Abstract
Background
Patients with irritable bowel syndrome (IBS) are often believed to attribute unexplained symptoms to physical disorders. We tested this hypothesis by assessing symptom interpretation, symptom severity, and quality of life in patients attending hospital gastroenterology clinics.
Aim
The main aims of this study were: to assess the symptom attributional styles of hospital gastroenterological outpatients with IBS and non-IBS disorders in comparison with unselected patients attending their GP; to establish the relationships between attributional style, quality of life, and IBS severity score in hospital gastroenterology outpatients; and to test the hypothesis that the IBS severity score correlates with a somatising style of symptom attribution.
Design of study
Systematic quantitative analysis.
Setting
General practice and gastroenterology outpatient clincs.
Method
Patients attending hospital gastroenterology clinics were recruited prospectively and completed validated questionnaires. These were the Medical Outcome Survey (MOS SF-36), the IBS Severity Score, and the Symptom Interpretation Questionnaire (SIQ). The latter measures the tendency to interpret somatic symptoms in three ways: as a physical disorder (somatising attributional style), as an emotional response to stress (psychologising attributional style), or as a normal experience (normalising attributional style). The diagnosis of IBS was based on the Rome II criteria; the control groups comprised gastroenterology outpatients with non-IBS diagnoses and unselected patients attending general practice.
Results
Quality of life in IBS patients attending hospital outpatients (n = 32, male:female ratio 9:23) was not significantly different from that of non-IBS patients (n = 70, male:female ratio 32:38). In all patient groups, the normalising style of symptom interpretation predominated; psychologising styles correlated with impaired quality of life in the mental health domains. In IBS patients, the tendency to seek a psychological explanation for physical symptoms correlated significantly with the severity of the abdominal pain.
Conclusions
Symptom interpretation does not differ between IBS and non-IBS patients referred to hospital gastroenterology clinics. The tendency to attribute somatic symptoms to a physical disorder does not explain why only a minority of IBS subjects seek medical attention. The idea that most IBS patients are committed to a somatic explanation of symptoms appears to be a myth.
Keywords: IBS severity score, irritable bowel syndrome, quality of life, questionnaires, symptoms
INTRODUCTION
Psychological disorders are commonly associated with irritable bowel syndrome (IBS) but the interplay between the two is complex and the contribution of psychological distress to the induction and maintenance of IBS symptoms remains controversial.1–3 IBS patients referred to hospital are more likely to have greater symptom severity and to attribute their symptoms to a somatic cause compared with IBS patients managed in general practice.4 Somatic symptom attribution is associated with an increased tendency to seek medical consultations and an adverse long-term prognosis.5–7 The corollary is also true: psychological attribution of IBS symptoms has been shown to be associated with a more positive outcome.8,9 However, the prevalence of different attributional styles among patients referred with IBS and the effects of attributional style on the consultation remain unknown.10
Study aims
This study aimed to determine the symptom attributional styles of those outpatients attending gastroenterology clinics with IBS or non-IBS disorders. These findings were then compared with those of unselected patients who had consulted with their GP. It was also hoped that relationships between attributional style, quality of life, and IBS Severity Score (IBSSS) in hospital gastroenterological outpatients could be established, and that the hypothesis that the IBSSS correlates with a somatising attributional style could be tested.
METHOD
Data collection
Subject groups
Subjects were recruited prospectively from two sources: new patients attending hospital gastroenterology outpatient clinics (IBS and non-IBS groups) and patients attending a local general practice (GP group).
Instruments
Gastroenterological outpatients were invited to complete questionnaires containing the IBS Severity Score,11,12 the Medical Outcomes Survey (MOS SF-36)13,14 (to assess quality of life), and the Symptom Interpretation Questionnaire (SIQ).15 The other patient group was an unselected group of GP attenders, all of whom completed the SIQ only. As such, the data sets included the SIQ, MOS-SF36, and the IBSSS in the hospital IBS and non-IBS groups, and the SIQ alone in the GP group.
Diagnosis validation
The primary diagnosis initiating outpatient referral was established on conventional clinical grounds, based on the presenting complaints, clinical examination, and appropriate further investigation. Rome II criteria16 were used to define the diagnosis of IBS and alternative or concurrent gastroenterological diagnoses were confirmed by the results of further investigations. Allocation to the IBS and non-IBS groups followed an independent review of the medical case record by one of the authors that took place 6–12 weeks after the first outpatient consultation.
Instruments
IBSSS
Subjective IBS severity scores were based on five visual analogue scales: severity of pain, duration of pain, abdominal bloating, bowel satisfaction, and interference with the activities of daily living.11–12 Overall IBS severity scores were expressed as a score from 0 (least severe) to 500 (most severe).
MOS SF-36
This 36-item questionnaire is a robust measure of quality of life that has been well validated in patient populations and was used to compare the quality of life in the GP-IBS, hospital IBS, and non-IBS outpatients.13,14 Quality of life is expressed in eight domains (each scored out of 100): physical functioning, role limitation due to physical factors because of health problems, bodily pain, social functioning, general mental health, role limitation due to emotional factors, vitality, general health perceptions.
How this fits in
Our prospective study provides a quantitative analysis of the relationship between symptom attributional style, symptom severity, and quality of life in patients with irritable bowel syndrome (IBS). Patients with IBS are often assumed to ‘somatise’ bodily sensations – although such a phenomenon is in reality an uncommon finding in patients referred with IBS. Our study shows that even in hospital clinics, IBS patients readily accept the possibility of a psychological contribution to their gut symptoms and are, however, no more likely to have a somatising attributional style than unselected GP attenders or non-IBS hospital clinic attenders.
SIQ
The SIQ records the occurrence of 13 common somatic symptoms such as headache or fatigue. For each symptom, patients are asked to consider if they were to experience that symptom whether they would assume that the symptom was the result of an emotional stress (psychologising attributional style), an environmental factor (normalising attributional style), or a physical illness (somatising attributional style). Each attribution is scored on a 4-point Likert scale from ‘not at all’ to ‘a great deal’. The SIQ scale has been validated with respect to its reliability and test-retest correlation over a 4-month period.15
Data analysis
Questionnaires that were inadequately completed due to missing data were excluded from analysis. Non-parametric tests of significance were used throughout and included Kruskal–Wallis, Friedman, ANOVA and Mann–Whitney tests. Within-group comparisons were performed using Wilcoxon rank, Spearman rank, and Friedman tests; significance levels were set at 5% (all tests two-tailed). All data analyses were performed using Excel (Microsoft) and Analyse-It® (Analyse-It, Leeds, UK).
RESULTS
The demographic profile of the study groups is shown in Table 1; non-IBS patients were significantly older and without a female preponderance.
Table 1.
Demographic data of the study groups.
| IBS | Non-IBS | GPa | Total | |
|---|---|---|---|---|
| Total questionnaires | 36 | 79 | 116 | 231 |
| Completed questionnaires | 32 | 70 | 79 | 181 |
| Female (%) | 23 (72.0) | 38 (54.0) | 58 (73.0) | 119 (66.0) |
| Mean age in years | 40.3 | 51.1 | 41.5 | 44.3 |
General practice attenders completed only the Symptom Interpretation Questionnaire.
The primary diagnoses considered to be responsible for the presenting complaint in non-IBS patients referred to the gastroenterology outpatient clinic are shown in Table 2.
Table 2.
Gastroenterological diagnoses in the non-IBS group (n = 70).
| Diagnoses | n (%) |
|---|---|
| Inflammatory bowel disease | 31 (44.3) |
| Hepatobiliary diseases | 17 (24.3) |
| GORD/gastritis/peptic ulcer | 9 (12.9) |
| Miscellaneous | 13 (18.6) |
GORD = gastro-oesophageal reflux disease.
SIQ
In each of the patient groups (hospital IBS, non-IBS, and GP attenders), the normalising style of symptom attribution predominated (P<0.001, Table 3). Overall, there were no significant differences in the relative distribution of symptom attributional styles between the groups (P = 0.3). GP attenders were significantly more likely than non-IBS patients to favour the psychologising attributional style (P<0.001). Similarly, the hospital IBS and GP patients were more likely to favour the normalising attributional style than the non-IBS hospital outpatients (P = 0.009 for IBS versus non-IBS; P<0.001 for GP versus non-IBS).
Table 3.
Symptom Interpretation Questionnaire.
| Mean SIQ scores ± SD | ||||
|---|---|---|---|---|
| Range | IBS (n = 32) | Non-IBS (n = 70) | GP (n = 79) | |
| Psychologising style | 0–39 | 24.6 ± 8.2 | 21.8 ± 8.2 | 27.9 ± 7.2 |
| Normalising style | 0–39 | 29.1 ± 6.4 | 25.6 ± 6.5 | 31.6 ± 6.3 |
| Somatising style | 0–39 | 21.2 ± 4.8 | 21.7 ± 5.6 | 23.9 ± 6.7 |
Quality of life (MOS SF-36)
Both hospital IBS and non-IBS patients showed a similar pattern regarding impairment of quality of life. Vitality was the most impaired domain for both groups, 45% (IBS) and 48% (non-IBS); other domains were reduced to between 60% and 70%.
Hospital IBS group
The psychologising attributional styles approach correlated weakly with the mental health domains of the MOS SF-36: role limitation (emotional) (rs = −0.38, P = 0.038), vitality (rs = −0.37, P = 0.036), emotional wellbeing (rs = −0.42, P = 0.017), somatising attributional style correlated with role limitation (physical) (rs = −0.51, P<0.003). The psychologising attributional style correlated with the pain severity component of the IBSSS (rs = 0.47, P = 0.007). These data are detailed in Figure 1.
Figure 1.
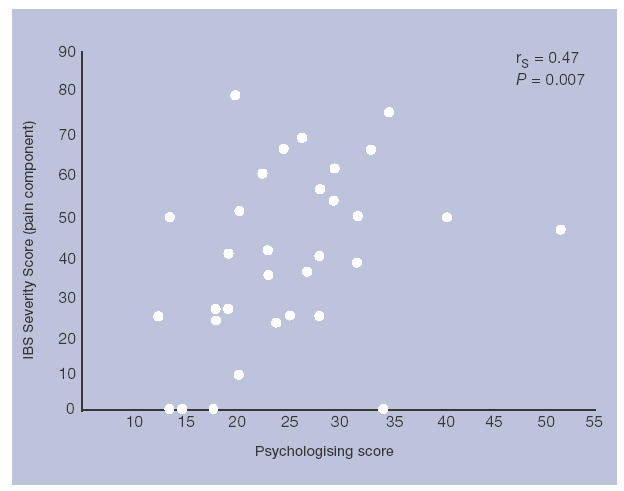
Psychologising score (SIQ) and IBS pain severity.
Hospital non-IBS group
Psychologising attributional styles correlated negatively with the mental health domains of the MOS SF-36: emotional wellbeing (rs = −0.54, P<0.001; Figure 2) and the social functioning domain (rs = −0.45, P<0.001). Somatising attributional styles correlated negatively with all domains of the MOS SF-36, apart from physical function (P<0.01 for all domains).
Figure 2.
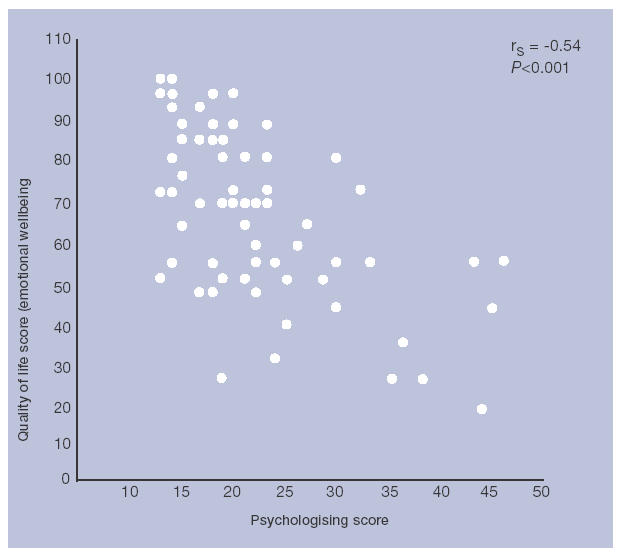
Psychologising score and quality of life in non-IBS patients: emotional wellbeing domain (MOS SF-36).
DISCUSSION
Summary of main findings
Symptom attributional styles were similar in hospital outpatients with IBS and GP attenders – in all groups a normalising style predominated, with no excess of a somatising style in the IBS group. Psychologising attributional styles correlated with the mental health domains of the MOS-SF36; this attributional style may be a feature of psychological comorbidity.
Patients attending general practice were significantly more likely to exhibit psychological and normalising attributions of common somatic symptoms. This may be because patients referred to hospital clinics have more severe symptomatology, more severe health-related anxiety, or are less likely to accept psychological or normalising explanations of unexplained symptoms. The severity of abdominal pain correlates with psychologising attributional styles of symptom interpretation. Previous studies have confirmed that psychological factors affect both symptom severity and health-seeking behaviour.1
The correlation between symptom severity and psychologising attributional styles may reflect the increased psychiatric comorbidity associated with IBS patients referred to hospital clinics.17 In non-IBS patients, psychologising style also correlated with mental health domains of quality of life (and approached significance in the IBS group, which was smaller), reflecting the possibility that this attributional style may be associated with psychological distress.
Strengths and limitations of the study
This prospective study comprises a systematic quantitative analysis of the relationship between attributional style, symptom severity, and quality of life in patients referred with IBS compared with non-IBS patients and patients attending the GP. The absence of a control group of IBS patients in the community not referred to hospital gastroenterology clinics makes it difficult to be confident that our findings are applicable to all patients with IBS. The small size of the IBS group also makes type II statistical errors more likely, such that the existence of a subset of ‘somatisers’ within the IBS group cannot be excluded.
Comparison with existing literature
The literature on the quality of life in patients with IBS shows that quality of life is comparable to that of non-IBS gastroenterology outpatients and similar to that in patients with severe illnesses such as angina and cardiac failure.18,19 Hospital IBS patients have a greater impairment of quality of life in the domains of vitality, emotional wellbeing, and social functioning compared with IBS patients in the community.18
Previous studies have confirmed that females with IBS in the community have less severe and less frequent IBS symptoms compared with hospital IBS outpatients.4
In primary care, patients with functional abdominal complaints can be helped to change their attribution of medically unexplained symptoms to a more psychological attribution, reducing both symptom severity and the persistence of symptoms during 6 months of follow up.8
Although a psychologising style of symptom attribution is associated with a better prognosis, in hospital IBS patients, its presence suggests significant psychological comorbidity.
Implications for clinical practice
Most patients with IBS accept a psychological dimension to their symptoms; they readily appreciate the concept of mind–body interaction and welcome discussion about how psychosocial factors may link with their symptoms.20,21 Many GPs refer IBS patients in the knowledge of the social and psychological context of their symptoms; they and their patients seek reassurance that there is no more sinister explanation for their problem. Hospital doctors need not be afraid to explore all of these factors. Awareness of patients' psychosocial narratives and a positive doctor–patient interaction can help to improve patient satisfaction, compliance with therapy, and reduce consultation rates for IBS-related symptoms.22 The idea that most IBS patients referred to hospital are committed to a somatic explanation of symptoms appears to be a myth.
Acknowledgments
We are particularly indebted to our patients for their participation in the study and to Linda Skeldon, Practice Manager and the practice receptionists for their help in patient recruitment to the study.
Funding body
None
Ethics committee
Lothian Research Ethics Committee (SSC4 – 2003)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Drossman DA. Do psychological factors define symptom severity and patient status in irritable bowel syndrome? Am J Med. 1999;107(5 Suppl 1):41–50. doi: 10.1016/s0002-9343(99)00081-9. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Whitehead WE, Toner BB, et al. What determines severity among patients with painful functional bowel disorders? Am J Gastroenterol. 2000;95(4):974–979. doi: 10.1111/j.1572-0241.2000.01936.x. [DOI] [PubMed] [Google Scholar]
- 3.Herschbach P, Henrich G, von Rad M. Psychological factors in functional gastrointestinal disorders: characteristics of the disorder or of the illness behaviour. Psychosom Med. 1999;61(2):148–153. doi: 10.1097/00006842-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Van der Horst HE, van Dulmen AM, Schellevis FG, et al. Do patients with irritable bowel syndrome in primary care really differ from outpatients with irritable bowel syndrome. Gut. 1997;41(5):669–674. doi: 10.1136/gut.41.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Dulmen AM, Fennis JF, Mokkink HG, Bleijenberg G. The relationship between complaint-related cognitions in referred patients with irritable bowel syndrome and subsequent health care seeking behaviour in primary care. Fam Pract. 1996;13(1):12–17. doi: 10.1093/fampra/13.1.12. [DOI] [PubMed] [Google Scholar]
- 6.Bleijenberg G, Fennis JF. Anamnestic and psychological features in diagnosis and prognosis of functional abdominal complaints: a prospective study. Gut. 1989;30(8):1076–1081. doi: 10.1136/gut.30.8.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fennis JFM, Bleijenberg G, Hermans-van Wordragen R. Psychologic factors in diagnosis, prognosis and treatment of functional abdominal complaints. Scand J Gastroenterol. 1990;25(Suppl 178):3–6. doi: 10.3109/00365529009093145. [DOI] [PubMed] [Google Scholar]
- 8.Van Dulmen AM, Fennis JF, Mokkink HG, et al. Persistent improvement in complaint-related cognitions initiated during medical consultations in functional abdominal complaints. Psychol Med. 1997;27(3):725–729. doi: 10.1017/s0033291796003777. [DOI] [PubMed] [Google Scholar]
- 9.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130(11):910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Dowrick CF, Ring A, Humphris GM, Salmon P. Normalisation of unexplained symptoms by general practitioners: a functional typology. Br J Gen Pract. 2004;54:165–170. [PMC free article] [PubMed] [Google Scholar]
- 11.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 12.Bijkerk CJ, de Wit NJ, Muris JW, et al. Outcome measures in irritable bowel syndrome: a comparison of psychometric and methodological characteristics. Am J Gastroenterol. 2003;98(1):122–127. doi: 10.1111/j.1572-0241.2003.07158.x. [DOI] [PubMed] [Google Scholar]
- 13.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26(7):724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Bensoussan A, Chang SW, Menzies RG, Talley NJ. Application of the general heath status questionnaire SF36 to patients with gastrointestinal dysfunction: initial validation and validation as a measure of change. Aust NZ J Public Health. 2001;25(1):71–77. doi: 10.1111/j.1467-842x.2001.tb00554.x. [DOI] [PubMed] [Google Scholar]
- 15.Robbins JM, Kirmayer LJ. Attributions of common somatic symptoms. Psychol Med. 1991;21(4):1029–1045. doi: 10.1017/s0033291700030026. [DOI] [PubMed] [Google Scholar]
- 16.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–II47. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomson AB, Kerr IJ, Ford MJ, et al. Quality of life (QOL) of Irritable Bowel Syndrome patients in the community. Gut. 1996;39(Suppl 3):A32, 194. [Google Scholar]
- 18.Whitehead WE, Burnett CK, Cook EW, III, Taub E. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996;41(11):2248–2253. doi: 10.1007/BF02071408. [DOI] [PubMed] [Google Scholar]
- 19.Yacavone RF, Locke GR, III, Provenzale DT, Eisen GM. Quality of life measurement in gastroenterology: what is available? Am J Gastroenterol. 2001;96(2):285–297. doi: 10.1111/j.1572-0241.2001.03509.x. [DOI] [PubMed] [Google Scholar]
- 20.Ford MJ, Miller PM, Eastwood J, Eastwood MA. Life events, psychiatric illness and the irritable bowel syndrome. Gut. 1987;28(2):160–165. doi: 10.1136/gut.28.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salmon P, Dowrick CF, Ring A, Humphris GM. Voiced but unheard agendas: qualitative analysis of the psychological cues that patients with unexplained symptoms present to general practitioners'. Br J Gen Pract. 2004;54:171–176. [PMC free article] [PubMed] [Google Scholar]
- 22.Owens DM, Nelson DK, Talley NJ. The irritable bowel syndrome: long-term prognosis and the physician–patient interaction. Ann Intern Med. 1995;122(2):107–112. doi: 10.7326/0003-4819-122-2-199501150-00005. [DOI] [PubMed] [Google Scholar]


