Abstract
Background
Otitis media is the most common reason for children to receive antibiotics, but there is no evidence about the effect of prescribing on reattendance.
Aim
To evaluate the changing workload of middle ear disease in general practice, and the impact on surgery reattendance of prescribing antibiotics at first attendance.
Design of study
A case-linked cohort analysis for antibiotic prescribing versus no prescribing at first consultation event.
Setting
Two hundred and ninety-one practices spread throughout the UK recording for the General Practice Research Database (GPRD) and incorporating individual patient data records for 2 265 574 patients.
Method
All middle ear disease coded events that can be classed within acute otitis media (AOM) or glue ear sub-categories (and excluding chronic suppurative otitis media) were selected for analysis when the first event was from 1991–2001. The effect of antibiotic prescription on the risk of reattendance using Cox proportional hazards regression was analysed.
Results
Total consultations for AOM have fallen markedly over this decade, and glue ear consultations have risen but by a much smaller extent (26 000 decrease versus 4000 increase in consultations per year), which makes re-labelling an unlikely explanation of the fall in AOM consultations. In the 2–10 years age range, consultations for AOM fell from 105.3 to 34.7 per 1000 per year, with glue ear consultations unaltered (15.2 to 16.7 per 1000 per year). Antibiotic prescribing for AOM has stayed remarkably constant (80–84% of consultations), but antibiotic prescribing for glue ear has risen sharply (13 to 62%). Prescribing antibiotics increased the risk of reattendance for AOM (hazard ratio [HR] = 1.09, 95% confidence interval [CI] = 1.07 to 1.10) and has reduced the risk of reattendance for glue ear (HR = 0.92, 95% CI = 0.88 to 0.96).
Conclusion
Prescribing antibiotics for AOM probably increased reattendance, but the opposite effect has been noted for glue ear, which suggests a treatment effect of antibiotics in glue ear. Further research is needed to clarify whether this possible benefit is worth the known harms, and if so in which subgroups of children.
Keywords: acute disease, antibiotics, case studies, cohort studies, otitis media with effusion, reattendance, risk factors
INTRODUCTION
Acute otitis media (AOM) is an acute inflammation of the middle ear with an effusion and is usually triggered by either a bacterial or viral infection.1 When the effusion is ‘sterile’ and there are no acute inflammatory signs then otitis media with effusion or glue ear (its persistent form) is diagnosed.2 This latter condition is the major cause of intermittent deafness and childhood disability.3 It has long been believed that the advent of antibiotics and their inappropriate use has resulted or contributed to grumbling low-key ear infections, which have not been fully eradicated and can lead to the condition of glue ear. More recently a biofilm infection has been mooted as the cause of such persistent effusions.4 This is a surface film infection where the bacteria are structurally organised into clusters and, as a consequence, are more resistant to the use of antibiotics. These two conditions make up the vast bulk of middle ear disease seen in modern western society, and are together responsible for sizeable costs of about £2–300 million annually, and reflect the magnitude of the problem to the NHS. These costs are mostly for consultations and antibiotic prescribing by the GP, but also include the costs of referral and grommets, the operation used to treat glue ear, and the commonest operation in childhood.
The purpose of our study is to evaluate the impact on consultation reattendance for otitis media from the changing use of antibiotics over the past decade, a decade in which restricted use has been advocated.5,6 In particular, we set out to evaluate the hypotheses that antibiotic prescribing for both AOM and glue ear increases GP workload by encouraging parents and patients to reconsult, as the only previous study in AOM was not powered to assess reattendance.7 The prescription/reattendance link has not been studied in glue ear. Related to this, we also sought to evaluate other potential risk factors for increased GP consultations for middle ear disease.
METHOD
We designed a case-linked cohort study where initial antibiotic prescribing for medication was compared with no antibiotic prescribing, and analysed for reattendance by diagnostic category (middle-ear disease: AOM/glue ear). We have chosen to define reattendance for study purposes as the proportions reconsulting in each group after an index episode. We imposed no limit on timing to next consultation event, and multiple events were not counted by our outcome measure.
We used the large well validated General Practice Research Database (GPRD) from 1991 to 2001 to extract our cohorts.8,9 All recorded consultation events coded as otitis media occurring at any age, but excluding all types of chronic suppurative otitis media were selected for our analysis of middle ear disease in general practice. We searched on the relevant OXMIS (Oxford Medical Information System), Read and other codes for all the many and various accepted labels of middle ear disease. Where these codes were less precise, for example, for symptom codes such as otalgia, we systematically classified such cases as AOM. For our glue ear category we have included single consultation data labelled as otitis media with effusion and other aliases, for example, serous otitis media. We also searched on all relevant antibiotic codes prescribed for such infections. Index of multiple deprivation was grouped into tertiles for inclusion into Cox proportional hazards regression models. The Schoenfeld test, having adjusted for all covariates in the model, was used to test for departure from the assumption of proportional hazards.
How this fits in
Otitis media is the commonest reason for children to be prescribed antibiotics, however, antibiotics are not known to be of significant benefit for glue ear. Prescribing antibiotics for the symptoms of AOM is debated, but there is no evidence about the effect of prescribing on reattendance. Overall consultation rates for AOM have fallen but consultations for glue ear have continued to rise. Prescribing antibiotics for AOM is associated with significantly increased reattendance. Prescribing antibiotics is associated with reduced reattendance in glue ear, and may therefore be beneficial in some children.
We only included patients whose first recorded consultation event was between January 1991 and December 2000. We derived specific diagnostic consultation data for AOM and glue ear separately, and did this for each successive study year using the total network figures. We express rates as patients consulting for AOM and glue ear, and as antibiotics prescribed per 1000 patients registered annually with the GPRD.
Case-linked cohort analysis
We identified the first network recorded episode of middle ear disease for each individual case. Those who were prescribed an antibiotic on this index occasion were designated to the antibiotic ‘prescribing’ group, and those who did not receive an antibiotic prescription to the ‘no prescribing’ group. We used follow up data for surgery reattendance on our cohorts. We computed the time between first middle ear disease event and any subsequent event between 1 January 1991 and 31 December 2000. We censored the data for non-recurrent cases. All patients who did not have a second event before 1 January 2001 were censored (that is, treated as having one event). We used a Cox proportional hazards regression model for our analysis of the effect of antibiotic prescribing on the risks of reattendance. Variables considered to be possible confounders of the effect of antibiotic prescription at first consultation event on reattendance (age at first event, sex, high prescribing practice, index of multiple deprivation, and referral to an ear, nose and throat (ENT) department were included in a multivariate Cox proportional hazards regression model, to estimate the adjusted risk for reattendance. A high prescribing practice was defined as in the top quintile of prescribing for AOM and glue ear separately. Stata (version 8, Stata Corporation) was used for the analysis.
RESULTS
Our sample is an all-ages population of 2 265 574 individual patients, whose records were available to the GPRD from 291 UK practices. We identified a total of 322 108 recorded AOM consultation events, and 63 808 glue ear events over a 10-year period. Total consultations for AOM have fallen markedly over the years from 1991 to 2001, and glue ear consultations have risen but to a much smaller extent (Figure 1). The greatest decline was in AOM consultations for children under 2 years of age, with rates falling from 231.0 to 122.7 per 1000 per year, whereas glue ear consultations rose in this age group from 9.0 to 29.4 per 1000 (Table 1). In the 2–10 years age range, AOM consultations fell from 105.3 to 34.7 per 1000 per year, with glue ear consultations unaltered (15.2 to 16.7). Antibiotic prescribing for AOM has stayed remarkably constant, ranging between 80 to 84%, but antibiotic prescribing for glue ear has risen sharply from 13 to 62% (Figure 2). Prescribing antibiotics increases the risk of reattendance for AOM (hazard ratio [HR] = 1.09; 95% confidence interval [CI] = 1.07 to 1.10) and reduced the risk of reattendance for glue ear (HR = 0.92; 95% CI = 0.88 to 0.96) after adjusting for age, sex, multiple deprivation index, ENT (ear, nose and throat) referral, and high prescribing practice (Tables 2 and 3). The unadjusted or crude hazard ratios are 1.13 (range = 1.12–1.15) and 0.94 (range = 0.91 to 0.98) for AOM and glue ear, respectively. Re-attendance was least in those with multiple deprivation index scores in the highest tertile (most economically disadvantaged) and highest in those with deprivation scores in the mid-tertile for AOM (HR = 1.07, 95% CI = 1.05 to 1.09), and glue ear (HR = 1.18, 95% CI = 1.13 to 1.24) (Tables 2 and 3).
Figure 1.
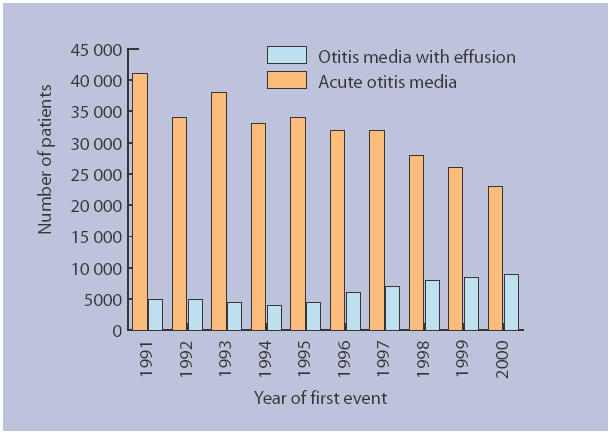
Numbers of consultations by year
Table 1.
Consultation rates per 1000 by age and year for acute otitis media and glue ear.
| Acute otitis media (age in years) | Glue ear (age in years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| >2 | 2–10 | 11–16 | 17–21 | >21 | >2 | 2–10 | 11–16 | 17–21 | >21 | |
| 1991 | 231.01 | 105.31 | 34.16 | 17.52 | 8.65 | 8.96 | 15.21 | 3.89 | 1.92 | 1.51 |
| 1992 | 210.89 | 72.93 | 25.44 | 14.64 | 7.71 | 8.71 | 13.28 | 3.63 | 1.74 | 1.34 |
| 1993 | 231.92 | 73.14 | 26.15 | 14.61 | 8.22 | 8.80 | 11.37 | 2.96 | 1.54 | 1.26 |
| 1994 | 209.49 | 55.69 | 18.36 | 12.01 | 7.40 | 7.23 | 10.58 | 2.28 | 1.39 | 1.14 |
| 1995 | 206.14 | 54.89 | 19.42 | 12.96 | 7.52 | 8.61 | 10.02 | 2.51 | 1.28 | 1.08 |
| 1996 | 195.62 | 47.34 | 13.00 | 9.03 | 6.61 | 16.07 | 11.57 | 2.78 | 1.50 | 1.36 |
| 1997 | 178.64 | 47.79 | 12.60 | 8.47 | 6.61 | 16.54 | 13.73 | 3.03 | 1.43 | 1.45 |
| 1998 | 162.76 | 42.78 | 10.77 | 7.64 | 5.61 | 23.65 | 16.02 | 3.71 | 1.94 | 1.43 |
| 1999 | 143.07 | 36.99 | 8.69 | 7.46 | 5.40 | 26.38 | 15.80 | 4.20 | 2.12 | 1.69 |
| 2000 | 122.73 | 34.69 | 7.69 | 5.90 | 4.86 | 29.35 | 16.74 | 4.55 | 2.52 | 1.93 |
Figure 2.
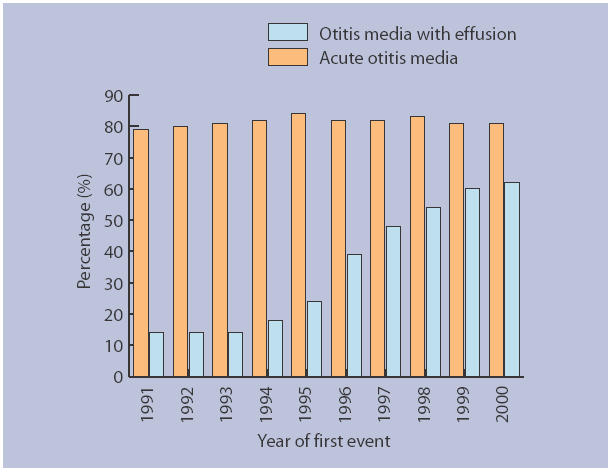
Percentage of acute otitis media/otitis media with effusion cases receiving antibiotics by year
Table 2.
Re-attendance after first consultation event.
| Acute otitis media events (n = 322 108) | Glue ear events (n = 63 808) | |||||
|---|---|---|---|---|---|---|
| Prescribed antibiotics at first event | Prescribed antibiotics at first event | |||||
| Yes (%) | No (%) | Total (%) | Yes (%) | No (%) | Total (%) | |
| All patients | 40.2 | 36.6 | 39.5 | 17.6 | 22.3 | 20.4 |
| Age group | ||||||
| <2 years | 63.9 | 59.6 | 63.3 | 24.91 | 30.4 | 27.1 |
| ≥2 years | 34.1 | 31.9 | 33.7 | 16.5 | 21.8 | 19.8 |
| Sex | ||||||
| Male | 41.7 | 37.8 | 41.0 | 18.6 | 23.1 | 21.3 |
| Female | 38.8 | 35.4 | 38.2 | 16.7 | 21.5 | 19.6 |
| High prescribing GP surgery | ||||||
| No | 39.0 | 36.4 | 38.5 | 17.6 | 22.5 | 21.0 |
| Yes | 43.0 | 38.1 | 42.5 | 17.5 | 20.2 | 18.3 |
| Index of multiple deprivation score | ||||||
| Low (2.16–13.47) | 41.7 | 37.3 | 41.0 | 19.6 | 23.2 | 21.7 |
| Medium (13.48–30.34) | 40.0 | 38.0 | 39.7 | 17.4 | 23.1 | 20.9 |
| High (>30.35) | 39.0 | 35.1 | 38.2 | 16.2 | 21.1 | 19.1 |
| Referral within 1 month | ||||||
| None | 40.1 | 36.5 | 39.5 | 17.2 | 21.7 | 19.9 |
| ENT/audiology department | 45.5 | 38.3 | 43.3 | 37.3 | 33.3 | 34.0 |
ENT = ear, nose and throat.
Table 3.
Multivariate analysis of risk factors for re-attendance.
| Acute otitis media events | Glue ear events | |||||
|---|---|---|---|---|---|---|
| Reattendance | HR (95% CI) | P-value | Reattendance | HR (95% CI) | P-value | |
| Antibiotic prescribed at first event | ||||||
| No | 16 992/46 259 (37%) | 1 | 6666/29 671 (22%) | 1 | ||
| Yes | 83 987/208 728 (40%) | 1.09 (1.07 to 1.10) | <0.001 | 3563/20 097 (18%) | 0.92 (0.88 to 0.96) | <0.001 |
| Age at first event | ||||||
| <2 years | 31 899/50 304 (63%) | 2.55 (2.52 to 2.58) | <0.001 | 1156/4188 (28%) | 1.61 (1.51 to 1.71) | <0.001 |
| ≥2 years | 69 080/204 683 (34%) | 1 | 9073/45 580 (20%) | 1 | ||
| Sex | ||||||
| Female | 50 605/132 478 (38%) | 1 | 5127/26 031 (20%) | 1 | ||
| Male | 50 374/122 509 (41%) | 1.06 (1.05 to 1.07) | <0.001 | 5102/23 737 (21%) | 1.07 (1.03 to 1.11) | 0.001 |
| High prescribing GP surgery | ||||||
| No | 71 451/185 513 (39%) | 1 | 8119/38 566 (21%) | 1 | ||
| Yes | 29 528/69 474 (42%) | 1.09 (1.07 to 1.10) | <0.001 | 2110/11202 (19%) | 1.04 (0.99 to 1.10) | 0.112 |
| Index of multiple deprivation score | ||||||
| Low (2.16–13.47) | 34 776/84 901 (41%) | 1.05 (1.03 to 1.07) | <0.001 | 3555/16 386 (22%) | 1.13 (1.08 to 1.18) | <0.001 |
| Medium (13.48–30.34) | 33 383/84 235 (40%) | 1.07 (1.05 to 1.09) | <0.001 | 3474/16 593 (21%) | 1.18 (1.13 to 1.24) | <0.001 |
| High (>30.35) | 32 820/85 851 (38%) | 1 | 3200/16 789 (19%) | 1 | ||
| Referral within 1 month | ||||||
| None | 100 118/252 941 (40%) | 1 | 9578/47 868 (20%) | 1 | ||
| ENT/Audiology | 861/2046 (42%) | 1.52 (1.43 to 1.63) | <0.001 | 651/1900 (34%) | 1.97 (1.82 to 2.14) | <0.001 |
ENT = ear, nose and throat. HR = hazard ratio.
DISCUSSION
Summary of main findings
This is the first study powered to assess the reattendance effect of prescribing antibiotics for middle ear disease, and demonstrates that prescribing antibiotics for AOM is associated with increased reconsultation, but that prescribing for glue ear has the opposite effect.
Strengths and weaknesses of the study
The strength of this study is the suitability of the design to assess the pragmatic effects of prescribing in routine and representative practice. The main limitations of this study are the inability to control for all possible confounding factors (particularly disease labelling, thresholds of prescribing, and confounding by severity) — although controlling for the level of antibiotic prescribing in practices made no difference. Confounding by severity is a possible explanation here with more severe cases being seen by the GP, who receive antibiotics and subsequently reattend. However, we found that severity indices did not predict subsequent reattendance in a study of patients with upper respiratory tract infections.10 Also we documented proportions reattending (that is, not all episodes of relapse) — but this would be expected to reduce the observed associations. It might have been hypothesised that referral, which is commoner in glue ear (9.9% versus 6.5%), reduced reattendance while parents awaited their child's definitive hospital treatment. In fact, this was not the case as there was an observed positive association between ENT/audiology referral and reattendance (Tables 2 and 3). Furthermore, when we adjusted for the possible confounding effects of referral within 1 month of the index episode, this had only a very marginal effect on the findings, that is, indicating very little confounding. The study is also limited by diagnostic imprecision, given that the diagnoses were those made in routine practice; conversely this means that the results are likely to apply to diagnoses made in routine practice. Any general imprecision in diagnosis, such as non-differential error in case ascertainment, is likely to reduce the size of the observed effects of antibiotics (Table 3).
Comparison with existing literature
Changes in diagnostic rates
There has been a remarkable fall in patients presenting with AOM over the past decade, particularly in the youngest children, and more so since 1997. This suggests that government initiatives to reduce unnecessary antibiotic prescribing — such as the Standing Medical Advisory Committee guidelines6 and the House of Lords Science and Technology report5 on judicious use of antibiotics — and an increase in primary research evidence,11 may have had some effect. Although the reported incidence of all respiratory infections,12 and the birth rate, have also fallen throughout this period it seems unlikely that the true incidence of AOM has become considerably less common, and are thus an insufficient explanation for these behavioural observations. GPs have continued to prescribe at a rate of about 80% suggesting that those patients who latterly presented were possibly those who either expected antibiotics for their children or themselves, and were relatively impervious to the considerable negative publicity surrounding antibiotic use, or indeed were those with more severe ear infections.
In contrast, we have observed a significant increase in presentations with glue ear over this decade, which is unlikely to be accounted for by simply relabelling cases of AOM. In practice, these two conditions are generally well distinguished by GPs with their different presentational history and clinical signs. Furthermore, the different effect of antibiotics in this data set supports reasonably well differentiated diagnoses. The overall rise in consultations for glue ear may be partly linked to the move away from grommets in secondary care, which occurred at the beginning of the 1990s.13 However the actual pattern in consultations is u-shaped for all ages, and this may therefore reflect a change in the disease incidence over the decade.
The effect of prescribing antibiotics on reattendance
It has been previously described that prescribing antibiotics encourages belief in their effectiveness, and this fuels reattendance and increases workload. Clinical severity has been shown to be less important in reattendance behaviour. Our study showed that such reinforcing doctor–patient behaviour in AOM is smaller than previously reported for other upper respiratory tract infections,10 but the latter study involved predominantly adults rather than children. The youngest children (<2 years) remain the most highly prescribed for, and male sex, referral and a high prescribing practice are additional risk factors for reattendance.
In contrast to the increase in reattendance for AOM with initial antibiotics in the current study, there was a reduction for glue ear. Given that the prescribing of antibiotics is likely to reinforce false perceptions of the benefit of antibiotics, and lead to further reattendance for this age group (as we have shown in the current study for AOM consultations, supported by our previous data on beliefs7 and a study on URTI10), the most likely explanation for this observed reduction in reattendance for glue ear is that antibiotics have a treatment effect. This is supported by the minimal effect that potential confounders had on the estimates of the effect of antibiotics. Two high quality meta-analyses estimated the effectiveness of antibiotics as 4% and 14% for glue ear, but have non-significant confidence intervals due to limited power.14,15 However, because this study has much more power it has demonstrated a similar effect size (8%), which is significant (95% CI = 4% to 12%). Prolonged and repeated courses of antibiotics are not without serious disadvantages and are likely to foster further problems with antibiotic resistance.16
Implications for future research
Our study shows that contrary to the long-held theory, antibiotics do not appear to promote glue ear and its recurrence, and would support further research to identify which subgroups of children might selectively benefit from the judicious use of antibiotics.
In conclusion, prescribing for AOM positively reinforces belief in the effectiveness of antibiotics and directly increases practice workload due to increased reattendance. However the opposite effect is noted for glue ear. We infer that antibiotics are likely to be effective in treating this condition in some children. Further research is needed to clarify the benefit, and whether this possible benefit outweighs the harms, and if so in which particular set(s) of children.
Acknowledgments
We wish to thanks Dr Tim Williams of the General Practice Research Database for help with provision of the datasets. We are also grateful for comments on the analysis from Professor Chris Butler.
Funding body
Deafness Research UK (35:SOU:IW)
Ethics committee
General Practice Research Database ethics (SEAG 462)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451–1465. doi: 10.1542/peds.113.5.1451. [DOI] [PubMed] [Google Scholar]
- 2.Stool SE, Berg AO, Berman S, et al. Otitis media with effusion in children. Guideline Technical Report, Number 12. Rockville MD: AHCPR; 1994. (95-0621) [Google Scholar]
- 3.Haggard M, Hughes E. Objectives values and methods of screening childrens' hearing — a review of the literature. London: HMSO; 1991. [Google Scholar]
- 4.Fergie N, Bayston R, Pearson JP, Birchall JP. Is otitis media with effusion a biofilm infection? Clin Otolaryngol. 2004;29:38–46. doi: 10.1111/j.1365-2273.2004.00767.x. [DOI] [PubMed] [Google Scholar]
- 5.Select Committee on Science and Technology. Resistance to antibiotics and other antimicrobial agents. 7th Report. London: HMSO; 1998. (HL 81-I) [Google Scholar]
- 6.Standing Medical Advisory Committee. The path of least resistance. Main report. London: Department of Health; 1998. [Google Scholar]
- 7.Little P, Gould C, Williamson I, et al. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ. 2001;332:336–342. doi: 10.1136/bmj.322.7282.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaye JA, del Malero Montes M, Jick H. Mumps measles and rubella vaccine and the incidence of autism recorded by general practitioners: a time trend analysis. BMJ. 2001;322:460–463. doi: 10.1136/bmj.322.7284.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaye JA, Derby LE, del Malero Montes M, et al. The incidence of breast cancer in the general practice research database compared with national cancer registration data. Br J Cancer. 2000;83:1556–1558. doi: 10.1054/bjoc.2000.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Little P, Gould C, Williamson I, et al. reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–352. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ. 2003;326:138. doi: 10.1136/bmj.326.7381.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleming DM, Ross AM, Cross KW, Kendall H. The reducing incidence of respiratory tract infection and its relation to antibiotic prescribing. Br J Gen Pract. 2003;53:778–783. [PMC free article] [PubMed] [Google Scholar]
- 13.Mason J, Freemantle N, Browning G. Impact of Effective Health Care Bulletin on treatment of persistent glue ear in children: time series analysis. BMJ. 2001;323:1096–1097. doi: 10.1136/bmj.323.7321.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams RL, Chalmers TC, Strange KC, et al. Use of antibiotics in preventing recurrent acute otitis media and in treating otitis media with effusion: a meta-analytic attempt to resolve the brouhaha. JAMA. 1993;270:1344–1351. [PubMed] [Google Scholar]
- 15.Cantekin EI, McGuire TW. Antibiotics are not effective for otitis media with effusion; reanalysis of metaanalysis. Oto Rhino Laryngol Nova. 1998;8:214–222. [Google Scholar]
- 16.Williamson I. Otitis media with effusion. Clinical Evid. http://www.clinicalevidence.org/ceweb/conditions/ent/ent.jsp (accessed 2 Feb 2006)


