Abstract
The survival of Brucella suis mutant strains in mice demonstrated different roles of the two high-oxygen-affinity terminal oxidases. The cbb3-type cytochrome c oxidase was essential for chronic infection in oxygen-deficient organs. Lack of the cytochrome bd ubiquinol oxidase led to hypervirulence of bacteria, which could rely on nitrite accumulation inhibiting the inducible nitric oxide synthase of the host.
Brucellosis is an ancient zoonosis that remains endemic in many South American and Mediterranean countries but is also spreading in near-eastern and central Asia (20). The infectious agents of this disease are the gram-negative intracellular bacteria of the genus Brucella, among which B. abortus, B. suis, and B. melitensis are the species most frequently associated with pathogenicity in humans. Acute brucellosis in humans is characterized by undulant fever and other less well defined clinical symptoms. In the absence of treatment, infection can spontaneously recede or result in chronicity, which sometimes causes mortality (5% of cases). The pathogenicity and chronicity of brucellae result from their ability to infect macrophages, which spread bacteria throughout the organism to specific organs. Brucella can evade the killing mechanisms within macrophages and of the host immune system by several means (8, 10, 12), allowing the pathogen to induce focal infections. Chronic infection can affect various organs including the liver, spleen, or brain of patients, where the bacteria reside inside granulomatous structures generated by the immune system (1, 5, 23). Granulomas are structures with multiple types of cells where microaerobic and anaerobic areas coexist (24) and which possibly evolve into oxygen-deprived abscesses (1, 5) at the late stage of the disease.
The expression of genes involved in adaptation to oxygen deficiency has appeared essential for long-term survival of Brucella inside the host. In a previous study, we showed that the two high-oxygen-affinity terminal oxidases of B. suis differently participated in adaptation to low-oxygen tension (18). The cbb3-type cytochrome c oxidase was specifically expressed in culture with maximal activation under microaerobiosis, whereas the cytochrome bd ubiquinol oxidase was preferentially expressed inside macrophages and involved in intracellular bacterial multiplication. These results indicated that Brucella needs a terminal oxidase with high affinity for oxygen for optimal survival inside the phagosomal compartment of the macrophage (18). In fact, the oxygen concentration inside phagosomes of stimulated macrophages is lower than that measured in the extracellular environment (11). Moreover, Brucella generates a specific replicative niche which was proposed to be oxygen limited (16).
Here, we investigated the need for a functional high-oxygen-affinity terminal oxidase to allow B. suis to establish and maintain chronic infection in a murine model of in vivo infection. Direct measurements in mice showed that oxygen pressure was highly variable depending on the tissue examined (3).
The cbb3-type cytochrome c oxidase but not the bd ubiquinol oxidase is required for persistence of B. suis in mice.
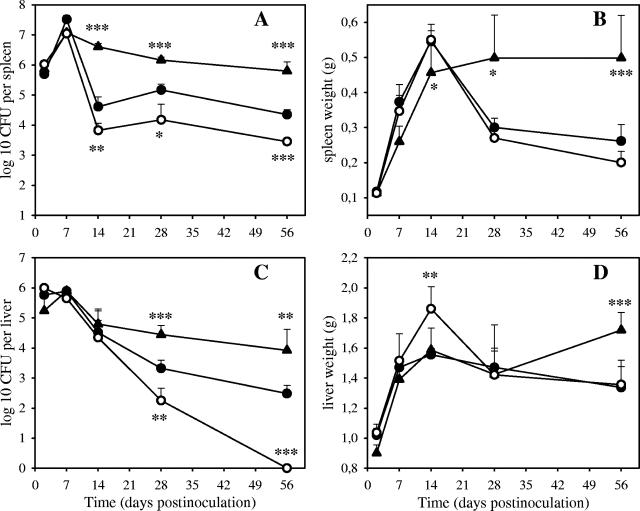
In order to evaluate a possible role of the cbb3-type and bd oxidases in virulence of B. suis, we examined the effect of mutations within the ccoNOQP and cydDCAB operons, respectively, on bacterial survival in mice. Wild-type B. suis 1330 and mutants harboring a deleted ccoN or cydB gene (18) were used to infect 7-week-old female BALB/c mice intraperitoneally at a dose of 105 CFU. At different time points, bacteria were recovered from the spleens and livers of five mice for each of the three strains. Organs were homogenized in phosphate-buffered saline, and bacterial numbers were determined by plating serial dilutions on tryptic soy (TS) agar. Gene amplifications from chromosomal DNAs of the wild-type and mutant strains were performed to verify their genotypes. Single PCR products whose sizes corresponded to deletion and replacement by the kanamycin or chloramphenicol resistance cassette in the mutants (18) were identical to those obtained before infection of mice. After an identical initial multiplication phase (Fig. 1A), the three strains showed different behaviors within the spleen. During the second week of infection, the ΔccoN mutant showed a stronger reduction of CFU numbers than the wild-type strain did (P < 0.01). This significant attenuation was observed over the phase of persistence, lasting until day 56, as shown by bacterial counts approximately 1 log lower than that of the parental strain (P < 0.001) (Fig. 1A). The ΔcydB mutant did not exhibit the strong decrease of the wild-type strain between the first and second weeks of infection (Fig. 1A) but showed only a slight reduction in bacterial numbers instead. CFU counts higher than that of the wild-type strain between days 14 and 56 (P < 0.001) showed a persistent colonization of the spleens by the ΔcydB mutant.
FIG. 1.
Infection of BALB/c mice with B. suis wild-type strain (•) and the ccoN (○) and cydB mutants (▴). Bacteria were recovered from spleens (A) and livers (C) of five mice per strain at 2, 7, 14, 28, and 56 days postinoculation. Counts on day 56 from livers of mice infected with the ccoN mutant were obtained from plating whole organs. Corresponding spleen and liver weights are represented in panels B and D, respectively. Error bars represent the standard deviations of the means. Analysis of variance using the Fisher protected least significant difference test and the Tukey-Kramer test was performed to determine the level of significance (P) of differences in CFU between the wild type and each of the mutants. Results of statistical analysis are indicated by asterisks (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
The weights of spleens were similar for infections of mice with the wild-type strain and with the ΔccoN mutant (Fig. 1B). This can be explained by the attenuation level of this mutant (see above), which could be insufficient to have an impact on the splenomegaly induced by B. suis. The ΔcydB mutant provoked a significantly lower increase of the weight of spleens until day 14 (P < 0.05). But, unlike the wild-type strain, the increase of spleen weight was prolonged between days 14 and 28 and remained at this level (P < 0.001) (Fig. 1B). This was in accordance with the persistence of infection with the ΔcydB strain in mice. The absence of elimination of this mutant probably triggered permanent recruitment of cells of the immune system, which reflected the inflammatory response of the host to infection.
This finding was in contrast with the attenuation of the cydB mutant of B. abortus (7). Experimental infections and determination of viable bacteria in spleens were repeated, giving reproducible results. The higher virulence of the cytochrome bd oxidase-deficient B. suis strain could be linked to its species-specific interaction with the immune response of the host. The cydB mutants of the two species also displayed greatly different phenotypes in vitro. In fact, under microaerobiosis, which allows low expression of the cytochrome bd oxidase, whereas aerobiosis does not (18), the cydB mutant of B. suis did not exhibit the increased sensitivity to the respiratory inhibitors (not shown) described for the cydB mutant of B. abortus (7). Moreover, a cydBA mutant of B. melitensis was also reported to be as virulent as the wild-type B. melitensis 16 M in the caprine model of brucellosis (13).
Within livers, despite lower multiplication, the overall survival curves of the three strains (Fig. 1C) displayed patterns similar to those observed in the spleens. From the second week of infection on, the ΔcydB mutant was also found to be more virulent than the parental strain because its elimination rate was highly reduced (Fig. 1C), with only a fivefold decrease in the bacterial counts, instead of the 102-fold decrease observed for the wild type (P < 0.01). Interestingly, the absence of native ccoN severely impaired the virulence of B. suis, since the ΔccoN strain showed a continuous decline in CFU numbers until total elimination at day 56 (Fig. 1C).
The weight of livers (Fig. 1D) infected by the ΔccoN strain was significantly elevated in comparison to that of livers infected by the wild-type bacteria at 2 weeks postinfection (P < 0.01). This was indicative of a stronger inflammatory response corresponding to the higher elimination rate of this mutant during the following weeks. Similarly to the situation described in spleens, the higher persistence of the ΔcydB mutant was accompanied by an increase in weight on day 56 (P < 0.001).
The cbb3-type cytochrome c oxidase is induced inside macrophages maintained under microaerobiosis.
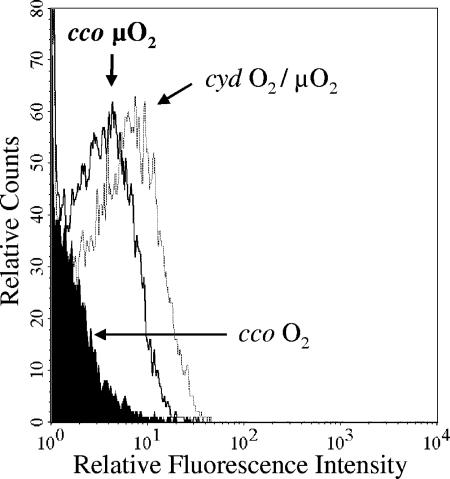
The results described above were surprising given that our previous data showed that the multiplication of the ΔccoN strain was not affected inside human THP-1 (18) or murine J774A.1 macrophage-like cells (not shown). Since no significant attenuation of the ΔccoN mutant was correlated with the absence of expression of the cbb3-type cytochrome c oxidase in the intracellular state (18), we decided to investigate the expression of the ccoNOQP promoter inside macrophages under various oxygenation conditions. As previously described (18), the activity of the cco promoter-gfp fusion was analyzed in B. suis multiplying within THP-1 cells under either aerobiosis or microaerobiosis. In the latter case, following phagocytosis, infected cells were placed in a jar containing GENbox generators (bioMérieux, Marcy l'Etoile, France) of microaerobic atmosphere (oxygen concentration ranging from 6.2 to 13.2% after 1 h). At 48 h postinfection, bacteria released after lysis of infected cells were prepared for flow cytometry analysis (18). Measurement of fluorescence intensity revealed that the ccoNOQP promoter was induced when THP-1 cells were maintained under microaerobiosis compared to the absence of fluorescence observed under aerobic conditions (Fig. 2). The expression level of the cydDCAB promoter (18) was found to be almost unchanged by lowering the level of oxygen available to the infected cells. Expression of the cco operon inside macrophages under microaerobiosis indicated that current models of in vitro cellular infection do not mimic in vivo conditions, such as the oxygen concentration (2), in particular at the site of infections. This was in line with the fact that the ΔccoN mutant was much more attenuated in the liver (Fig. 1C), where the oxygen level is lower than in the spleen (3).
FIG. 2.
Intramacrophagic expression of terminal cytochrome oxidases. The figure shows flow cytometry analysis of expression of the cyd and cco promoter-gfp fusions, inside macrophages maintained under aerobic (O2) or microaerobic (μO2) conditions during infection. Under the two conditions, fluorescence values produced by the cyd-gfp fusion were almost identical. The control curve corresponding to intracellular bacteria containing promoterless plasmid pBBR1-CGFP (18) was identical to that of pcco-CGFP under aerobiosis (black curve) and is omitted for clarity.
Lack of the cytochrome bd ubiquinol oxidase impairs nitrite utilization by B. suis under microaerobiosis.
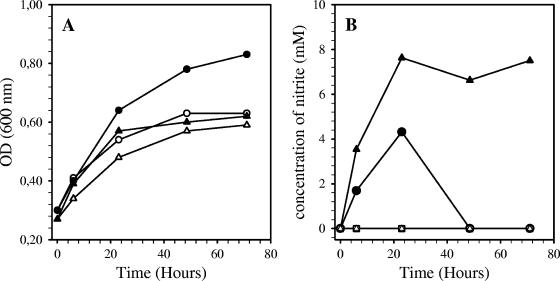
The cytochrome cbb3-type and cytochrome bd oxidases showed very different phenotypes of expression in a cellular model of infection and of persistence of the respective mutants in vivo, in response to low oxygen concentrations. The behavior of the ccoN and cydB mutant strains was therefore checked during cultures under microaerobiosis in the presence of nitrate as an alternative electron acceptor. In fact, we previously showed (17) that B. suis can use reduction of nitrogen oxides to survive under anaerobiosis. Under a microaerobic atmosphere generated as described above, all the strains grew in TS broth. The wild-type strain showed a higher growth rate in the presence than in the absence of 10 mM NaNO3 (Fig. 3A), identical to that of the ΔccoN mutant (not shown). In contrast, the growth of the ΔcydB mutant was not improved by the presence of nitrate in the medium (Fig. 3A). Moreover, production and utilization of nitrite by the bacteria were assessed by measuring the concentration of NO2 in the culture supernatant, using the Griess reagent (9). Nitrite production by the wild-type strain (Fig. 3B) resulted from activity of the bacterial nitrate reductase (Nar), since nitrite was undetectable in the culture medium of the narG strain (17). After the peak at 24 h, the nitrite concentration strongly decreased, below the limit of detection at 48 h, probably because nitrogen oxides were totally reduced by the denitrification pathway (17). Similar results were obtained with the ΔccoN mutant (not shown). Unlike the wild type, the cydB strain accumulated nitrites, which reached a concentration of around 8 mM at 72 h (Fig. 3B). This result was unexpected and suggested that aerobic respiration and denitrification were coordinated. On the basis of knowledge concerning bacteria of the genus Rhodobacter, we can postulate that the cytochrome bd oxidase of B. suis might play a role in redox signal transmitting to the two-component system RegB/RegA (6), which could control nitrite reductase activity. The latter point was suggested by our preliminary results (not shown).
FIG. 3.
Growth of B. suis strains and nitrite accumulation under microaerobic conditions. Each strain was previously grown under aerobiosis until an optical density of approximately 0.25 was reached. Wild-type (•) and cydB (▴) mutant bacteria were then cultivated in TS medium supplemented or not (corresponding open symbols) with 10 mM NaNO3, in a jar containing GENbox generators of microaerobic atmosphere. At various time points, an aliquot was collected to measure the optical density at 600 nm (A) and centrifuged to measure nitrite concentration in the supernatant (B). The narG (▪) strain was used as a negative control of nitrite production.
Conclusion.
The ΔccoN and ΔcydB B. suis mutants had opposite fates in a mouse model of infection, characterized by the higher elimination of the first one in contrast to the hypervirulence of the latter. These findings corroborated the differential use of the two high-oxygen-affinity terminal oxidases of B. suis that we previously observed in vitro (18). Intracellular expression showed that the cytochrome cbb3-type oxidase, but not the cytochrome bd oxidase, adapted its expression when the environmental oxygen tension of the infected macrophages became low, consistent with the fact that only the cytochrome cbb3-type oxidase was strongly induced in cultures under microaerobiosis (18). In agreement, the increased elimination of the ΔccoN strain in liver can be correlated with the very low oxygen concentration of the liver in comparison to that of the spleen (3). This study demonstrated that functional cbb3-type cytochrome c oxidase was necessary for the persistence of B. suis in mouse organs, probably because this terminal oxidase played a role in adaptation to the reduced oxygen availability inside the host.
In contrast, the persistence of the B. suis strain lacking the cytochrome bd oxidase during the chronic phase of infection suggested an effect of the cydB deletion on the immune system of the mice. This could not be detected using a cellular model of infection (18). Given that nitrate is present in mammalian tissues (14, 19), we speculated about a link between the higher survival of the ΔcydB strain in mouse organs and the slow nitrite accumulation by this mutant during microaerobic growth. Nitrite acidification leads to nonenzymatic nitric oxide (NO) production, which can greatly increase (19, 25) under acidic conditions such as those encountered in the phagosome specific to B. suis (21) and under hypoxia, which is more drastic in vivo than in cell cultures (2). Furthermore, under particular conditions of kinetics and concentrations, release of NO can inhibit expression of inducible NO synthase (4, 22), whose activity is a major component of the innate immune response against Brucella infection in mice (9, 15). We tentatively assume that impairment of nitrite consumption by the ΔcydB strain might improve its persistence in vivo, by this means.
Whatever the underlying mechanisms are, we can conclude that the two high-oxygen-affinity terminal oxidases of B. suis play different roles with divergent impacts on virulence in vivo.
Acknowledgments
S. Loisel-Meyer was supported by fellowships from the Institut National de la Santé et de la Recherche Médicale and the Conseil Régional of Languedoc-Roussillon. M. P. Jiménez de Bagüés was the recipient of a grant of the Communauté de Travail des Pyrénées (CTP) Region Aragón (Spain) (CTP M01/2002).
Editor: D. L. Burns
Footnotes
Published ahead of print on 13 November 2006.
REFERENCES
- 1.Ariza, J., C. Pigrau, C. Canas, A. Marron, F. Martinez, B. Almirante, J. M. Corredoira, A. Casanova, J. Fabregat, and A. Pahissa. 2001. Current understanding and management of chronic hepatosplenic suppurative brucellosis. Clin. Infect. Dis. 32:1024-1033. [DOI] [PubMed] [Google Scholar]
- 2.Atkuri, K. R., and L. A. Herzenberg. 2005. Culturing at atmospheric oxygen levels impacts lymphocyte function. Proc. Natl. Acad. Sci. USA 102:3756-3759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balazuc, A. M., M. Lagranderie, P. Chavarot, P. Pescher, E. Roseeuw, E. Schacht, D. Domurado, and G. Marchal. 2005. In vivo efficiency of targeted norfloxacin against persistent, isoniazid-insensitive, Mycobacterium bovis BCG present in the physiologically hypoxic mouse liver. Microbes Infect 7:969-975. [DOI] [PubMed] [Google Scholar]
- 4.Colasanti, M., and H. Suzuki. 2000. The dual personality of NO. Trends Pharmacol. Sci. 21:249-252. [DOI] [PubMed] [Google Scholar]
- 5.Colmenero Jde, D., M. I. Queipo-Ortuno, J. Maria Reguera, M. Angel Suarez-Munoz, S. Martin-Carballino, and P. Morata. 2002. Chronic hepatosplenic abscesses in brucellosis. Clinico-therapeutic features and molecular diagnostic approach. Diagn. Microbiol. Infect. Dis. 42:159-167. [DOI] [PubMed] [Google Scholar]
- 6.Elsen, S., L. R. Swem, D. L. Swem, and C. E. Bauer. 2004. RegB/RegA, a highly conserved redox-responding global two-component regulatory system. Microbiol. Mol. Biol. Rev. 68:263-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Endley, S., D. McMurray, and T. A. Ficht. 2001. Interruption of the cydB locus in Brucella abortus attenuates intracellular survival and virulence in the mouse model of infection. J. Bacteriol. 183:2454-2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gross, A., M. Bouaboula, P. Casellas, J. P. Liautard, and J. Dornand. 2003. Subversion and utilization of the host cell cyclic adenosine 5′-monophosphate/protein kinase A pathway by Brucella during macrophage infection. J. Immunol. 170:5607-5614. [DOI] [PubMed] [Google Scholar]
- 9.Gross, A., S. Spiesser, A. Terraza, B. Rouot, E. Caron, and J. Dornand. 1998. Expression and bactericidal activity of nitric oxide synthase in Brucella suis-infected murine macrophages. Infect. Immun. 66:1309-1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gross, A., A. Terraza, S. Ouahrani-Bettache, J. P. Liautard, and J. Dornand. 2000. In vitro Brucella suis infection prevents the programmed cell death of human monocytic cells. Infect. Immun. 68:342-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James, P. E., O. Y. Grinberg, G. Michaels, and H. M. Swartz. 1995. Intraphagosomal oxygen in stimulated macrophages. J. Cell Physiol. 163:241-247. [DOI] [PubMed] [Google Scholar]
- 12.Jubier-Maurin, V., R. A. Boigegrain, A. Cloeckaert, A. Gross, M. T. Alvarez-Martinez, A. Terraza, J. Liautard, S. Köhler, B. Rouot, J. Dornand, and J. P. Liautard. 2001. Major outer membrane protein Omp25 of Brucella suis is involved in inhibition of tumor necrosis factor alpha production during infection of human macrophages. Infect. Immun. 69:4823-4830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kahl-McDonagh, M. M., P. H. Elzer, S. D. Hagius, J. V. Walker, Q. L. Perry, C. M. Seabury, A. B. den Hartigh, R. M. Tsolis, L. G. Adams, D. S. Davis, and T. A. Ficht. 2006. Evaluation of novel Brucella melitensis unmarked deletion mutants for safety and efficacy in the goat model of brucellosis. Vaccine 24:5169-5177. [DOI] [PubMed] [Google Scholar]
- 14.Kelm, M. 1999. Nitric oxide metabolism and breakdown. Biochim. Biophys. Acta 1411:273-289. [DOI] [PubMed] [Google Scholar]
- 15.Ko, J., A. Gendron-Fitzpatrick, and G. A. Splitter. 2002. Susceptibility of IFN regulatory factor-1 and IFN consensus sequence binding protein-deficient mice to brucellosis. J. Immunol. 168:2433-2440. [DOI] [PubMed] [Google Scholar]
- 16.Köhler, S., S. Michaux-Charachon, F. Porte, M. Ramuz, and J. P. Liautard. 2003. What is the nature of the replicative niche of a stealthy bug named Brucella? Trends Microbiol. 11:215-219. [DOI] [PubMed] [Google Scholar]
- 17.Loisel-Meyer, S., M. P. Jiménez de Bagüés, E. Basseres, J. Dornand, S. Köhler, J. P. Liautard, and V. Jubier-Maurin. 2006. Requirement of norD for Brucella suis virulence in a murine model of in vitro and in vivo infection. Infect. Immun. 74:1973-1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loisel-Meyer, S., M. P. Jiménez de Bagüés, S. Köhler, J. P. Liautard, and V. Jubier-Maurin. 2005. Differential use of the two high-oxygen-affinity terminal oxidases of Brucella suis for in vitro and intramacrophagic multiplication. Infect. Immun. 73:7768-7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lundberg, J. O., E. Weitzberg, J. A. Cole, and N. Benjamin. 2004. Nitrate, bacteria and human health. Nat. Rev. Microbiol. 2:593-602. [DOI] [PubMed] [Google Scholar]
- 20.Pappas, G., P. Papadimitriou, N. Akritidis, L. Christou, and E. V. Tsianos. 2006. The new global map of human brucellosis. Lancet Infect. Dis. 6:91-99. [DOI] [PubMed] [Google Scholar]
- 21.Porte, F., J. P. Liautard, and S. Köhler. 1999. Early acidification of phagosomes containing Brucella suis is essential for intracellular survival in murine macrophages. Infect. Immun. 67:4041-4047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ronchetti, D., F. Impagnatiello, M. Guzzetta, L. Gasparini, M. Borgatti, R. Gambari, and E. Ongini. 2006. Modulation of iNOS expression by a nitric oxide-releasing derivative of the natural antioxidant ferulic acid in activated RAW 264.7 macrophages. Eur. J. Pharmacol. 532:162-169. [DOI] [PubMed] [Google Scholar]
- 23.Sohn, A. H., W. S. Probert, C. A. Glaser, N. Gupta, A. W. Bollen, J. D. Wong, E. M. Grace, and W. C. McDonald. 2003. Human neurobrucellosis with intracerebral granuloma caused by a marine mammal Brucella spp. Emerg. Infect. Dis. 9:485-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wayne, L. G., and C. D. Sohaskey. 2001. Nonreplicating persistence of Mycobacterium tuberculosis. Annu. Rev. Microbiol. 55:139-163. [DOI] [PubMed] [Google Scholar]
- 25.Zweier, J. L., A. Samouilov, and P. Kuppusamy. 1999. Non-enzymatic nitric oxide synthesis in biological systems. Biochim. Biophys. Acta 1411:250-262. [DOI] [PubMed] [Google Scholar]