Abstract
We describe a patient who presented with excessive daytime sleepiness (EDS) and was eventually diagnosed with anti-Ma2 encephalitis. Neurological examination disclosed somnolence, left palpebral ptosis, and vertical gaze paresis. A brain MRI showed high signal intensity in the hypothalamus and each hippocampus. Ma2 antibodies were found in the patient’s serum, and fiberbronchoscopy disclosed a lung carcinoma. After three months of steroid treatment, the results of the patient’s neurological exam became normal. We conclude that anti-Ma2 encephalitis may present with mostly isolated EDS and that it may respond to steroids despite old age and the presence of an untreated lung cancer.
Keywords: anti-Ma2 antibodies, diencephalic encephalitis, excessive daytime sleepiness, hypersomnia, paraneoplastic syndrome
Anti-Ma2-associated encephalitis is a paraneoplastic neurological disorder with preferential involvement of limbic, diencephalic, and upper brain-stem regions (Dalmau et al., 2004; Rosenfeld et al., 2001; Voltz et al., 1999). When diencephalic structures are affected, these patients may develop excessive daytime sleepiness (EDS),2 cataplexy, and hallucinations, and may present undetectable or low cerebrospinal fluid (CSF) hypocretin-1 (Dalmau et al., 2004; Landolfi and Nadkarni, 2003; Overeem et al., 2004). Patients with anti-Ma2 encephalitis usually present a combination of symptoms that reflect the dysfunction of the brain areas described above. The isolated involvement of the diencephalic region is very rare. Anti-Ma2 antibodies are mainly associated with testicular and non-small-cell lung cancer, although associations with other tumors have been reported (Dalmau et al., 2004). We describe a patient with EDS leading to the diagnosis of anti-Ma2 encephalitis and detection of a lung cancer.
Case Study
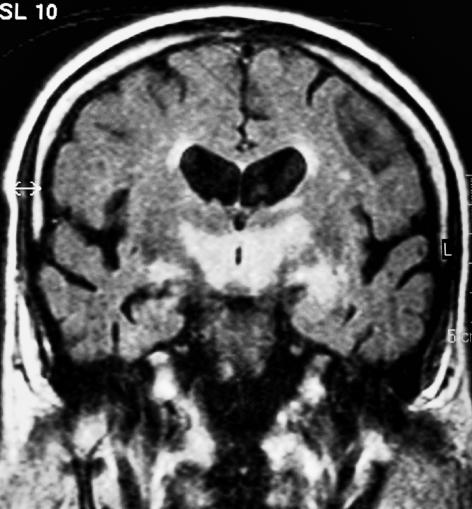
A 71-year-old man was admitted to the neurology ward with somnolence in July 2004. In the previous three months, he had developed asthenia, postural tremor, and increasing somnolence, which after two months left him sleeping for most of the day. During the few moments he was awake, he was confused and disoriented. He had no cataplexy or hallucinations. His past history was remarkable for mild obstructive sleep apnea syndrome (OSAS), cigarette smoking, arterial hypertension, and diabetes. Initially, his pulmonologist suspected severe OSAS and started treatment with continuous positive airway pressure with no response. Neurological examination at admission showed somnolence, left palpebral ptosis, and vertical gaze paresis. The patient remained sleeping during the whole day, and awake periods were rare. The results of routine analyses were normal except for serum and urine sodium levels that were compatible with inadequate secretion of antidiuretic hormone (serum Na, 122 mEq/liter). CSF analysis showed normal glucose, protein level of 59 mg/dl, and 42 white cells, 50% mononuclear cells. Malignant cells were absent in CSF. CSF hypocretin-1 was 58 pg/ml (normal, >110 pg/ml) (Mignot et al., 2002). Ma2 antibodies were positive in serum but were not determined in the CSF. A brain MRI showed high signal intensity in the hypothalamus around the third ventricle and each hippocampus (Fig. 1). The EEG demonstrated bilateral frontal rhythmic delta activity. The results of testicular echography were normal. Thoracic CT and body [18F]fluorodeoxyglucose PET scan showed mediastinic adenopathies. Fiberbronchoscopy disclosed a right bronchopulmonary epidermoid carcinoma.
Fig 1.
Brain MRI FLAIR (fluid-attenuated inversion recovery) sequence showing high signal intensity in the hypothalamus around third ventricle and in each hippocampus.
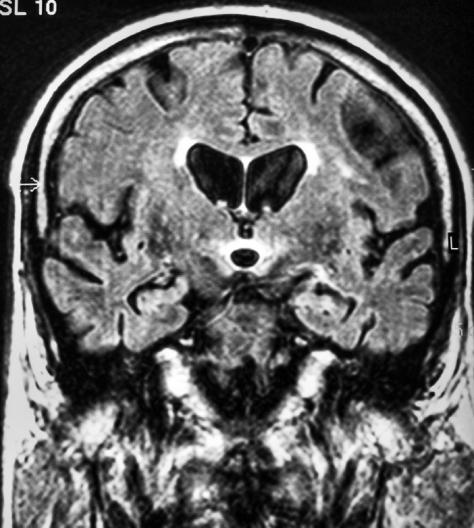
Oncological treatment was initially refused by the patient. He was put on oral steroids (prednisone, 1 mg/kg/day) with progressive improvement of the EDS. Three months later, he was asymptomatic, and the results of a neurological examination were normal. At that time, a new brain MRI showed a remarkable improvement of the diencephalic hyperintensity (Fig. 2). In January 2005, tapering steroids resulted in a neurological relapse with increasing somnolence, which was resolved by raising the dose of steroids. In February 2005, the results of a neurological examination were normal, with a Mini-Mental State Exam score of 28/30.
Fig. 2.
A new brain MRI after treatment and clinical improvement showed reduction of the hyperintensity in the hypothalamus and passive dilatation of the third ventricle.
Discussion
The case of this patient emphasizes that anti-Ma2 encephalitis may present with mostly isolated EDS and that it may respond to steroids despite old age and presence of an untreated lung cancer. EDS was the initial and distinctive symptom along the clinical course. The diencephalic involvement was also confirmed by the low CSF hypocretin-1 (Ripley et al., 2001). Hypocretins are neuropeptides that originate in lateral neurons of the hypothalamus. They probably play a role in regulating normal sleep, appetite, neuroendocrine function, and energy metabolism (Mignot, 2004). Low levels of hypocretin-1 are found in narcolepsy and other neurological disorders like Guillain-Barré syndrome, trauma, brain tumors, and encephalitis. This may reflect hypothalamic lesions or dysfunction, which in some instances may have an autoimmune origin (Arii et al., 2004; Ripley et al., 2001).
In addition, in this patient there were features of limbic (mainly radiological, as somnolence precluded exhaustive neuropsychological examination) and brainstem (mild vertical gaze paresis and ptosis) involvement.
The differential diagnosis of a diencephalic syndrome usually does not include the possibility of a paraneoplastic origin, and this diagnosis may be delayed for several months. In this patient, the previous history of OSAS was probably misleading. As illustrated here, neuroimaging features may be very suggestive of paraneoplastic encephalitis (Fig. 1) but, if unrecognized, may lead to an avoidable biopsy before anti-Ma2 antibodies are investigated (Dalmau et al., 2004).
Neurological improvement is more likely in patients with anti-Ma2 encephalitis than in patients with other paraneoplastic neurological syndromes involving the CNS (Dalmau et al., 2004). This is probably due to the higher chance of curing a testis tumor and completely removing the neoplastic antigenic source. In anti-Ma2 encephalitis, a favorable prognosis is associated with age <45, testicular cancer, complete response to antineoplastic therapy, limited neurological involvement, and absence of anti-Ma1 antibodies (Dalmau et al., 2004). In addition, clinical experience supports that immunotherapy is useful in some of these patients (Dalmau et al., 2004; Scheid et al., 2003). In a recent series of patients with anti-Ma2 encephalitis, 11 of 33 patients had objective neurological improvement. Tumor was treated in all (10 testis tumors and one lung tumor). In three patients, improvement may be attributable to immunotherapy, because the tumor (testis in all) was in remission at the onset of neurological symptoms (Dalmau et al., 2004). Although the lack of anti-Ma1 antibodies was the single favorable factor in our patient, response to steroids was clear and complete and supported by clinical relapse after tapering steroids and subsequent resolution when these were resumed.
We conclude that EDS may be the presenting and main symptom in patients with anti-Ma2 encephalitis. In this clinical setting, paraneoplastic diencephalic encephalitis should be suspected and a brain MRI performed. If, after lumbar puncture and EEG, this diagnosis is still supported, serum onconeuronal antibodies should be searched. Early recognition of this syndrome will increase the chance of achieving a neurological stabilization or improvement and the early detection of a hidden tumor.
Acknowledgments
The authors thank J. Santamaría and J.E. Martínez for the determination of hypocretin-1 and V. Nieto for assistance with the English language.
Footnotes
Abbreviations used are as follows: CSF, cerebrospinal fluid; EDS, excessive daytime sleepiness; OSAS, obstructive sleep apnea syndrome.
References
- Arii J, Kanbayashi T, Tanabe Y, Sawaishi Y, Kimura S, Watanabe A, Mishima K, Hishikawa Y, Shimizu T, Nishino S. CSF hypocretin-1 levels in childhood narcolepsy and neurologic disorders. Neurology. 2004;63:2440–2442. doi: 10.1212/01.wnl.0000147328.15956.b4. [DOI] [PubMed] [Google Scholar]
- Dalmau J, Graus F, Villarejo A, Posner JB, Blumenthal D, Thiessen B, Saiz A, Meneses P, Rosenfeld MR. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004;127:1831–1844. doi: 10.1093/brain/awh203. [DOI] [PubMed] [Google Scholar]
- Landolfi JC, Nadkarni M. Paraneoplastic limbic encephalitis and possible narcolepsy in a patient with testicular cancer: Case study. Neuro-Oncology. 2003;5:214–216. doi: 10.1215/S1152-8517-02-00046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mignot E. Sleep, sleep disorders and hypocretin. Sleep Med. 2004;5 (suppl. 1):S2–S8. doi: 10.1016/s1389-9457(04)90001-9. [DOI] [PubMed] [Google Scholar]
- Mignot E, Lammers GJ, Ripley B, Okum M, Nevsimalova S, Overeem S, Vankova J, Black J, Harsh J, Bassetti C, Schrader H, Nishino S. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002;59:1553–1562. doi: 10.1001/archneur.59.10.1553. [DOI] [PubMed] [Google Scholar]
- Overeem S, Dalmau J, Bataller L, Nishino S, Mignot E, Verschuuren J, Lammers GJ. Hypocretin-1 CSF levels in anti-Ma2 associated encephalitis. Neurology. 2004;62:138–140. doi: 10.1212/01.wnl.0000101718.92619.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ripley B, Overeem S, Fujiki N, Nevsimalova S, Uchino M, Yesavage J, Di Monte D, Dohi K, Melberg A, Lammers GJ, Nishida Y, Roelandse FWC, Hungs M, Mignot E, Nishino S. CSF hypocretin/orexin levels in narcolepsy and other neurological conditions. Neurology. 2001;57:2253–2258. doi: 10.1212/wnl.57.12.2253. [DOI] [PubMed] [Google Scholar]
- Rosenfeld MR, Eichen JG, Wade DF, Posner JB, Dalmau J. Molecular and clinical diversity in paraneoplastic immunity to Ma proteins. Ann Neurol. 2001;50:339–348. [PubMed] [Google Scholar]
- Scheid R, Voltz R, Guthke T, Bauer J, Sammler D, von Cramon DY. Neuropsychiatric findings in anti-Ma2-positive paraneoplastic encephalitis. Neurology. 2003;61:1159–1160. doi: 10.1212/01.wnl.0000085873.45099.e2. [DOI] [PubMed] [Google Scholar]
- Voltz R, Gultekin SH, Rosenfeld MR, Gerstner E, Eichen J, Posner JB, Dalmau J. A serologic marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer. N Engl J Med. 1999;340:1788–1795. doi: 10.1056/NEJM199906103402303. [DOI] [PubMed] [Google Scholar]