Abstract
BACKGROUND
Quality of cardiovascular disease (CVD) preventive care is suboptimal. Recent data correlated increasing years in practice for physicians with lower-quality health care.
OBJECTIVE
The purpose of this study was to assess physician awareness/adherence to national blood pressure, cholesterol, and CVD prevention guidelines for women according to physician/practice characteristics.
DESIGN
Standardized online survey and experimental case studies were administered to 500 randomly selected U.S. physicians. Multivariable regression models tested physician age, gender, specialty, and practice type as independent predictors of guideline awareness/adherence.
RESULTS
Compared with older physicians (50+ years), younger physicians (<50 years) reported a lower level of awareness of cholesterol guidelines (P=.04) and lower incorporation of women's guidelines (P=.02). Yet, older physicians were less likely to recommend weight management for high-risk cases (P=.03) and less confident in helping patients manage weight (P=.045) than younger physicians. Older physicians were also less likely to identify a low-density lipoprotein<100 mg/dL as optimal versus younger physicians (P=.01), as were solo versus nonsolo practitioners (P=.02). Solo practitioners were less aware of cholesterol guidelines (P=.04) and were more likely to prescribe aspirin for low-risk female patients than nonsolo practitioners (P<.01). Solo practitioners rated their clinical judgment as more effective than guidelines in improving patient health outcomes (P<.01) and more frequently rated the patient as the greatest barrier to CVD prevention versus nonsolo practitioners (P<.01).
CONCLUSIONS
Though guideline awareness is high, efforts to promote their utilization are needed and may improve quality outcomes. Targeted education and support for CVD prevention may be helpful to older and solo physicians.
Keywords: cardiovascular disease, prevention, physician behavior
Cardiovascular disease (CVD) is the leading cause of death among both men and women in the United States (U.S.).1 Quality of CVD preventive care is suboptimal in the U.S., particularly among women, contributing to documented gender disparities in CVD outcomes.2–8 Numerous expert guidelines have been developed to assist physicians in determining appropriate CVD preventive care based on an individual's risk level.9–11 Utilization of these guidelines in practice is essential to reduce the burden of CVD; yet, little is known about barriers to widespread adoption of guidelines.
Delivering high-quality care is important for all health care providers. Physicians in specific subgroups, such as younger physicians and those in solo practices, may be at heightened risk of delivering less optimal care because of lack of experience and support. A recent systematic review that included studies of self-reported knowledge, attitudes, and observed medical practice (i.e., chart audits and administrative data review) assessed length of time in clinical practice as a physician characteristic that may explain variations in quality of care.12 The review suggested that older physicians were at risk of providing lower-quality health care than their younger counterparts.12 However, the association between physician/practice characteristics and quality of CVD preventive care was not specifically evaluated. Therefore, it is unknown whether physician/practice characteristics predict physician awareness/incorporation, effectiveness, perceived barriers, and clinical judgment/practice regarding CVD preventive care.
The purpose of this study was to determine whether there is an association between physician/practice characteristics and quality of CVD preventive care among a random sample of U.S. physicians using a cross-sectional survey and an experimental case-study design. For purposes of this study, quality of CVD preventive care was defined by several parameters including: (1) awareness and incorporation of CVD prevention guidelines, (2) self-reported effectiveness in helping patients prevent CVD, and (3) accuracy of calculation of CVD risk and consistency of preventive recommendations with national guidelines based on experimental case studies. A secondary objective was to evaluate barriers to CVD guideline adherence by physician/practice characteristics.
METHODS
Subjects
The methods of physician selection and survey design have been published previously.13 Briefly, in November 2004, an online cross-sectional survey was administered to a stratified random sample of 500 full-time, U.S. physicians (300 primary care physicians [PCPs], 100 obstetricians/gynecologists [OBGyns], and 100 cardiologists [CARDs]) drawn from the J. Reckner Associates national database of over 300,000 representative health care professionals. The research panel participants have been compiled over the years by multiple mechanisms (e.g., random dialing, purchased samples, referrals) and are unbiased with respect to an artificially high concentration of internet users. Regional samples for large population specialties were drawn using a “rolling over blocks” method to ensure that there is no overuse of samples within specialty.
The initial response rate was 13%, 10%, and 15% among PCPs, OBGyns, and CARDs respectively, typical of a single mailing response rate for an epidemiologic survey. Rather than repeated mailings to individual physicians, invitations were sent to additional physicians in the database until the prespecified stratified sample sizes were achieved.
To qualify for the research study, physicians had to be board certified or board eligible in their respective specialties and be in full-time clinical practice between 3 and 30 years postresidency. Each physician completed a standardized questionnaire including demographic information, practice type and setting, and characteristics of patients in their practice.
Survey Methods
The survey included standardized questions about awareness/incorporation of 3 national CVD prevention guidelines (National Cholesterol Education Program [NCEP], Adult Treatment Panel [ATP] III, the Joint National Committee on the Prevention, Detection, and Treatment of High Blood Pressure [JNC] 7, and the American Heart Association [AHA] Evidence-Based Guidelines for Women). Effectiveness in helping patients prevent CVD and perceived barriers to CVD prevention were evaluated using a 4- and 10-point Likert scale of agreement, respectively. Physicians were also asked to identify optimal levels of low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, Hemoglobin (HbA1c), and fasting plasma glucose for males and females. In addition, physicians were given experimental case studies to test their knowledge of the NCEP ATP III Framingham risk categories based on the Framingham global risk score (high risk=10-year absolute coronary heart disease risk >20%, established CVD, or coronary heart disease risk equivalent; intermediate risk=10-year absolute coronary heart disease risk 10% to 20%; or low risk=10-year absolute risk <10%).
Each physician was presented with 10 experimental patient cases (2 low risk, 4 intermediate risk, and 4 high- risk based on the Framingham global risk score), which included experimentally varied information about the patient's age, gender, ethnicity/race, smoking status, total cholesterol level, LDL-cholesterol level, HDL-cholesterol level, triglycerides, blood pressure, treatment for hypertension, body mass index, family history of coronary heart disease, personal history of coronary heart disease, or diabetes mellitus. The physician was asked to assign a level of risk to each of the 10 cases and then to make specific CVD preventive recommendations for the case based upon their risk level. A detailed description of the 10 experimental cases has been published previously.13
Statistical Methods
Descriptive statistics of the physicians' and their practices are presented as proportions and means (±standard deviation). Agreement with statements about awareness and incorporation of CVD prevention guidelines and perceived barriers to CVD prevention was assessed by a 10-point Likert scale (top 2 points: strongly agree/agree vs others). Agreement with statements about physician effectiveness was evaluated using a 4-point Likert scale (top point: very effective vs others). A z-statistic of proportions was used to test differences in awareness, incorporation, effectiveness, and perceived barriers between physicians based upon their age and practice type. Correct identification of lipid and glucose levels was categorized according to levels recommended by prevention guidelines.9,10 Differences in the percent of physicians making each type of preventive therapy recommendation by age and practice type were also evaluated with a z-statistic of proportions.
Multivariable regression models were used to investigate the effect of physician age and practice type on awareness of and adherence to CVD prevention guidelines, independent of other physician characteristics including gender and specialty. Cut points for physician age (<50 years [younger] vs 50+ years [older]) were based on the age distribution of the sample. All analyses were performed using SAS software (Version 9.1.3, SAS Institute Inc., Cary, NC). Statistical significance was set at P<.05.
RESULTS
Physician/Practice Characteristics
Characteristics of the physician's and their practices are provided in Table 1. Compared with younger physicians (<50 years), older physicians (50+ years) were more likely to be male (P<.001) and in solo practices (P<.001), and less likely to specialize in primary care (P=.02). Similar to previous research,12 physician age and number of years in practice were highly correlated (r=.89, P<.001).
Table 1.
Characteristics of Physicians and Physician Practices
| Overall (N=500) | Physician Age | ||
|---|---|---|---|
| Younger (<50y)(N=283) | Older (50+ y) (N=217) | ||
| Age, mean±SD | 48 (±8) | 43 (±5) | 55 (±5) |
| Years practicing, mean±SD | 17 (±7) | 12 (±5) | 23 (±4)* |
| Gender (%) | |||
| Male | 85 | 78 | 95* |
| Specialty (%) | |||
| PCP | 60 | 65 | 54† |
| CARD | 20 | 17 | 24 |
| OBGyn | 20 | 18 | 23 |
| Practice region (%) | |||
| East | 30 | 32 | 28 |
| West | 16 | 16 | 16 |
| South | 32 | 31 | 35 |
| Central | 22 | 22 | 22 |
| Solo practice type (%) | 28 | 20 | 38* |
| % Patients ≥65 y, mean (SD) | 33 (±16) | 32 (±15) | 35 (±17) |
| % Caucasian patients, mean (SD) | 70 (±22) | 69 (±22) | 71 (±22) |
| % Female patients, mean (SD) | 64 (±19) | 64 (±18) | 65 (±20) |
Significant difference between older (50+ years) and younger (<50 years) physicians at P<.01, using a z-statistic of proportions.
Significant difference between older (50+ years) and younger (<50 years) physicians at P<.05, using a z-statistic of proportions.
SD, standard deviation; PCP, Primary care; CARD, cardiology; OBGyn, obstetrics/gynecology. Rounding error may result in sums<or>than 100.
Awareness/Incorporation of CVD Prevention Guidelines
Among all physicians, there was a relatively high level of awareness of NCEP ATP III (89%) and JNC 7 guidelines (86%), while awareness of the more recently published AHA Evidence-Based Guidelines for Women was lower (64%). Physician awareness of these CVD prevention guidelines differed significantly by physician age and practice type (solo vs nonsolo) after controlling for physician specialty and gender in a multivariable logistic regression model (Fig. 1). Age was a significant, independent predictor of NCEP ATP III guideline awareness, with older physicians (50+ years) reporting greater awareness than physicians <50 years (P=.04). In addition, nonsolo practitioners reported heightened awareness of NCEP ATP III guidelines versus solo practitioners (P=.04).
FIGURE 1.
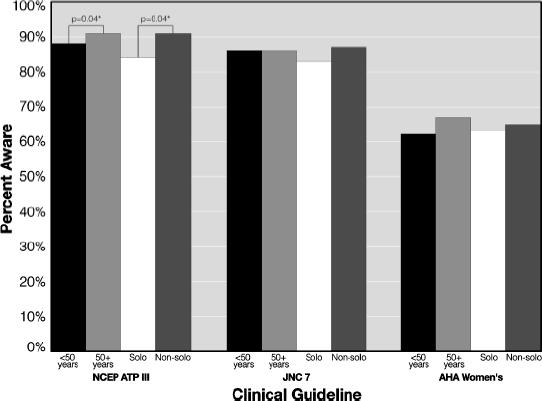
Awareness of national CVD prevention guidelines by physician age and practice type.
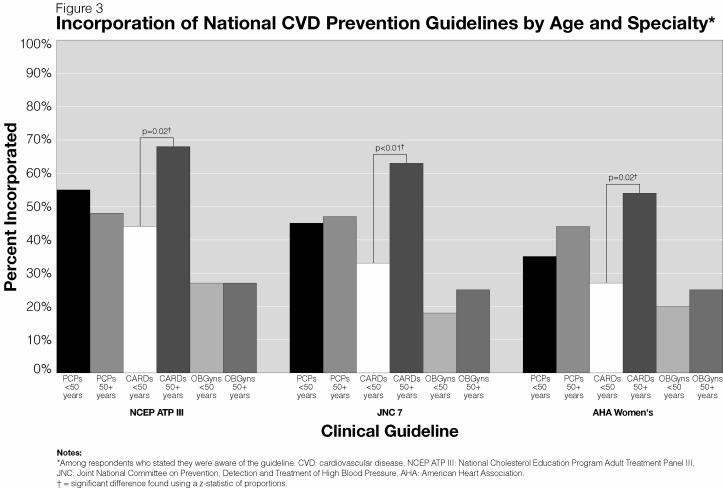
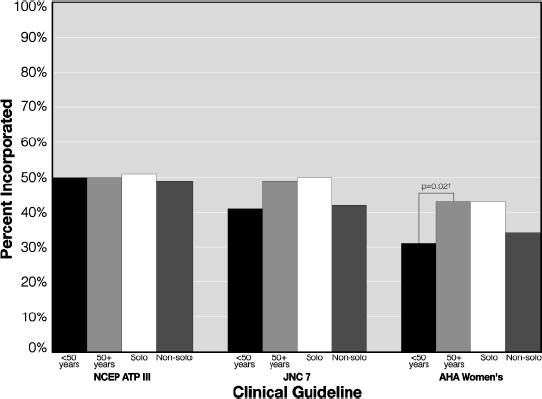
Despite relatively high levels of guideline awareness among physicians, Figure 2 demonstrates that self-reported incorporation of guidelines was lower than awareness levels (NCEP ATP III 50% versus JNC 7 44% versus AHA Women's 36%). Incorporation of the AHA Women's Guidelines varied by physician age; older physicians (50+ years) were significantly more likely to report incorporating the AHA Women's Guidelines for the treatment and prevention of CVD in women and using them in evaluating risk and making treatment recommendations in their practice when compared with physicians <50 years in a multivariable model controlling for physician specialty, gender, and practice type (P=.02). In stratified analysis according to physician age and specialty (Fig. 3, online), older cardiologists (50+ years) were significantly more likely to report incorporating NCEP ATP III (P=.02), JNC 7 (P<.01), and AHA Women's Guidelines (P=.02) compared with younger cardiologists (<50 years).
FIGURE 2.
Incorporation of national CVD prevention guidelines by physician age and practice type*.
Notes: *Among respondents who stated they were aware of the guideline. CVD, cardiovascular disease; NCEP ATP III, National Cholesterol Education Program Adult Treatment Panel III; JNC, Joint National Committee on Prevention, Detection and Treatment of High Blood Pressure; AHA, American Heart Association. †Significant difference found in a multivariable regression model when controlling for physician specialty and gender.
Physician Effectiveness
Overall, physicians' self-reported effectiveness for helping patients prevent CVD was low (Table 2, online). Physicians' effectiveness varied by age, with younger physicians (<50 years) significantly more likely to report feeling effective in helping patients manage their weight (11% vs 6%, P=.045) compared with older physicians (50+ years).
Framingham/ATP III Risk Versus Perceived Risk
Physicians' perceptions of patients' risk levels, based on experimental cases, were compared with calculated risk, based on NCEP ATP III Framingham risk scores,10 and stratified by physician age and patient gender. Less than half of all physicians (47%) correctly categorized patient risk level according to Framingham scores. Among the remaining 53% of physicians, 27% overestimated the experimental case's risk level and 26% underestimated their risk. The accuracy of CVD risk assessment did not differ significantly by practice type or physician age.
Preventive Recommendations
Preventive recommendations made for patients, based upon experimental case studies, are listed in Table 3 according to the experimental case's risk level (as assessed by the physician) and physician age. In a multivariable model controlling for physician specialty, gender, and practice type, older physicians (50+ years) were less likely than younger physicians (<50 years) to recommend weight management for high-risk cases with a body mass index=27 kg/m2 (68% vs 76%, P=.03).
Table 3.
CVD Preventive Recommendations by Physician Age According to Risk Level of Experimental Case
| Calculated Risk Level of Case | ||||||
|---|---|---|---|---|---|---|
| High | Intermediate | Low | ||||
| Physician Age | ||||||
| <50 y (N=283) | 50+ y (N=217) | <50 y (N=283) | 50+ y (N=217) | <50 y (N=283) | 50+ y (N=217) | |
| Physical activity | 91 | 91 | 94 | 92 | 89 | 85 |
| Cardiac rehabilitation | 13 | 8 | 4 | 2 | 3 | 1 |
| Dietary counseling | 82 | 79 | 80 | 76 | 76 | 74 |
| Weight management | 77 | 70* | 76 | 68 | 24 | 23 |
| Dietary supplementation | 16 | 13 | 15 | 12 | 15 | 12 |
| Pharma BP control | 85 | 89 | 49 | 51 | 2 | 3 |
| Pharma lipid control | 48 | 48 | 44 | 46 | 75 | 77 |
| Aspirin therapy | 80 | 82 | 65 | 69 | 36 | 45 |
| Hormone therapy | 0 | 1 | 0 | 0 | 1 | 1 |
Values are percentages.
Significant difference between older (50+ years) and younger (<50 years) physicians at P<.05, using a multivariable logistic regression model controlling for physician specialty, gender, and practice type.
CVD, cardiovascular disease; Pharma, pharmacological; BP, blood pressure.
Preventive recommendations made by practice type and case risk level (calculated by the physician) are presented in Table 4. Solo practitioners were more likely to recommend aspirin therapy for low-risk female cases than nonsolo practitioners (49% vs 36%, P=.02).
Table 4.
CVD Preventive Recommendations by Practice Type According to Risk Level of Experimental Case
| Calculated Risk Level of Case | ||||||
|---|---|---|---|---|---|---|
| High | Intermediate | Low | ||||
| Practice Type | ||||||
| Solo (N=139) | Nonsolo (N=361) | Solo (N=139) | Nonsolo (N=361) | Solo (N=139) | Nonsolo (N=361) | |
| Physical activity | 91 | 91 | 93 | 93 | 90 | 86 |
| Cardiac rehabilitation | 13 | 10 | 5 | 2 | 3 | 2 |
| Dietary counseling | 80 | 81 | 79 | 77 | 74 | 76 |
| Weight management | 73 | 75 | 71 | 73 | 25 | 23 |
| Dietary supplementation | 17 | 14* | 16 | 12 | 15 | 13 |
| Pharma BP control | 87 | 87 | 49 | 49 | 4 | 1 |
| Pharma Lipid control | 49 | 48 | 50 | 43 | 81 | 74 |
| Aspirin therapy | 85 | 79 | 73 | 64 | 49 | 36* |
| Hormone therapy | 0 | 0 | 0 | 0 | 1 | 1 |
Values are percentages.
Significant difference between solo and nonsolo practitioners at P<.05, using a multivariable logistic regression model controlling for physician specialty, gender, and age.
CVD, cardiovascular disease; Pharma, pharmacological; BP, blood pressure.
Correct identification of an optimal LDL-cholesterol level varied by physician/practice characteristics. While over 50% of the sample identified an optimal LDL-cholesterol level as <100 mg/dL (2.59 mmol/L), younger physicians (<50 years) were significantly more likely to identify this goal than older physicians (50+ years) in a multivariable regression model controlling for physician specialty and gender (60% vs 46%, P=.01), as were nonsolo practitioners versus solo practitioners (58% vs 45%, P=.02).
Physician Barriers to CVD Prevention
Barriers to CVD prevention rated by the respondents are presented in Table 5 (online) by physician age and practice type. A greater percentage of older physicians (50+ years) reported that they are more likely to adopt treatment guidelines into practice that are published within their own specialty versus physicians <50 years (26% vs 18%, P=.03), as did solo practitioners versus nonsolo practitioners (28% vs 19%, P=.03). Solo practitioners also rated their clinical judgment as more effective than guidelines in improving health outcomes for their patients versus nonsolo practitioners (14% vs 6%, P=.004), and more frequently rated the greatest barrier to CVD prevention to be the patient him/herself (39% vs 24%, P=.003).
DISCUSSION
A main finding in our study was that while older physicians (50+ years) reported a higher level of awareness and incorporation of national CVD prevention guidelines than younger physicians, they demonstrated equal or poorer adherence to national CVD prevention guidelines as their younger counterparts based upon their responses to experimental case studies. The discrepancy between self-reported awareness/incorporation and case-study performance may be attributed to self-report bias or deficits in the application of CVD prevention guidelines.
Our data are concordant with a systematic review of studies published between 1966 and 2004, which provided empirical results about medical knowledge and quality-of-care outcomes using years in clinical practice (or physician age) as an explanatory variable.12 The review found that increasing physician age independently influenced knowledge and quality of care. In particular, it was found that physicians who were in practice longer were at risk for providing lower-quality care. Our study also found physician/practice characteristics to be significant predictors of preventive recommendations and self-reported effectiveness. Specifically, increased age and solo practice type were correlated with nonadherence to aspirin therapy and weight-management recommendations and reduced self-reported effectiveness in counseling patients on weight management.
Our data found that older physicians were less likely to recommended weight management when appropriate.9 The documented undertreatment of overweight/obesity by physicians may be, in part, because of the relatively poor efficacy of current treatments for obesity.14,15 However, even minor, short-term weight loss can lead to improved cardiovascular health, suggesting that continuing medical education and support on weight-management recommendations should be targeted to older physicians, especially in light of the growing obesity epidemic identified in the U.S. and the association between obesity and CVD.1,16 Additionally, we found that, overall, physicians felt ineffective in helping patients maintain a healthy weight, consistent with previous research. Tsui et al.17 showed that few physicians' feel very effective in weight-management counseling. Our data extend this finding to show that older physicians feel even less effective than younger physicians, a potential result of a physician's professional and personal experience with weight/waist expansion in middle to older age.
Our study found that older physicians and solo practitioners were less likely to correctly identify an LDL-cholesterol level <100 mg/dL (2.59 mmol/L) as optimal despite NCEP ATP III and AHA guidelines consistently stating <100 mg/dL (2.59 mmol/L) is optimal for all persons and a recent update to NCEP ATP III suggesting an LDL-cholesterol level <70 mg/dL (1.81 mmol/L) is an optional target for high-risk patients.9,10,18 Both epidemiological and randomized clinical trial data support that the attainment of optimal lipid levels is associated with decreased CVD morbidity and mortality. Our data underscore the need for physician education on optimal lipid levels and established therapies to manage lipids.
Our data documented that nonsolo practitioners reported a higher level of awareness of national CVD prevention guidelines and that solo practitioners were more likely to recommend aspirin therapy for low-risk female cases, which is inconsistent with national evidence-based guidelines for CVD prevention in women.9 The routine use of aspirin among women with a 10-year absolute risk <10% is a Class III, Level B recommendation, suggesting there is no overall benefit and possible adverse effects of aspirin in low-risk women.9 Although a recent study among low-risk women found a benefit for ischemic stroke among women over 65 years of age who were randomized to aspirin versus placebo, this study was not published at the time of our data collection. Moreover, the overall CVD impact for low-risk women was null and side effects were frequent.19 Compared with previous research on myocardial infarction patients, we did not find differences in aspirin therapy recommendations for high-risk cases in our study, which may be because of secular trends in management as most recent research on utilization of aspirin among high-risk subjects' shows significant levels of adherence.13,20–23
Overall, awareness of CVD prevention guidelines was found to be high in our study. However, the majority of physicians reported much lower rates of incorporation of CVD prevention guidelines into practice. A similarly low rate of guideline incorporation was found in a national survey of family physicians.24 Solo practitioners in this study were less aware of and vested in CVD prevention guidelines, consistent with previous literature documenting that physicians in solo practices adopt significantly fewer guidelines/procedures compared with those in nonsolo practices.25,26 Significantly more solo practitioners strongly agreed that their clinical judgment is usually more effective than guidelines in improving health outcomes in their patients and that the greatest barrier to CVD prevention is the patient compared with nonsolo practitioners. Both older physicians and solo practitioners reported a greater willingness to adopt treatment guidelines into their practice that have been published by professionals within their own specialty, rather than outside their specialty, compared with their counterparts. This finding may explain why CVD prevention guidelines are less likely to be adopted by physicians in specialties other than those writing the guidelines and suggests a more inclusive approach to writing groups may lead to more robust acceptance of guidelines.13 Future research should explore these and other potential barriers to guideline adoption. Efforts should be directed toward the establishment of cross-discipline partnerships to develop and disseminate CVD prevention guidelines, as this may lead to improved quality of CVD preventive care.
Less than half of all physicians (47%) in this study correctly categorized a patient's risk level based upon the experimental case data provided. An equal proportion of the remaining 53% of physicians either overestimated or underestimated the patient's risk level. This finding suggests that almost half of all physicians are misclassifying their patients risk level and, thus, providing inappropriate treatment. Further education and training on appropriate utilization of CVD prevention guidelines are desperately needed to improve classification of risk and quality of CVD preventive care provided.
Our study has limitations. The results may not generalize to all physicians as our response rate was limited by design, we did not survey every specialty, and only full-time, practicing physicians participated. Also, there are inherent limitations on self-report of outcomes. Despite this, our data may represent a best-case scenario among full-time practitioners as survey respondents may be more likely to be aware of and adhere to guidelines because of selection bias. We were unable to evaluate differences in recommendations for beta blocker therapy observed in other research studies as high-risk cases in our study were already assigned treatment. We lacked the power to examine whether awareness/incorporation of and adherence to CVD prevention varied by physician gender or race/ethnicity, and no adjustments were made for multiple comparisons and statistical tests. Our results need to be validated in other cohorts and by other study designs.
In conclusion, our data suggest that targeting education and support for CVD prevention may be helpful for physicians, especially those demonstrating deficits in knowledge, risk-level calculation, or performance. Educational interventions for physician subpopulations may improve knowledge of and adherence to CVD prevention guidelines and lead to improved quality outcomes.
Acknowledgments
This research was partially funded by an unrestricted educational grant to the American Heart Association from KOS Pharmaceuticals. A National Institutes of Health training grant provided funding for Dr. Allison Christian to work on this study. Everyone who has contributed significantly to this work has been acknowledged.
Supplementary Material
The following supplementary material is available for this article online at:
Incorporation of National CVD Prevention Guidelines by Age and Specialty.
Physician Self-Reported Effectiveness by Pratice Type and Age.
Physician's Agreement with Statements About CVD Prevention and Guidelines by Practice Type and Age.
REFERENCES
- 1.American Heart Association. Dallas, Texas: American Heart Association; 2005. [May 19, 2005]. Heart disease and stroke statistics—2005 update. Accessed from http://www.americanheart.org. [Google Scholar]
- 2.Mosca L, Manson JE, Sutherland SE, Langer RD, Manolio T, Barrett-Connor E. Cardiovascular disease in women: a statement for healthcare professionals from the American Heart Association. Writing Group. Circulation. 1997;96:2468–82. doi: 10.1161/01.cir.96.7.2468. [DOI] [PubMed] [Google Scholar]
- 3.Kim C, Hofer TP, Kerr EA. Review of evidence and explanations for suboptimal screening and treatment of dyslipidemia in women. A conceptual model. J Gen Intern Med. 2003;18:854–63. doi: 10.1046/j.1525-1497.2003.20910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sueta CA, Chowdhury M, Boccuzzi SJ, et al. Analysis of the degree of undertreatment of hyperlipidemia and congestive heart failure secondary to coronary artery disease. Am J Cardiol. 1999;83:1303–7. doi: 10.1016/s0002-9149(99)00117-4. [DOI] [PubMed] [Google Scholar]
- 5.Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003;107:2185–9. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 7.Jha A, Varosy PD, Kanaya AM, et al. Differences in medical care and disease outcomes among black and white women with heart disease. Circulation. 2003;108:1089–94. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 8.CDC. Missed opportunities in preventive counseling for cardiovascular disease—United States 1199099991995. Morb Mortal Wkly Rep. 1998;47:91–5. [PubMed] [Google Scholar]
- 9.Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672–93. doi: 10.1161/01.CIR.0000114834.85476.81. [DOI] [PubMed] [Google Scholar]
- 10.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Circulation. 2002;106:3143–21. [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Annals Intern Med. 2005;142:260–73. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Mosca L, Linfante AH, Benjamin EJ, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 14.Castaldo J, Nester J, Wasser T, et al. Physician attitudes regarding cardiovascular risk reduction: the gaps between clinical importance, knowledge, and effectiveness. Dis Manag. 2005;8:93–105. doi: 10.1089/dis.2005.8.93. [DOI] [PubMed] [Google Scholar]
- 15.Galuska DA, Will JC, Serdula MK, Ford EA. Are health care professional advising obese patients to lose weight? JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 16.Yanovski SZ, Yanovski JA. Obesity. N Engl J Med. 2022;346:591–602. doi: 10.1056/NEJMra012586. [DOI] [PubMed] [Google Scholar]
- 17.Tsui JI, Dodson K, Jacobson TA. Cardiovascular disease prevention counseling in residency: resident and attending physician attitudes and practices. J Natl Med Assoc. 2004;96:1080–3. [PMC free article] [PubMed] [Google Scholar]
- 18.Grundy SM, Cleeman JI, Bairey Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227–39. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 19.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 20.Willison DJ, Soumerai SB, Palmer RH. Association of physician age and hospital volume with use of aspirin and reperfusion therapy in acute myocardial infarction. Med Care. 2000;38:1092–102. doi: 10.1097/00005650-200011000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Beaulieu MD, Blais R, Jacques A, Battista RN, Lebeau R, Brophy J. Are patients suffering from stable angina receiving optimal medical treatment? QJM. 2001;94:301–8. doi: 10.1093/qjmed/94.6.301. [DOI] [PubMed] [Google Scholar]
- 22.Fehrenbach SN, Budnitz DS, Gazmararian JA, Krumholz HM. Physician characteristics and the initiation of beta-adrenergic blocking agent therapy after acute myocardial infarction in a managed care population. Am J Manag Care. 2001;7:717–23. [PubMed] [Google Scholar]
- 23.Mehta RH, Montoye CK, Gallogly M, et al. Improving quality of care for acute myocardial infarction: The Guidelines Applied in Practice (GAP) Initiative. JAMA. 2002;287:1269–76. doi: 10.1001/jama.287.10.1269. [DOI] [PubMed] [Google Scholar]
- 24.Wolff M, Bower DJ, Marbella AM, Casanova JE. US family physicians' experiences with practice guidelines. Fam Med. 1998;30:117–21. [PubMed] [Google Scholar]
- 25.Freiman MP. The rate of adoption of new procedures among physicians. The impact of specialty and practice characteristics. Med Care. 1985;23:939–45. doi: 10.1097/00005650-198508000-00001. [DOI] [PubMed] [Google Scholar]
- 26.James PA, Cowan TM, Graham RP, Majeroni BA. Family physicians' attitudes about and use of clinical practice guidelines. J Fam Practice. 1997;45:341–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Incorporation of National CVD Prevention Guidelines by Age and Specialty.
Physician Self-Reported Effectiveness by Pratice Type and Age.
Physician's Agreement with Statements About CVD Prevention and Guidelines by Practice Type and Age.