Abstract
Background
Peer support may improve breastfeeding rates but the evidence is inconclusive. Previous studies and reviews recommend trials in different healthcare settings.
Aim
To test if a specified programme of peer support affects the initiation and/or the duration of breastfeeding.
Design of study
A two-group randomised controlled trial of peer support for breastfeeding with evaluation of breastfeeding initiation and duration on an intention-to-treat basis.
Setting
General practice in Ayrshire, Scotland.
Method
Following informed consent, 225 women at 28 weeks gestation were allocated to control or peer support group by post-recruitment concealed allocation. All peer support and control group mothers received normal professional breastfeeding support. Additionally, those in the peer support group still breastfeeding on return home from hospital had peer support until 16 weeks.
Results
Thirty-five of the 112 (31%) women in the peer support group were breastfeeding at 6 weeks compared to 33/113 (29%) in the control group, a difference of 2% (95% confidence interval = −10% to 14%). The median breastfeeding duration for all women in the peer support group was 2 days compared to 1 day for the control group and the Kaplan–Meier survival plot shows the peer support group overall breastfeeding slightly longer than the control group, with no statistically significant difference by log-rank test (P = 0.5). The median breastfeeding duration among primagravidae in the peer support group was 7 days, compared to 3 days for the control group. Among women who started to breastfeed the medians were 72 days in the peer support group and 56 days in the control group. These differences were not statistically significant.
Conclusions
Peer support did not increase breastfeeding in this population by a statistically significant amount.
Keywords: breastfeeding, infant nutrition, lactation, peer group, support groups
INTRODUCTION
Interventions to increase the initiation and duration of breastfeeding have been reviewed by Fairbank et al,1 Sikorski et al,2 Protheroe et al,3 and Guise et al.4 Meta-analysis of randomised or ‘quasi-randomised’ studies of peer (or ‘lay’) support2 showed effectiveness in reducing cessation of exclusive breastfeeding (relative risk [RR] = 0.66; 95% confidence interval [CI] = 0.49 to 0.89) but not in non-exclusive breastfeeding (RR = 0.84; 95% CI = 0.69 to 1.02). A different meta-analysis4 of various programmes of breastfeeding education and support by lactation consultants, nurse or peer counsellors showed increased initiation and duration of breastfeeding. However, this review4 judged four published studies of breastfeeding support by peer counsellors to be of poor quality. Fairbank et al1 reviewed two peer support studies (one of which was included in Guise et al4) which were not randomised controlled trials and conducted in quite different settings but suggested positive effects on breastfeeding.
Morrow et al5 reported a marked increase in the duration of exclusive breastfeeding in a cluster-randomised study of peer counselling and practical support given by three peer counsellors recruited from the local community and trained by La Leche League. The area, on the outskirts of Mexico City, had high breastfeeding initiation rates (92% in a previous study5), but no other sources of breastfeeding support apart from the women's own physicians. The authors commented that their findings could not be generalised to countries with lower initiation rates, or well-established professional community nursing and midwifery support and that further studies are required.
How this fits in
Previous studies report varying degrees of success with the use of peer support as a way of increasing the uptake and duration of breastfeeding. Reviews have pointed out a need for rigorous trials of methods of supporting breastfeeding — particularly in settings with differing degrees of existing professional or volunteer support. A rigorously conducted randomised controlled trial of peer support for breastfeeding women in a primary care setting with existing professional support but little volunteer support shows no statistically significant increase in the overall duration of breastfeeding.
A trial of telephone peer support for 256 mothers in Toronto Canada by Dennis et al,6 using peer supporters who had breastfeeding experience and had undergone a 2.5 hour-long ‘orientation session’, showed significantly increased breastfeeding duration in the intervention group compared to control at 4, 8 and 12 weeks post-partum.
Graffy et al7 recently published the results of a substantial randomised controlled trial of breastfeeding support given by the National Childbirth Trust accredited counsellors to 720 women from 32 general practices in London and Essex between 1995 and 1998. No significant difference was found in prevalence of breastfeeding or formula introduction between control and intervention groups up to 4 months.
Peer support may offer a potentially cost-effective way of increasing breastfeeding rates but published evidence remains inconclusive.
Objective
To test if a specified programme of additional practical help by trained peer supporters affects the initiation and/or the duration of breastfeeding.
METHOD
A two-group randomised controlled trial of peer support for breastfeeding with evaluation of breastfeeding initiation and duration on an intention-to-treat basis.
Sample size calculation
From previous unpublished work, approximately 50% of women in the population start breastfeeding, of whom only about one half (that is 25–30% of the total number), continue to breastfeed until 6 weeks or beyond. The Health of the Nation8 national target is to increase the number breastfeeding at 6 weeks to 50% and, therefore, it was decided to design the trial with adequate power to detect an increase in breastfeeding from 30% to 50% at 6 weeks, if such an increase occurred.
Sample sizes were calculated using methods described by Altman.9 The trial would have had 95% power to detect (at the 5% level) a difference of 20% (that is; 30 versus 50%) at 6 weeks if 160 women were recruited to each of the peer support and control groups. Similarly, a 15% difference (30–45%) would have been be detectable with 80% power.
Setting, participants and allocation
From July 1997 to March 2002, women at 28 weeks gestation from a general practice in Ayrshire, Scotland were provided with a written description of the trial and invitation to participate. Informed consent was obtained by a research assistant or health professional. Parity, previous breastfeeding experience and intention to feed were also noted at this stage.
Allocation to control or peer support group was by post-recruitment concealed allocation, separate for each of four strata (primagravidae, previous formula feeder, previously breastfed <6 weeks, previously breastfed >6 weeks) to ensure an overall balance of previous infant feeding experience between peer support and control groups.
Allocation sequences for each stratum were generated at the start of the trial by computer in blocks of 10 (that is, five random allocations to each of the peer support and control groups in each different block of 10) to give approximate numerical balance between groups. These lists were never seen by those doing the recruiting. The allocation of each woman was done by post-recruitment telephone call to obtain the next allocation from the lists.
There was no post-allocation concealment as once a woman was allocated to the peer support or control group this was known to the peer supporters and others associated with the trial. No variation of the allocation protocol was permitted and no violations occurred. Figure 1 illustrates the participant flow.
Figure 1.
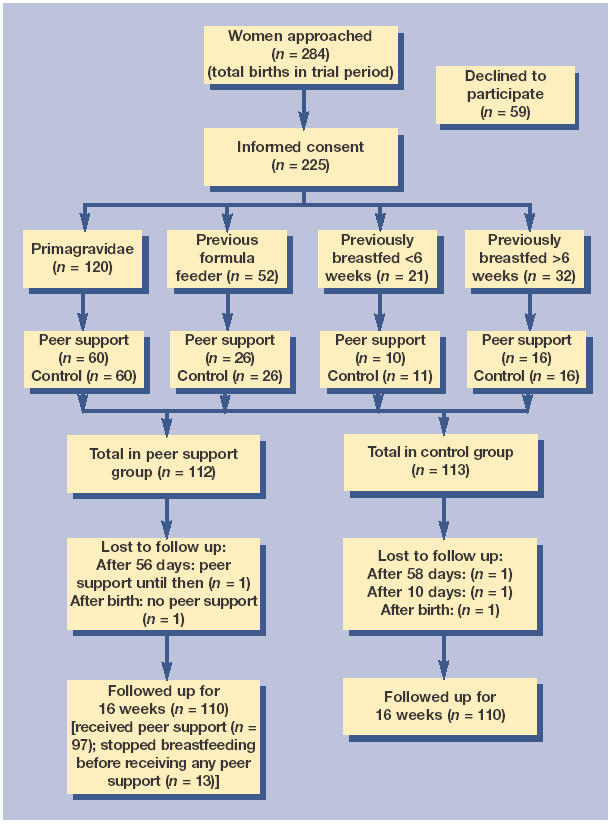
Participant flow.
Peer supporter selection, recruitment, training and supervision
Twelve peer supporters, experienced breastfeeding mothers known to the trial team, were recruited and trained. Two written references were required and security vetting was carried out in all cases.
All peer supporters completed a training programme developed and supervised by the authors, which is described in Box 1.
Box 1. Peer supporter training.
The aim of the training was to prepare peer supporters with the knowledge and skills necessary to provide appropriate support to women before and following childbirth.
The content included both specific breastfeeding information and skills and the development of other transferable skills to enhance peer support.
Breastfeeding
-
▸
Information about breastfeeding and breastmilk
-
▸
Factors to promote and inhibit breastfeeding
-
▸
Taking a feeding history
-
▸
Initiation of breastfeeding
-
▸
Practical skills — position and good attachment
-
▸
Common problems
Transferable skills
-
▸
Effective communication skills
-
▸
Listening, questioning and sharing information
-
▸
Identifying and dealing with problems
-
▸
Recognising and overcoming barriers
-
▸
Cues and prompts
Health and safety and confidentiality
-
▸
Identification
-
▸
Personal safety
-
▸
Confidentiality
Relationship with patients and professionals
-
▸
Conduct and demeanour
-
▸
Roles of the multidisciplinary team
-
▸
Referrals
The most common teaching and learning strategies used were interactive workgroups and practical sessions supported by facilitators. This enabled discussion and the opportunity to practise skills using scenarios and case studies.
Duration
Initially 2 full days and four evening sessions with regular follow-up sessions where supporters presented case studies and reflected on their input.
Peer supporter equipment and costs
Peer supporters were given an identity badge, polo-shirt and sweat-shirt bearing the trial logo. They were paid £5 per contact to cover their out-of-pocket expenses for travel, telephone costs and child care while visiting.
Intervention
Two peer supporters were assigned to each mother in the peer support group. Each pair of peer supporters was given health professional supervision by either GB or JR, who were not otherwise involved in providing breastfeeding support for mothers in the trial.
Women in both peer support and control groups received normal breastfeeding support (that is, a community midwife for the first 10 days, health visitor after 10 days, breastfeeding support groups and breastfeeding workshops). Peer support group women received peer support in addition to the normal provision.
Peer supporters visited participants at least once during the antenatal period. Further antenatal peer support was provided to women who requested it. Peer support was available to women in the intervention group if they were breastfeeding on returning home from hospital after delivery and if the peer supporters were informed in time. Peer supporters therefore had little or no contact with women in hospital, so that only hospital midwives helped mothers in both groups to initiate breastfeeding. Mothers still breastfeeding on return home from hospital would be contacted by their peer supporters at least every 2 days or as often as required either by phone or a personal visit up until day 28. If requested by the mother, the same peer supporters provided further support after 28 days until 16 weeks.
Breastfeeding problems encountered by peer support group women were solved where possible by the peer supporters directly during a visit or by telephone advice. The peer supporters were able to consult their supervising professional for additional help if required.
For the first 6 months, a monthly supervision meeting of around 3 hours duration was held with the peer supporters and trial team. From 6 months onwards, supervision continued by direct contact between the trial team and the pairs of peer supporters working with each mother. Training and feedback meetings were held approximately once per quarter until the final women had been recruited.
Data collection
Women completed questionnaires for breastfeeding stop day, formula and solid start days plus qualitative data on problems, solutions and types of support at 10 days, 8 weeks and 16 weeks. The 10-day questionnaire was completed in the presence of the health visitor. The 8-week and 16-week questionnaires were completed in the presence of a GP or practice nurse. The trial team were not involved in questionnaire completion. Questionnaire data were entered into a database by an assistant during the first 6 months and subsequently by one of the researchers. Post-entry check was carried out by another researcher prior to final analysis.
Main outcome measures
Main outcomes were the differences in breastfeeding initiation and duration between the peer support and control groups on an intention-to-treat basis with the four strata pooled.
Statistical analysis
The number and percentage of women in each group breastfeeding at birth, 10 days, 6 weeks, 8 weeks and 16 weeks, plus the difference between groups at each of these times with 95% CIs were calculated, as was the median breastfeeding duration in each group, for each of the four strata separately and combined. Comparison of overall breastfeeding duration between groups was by Kaplan–Meier plot and log-rank test. Similar secondary analyses were carried out on the separate strata and also on time to introduction of formula and/or solids.
RESULTS
Table 1 shows baseline comparison data for the control and peer support groups. Recruitment of women ended when 225 of the planned 320 women had been recruited for reasons discussed below. With the exception of the five women lost to follow-up, questionnaires were completed by all women at 10 days, 8 weeks and 16 weeks.
Table 1.
Baseline comparison of control and peer support groups by stratum.
| Control group | Peer support group | |
|---|---|---|
| (n = 113) | (n = 112) | |
| Parity | ||
| 0 | 60 | 60 |
| 1 | 25 | 37 |
| 2 | 21 | 6 |
| 3 | 3 | 3 |
| ≥4 | 3 | 6 |
| Previous breastfeeding | ||
| Primagravidae | 60 | 60 |
| <6 weeks | 11 | 10 |
| >6 weeks | 16 | 16 |
| Formula | 26 | 26 |
| Feeding intention | ||
| Breastfeed | 59 | 57 |
| Formula | 36 | 35 |
| Undecided | 18 | 20 |
| Age | ||
| Mean | 27.8 | 28.5 |
| Standard deviation | 5.5 | 5.2 |
| Range | 16–40 | 17–43 |
Of the 113 and 112 women recruited to the control and peer support groups, respectively, 60 (53%) and 61 (54%) started to breastfeed. The most common reason women gave for not breastfeeding was that they simply did not want to. Other reasons given were (control group/peer support group): difficult or premature labour or baby in special care (6 [5.3%]/7 [6.25%]); family circumstances or no family support (4 [3.5%]/6 [5.4%]); baby given bottle on hospital ward (0/1); told by midwife during labour not to breastfeed if undecided (0/1).
Of the 61 peer support group women who started to breastfeed, 13 stopped breastfeeding before receiving any peer support but were kept in the following analysis on an intention-to-treat basis.
Table 2 gives the number and percentage of women in each group breastfeeding at birth, 10 days, 6 weeks, 8 weeks and 16 weeks plus the difference between groups at each of these times with CIs. It can be seen that although more women in the peer support group are still breastfeeding at all intervals the difference between groups at any point in time is not statistically significant. The trial would not have had the statistical power for the small differences seen between the groups even if the planned 320 women had participated.
Table 2.
Numbers of women recruited to each group; numbers of women who start breastfeeding and who are still breastfeeding at each time interval until 16 weeks. Data shown for all four strata combined.
| Control group | Peer support group | |||||
|---|---|---|---|---|---|---|
| n | % | n | % | Difference (%) | 95% CI | |
| Recruited | 113 | 100 | 112 | 100 | ||
| Breastfeeding: | ||||||
| started | 60 | 53.1 | 61 | 54.5 | 1.4 | −11.7 to 14.4 |
| at 10 days | 46 | 40.7 | 46 | 41.1 | 0.4 | −12.5 to 13.2 |
| at 6 weeks | 33 | 29.2 | 35 | 31.3 | 2.0 | −10.0 to 14.0 |
| 6 weeks exclusivea | 24 | 21.2 | 27 | 24.1 | 2.9 | −8.1 to 13.8 |
| 8 weeks exclusive | 16 | 14.2 | 23 | 20.5 | 6.4 | −3.5 to 16.2 |
| 16 weeks | 20 | 17.7 | 26 | 23.2 | 5.5 | −5.0 to 16.0 |
| 16 weeks exclusive | 0 | 0.0 | 2 | 1.8 | 1.8 | −0.7 to 4.2 |
| No formulab by 16 weeks | 9 | 8.0 | 16 | 14.3 | 6.3 | −1.9 to 14.5 |
Exclusive means no other feeding apart from breastfeeding.
No formula by 16 weeks means baby breastfed, not given formula, but solids introduced by 16 weeks.
Figure 2a shows the Kaplan–Meier survival plot for all women recruited to the two groups, pooled over all strata, on an intention-to-treat basis including those who did not initiate breastfeeding. Again, although the peer support group appears higher than the control group the difference is not statistically significant by log-rank test (P = 0.5). The median breastfeeding duration among women in the peer support group was 2 days compared to 1 day for the control group.
Figure 2.
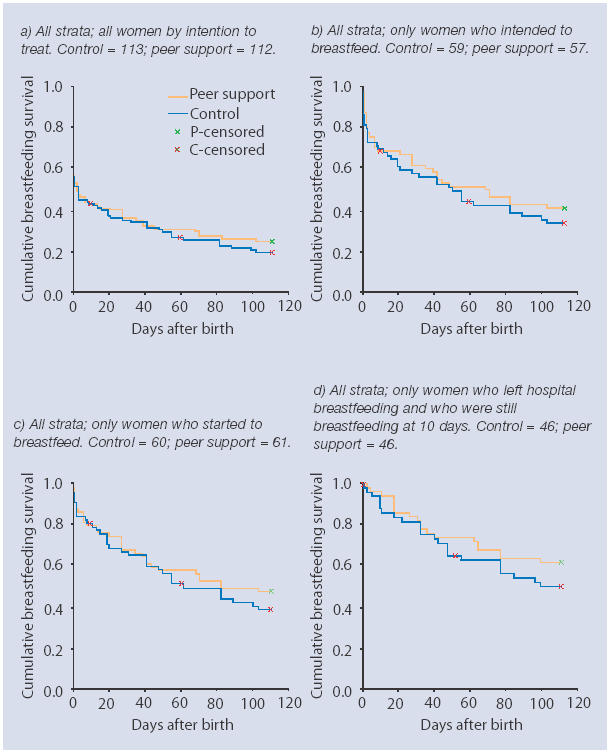
Kaplan–Meier plots of breastfeeding survival for the control and peer support groups with all strata combined. Plotted lines show the fraction of each group still giving any breastmilk up to 112 days after birth.
Figures 2b, 2c and 2d show the same comparison but only including women who intended to breastfeed (P = 0.4), those who started to breastfeed (P = 0.4).) and those who left hospital breastfeeding and were still breastfeeding at 10 days respectively (P = 0.26). Median breastfeeding durations in Figure 2b were 72 days (95% CI = 28 to 116) in the peer support group and 56 days (95% CI = 28 to 84) in the control group. In Figure 2c the medians were 72 days (95% CI = 6 to 138) in the peer support group and 56 days (95% CI = 22 to 90) in the control group. In Figure 2d more than half the peer support women were still breastfeeding at 112 days whereas in the control group the median was 102 days.
No significant differences were found between the groups in each of the four strata analysed separately by Kaplan–Meier plot and log-rank test. The median breastfeeding duration among primagravidae in the peer support group (7 days; 95% CI = 0 to 23) was greater than that for the control group (3 days; 95% CI = 0 to 13), while median breastfeeding durations in all other strata were 0 or 1 day except for those previously breastfeeding more than 6 weeks where more than half of both groups were still breastfeeding by 16 weeks. In the case of women previously breastfeeding for less than 6 weeks the median breastfeeding duration in the control group was 1 day compared to 0 days in the peer support group.
No statistically significant difference was found by Kaplan–Meier plot and log-rank test between the groups in the time to introduction of formula or solids in any of the strata separately or combined.
The median time to introduction of formula among primagravidae in the peer support group was 7 days (95% CI = 0 to 23) compared to 2 days (95% CI = 0 to 4). Among women who had previously breastfed for more than 6 weeks the median time to introduction of formula in the control group was 70 days (95% CI = 29 to 111) while in peer support group less than half the women had introduced formula by 112 days. In the case of women previously breastfeeding less than 6 weeks the Kaplan–Meier plot shows the peer support group introducing formula more quickly than the control group but the difference is not significant (P = 0.26) and the median time to formula introduction in both groups was 1 day. With all strata combined, median times for introduction of formula and solids were almost identical.
Women's questionnaire responses suggested satisfaction with peer support among women whose intention was to breastfeed, particularly among primagravidae. Some women also found the limited antenatal contact helpful in supporting their intention to breastfeed. A small number of previous formula feeders who wanted to try breastfeeding found that peer support helped them succeed. On the other hand, some women did not want peer support and of course half of the women in the population simply did not want to breastfeed. Formal analysis of questionnaire responses will be reported separately.
DISCUSSION
Summary of main findings
A specified programme of trained, supervised peer support did not significantly increase the incidence or duration of breastfeeding. Small increases in the duration of breastfeeding were observed among women who received peer support, particularly among primagravidae and women whose pre-delivery intention was to breastfeed. None of the observed differences were statistically significant by Kaplan–Meier plot and log-rank test.
Strengths and limitations of the study
There was limited antenatal contact and no contact with women while in hospital, therefore no conclusions are drawn about the effect of peer support in those circumstances.
Women in the peer support group who did not commence breastfeeding or who stopped while still in hospital received no peer support postnatally. The outcome included all such women on an intention-to-treat basis. Absence of peer support during the first few days prior to homecoming may have reduced the effect of peer support.
Peer supporters dealing with breastfeeding may have allowed health professionals more time for other women. It was neither possible nor ethical to prevent health professionals from providing more help to women in the control group and this may have affected the result. Health professionals varied in their commitment to breastfeeding and also in their acceptance of lay assistance, such as peer support, but in this trial it was not possible to evaluate any evidence of a change in the pattern of breastfeeding support provided by health professionals. There was no evidence of interaction between women in the peer support group helping mothers in the control group.
The pre-calculated sample size of 160 per group would have been adequate to detect a change in the numbers breastfeeding at 6 weeks from 30% (typically seen in the area at the time) to 50% (a UK national target for 2005). Time and resource limitations, plus a greater than expected number of women being excluded due to previous participation, resulted in only 225 women being recruited which reduced the power to 87%.
Comparison with existing literature
The findings of Morrow et al5 and Dennis et al6 showed significant improvements in breastfeeding rates resulting from peer support whereas those from Graffy et al7 and McInnes et al10 did not. The McInness et al trial was a quasi-experimental evaluation of a community-based breastfeeding promotion programme in an urban setting with intervention and control groups defined by area of residence. The setting, participants and intervention in our trial differed from those in the Graffy7 trial in key aspects. There was more extensive pre-existing availability of voluntary support (La Leche League counsellors) in the Graffy trial and indeed women who had planned to contact a counsellor were excluded on ethical grounds. In our trial there was very little availability of voluntary support and none of the women had previously asked for voluntary help. Only 720 out of 2439 women satisfied the inclusion criteria in the Graffy trial and of the 363 allocated to the intervention group only 179 tried to contact a counsellor; whereas in our trial 225 women out of 284 satisfied the criteria and consented to participate. Breastfeeding initiation in the Graffy trial was much higher (95%) than in our population (around 50%). The peer supporters in our trial were from the same community as the participants whereas Graffy et al identified cultural and social barriers as possible reasons preventing participants from contacting their counsellors. Nevertheless, despite these differences our results and conclusions are in overall agreement with those of Graffy et al.
Implications for future research
This type of peer support appeared to give a small increase in the duration of breastfeeding, particularly in first babies and among women who intended to breastfeed. The results did not show that peer support could increase breastfeeding in this population at 6 weeks from 30% to 50%. The support and cooperation of health professionals is required for peer supporters to function, and some may be unwilling to accept lay people being involved in the care of women. Not all women want peer support but similarly some women preferred peer support. Further research is required to examine the effectiveness of comprehensive breastfeeding encouragement and support strategies covering antenatal, hospital and postnatal settings.
Acknowledgments
The authors thank Harper Gilmour of the Section for Public Health and Health Policy, Division of Community Based Sciences, University of Glasgow, for his advice and assistance on statistics, design, sample size calculations and comment on the draft paper. The authors also thank colleagues for helpful discussion and comment, health professionals, the 12 peer supporters and all of the mothers who participated in the trial.
Funding body
The trial was funded by departments of Ayrshire and Arran Health Board which took no further part in the trial. Oxenward Surgery was part of the Chief Scientist Office Research Practice Programme during 2000 to 2003 (CZP/1/13)
Ethics committee
Ethical approval for the trial was obtained from Ayrshire & Arran Health Board ethical committee in May 1996 (Ayrshire & Arran Research Ethics Committee 2021)
Competing interests
The authors are of the opinion that breastfeeding is best for babies in most circumstances but otherwise all authors declare that they have no competing interests
REFERENCES
- 1.Fairbank L, O'Meara S, Renfrew MJ, et al. A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding. Health Technol Assess. 2000;4:25. [PubMed] [Google Scholar]
- 2.Sikorski J, Renfrew MJ, Pindoria S, Wade A. Cochrane Library. Issue 1. Oxford: Update Software; 2002. Support for breastfeeding mothers. In: Cochrane Review. [DOI] [PubMed] [Google Scholar]
- 3.Protheroe L, Dyson L, Renfrew MJ, et al. The effectiveness of public health interventions to promote the initiation of breastfeeding. Evidence briefing. London: Health Development Agency; 2003. [Google Scholar]
- 4.Guise J-M, Palda V, Westhoff C, et al. The effectiveness of primary care-based interventions to promote breastfeeding: systematic evidence review and meta-analysis for the US Preventive Services Task Force. Ann Fam Med. 2003;1:70–78. doi: 10.1370/afm.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrow AL, Guerrero ML, Shults J, et al. Efficacy of home-based peer counselling to promote exclusive breastfeeding: a randomised controlled trial. Lancet. 1999;353:1226–31. doi: 10.1016/S0140-6736(98)08037-4. [DOI] [PubMed] [Google Scholar]
- 6.Dennis CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast-feeding duration among primiparous women: a randomised controlled trial. CMAJ. 2002;166(1):21–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ. 2004;328:26–29. doi: 10.1136/bmj.328.7430.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Management Executive. Local breastfeeding targets. Edinburgh: Scottish Office; 1994. p. 1. (MEL (1994) 110) [Google Scholar]
- 9.Altman DG. Practical statistics for medical research. London: Chapman and Hall; 1996. [Google Scholar]
- 10.McInnes R, Love J, Stone D. Evaluation of a community-based intervention to increase breastfeeding prevalence. J Pub Health Med. 2000;22(2):138–145. doi: 10.1093/pubmed/22.2.138. [DOI] [PubMed] [Google Scholar]


