Number of respondents | Percent | |
|---|---|---|
| Female | 61 | 58 |
| PGY | ||
| I | 39 | 37 |
| II | 28 | 26 |
| III | 39 | 37 |
| Age | ||
| 26–30 | 71 | 67 |
| 31–35 | 27 | 26 |
| 36–40 | 7 | 6.7 |
| Residents with burnout | 58 | 55 |
| Training Track | ||
| Categorical | 79 | 75 |
| Primary care | 24 | 23 |
| Preliminary | 3 | 2.8 |
| Previous rotation | ||
| Hospital rotation | 71 | 67 |
| Consults | 8 | 7.5 |
| Other | 21 | 20 |
The majority of residents disagreed with the notion of extending training to 4 or 5 years (disagree 32% and strongly disagree 53%) (Table 2). Residents that met the criteria for burnout tended to be less averse to extending training (Fig. 1). The majority of residents disagreed with establishing a 60-hour work week cap instead of the current 80 hours/week restriction (disagree 52% and strongly disagree 17%). Residents with burnout preferred a more strict work restriction (Fig. 2). In addition, the majority of residents disagreed with the notion that the work-hour restrictions would increase their learning opportunities (disagree 38% and strongly disagree 17%). This opinion was the same for burned-out and nonburned-out residents (Fig. 3). Forty-two percent of residents either agreed or strongly agreed with the statement “I enjoy medicine more with the work-hour limits,” 42% of residents reported improved personal life, while 69% agreed or strongly agreed that they were “glad the new work restrictions were implemented.” There was no difference noted between burned-out and nonburned-out residents for these three questions. When asked about patient safety, 45% of the residents agreed or strongly agreed that “overall, I think the new work restrictions improved patient safety,” which did not differ with regard to burnout.
Table 2.
Survey Results of Residents’ Opinions on Work-hour Restrictions
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| I would be willing to train longer (4–5 years for Internal Medicine) if I could work fewer hours. | 2 (1.9) | 11 (10) | 3 (2.9) | 34 (32) | 55 (53) |
| Overall, an 80-hour work week is still too much. A 60-hour limit would be better. | 3 (2.9) | 14 (13) | 15 (14) | 55 (52) | 18 (17) |
| I think the new work-hour restrictions will increase the amount I learn. | 3 (2.9) | 23 (22) | 24 (23) | 38 (36) | 17 (16) |
| I enjoy medicine more with the work-hour limits. | 5 (8.1) | 20 (33) | 18 (29) | 12 (19) | 7 (11) |
| My personal life has improved with the new work schedule | 8 (13) | 18 (29) | 18 (29) | 15 (24) | 3 (4.8) |
| Overall, I am glad the new work restrictions were implemented. | 24 (23) | 47 (46) | 12 (12) | 11 (11) | 9 (8.7) |
| Overall, I think the new work restrictions improve patient safety. | 15 (15) | 31 (30) | 27 (26) | 16 (16) | 14 (14) |
Figure 1.
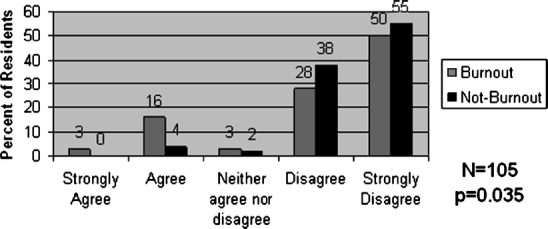
Percent of residents with burnout versus no burnout willing to train longer (4–5 years for Internal Medicine) if they could work fewer hours. P value represents 2 × 2 comparison of burned-out versus nonburned-out residents that strongly agree or agree versus those residents the neither agree nor disagree, disagree, or strongly disagree.
Figure 2.
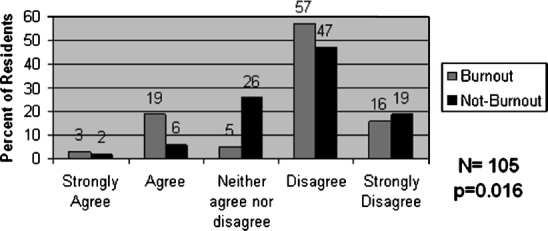
Percent of residents with burnout versus no burnout preferring 60-hour work week limit over an 80-hour work week. P value represents 2 × 2 comparison of burned-out versus nonburned-out residents that strongly agree or agree versus those residents the neither agree nor disagree, disagree, or strongly disagree.
Figure 3.
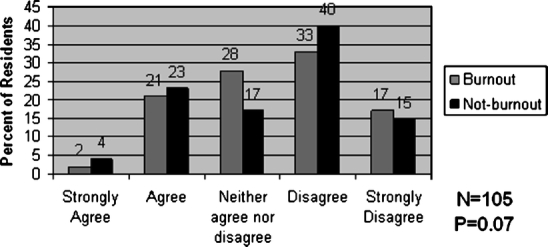
Percent of residents with burnout versus no burnout agreeing with the statement that “I think the new work-hour restrictions will increase the amount I will learn.” P value represents 2 × 2 comparison of burned-out versus nonburned-out residents that strongly agree or agree versus those residents the neither agree nor disagree, disagree, or strongly disagree.
Conclusions
To our knowledge, this is the first survey of Internal Medicine residents concerning desired work hours and length of training since the nationwide enforcement of the ACGME work restrictions in July 2003. Other studies have looked at the impact of work-hour restrictions on resident’s quality of life and education. A 2005 survey of Internal Medicine and General Surgery residents who trained before and after work-hour restrictions showed that all residents, particularly surgical residents, believed that their quality of life had improved with fewer hours worked.12 Our study also showed that more residents endorsed that the new restrictions improved their quality of life, including their enjoyment of medicine and their personal life. The combined improvement in work and social life yielded more than two thirds of residents being glad the new work hours were implemented. Other studies have looked at resident’s opinions of the educational impact of the ACGME work-hour restrictions. Two surveys of Internal Medicine residents in San Francisco and Seattle evaluated the impact of work-hour reform on aspects of resident life.13,14 In San Francisco, 28% of the respondents reported a negative impact and 39% reported no impact on education, while in Seattle 47% of the residents reported a negative impact and 32% neutral effect on education. A General Surgery resident survey showed that 60% of residents reported doing fewer operations and half reported missing out on learning opportunities.15 Interestingly, only 39% of the surgical residents reported an overall worsening in the quality of training. Our study concurs with these studies with 52% of the University of Colorado residents either disagreed or strongly disagreed with the idea that work-hour reform increased that amount they learned.
Our study also asked residents about their desired length of training. Interestingly, even though residents believed that the quality of their education had worsened with the new work schedule, they rejected the idea of lengthening their training to compensate for this deficit. They also rejected the idea of a further reduction in work-hour restrictions. Those residents with high EE or DP on the MBI were more likely to desire a longer and gentler residency training. These residents probably feel overwhelmed with the current work schedule and desire to spread the work out over more years. However, an earlier survey at University of Colorado and another survey at University of Washington did not show an improvement in resident burnout with restricting work hours.14,16 Therefore, even though these residents desire a less rigorous residency, it may not decrease their burnout.
There are significant limitations to this study. We do not know the opinions of the nonresponding residents; however, the high response rate suggests that the data are an accurate representation of the residency program. Importantly, as with all surveys, recall bias and inaccuracies are a concern. However, we blinded the residents to the hypothesis and the nature of the validated instruments, so they were unable to consciously manipulate the results. Also, the survey asked about “willingness to train longer (4–5 years for Internal Medicine).” We do not know if the resident may accept a 4-year program but disagreed with the statement because they rejected a 5-year training program. This ambiguity may have altered the results. Because this survey was conducted at one institution at one point of time, we do not know if residents’ opinions change during their training or if these residents’ opinions are generalizable to all Internal Medicine residents as a whole.
In light of the ever-increasing knowledge and procedural skills necessary to practice quality health care, reforming residency training will need to be debated. Either residency training will need to be lengthened so that the resident becomes adept at all facets of Internal Medicine practice or restructured as recommended by the American College of Physicians so that the third year is customized to the resident’s future career goals.17 Even though the number of medical school graduates entering Internal Medicine residencies at this time is fairly constant,18,19 prolonging training may make the Internal Medicine specialty less attractive and decrease the pool of practicing Internists in the future.
Acknowledgment
This study was funded by an internal small grant from Division of General Internal Medicine, University of Colorado Health Science Center.
Potential Financial Conflicts of Interest None disclosed.
References
- 1.ACGME. Information related to the ACGME’s effort to address resident duty hours. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_dutyHoursCommonPR.pdf.
- 2.Thomas NK. Resident burnout. JAMA. 2004;292:2880–9. [DOI] [PubMed]
- 3.Maslach C, Jackson SE. Maslach burnout inventory manual. 3rd edn. Palo Alto, Ca: Consulting Psychology Press; 1986.
- 4.Cherniss C. Role of professional burnout self-efficacy in the etiology and amelioration of burnout. Professional burnout: recent developments in theory and research. Washington, D.C.: Taylor & Francis; 1993.
- 5.Leiter MP. Burnout as a crisis in self-efficacy: conceptual and practical considerations. Work Stress. 1992;6:107–15.
- 6.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1986;98:310–57. [DOI] [PubMed]
- 7.Nowack KM, Hanson AL, Gibbons J. Factors affecting burnout and job performance in resident assistants. J Coll Stud Pers. 1985;26:137–42.
- 8.Lee RT, Ashforth BE. On the meaning of Maslach’s three dimensions of burnout. J Appl Psychol. 1990;75:743–7. [DOI] [PubMed]
- 9.Society of General Internal Medicine. The Society of General Internal Medicine Task Force on the Future of General Internal Medicine: http://www.sgim.org/futureofGIM.pdf. Access 18 Aug 2005.
- 10.Dillman D. Mail and telephone surveys: the total design method. New York, NY: Wiley Press; 1978.
- 11.Raferty JP, Leamkau JP, Purdy RR, Rudisill JR. Validity of the Maslach burnout inventory for family practice physicians. J Clin Psychol. 1986;42:488–92. [DOI] [PubMed]
- 12.Myers J, Bellini L, Morris J, et al. Internal Medicine and General Surgery residents’ attitudes about the ACGME duty hour regulations: a multicenter study. J Gen Intern Med. 2006;21(S4):75. [DOI] [PubMed]
- 13.Vidyarthi A, Katz P, Wall S, et al. Impact of reduced duty hours on residents’ educational satisfaction at the University of California, San Francisco. Acad Med. 2006;81:76–81. [DOI] [PubMed]
- 14.Goiten L, Shanafelt, T, Wopf, J, et al. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Int Med. 2005;165:2601–6. [DOI] [PubMed]
- 15.Irani J, Mello, M, Ashley S, et al. Surgical residents’ perceptions of the effects of the ACGME duty hour requirements 1 year after implementation. Surgery. 2005;138;246–53. [DOI] [PubMed]
- 16.Gopal R, Glasheen J, Miysohi T, Prochazka A. Burnout and internal medicine work-hour restrictions. Arch Int Med. 2005;165:2595–600. [DOI] [PubMed]
- 17.Weinberg S, Smith L, Collier V. Position paper: redesigning training for internal medicine. Ann Int Med. 2006;144:927–32. [DOI] [PubMed]
- 18.Brotherton S, Rockey P, Etzel S. US graduate medical education, 2003–2004. JAMA. 2004;292:1032–7. [DOI] [PubMed]
- 19.American Board of Internal Medicine. American Board of Internal Medicine Residency Match Statistics. Available at http://www.abim.org/resources/trainim.shtm. Accessed 2 Feb 2006.


