Abstract
Background
GPs decide whether or not to prescribe antibiotics for acute cough. Apart from clinical signs and symptoms, non-medical reasons influence this decision as well.
Aim
To obtain a valid estimate of the effect of perceived patient demand.
Design of study
Secondary analysis of cluster randomised controlled trial data.
Setting
Eighty-five Flemish GPs.
Method
GPs completed a preprinted form with medical as well as non-medical information and their prescription for 20 consecutive adult patients consulting with acute cough in the periods February to April 2000 and 2001. The effect of perceived patient demand on antibiotic prescribing was estimated by performing alternating logistic regression analysis. A hierarchical backwards elimination procedure, described by Kleinbaum, was used.
Results
Seventy-two GPs participated, including 1448 patients eligible for analysis; 500 (34.5%) were prescribed an antibiotic and, according to the GP, 218 (15.1%) asked for an antibiotic. In cases of perceived patient demand antibiotics were prescribed significantly more often (odds ratio [OR] = 4.64, 95% confidence interval [CI] = 2.96 to 7.26). In the final model (n = 819; OR = 4.60, 2.59 to 8.17); Hosmer–Lemeshow goodness-of-fit P = 0.72), the effect of perceived patient demand for an antibiotic depended on the outcome of the lung auscultation. When patient demand was perceived, antibiotics were prescribed significantly more often only in the case of a normal lung auscultation or in the case of only one abnormal auscultatory finding (adjusted OR = 20.83, 95% CI = 8.86 to 48.99; adjusted OR = 4.79; 95% CI = 2.16 to 10.60, respectively).
Conclusions
Perceived patient demand has a significant, independent and clinically relevant effect on antibiotic prescribing for acute cough with negative findings on the lung auscultation. Practice guidelines and interventions to optimise antibiotic prescribing have to take this effect into account.
Keywords: antibiotics, general practice, medical decision-making, respiratory tract infections
INTRODUCTION
In general practice, medical decisions are prompted most often by complaints about coughing: 169 times per 1000 patients per year for a new illness episode, especially for acute respiratory tract infections (RTIs).1 Despite the lack of evidence to support the prescription of antibiotics for coughing in case of suspected RTIs,2,3 antibiotics are being overprescribed for this condition, especially in primary care.4,5 This results in an unnecessary financial burden on both the patient and society, as well as adverse effects and development of bacterial resistance.6 Because it is difficult to establish accurate diagnoses of RTIs in general practice, we chose to study this acute problem in primary care based on the most frequent symptom, that is, coughing.7 When we explored the diagnostic and therapeutic decisions of Flemish GPs regarding adult coughing patients by means of focus groups,8 we found medical as well as non-medical reasons for antibiotic prescriptions in case of a suspected RTI.9 Our hypotheses on Flemish GPs' decisions were in line with previous research. In the case of suspected RTI, there is a low degree of certainty in the differentiation between RTIs, for example, between acute bronchitis and pneumonia.10,11 Clinical signs and symptoms, medical reasons, often leave GPs with a diagnostic uncertainty. In the end, the decision whether or not to prescribe antibiotics is taken.12 Prescription behaviour is also determined by doctor- and patient-related factors, for example patient expectations and the GP's perception of them.13 These are clearly non-medical reasons.
How this fits in
Antibiotics are being overprescribed, especially for respiratory tract infections (RTIs). Medical decisions (about RTIs) are prompted most often by complaints about coughing. The evidence base to identify which patient will benefit from antibiotics is poor. Non-medical factors seem to play a part in the prescribing decision as well. Increasing bacterial resistance calls for action. In adult patients with acute cough and a normal lung auscultation or only one abnormal auscultatory finding, perceived patient demand for an antibiotic significantly increased the odds of being prescribed one in general practice. Interventions to optimise antibiotic prescribing have to take this effect into account to support good clinical practice.
A questionnaire study assessing the importance of the focus group determinants for the decision to prescribe antibiotics confirmed that non-medical as well as medical reasons may give rise to antibiotic treatment.14 Patient demand for an antibiotic was mentioned in the focus groups and scored high in the questionnaire study as a non-medical reason for antibiotic prescribing.
Other non-medical reasons have been shown to affect antibiotic prescribing behaviour of GPs as well, such as patient expectations,15,16 and, to a greater extent, GPs' perception of patient expectations.17,18 However, the size of the effect of non-medical reasons, adjusted for medical reasons associated with the prescription of antibiotics has not been presented before.19,20 Therefore, besides validating our focus group and questionnaire study findings, this study aims to establish a valid estimate of the effect of perceived patient demand on GPs' antibiotic prescribing, specifically for patients consulting with acute cough as one of the most prominent complaints, and to contribute to the necessary understanding of this complex prescription decision.
METHOD
Design
We performed a secondary analysis of data collected during a cluster randomised controlled trial.21 This trial aimed to optimise antibiotic prescribing by implementing an evidence-based guideline for acute cough by means of academic detailing. The main recommendation is that most patients with acute cough do not need antibiotics. Nevertheless we mentioned first-choice antibiotics. The primary outcome was the antibiotic prescribing rate by GPs for adult patients with acute cough. We were also interested in the kind of antibiotics prescribed, if any, and whether any change in antibiotic prescribing affected symptom resolution.
Setting and sample
We approached 149 Flemish GPs not reluctant to take part in further study on this topic at the time of the postal questionnaire study.14 Eighty-five GPs agreed to participate in the randomised controlled trial by returning a completed and signed form to collect their characteristics (Figure 1 and Table 1). The ratios the gross amount for antimicrobials for systemic use (Anatomical Therapeutic Chemical (ATC) J; www.whocc.no/atcddd/) on the gross amount for all pharmaceutical specialties and the volume (daily defined dosage [DDD]) of ATC J on the volume for all pharmaceutical specialties are both expressed as percentages on individual prescribing feedback from the National Sickness and Invalidity Insurance Institution (NSIII) to GPs. We asked the participating GPs for these percentages and calculated their mean. The participating GPs were asked to include 20 consecutive adult acute cough patients (for inclusion criteria see Box 1) in the periods February to April 2000 and 2001.
Figure 1.
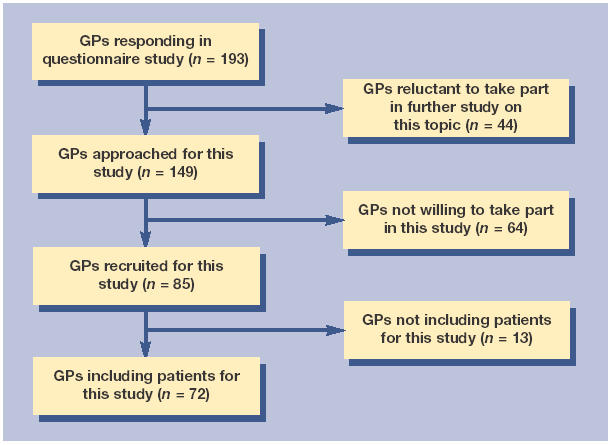
Flow of GPs through the study.
Table 1.
Characteristics of participating GPs (n = 72).a
| Variable | n (%)b |
| Men | 53 (74) |
| University of Antwerp graduates | 32 (44) |
| Professional training | 19 (28) |
| Fee for service | 69 (96) |
| Not single-handed | 35 (49) |
| GPPTsc in practice | 16 (22) |
| Part time | 13 (19) |
| Province | |
| Antwerp | 44 (61) |
| Brussels | 2 (3) |
| Limburg | 5 (7) |
| West Flanders | 12 (17) |
| East Flanders | 9 (13) |
| Peakflow meter | 67 (93) |
| Spirometer | 16 (22) |
| Training practice | 24 (33) |
| Academic link | 23 (32) |
| Records of home visits | 59 (82) |
| Computerised records | 51 (71) |
| Complementary medicine | 2 (3) |
| Mean (SD) | |
| Age at start of this study (years) | 44 (8) |
| Patient encounters per week | 104 (42) |
| Home visits per week | 34 (19) |
| Medical representatives per month | 15 (10) |
| ATC J cost ratio | 15 (7) |
| ATC J volume ratio | 3 (1) |
ATC J = Anatomical Therapeutic Chemical J. SD = standard deviation.
GPs including the 1448 patients eligible for analysis. Their characteristics do not differ from the characteristics of the other GPs who agreed to participate in this study (n = 13).
Denominators vary due to missing values.
GPs in professional training.
Box 1. Inclusion criteria of adult acute cough patients.
-
▸
18–65 years old
-
▸
No compromised immunity
-
▸New or worsening cough:
-
▸present for less than 30 days
-
▸as (one of the) most prominent complaint(s)
-
▸as the reason for the first encounter at the GP's practice
-
▸
Data collection and measures
The GPs were asked to use preprinted forms to record patient demographics, the presence of comorbidity and risk, symptoms and signs, as well as the circumstances of the consultation, the tests ordered, and the prescription of a follow-up visit, of a referral and of an antibiotic (Table 2 and the extended version, Supplementary Table 1). For comorbidity and risk, symptoms, signs, and for the circumstances ‘demands for antibiotics' and ‘demands for other medication’, the three possible answer categories were ‘yes’, ‘no’, and ‘don't know’. For the circumstances ‘workload’ and ‘impression’ the three categories were ‘low’, ‘high’, and ‘very high’, and ‘not ill’, ‘ill’, and ‘very ill’, respectively. For ‘tests ordered’ and ‘prescriptions’, there were only two possible answer categories, ‘yes’ and ‘no’.
Table 2.
Predictors of the prescription of antibiotics by Flemish GPs in adult acute cough patients. Figures are numbers (%) unless stated otherwise.a
| Prescribed antibiotics (n = 500)a | Not prescribed antibiotics (n = 948)a | Crude OR (95% Cl)b (n=1448) | Significance | Adjusted ORc (95% Cl)b (n=819) | Significance | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Mean age in years (SD) | 42.05 (13.03) | 40.23 (13.05) | 1.01 (1.00 to 1.02) | † | 1.02 (1.00 to 1.04) | |
| Comorbidity and risk | ||||||
| COPD | 54/493 (11) | 57/930 (6) | 2.39(1.57 to 3.64) | † | 0.77(0.35 to 1.69) | |
| ACE inhibitor | 17/490 (3) | 18/926 (2) | 2.13 (1.01 to 4.49) | † | 1.05 (0.26 to 4.19) | |
| Aspiration risk | 6/488 (1) | 8/925 (1) | 2.85 (1.87 to 4.34) | † | 14.79 (1.24 to 176.71) | † |
| Smoking | 183/499 (37) | 281/944 (30) | 1.56 (1.25 to 1.95) | † | 1.00 (0.59 to 1.68) | |
| Circumstances | ||||||
| Impression of sickness: ill | 295/480 (61) | 319/901 (35) | 3.04 (2.29 to 4.04) | † | 2.28 (1.47 to 3.53) | † |
| Demand for antibiotics | 125/500 (25) | 93/948 (10) | 4.64 (2.96 to 7.26) | † | 20.83 (8.86 to 48.99) | † |
| Symptoms | ||||||
| Mean (SD) duration of coughing (days) | 6.45 (5.04) | 5.35 (4.73) | 1.05 (1.03 to 1.07) | † | 1.04 (0.99 to 1.10) | |
| Sputum | 374/500 (75) | 458/942 (49) | 3.04 (2.32 to 3.97) | † | 2.52 (1.62 to 3.92) | † |
| Fever | 166/500 (33) | 243/943 (26) | 1.49 (1.17 to 1.89) | † | 1.11 (0.67 to 1.83) | |
| Headache | 281/492 (57) | 446/923 (48) | 1.38 (1.12 to 1.71) | † | 1.57 (1.03 to 2.37) | † |
| Muscle ache | 175/486 (36) | 301/925 (33) | 1.27 (1.01 to 1.59) | † | 0.75 (0.48 to 1.17) | |
| Wheezing | 138/487 (28) | 136/929 (15) | 2.34 (1.78 to 3.07) | † | 0.63 (0.34 to 1.17) | |
| Short of breath | 185/487 (38) | 216/927 (23) | 2.38 (1.85 to 3.05) | † | 1.27 (0.68 to 2.37) | |
| Chest pain | 215/489 (44) | 263/922 (29) | 2.02 (1.61 to 2.52) | † | 1.68 (1.07 to 2.65) | † |
| Loss of appetite | 164/482 (34) | 194/901 (22) | 2.20 (1.69 to 2.87) | † | 1.22 (0.74 to 2.02) | |
| Limited activity | 255/488 (52) | 374/915 (41) | 1.92 (1.47 to 2.52) | † | 1.73 (0.87 to 3.42) | |
| Signs | ||||||
| ‘Higher risk’ | 212/500 (42) | 323/948 (34) | 1.38 (1.11 to 1.71) | † | 1.21 (0.78 to 1.87) | |
| Mean (SD) number of abnormal auscultatory findings | 1.01 (1.09) | 0.36 (0.75) | 2.53 (2.02 to 3.18) | † | 3.04 (2.03 to 4.54) | † |
| Percussion dullness | 9/473 (2) | 6/889 (1) | 6.15 (0.71 to 53.21) | 1.46 (0.15 to 13.80) | ||
| Prescriptions | ||||||
| Referral | 13/496 (3) | 21/932 (2) | 1.71 (0.98 to 3.00) | 0.04 (0.01 to 0.14) | † | |
| Follow-up contact | 69/479 (14) | 68/880 (8) | 3.06 (1.99 to 4.69) | † | 2.18 (0.81 to 5.85) | |
| GPs' characteristics | ||||||
| Professional training | 111/456 (24) | 259/890 (29) | 0.85 (0.56 to 1.29) | 0.20 (0.10 to 0.42) | † | |
| Fee for service | 497/500 (99) | 926/948 (98) | 4.06 (2.64 to 6.23) | † | 1.63 (0.10 to 26.09) | |
| Part-time | 59/489 (12) | 198/333 (21) | 0.52 (0.32 to 0.86) | † | 1.35 (0.35 to 5.16) | |
| Province | ||||||
| Antwerp | 269 (54) | 670 (71) | 1 | 1 | ||
| Brussels | 41 (8) | 28 (3) | 3.38 (1.16 to 9.84) | † | 29.20 (4.85 to 176.71) | † |
| Limburg | 35 (7) | 37 (4) | 2.24 (0.86 to 5.89) | 2.75 (0.88 to 8.63) | ||
| West Flanders | 98 (20) | 93 (10) | 2.07 (1.25 to 3.43) | † | 3.95 (1.60 to 9.76) | † |
| East Flanders | 57 (11) | 120 (13) | 1.12 (0.60 to 2.11) | 1.88 (0.37 to 9.50) | ||
| Spirometer | 93/500 (19) | 303/948 (32) | 0.61 (0.37 to 0.99) | † | 0.44 (0.21 to 0.90) | † |
| Year of birth | 55.99 (7.64) | 55.56 (8.39) | 1.01 (0.99 to 1.03) | 1.22 (1.01 to 1.47) | † | |
| Mean (SD) number of patient encounters per week | 112.14 (46.08) | 101.06 (40.08) | 1.01 (1.00 to 1.01) | † | 1.00 (0.99 to 1.02) | |
| Mean (SD) number of home visits per week | 38.63 (18.80) | 30.53 (17.41) | 1.02 (1.01 to 1.03) | † | 1.03 (1.00 to 1.06) | |
| Mean (SD) ATC J cost ratio | 16.54 (6.64) | 14.28 (6.23) | 1.05 (1.02 to 1.08) | † | 0.94 (0.84 to 1.06) | |
| Mean (SD) ATC J volume ratio | 3.60 (1.44) | 2.91 (1.28) | 1.35 (1.19 to 1.53) | † | 1.58 (0.97 to 2.57) | |
| Design | ||||||
| Registration year: 2001 | 190/500 (38) | 481/948 (51) | 0.64 (0.52 to 0.80) | † | 0.74 (0.42 to 1.28) | |
| Year*group: 2001*intervention | 78/190 (41) | 206/481 (43) | 0.57 (0.40 to 0.82) | † | 0.72 (0.23 to 2.29) | |
| Interaction terms of final model | ||||||
| Demand for antibiotics*number of abnormal auscultatory findings | 1.76 (1.30 to 2.38) | 0.23 (0.13 to 0.41) | ||||
| GP's sex*year of birth | 1.01 (1.00 to 1.01) | 0.90 (0.76 to 1.06) | ||||
ACE = angiotensin converting enzyme. ATC J = Anatomical Therapeutic Chemical J. SD = standard deviation.
Denominators vary due to missing values.
Score test using alternating logistic regression; † = P < 0.05.
Adjusted for all variables in the final model.
GPs in professional training.
Statistical analyses
We calculated frequency distributions of individual variables and assessed univariate associations between each variable and the prescription of antibiotics. We developed a model to obtain a valid estimate of the relationship between perceived patient demand for an antibiotic and GPs' antibiotic prescribing. We used a hierarchical backwards elimination procedure described by Kleinbaum,22 taking clustering of the data into account (Box 2). Before starting the procedure, all categorical variables were dichotomised. Since we aimed to estimate the effect of perceived patient demand for an antibiotic, and since we wanted to control the above relationship only for the presence of the other covariates, we dichotomised comorbidity and risk, symptoms, signs, and the circumstances ‘demands antibiotics’ and ‘demands other medication’ by recoding ‘don't know’ into ‘no’, and the circumstances ‘workload’ and ‘impression’ by recoding ‘very high’ into ‘high’, and ‘very ill’ into ‘ill’, respectively. To deal with co-linearity, the variables ‘reduced breathing sounds’, ‘wheezing’, ‘ronchi’, and ‘crepitations’ were replaced by the variable ‘lung auscultation’, representing the number of abnormal auscultatory findings, while a new dichotomous variable ‘higher risk’ was created based upon Fine's prediction rule to identify patients with community-acquired pneumonia at low risk for mortality or complications,23 and equals one, if the patient's age is over 50 years or if the patient has congestive heart failure, cerebrovascular disease, liver disease, renal disease or neoplastic disease, or has altered consciousness, pulse rate >125/min, respiratory rate >30/min, temperature >38°C or systolic blood pressure >90 mmHg, and which equals zero otherwise (Table 2).
Box 2. Hierarchical backwards elimination procedure and cluster data.
To obtain a valid estimate of the relationship between perceived patient demand for an antibiotic and GPs’ antibiotic prescribing, we estimated a logistic model which contained all covariates as possible confounders and all interaction terms between perceived patient demand and the covariates as possible effect modifiers. The covariates were the other information the GPs recorded about the patients, as well as their characteristics (Table 2). We also added the interaction terms of patient sex and age, and GP's sex and year of birth, respectively, as well as the variables year, group and year*group to control for the randomised controlled trial design. If some of the covariates or interaction terms dropped out of the starting model due to co-linearity, confounding and interaction were evaluated in a stratified analysis of perceived patient demand versus GPs' antibiotic prescribing, controlling for each covariate separately.
First, interactions were assessed by eliminating one by one the interaction term with least significant type 3 score statistics. Only significant interactions were retained in a ‘gold standard’ model. P values of their parameter estimates would be considered significant if smaller than 0.01 instead of smaller than 0.05 only if necessary for a clear interpretation of the effect of perceived patient demand on GPs antibiotic prescribing.
Second, the confounding effect of all covariates not in significant interaction terms in the full model was assessed, followed by precision considerations. We looked for a subset of covariates for which the model gave roughly the same parameter estimates for perceived patient demand and the significant interaction terms, but with narrower confidence intervals.
Alternating logistic regression (ALR),24 a technique closely related to generalised estimating equations (GEE),25,26 was used to adjust the logistic regression estimates for clustering within our data (patients are nested within GPs).27 The marriage of GEE or ALR with goodness-of-fit (GOF) is not an easy one.28–31 In addition to the original Hosmer and Lemeshow GOF statistic,32 we used an extension of that to marginal regression models for repeated binary responses.31 Our approach to fit a broader model with interactions and to test whether the additional terms are significant is regarded as an appropriate way to determine the fit as well.31
Statistical analyses were performed with SAS statistical software.
RESULTS
Seventy-two GPs participated in the study (Figure 1), with 1448 patients eligible for analysis. According to these GPs, 218 (15%) asked for an antibiotic and 500 (35%) were prescribed an antibiotic (Table 2).
Univariate analysis
The prescription of antibiotics was associated with medical and non-medical information. Antibiotics were prescribed more often for older patients, in cases of a medical history of chronic obstructive pulmonary disease (COPD) or a patient reporting a feeling of sickness, in cases of prolonged coughing or symptoms like sputum, fever and shortness of breath, and in cases of more abnormal auscultatory findings or signs such as percussion dullness (Table 2). There was also a higher incidence of antibiotic prescription among the GPs with the highest number of patient encounters and home visits on a weekly basis, and GPs prescribing relatively more antimicrobials for systemic use (ATC J) in cost and in volume (ATC J cost ratio and ATC J volume ratio, respectively). Likewise, there was a strong link between perceived patient demand for an antibiotic and the prescription of one (odds ratio [OR] = 4.64, 95% confidence interval [CI] = 2.96 to 7.26).
For these associations, the dependence of a pair of responses belonging to the same cluster was highly significant, with the intra-cluster correlation coefficient being 0.20 on average.
Multivariate analysis
Interaction terms that were not statistically significant or prevented the model from converging were not retained in the model. Of the variables dropped for the latter reason, only the GPs' year of birth, the number of patient encounters per week and ATC J cost ratio were significant effect modifiers of the univariate relationship between perceived patient demand for antibiotics and the prescription of antibiotics. For younger GPs (year of birth 1965 versus 1945), GPs with fewer patient encounters per week (80 versus 150) and GPs with a higher ATC J cost ratio (0.20 versus 0.10), patient demand was even more strongly associated with antibiotic prescription.
This resulted in a model containing seven interaction terms (patient age, smoking, number of abnormal auscultatory findings, GPs’ university of graduation, part-time working status, registration group [control versus intervention] and registration year [2000 versus 2001]) (P<0.05). After eliminating interaction terms with a P-value greater than 0.01, only one interaction term was retained in the model. In order to obtain a comprehensible and valid estimate of the effect of perceived patient demand for antibiotics on GPs’ antibiotic prescribing, the final model controls for this interaction term and all possible confounders (Table 2).
This model fits the data well (Horton goodness-of-fit [GOFHorton]31 P = 0.71; GOFHosmer–Lemeshow32 P = 0.72). For the patients in the final models (n = 819), the univariate association between perceived patient demand for antibiotics and the prescription of an antibiotic (OR = 4.60, 95% CI = 2.59 to 8.17) was very similar to that for all patients (n = 1448).
Because of the introduction of GPs' characteristics in this model, the dependence for a pair of responses belonging to the same cluster was no longer significant, the intra-cluster correlation coefficient being 0.02.
From the final model we learn that perceived patient demand for antibiotics is still significantly associated with the prescription of antibiotics. This association is independent of the other information the GPs recorded and of their characteristics (Table 2). Significant confounders of this association are aspiration risk (adjusted OR = 14.79, 95% CI = 1.24 to 176.71), an impression of sickness (adjusted OR = 2.28, 95% CI = 1.47 to 3.53), the presence of sputum (adjusted OR = 2.52, 95% CI = 1.62 to 3.92), the presence of of a headache (adjusted OR = 1.57, 95% CI = 1.03 to 2.37), thoracic pain (adjusted OR = 1.68, 95% CI = 1.07 to 2.65), the number of abnormal auscultatory findings (adjusted OR = 3.04, 95% CI = 2.03 to 5.54), investigating infection parameters (adjusted OR = 28.04, 95% CI = 2.86 to 274.54), patient referral (adjusted OR = 0.04, 95% CI = 0.01 to 0.14), the age of the GPs at the start of this study (adjusted OR of year of birth = 1.22, 95% CI = 1.01 to 1.47), previous professional training (adjusted OR = 0.20, 95% CI = 0.10 to 0.42]), having a spirometer in the practice (adjusted OR = 0.44, 95% CI = 0.21 to 0.90), and the practice location (Figure 2).
Figure 2.
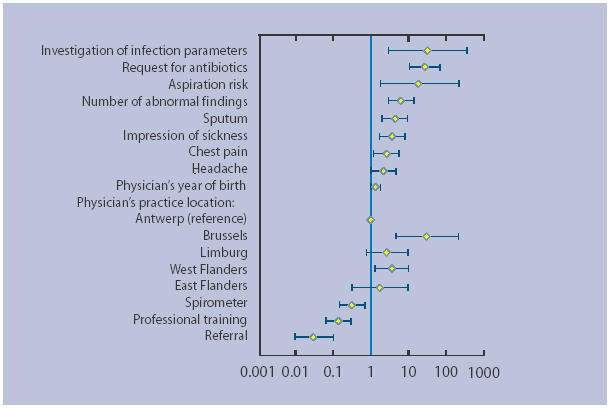
The relationship between the effect of perceived patient demand on antibiotic prescribing for acute cough and the significant confounders of this relation. Adjusted odds ratios and 95% confidence limits.
However, the effect of perceived patient demand for an antibiotic on GPs' antibiotic prescribing depends on the outcome of the lung auscultation. When patient demand for antibiotics is perceived, patients are prescribed an antibiotic significantly more often when the lung auscultation is normal (adjusted OR = 20.83, 95% CI = 8.86 to 48.99]) (Figure 2), or in case of only one abnormal auscultatory finding (adjusted OR = 4.79, 95% CI = 2.16 to 10.60]).
In case of a normal lung auscultation, the adjusted predicted probability for an antibiotic prescription is 0.09 (95% CI = 0.02 to 0.30) if no patient demand for antibiotics is perceived, compared to 0.84 (95% CI = 0.52 to 0.97) if patient demand is perceived. If only one abnormal auscultatory finding is present these probabilities are 0.16 (95% CI = 0.03 to 0.53) and 0.98 (95% CI = 0.92 to 1.00), respectively. If there is more than one abnormal auscultatory finding there is no relevant and significant difference between perceived patient demand and no perceived patient demand.
DISCUSSION
Summary of main findings
Perceived patient demand for antibiotics is significantly associated with the prescription of antibiotics to adult acute cough patients, even when controlling for the other information the GPs recorded and for their characteristics. Antibiotics were prescribed significantly more often when a patient was perceived to demand an antibiotic and the lung auscultation was normal or revealed only one abnormal finding. Aspiration risk, an impression of sickness, the presence of sputum, of headache, and of thoracic pain, abnormal auscultatory findings, investigating infection parameters and a younger GP were also associated with increased antibiotic prescribing. Prescribing depended on the GP's practice location as well. This rather reflects the influence of university departments of general practice involved in RTI research in Antwerp and Ghent, than differences in the competition for patients. Patient referral, previous professional training and having a spirometer in the practice were associated with less prescribing.
Strengths and limitations of the study
Although it is possible, it is unlikely that the results are biased due to the recruitment or the non-response of the GPs, as was stated elsewhere.21,33 The antibiotic prescription volume in packages or in DDDs per GP did not differ between participating GPs and the other Flemish GPs in the period 2000–2001. The age and sex distribution of the GPs who included the 1448 patients eligible for analysis is similar to national averages. Furthermore, in terms of all recorded characteristics, these GPs did not differ from the other GPs willing to participate in the randomised controlled trial (n = 13), nor did those with patients differ from those without patients in the final model.
Patient characteristics might also influence the results of this study. Face-to-face interviews of two samples of about 1000 people representative of the Belgian population aged over 14 years also showed that about 15% of the responders would ask the GP for an antibiotic.34 There were no differences in the patients' characteristics between those records included in the analysis (n = 1448) and those records eligible for the randomised controlled trial (but excluded here because of incomplete data for perceived patient demand for an antibiotic),21 or between those records included and those left out of the final model. Furthermore, the crude OR for all eligible patients (n = 1448) and that of all patients with complete information (n = 819) is 4.64 (95% CI = 2.96 to 7.26) and 4.60 (95% CI = 2.59 to 8.17), respectively, suggesting that there is no bias due to the selection of patients with complete information in the final model.
There was no formal assessment of either the internal validity or the reliability of the preprinted forms; rather, they were assumed acceptable as they had been developed based upon our focus group study,9 and questionnaire study.14 After all, doctors often report abnormal examination findings to justify the decision to prescribe, but even in Belgium, where GPs are remunerated largely on a fee-for-service basis, patient demand is not seen as being an acceptable reason for that, even if actually expressed by the patient. Still, our data show that a non-medical reason is independently associated with increased prescription of antibiotics.
Comparison with existing literature
Acute cough
Knowledge about the determinants that play an important role in clinicians' decisions to prescribe antibiotics for respiratory infections is useful in designing interventions to decrease inappropriate antibiotic prescribing.19,20 For this study, we chose to include patients with acute cough. Although it is the most frequent complaint in general practice there is much uncertainty as to the diagnosis and treatment of patients with an acute cough.20 Surprisingly little evidence is available to support decisions concerning these patients in daily practice.35 It is therefore not surprising that diagnostic labels such as acute bronchitis are used inconsistently in general practice.36 To avoid misclassification, rather broad definitions such as ‘lower respiratory tract illness’ are used in patients with an acute cough.37 When applying the criteria described by Hopstaken and co-workers to our data,38 it was found that 624 acute cough patients (43%) had a lower respiratory tract infection (LRTI). Even more patients met the criteria described by Holmes and MacFarlane (n = 1112 [77%]).37,39 In about 60% of patients with a LRTI and perceived demand for an antibiotic, the lung auscultation was normal or revealed only one abnormal finding, and the effect of perceived demand for an antibiotic on the prescription of antibiotics did not differ between patients with or without a LRTI. This suggests not only that our findings also apply to patients with a LRTI as defined in the literature, but also that choosing to study patients with acute cough is more than justified. After all, there is only limited agreement between the classification of patients with acute cough when applying the above criteria to define patients with a LRTI.
The prescribing decision
In addition to estimating the effect of perceived patient demand on GPs' antibiotic prescribing after adjustment for clinical factors, this study aimed to validate our focus group and questionnaire study findings and to contribute to the necessary understanding of this complex prescription decision. Therefore, we used a hierarchical backwards elimination procedure, starting with interaction assessment.22 Only one interaction term was retained in the final model for a clear interpretation of the estimate of the effect of perceived patient demand. The more conservative model contained seven interaction terms. It would seem that the only meaningful description of these results is that the lower the number of auscultatory findings the more perceived patient demand favours antibiotic prescribing. In previous studies we, and others, also found that a positive lung auscultation in itself was associated with antibiotic prescribing, and that diagnostic uncertainty influenced the complex decision-making process.9,14,19,20 The results of this study support these findings and contribute to the understanding of the prescription decision. After all, it sounds sensible that more abnormal auscultatory findings provide GPs with more certainty regarding the need of an antibiotic, and vice versa. Antibiotics are thus prescribed for medical reasons if these are available, but when GPs have to deal with diagnostic uncertainty, non-medical reasons favour antibiotic prescribing. This can also be attributed to the so-called chagrin factor.9,40 In the present study GPs consider it less appropriate not to prescribe antibiotics when patient demand is perceived, since this causes more chagrin, even if the evidence shows that the limited benefit for patients with acute (productive) cough is outweighed by the side-effects,2,3 and the medicalising effect, the financial costs and the effect on antimicrobial resistance.6
Implications for future research and clinical practice
A clinical practice guideline and an intervention to optimise antibiotic prescribing for acute cough in Flemish general practice have taken non-medical reasons into account. We performed a multifaceted intervention, including educational outreach visits (academic detailing),21 to implement a guideline for acute cough,41 since this might be most effective.42,43 Planning other cluster-randomised trials on this topic one should take into account an intra-cluster correlation coefficient of 0.20 to adjust power calculations.
This study enabled us to obtain a valid estimate of the effect of perceived patient demand for antibiotics on GPs' antibiotic prescribing and confirmed our focus group study and questionnaire study findings, that is, that GPs' decisions to prescribe antibiotics are determined by both medical and non-medical reasons.9,14 Hence, good clinical practice guidelines and interventions to optimise antibiotic prescribing have to take into account non-medical reasons in the prescription of antibiotics.
Supplementary Material
Acknowledgments
We thank all participating GPs and patients, and all who volunteered to help, for their enthusiasm, support and advice. The ISRCTN for this trial assigned by Current Controlled Trials Ltd is 09811591.
Supplementary information
Additional information accompanies this article at http://www.rcgp.org.uk/journal/supp/index.asp
Funding body
Samuel Coenen was research assistant of the Fund for Scientific Research — Flanders. The research was partly funded by a grant (23S/3407) from the University of Antwerp, partly self-funded by the Centre for General Practice of the University of Antwerp
Ethics committee
This study was approved by the medical ethics committee of the University of Antwerp (A99-088)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Okkes I, Oskam S, Lamberts H. Van klacht naar diagnose. Bussum: Coutinho; 1998. [From complaint to diagnosis] [Google Scholar]
- 2.Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomised controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ. 1998;316:906–910. doi: 10.1136/bmj.316.7135.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smucny J, Fahey T, Becker L, et al. Antibiotics for acute bronchitis. In: Cochrane Collaboration, editor. The Cochrane Library. Issue 4. Oxford: Update Software; 2002. [Google Scholar]
- 4.Wise R, Hart T, Cars O, et al. Antimicrobial resistance. Is a major threat to public health [editorial] BMJ. 1998;317:609–610. doi: 10.1136/bmj.317.7159.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koninklijke Academie voor Geneeskunde van België [Belgian Royal Academy for Medicine] Advies inzake het overgebruik van antibiotica [Advice concerning the overuse of antibiotics] Tijdschr Geneesk. 1999;55:173–174. [Google Scholar]
- 6.Butler C, Rollnick S, Kinnersley P, et al. Reducing antibiotics for respiratory tract symptoms in primary care: consolidating ‘why’ and considering ‘how’. Br J Gen Pract. 1998;48:1865–1870. [PMC free article] [PubMed] [Google Scholar]
- 7.Coenen S, Van Royen P, Denekens J. Diagnosis of acute bronchitis [letter; see reply] J Fam Pract. 1999;48:741–742. [PubMed] [Google Scholar]
- 8.Coenen S, van Royen P, Denekens J. Reducing antibiotics for respiratory tract symptoms in primary care: ‘why’ only sore throat, ‘how’ about coughing? [letter] Br J Gen Pract. 1999;49:400–401. [PMC free article] [PubMed] [Google Scholar]
- 9.Coenen S, Van Royen P, Vermeire E, et al. Antibiotics for coughing in general practice: a qualitative decision analysis. Fam Pract. 2000;17:380–385. doi: 10.1093/fampra/17.5.380. [DOI] [PubMed] [Google Scholar]
- 10.Metlay J, Kapoor W, Fine M. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440–1445. [PubMed] [Google Scholar]
- 11.Zaat J, Stalman W, Assendelft W Hoort. wie klopt daar? Een systematische literatuurstudie naar de waarde van anamnese en lichamelijk onderzoek bij verdenking op een pneumonie [Listen, who is knocking? A systematic review on the value of history and physical examination in case of suspected pneumonia] Huisarts Wet. 1998;41:461–469. [Google Scholar]
- 12.Kassirer J. Our stubborn quest for diagnostic certainty. A cause of excessive testing. N Engl J Med. 1989;320:1489–1491. doi: 10.1056/NEJM198906013202211. [DOI] [PubMed] [Google Scholar]
- 13.Butler CC, Rollnick S, Pill R, et al. Understanding the culture of prescribing: qualitative study of general practitioners' and patients' perceptions of antibiotics for sore throats. BMJ. 1998;317:637–642. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coenen S, Michiels B, Van Royen P, et al. Antibiotics for coughing in general practice: a questionnaire study to quantify and condense the reasons for prescribing. BMC Fam Pract. 2002;3:16. doi: 10.1186/1471-2296-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Little P, Williamson I, Warner G, et al. Open randomised trial of prescribing strategies in managing sore throat [see comments] BMJ. 1997;314:722–727. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients' expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315:1211–1214. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cockburn J, Pit S. Prescribing behaviour in clinical practice: Patients' expectations and doctors' perceptions of patients' expectations — a questionnaire study. BMJ. 1997;315:520–523. doi: 10.1136/bmj.315.7107.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Britten N, Ukoumunne O. The influence of patients' hopes of receiving a prescription on doctors' perceptions and the decision to prescribe: a questionnaire survey [see comments] BMJ. 1997;315:1506–1510. doi: 10.1136/bmj.315.7121.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dosh S, Hickner J, Mainous AI, Ebell M. Predictors of antibiotic prescribing for nonspecific upper respiratory tract infections, acute bronchitis, and acute sinusitis. J Fam Pract. 2000;49:407–414. [PubMed] [Google Scholar]
- 20.Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: implications for developing management guidelines. Respir Med. 1997;91:427–434. doi: 10.1016/s0954-6111(97)90258-4. [DOI] [PubMed] [Google Scholar]
- 21.Coenen S, Van Royen P, Michiels B, Denekens J. Optimising antibiotic prescribing for acute cough in general practice: a cluster-randomised controlled trial. J Antimicrob Chemother. 2004;54:661–672. doi: 10.1093/jac/dkh374. [DOI] [PubMed] [Google Scholar]
- 22.Kleinbaum D. Logistic regression: a self-learning text. New York: Springer-Verlag; 1994. [Google Scholar]
- 23.Fine M, Auble T, Yealy D, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 24.Carey V, Zeger S, Diggle P. Modelling multivariate binary data with alternating logistic regression. Biometrika. 1993;80:517–526. [Google Scholar]
- 25.Liang K, Zeger S. Longitudinal data analysis using generalised linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 26.Ridout M, Demétrio C, Firht D. Estimating intraclass correlation for binary data. Biometrics. 1999;55:137–148. doi: 10.1111/j.0006-341x.1999.00137.x. [DOI] [PubMed] [Google Scholar]
- 27.Wears R. Advanced statistics: Statistical methods for analysing cluster and cluster-randomised data. Acad Emerg Med. 2002;9:330–341. doi: 10.1111/j.1553-2712.2002.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 28.Rotnitzky A, Jewell NP. Hypothesis testing of regression parameters in semiparametric generalised linear models for cluster correlated data. Biometrika. 1990;77:485–497. [Google Scholar]
- 29.Pan W. GOF tests for GEE with correlated binary data. Scand J Stat. 2002;29:101–110. [Google Scholar]
- 30.Barnhart HX, Williamson J. GOF tests for GEE modelling with binary responses. Biometrics. 1998;54:720–729. [PubMed] [Google Scholar]
- 31.Horton NJ, Bebchuk JD, Jones CL, et al. GOF for GEE: an example with mental health service utilisation. Stat Med. 1999;18:213–222. doi: 10.1002/(sici)1097-0258(19990130)18:2<213::aid-sim999>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 32.Hosmer DJ, Lemeshow S. Applied logistic regression. New York, NY: John Wiley and Sons; 1989. [Google Scholar]
- 33.Coenen S, Welschen I, Van Royen P, et al. Management of acute cough: differences between Belgian and Dutch GPs. Eur J Gen Pract. 2004;10:152–156. doi: 10.3109/13814780409044303. [DOI] [PubMed] [Google Scholar]
- 34.Bauraind I, Lopez-Lozano J-M, Beyaert A, et al. Association between antibiotic sales and public campaigns for their appropriate use. JAMA. 2004;292:2468–2470. doi: 10.1001/jama.292.20.2468-b. [DOI] [PubMed] [Google Scholar]
- 35.Verheij T. Diagnosis and prognosis of lower respiratory tract infections: a cough is not enough. Br J Gen Pract. 2001;51:174–175. [PMC free article] [PubMed] [Google Scholar]
- 36.Hueston W, Mainous Ar, Dacus E, Hopper J. Does acute bronchitis really exist? J Fam Pract. 2000;49:401–406. [PubMed] [Google Scholar]
- 37.Holmes W, Macfarlane J, Macfarlane R, Hubbard R. Symptoms, signs, and prescribing for acute lower respiratory tract illness. Br J Gen Pract. 2001;51:177–181. [PMC free article] [PubMed] [Google Scholar]
- 38.Hopstaken R, Nelemans P, Stobberingh E, et al. Is roxithromycin better than amoxicillin in the treatment of acute lower respiratory tract infections in primary care? A double-blind randomised controlled trial. J Fam Pract. 2002;51:329–336. [PubMed] [Google Scholar]
- 39.Macfarlane J, Holmes W, Gard P, et al. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax. 2001;56:109–114. doi: 10.1136/thorax.56.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feinstein A. The ‘chagrin factor’ and qualitative decision analysis. Arch Intern Med. 1985;145:1257–1259. [PubMed] [Google Scholar]
- 41.Coenen S, Van Royen P, Van Poeck K, et al. Aanbeveling voor goede medische praktijkvoering: acute hoest [Good clinical practice guideline: acute cough] Huisarts Nu. 2002;31:391–411. [Google Scholar]
- 42.Wensing M, van der Weijden T, Grol R. Implementation guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48:991–997. [PMC free article] [PubMed] [Google Scholar]
- 43.Gross P, Pujat D. Implementing practice guidelines for appropriate antimicrobial usage: a systematic review. Med Care. 2001;39:II55–II69. doi: 10.1097/00005650-200108002-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


