Abstract
Helicobacter pylori strains with reduced susceptibility to fluoroquinolones have a mutation at either codon 87 Asn or 91 Asp of the gyrA gene. A rapid test based on an allele-specific PCR (AS-PCR) was designed to detect the gyrA mutations. Clinical H. pylori isolates were obtained from the stomachs of 51 patients with H. pylori infections who showed treatment failure. The MICs of gatifloxacin (GAT) were determined by the agar dilution method. Identical genotyping results were obtained with AS-PCR and conventional PCR. The gyrA mutations of H. pylori causing reduced susceptibility to fluoroquinolones could be detected successfully by this method. A significant association was observed between the presence of mutations, as detected by AS-PCR, and the resistance of the strains to GAT. Moreover, genotyping by AS-PCR took less than 3 to 4 h. The AS-PCR method for the detection of gyrA mutations in H. pylori is useful for easy identification of fluoroquinolone-resistant strains of H. pylori.
Failure of proton pump inhibitor-based triple therapies for the eradication of Helicobacter pylori infection has been shown to frequently be due to resistance to either clarithromycin or metronidazole. Furthermore, concomitant resistance to both drugs is not rare either, particularly in cases showing failure of first-line therapy (4). Alternative regimens need to be developed for such cases showing concomitant resistance to both drugs.
Recently, Sharara et al. reported a 7-day regimen of gatifloxacin (8-methoxy fluoroquinolone [GAT]), amoxicillin, and rabeprazole as an effective and safe secondary eradication treatment regimen for H. pylori, with an eradication rate of 84.4% (20). Therefore, GAT-based triple therapy might be a promising alternative treatment option for H. pylori infection. However, we recently reported a high resistance rate (47.9%) to GAT of Helicobacter pylori strains isolated from Japanese patients after unsuccessful eradication therapy (17).
The resistance of H. pylori to fluoroquinolones, which exert their antimicrobial action by affecting the A subunit of the DNA gyrase of H. pylori, has been reported to be caused by point mutations in the so-called quinolone resistance-determining region of the gyrA gene of H. pylori (9, 12, 17, 19, 22, 23), mainly at amino acid 87 (Asn to Lys) or 91 (Asp to Gly, Asp to Asn, or Asp to Tyr) (17, 22). H. pylori does not possess a gene encoding topoisomerase IV, an important fluoroquinolone target in other bacteria. Therefore, bacterial resistance to fluoroquinolone can be tested by a genetic test of gyrA. Development of an inexpensive and reliable high-throughput method for the detection of gyrA mutations is expected to be highly useful for H. pylori eradication therapy with regimens containing fluoroquinolones.
Allele-specific PCR (AS-PCR) is one of the techniques used to determine point mutations in genomic samples, with a high degree of specificity and sensitivity. Point mutations can be identified easily within a short period of time by PCR amplification alone, without direct sequencing or digestion with restriction enzymes. In the AS-PCR analysis, PCR amplification is performed using a specific primer in which the second nucleotide from the 3′ end is designed to match the site of the point mutation and the third nucleotide is designed to produce a mismatch in order to yield allele-specific PCR amplification (8). The point mutations can be identified by determining whether or not the PCR amplicons corresponding to the specific primers can be observed.
The aim of this study was to develop a rapid genotyping method based on AS-PCR for detecting gyrA mutations in H. pylori.
MATERIALS AND METHODS
Patients and isolation of H. pylori.
A total of 51 patients (33 males and 18 females; age, 56.7 ± 12.7 years [mean ± standard deviation]) with H. pylori infection who showed treatment failure were enrolled in this study. Of the total, 43 patients had one treatment failure, 6 patients had two treatment failures, and 2 patients had three treatment failures. (The first-line treatment used was triple therapy with clarithromycin, amoxicillin [AMX], and a proton pump inhibitor [PPI] for 7 days; the second-line treatment used was triple therapy with metronidazole, AMX, and PPI for 7 days; and the third-line treatment used was triple therapy with levofloxacin, AMX, and PPI.) Informed consent was obtained from all patients prior to their participation in the study. All patients underwent upper-gastrointestinal endoscopy; biopsy specimens obtained from the greater curvature of the upper corpus were then used to isolate H. pylori. The clinical isolates of H. pylori used in the present study were previously examined and reported only in terms of gyrA mutation and the MIC for GAT (17). In addition to 48 previous isolates (17), isolates with known GAT MICs were examined for gyrA mutation (KS0203, KS0205, KS0193, and KS0195). However, KS0166 (GAT MIC, 0.5 μg/ml) was excluded from the present study because sequencing of the gyrA gene revealed that it was a mixed strain of mainly the wild type and a trivial amount of a mutant (A272G).
Microaerobic bacterial culture and determination of MICs.
Primary culture was performed using Columbia HP agar (Becton Dickinson, Cockeysville, MD) under a 10% CO2 and 5% O2 atmosphere at 35°C for 4 to 7 days. The colonies were harvested and subcultured on sheep blood agar (Becton Dickinson) under a 10% CO2 and 5% O2 atmosphere at 35°C for 3 days (11).
The susceptibility of the H. pylori isolates to GAT (Kyorin Pharmaceutical Co., Ltd., Tokyo, Japan) was determined by the agar dilution method according to the guidelines established by the CLSI (formerly NCCLS) (13). A saline suspension equivalent to a 2.0 McFarland standard (containing 1 × 107 to 1 × 108 CFU/ml) was prepared from a 72-hour subculture from a blood agar plate. The inoculum (1 to 3 μl per spot) was plated directly on the antimicrobial agent-containing agar dilution plates. All of the plates were incubated in a 10% CO2 and 5% O2 atmosphere at 35°C for 3 days. The MIC was defined as the lowest concentration of antibiotic that completely inhibited the growth of the inoculum. Isolates were considered resistant to GAT if the MIC of the drug was ≥1 μg/ml (2, 11, 14, 17).
DNA preparation and PCR assay.
Total DNAs were extracted from H. pylori isolates by using a QIAamp DNA mini kit (QIAGEN GmbH, Hilden, Germany). Primers complementary to regions flanking the 428-bp coding sequence of the quinolone resistance-determining region of gyrA (codons 38 to 154) were used. The PCR mixture (50-μl final volume) contained HotStar Taq master mix (QIAGEN) and 0.5 μM (each) primer gyrA.f (5′-TTTRGCTTATTCMATGAGCGT [forward]) and primer gyrA.r (5′-GCAGACGGCTTGGTARAATA [reverse]) for the gyrA gene. PCR was performed in a Gene Amp PCR system 9700 instrument (Applied Biosystems, Foster City, CA) under the following amplification conditions: initial denaturation at 95°C for 15 min, followed by 40 cycles of denaturation at 94°C for 30 s, annealing at 55°C for 30 s, and extension at 72°C for 1 min, with a final extension at 72°C for 10 min. The products of amplification were purified using a QIAquick PCR purification kit (QIAGEN).
Sequencing.
Amplicons of gyrA were sequenced using gyrA.f and gyrA.r and an ABI Big Dye Terminator cycle sequencing ready reaction kit (PE Applied Biosystems, Norwalk, CT). The sequenced PCR products were analyzed in an ABI Prism 3700 genetic analyzer (Applied Biosystems). The sequences obtained were determined using Sequencher (Lasergene, DNAStar, Madison, WI) and were compared with the published sequence of the H. pylori gyrA gene (GenBank accession no. L29481) (2).
Allele-specific PCR with mismatch primers.
Analysis of alleles with point mutations in gyrA (C261A, C261G, G271A, G271T, and A272G) was performed with standard thin-walled PCR tubes, using KOD-Plus DNA polymerase (Toyobo, Osaka, Japan), on a Gene Amp PCR system 9700 instrument. Details concerning the design of the allele-specific primers used in this study are given in Table 1. The following mixture was prepared for the AS-PCR: 7.9 μl of distilled water, 2.5 μl of 10× reaction buffer, 2.5 μl of deoxynucleoside triphosphates (2 mM [each]), 0.5 μl of KOD-Plus DNA polymerase, 1 μl of 25 mM MgSO4, 9.6 μl of primer mixture (10 pmol of gyrA primer R, 5 pmol of primer F261A1, 2.5 pmol of primer F261G1, 5 pmol of primer F271A5, 16 pmol of primer F271A9, 5.5 pmol of primer F271T9, 1.25 pmol of primer F272G1, and 1 pmol of primer F272G9), and 1 μl of genomic DNA. The amplification was conducted under the following conditions: an initial denaturing step at 95°C for 5 min, followed by 35 cycles at 95°C for 15 s, 62.5°C for 30 s, and 68°C for 30 s, with a final elongation step at 68°C for 2 min. The PCR products were analyzed by electrophoresis on 2% agarose gels, followed by ethidium bromide staining and inspection under UV light.
TABLE 1.
Oligonucleotide sequences of primers used in AS-PCR method to determine gyrA mutation of H. pylori at positions 261, 271, and 272
| Primer direction | Mutation | Primer name | Primer sequencea | PCR product size (bp) |
|---|---|---|---|---|
| Forward | C261A | F261A1 | CCCCCATGGCGAGAAaG | 262 |
| C261G | F261G1 | CCCCCATGGCGAGAAgG | 262 | |
| G271A | F271A5 | GCGATAACGCGGTTTAGaA | 254 | |
| F271A9 | GCGATAATGCGGTTTAGaA | 254 | ||
| G271T | F271T9 | GGCGATAATGCGGTTAATtA | 255 | |
| A272G | F272G1 | GCGATAACGCGGTTTAGGgT | 254 | |
| F272G9 | GCGATAATGCGGTTTAGGgT | 254 | ||
| Reverse | gyrA R | GTTAGGCAGACGGCTTGGTARAATA |
The penultimate nucleotide to distinguish between wild-type and mutant sequences is shown in lowercase. The 1-bp mismatch at another nucleotide is underlined.
Statistical analysis.
Fisher's exact test was used to test the association between the presence of mutations in the genotype, as determined by AS-PCR, and resistance of the strains to GAT. P values of <0.05 were considered to denote statistical significance.
RESULTS
Point mutations in the gyrA gene at codon 87 Asn or 91 Asp were detected in 24 of the 25 (96%) GAT-resistant strains isolated in this study. On the other hand, only 1 of the 26 (3.8%) susceptible strains had the mutation, with a substitution at amino acid 87. At base triplet 87, we found two wild-type variants, namely, an AAC triplet and an AAT triplet (C261T mutation, both coding for Asn).
Of all the strains, 26 were wild-type H. pylori strains (AAC triplet, 17 isolates; AAT triplet [C261T], 9 isolates), 8 strains had the C261A mutation (Asn 87 Lys), 3 strains had the C261G mutation (Asn 87 Lys), 9 strains had the C271A mutation (Asp 91 Asn), 2 strains had the C271T mutation (Asp 91 Tyr), and 3 strains had the A272G mutation (Asp 91 Gly). We did not see any significant association between the type of gyrA mutation and the MIC of GAT.
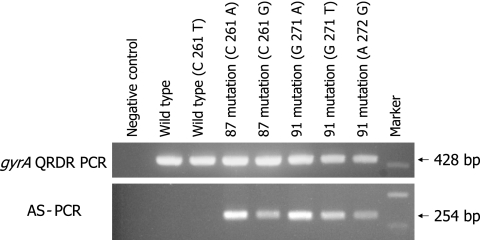
For the 51 samples, AS-PCR clearly differentiated the wild type from the gyrA mutants of H. pylori (Fig. 1). A significant association was observed between the presence of mutations in the genotype, as determined by AS-PCR, and the resistance of the strains to GAT (P < 0.001). Moreover, AS-PCR for genotyping of the strains took less than 3 to 4 h.
FIG. 1.
Representative electrophoresis patterns of gyrA quinolone resistance-determining region (QRDR) PCR products and allele-specific PCR products amplified with mixed primers for determination of C261A, C261G, G271A, G271T and A272G mutant gyrA genotypes of H. pylori. The theoretical fragment sizes according to the gyrA sequence are mentioned in the text.
DISCUSSION
Various assay techniques have been developed to investigate polymorphisms, including PCR-restriction fragment length polymorphism analysis, AS-PCR, multiplex PCR, single-strand confirmation polymorphism analysis, oligonucleotide ligation assay, and real-time PCR (3, 5, 6, 10, 15, 16, 18). AS-PCR is an excellent genotyping method, although it frequently requires extensive optimization and its background amplification is often high. It has been reported that the configuration of mismatched base pairs at the template primer 3′-terminal and penultimate nucleotides is involved in the extension efficiency of PCR (7). In this study, PCR amplification was performed with allele-specific primers in which the second nucleotide from the 3′ end was designed to match the site of the point mutation; furthermore, the third, fourth, or fifth nucleotide from the 3′ end was designed to produce a 1-bp mismatch in order to attain high specificity in the AS-PCR for mutant alleles with point mutations. AS-PCR does not require restriction enzyme cleavage, purification of PCR products, or a real-time PCR machine.
In the present study, we applied the AS-PCR method to detect mutations in the gyrA gene of H. pylori. The method was useful for easily identifying whether an H. pylori strain was sensitive or resistant to GAT. To the best of our knowledge, this is the first report of successful simultaneous detection of five kinds of point mutations by AS-PCR requiring only two PCR tubes.
Because the traditional culture test for bacterial susceptibility to antibiotics is costly and requires 10 to 14 days, this test has not been feasible in routine clinical practice, and MIC-based individualized H. pylori eradication therapy has not been prevalent among general practitioners. However, the AS-PCR method can be used to determine bacterial susceptibility to fluoroquinolones within only several hours, which we suggest would make individualized treatment really feasible in daily clinical practice. This individually tailored therapeutic strategy may be expected to increase the eradication rates for H. pylori achieved by fluoroquinolone-based triple therapy as an alternative treatment regimen.
In conclusion, we developed a reliable AS-PCR technique to detect GAT-resistant H. pylori strains with the aim of identifying potential responders to a fluoroquinolone-based eradication regimen. The method was developed with DNA extracts from H. pylori isolates, but it may be performed directly on gastric specimens (1). Because of the genetic heterogeneity of H. pylori strains (21) and other new mutants, the assay may fail for strains isolated outside Japan, but it could be adapted to detect genetic gyrA variants found in different geographical regions.
Acknowledgments
This study was supported by a grant-in-aid for scientific research C from JSPS (no. 15590686, to H.S.) and by a grant from Keio Gijuku Academic Development Funds.
Footnotes
Published ahead of print on 22 November 2006.
REFERENCES
- 1.Chisholm, S. A., R. J. Owen, E. L. Teare, and S. Saverymuttu. 2001. PCR-based diagnosis of Helicobacter pylori infection and real-time determination of clarithromycin resistance directly from human gastric biopsy samples. J. Clin. Microbiol. 39:1217-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fujimura, S., S. Kato, K. Iinuma, and A. Watanabe. 2004. In vitro activity of fluoroquinolone and the gyrA gene mutation in Helicobacter pylori strains isolated from children. J. Med. Microbiol. 53:1019-1022. [DOI] [PubMed] [Google Scholar]
- 3.Glocker, E., and M. Kist. 2004. Rapid detection of point mutations in the gyrA gene of Helicobacter pylori conferring resistance to ciprofloxacin by a fluorescence resonance energy transfer-based real-time PCR approach. J. Clin. Microbiol. 42:2241-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heep, M., M. Kist, S. Strobel, D. Beck, and N. Lehn. 2000. Secondary resistance among 554 isolates of Helicobacter pylori after failure of therapy. Eur. J. Clin. Microbiol. Infect. Dis. 19:538-541. [DOI] [PubMed] [Google Scholar]
- 5.Hersberger, M., J. Marti-Jaun, K. Rentsch, and E. Hanseler. 2000. Rapid detection of the CYP2D6*3, CYP2D6*4, and CYP2D6*6 alleles by tetra-primer PCR and of the CYP2D6*5 allele by multiplex long PCR. Clin. Chem. 46:1072-1077. [PubMed] [Google Scholar]
- 6.Hiratsuka, M., Y. Agatsuma, F. Omori, K. Narahara, T. Inoue, Y. Kishikawa, and M. Mizugaki. 2000. High throughput detection of drug-metabolizing enzyme polymorphisms by allele-specific fluorogenic 5′ nuclease chain reaction assay. Biol. Pharm. Bull. 23:1131-1135. [DOI] [PubMed] [Google Scholar]
- 7.Huang, M. M., N. Arnheim, and M. F. Goodman. 1992. Extension of base mispairs by Taq DNA polymerase: implications for single nucleotide discrimination in PCR. Nucleic Acids Res. 20:4567-4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ishiguro, A., T. Kubota, Y. Soya, H. Sasaki, O. Yagyu, Y. Takarada, and T. Iga. 2005. High-throughput detection of multiple genetic polymorphisms influencing drug metabolism with mismatch primers in allele-specific polymerase chain reaction. Anal. Biochem. 337:256-261. [DOI] [PubMed] [Google Scholar]
- 9.Kreuzer, K. N., and N. R. Cozzarelli. 1979. Escherichia coli mutants thermosensitive for deoxyribonucleic acid gyrase subunit A: effects on deoxyribonucleic acid replication, transcription, and bacteriophage growth. J. Bacteriol. 140:424-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landegren, U., R. Kaiser, J. Sanders, and L. Hood. 1988. A ligase-mediated gene detection technique. Science 241:1077-1080. [DOI] [PubMed] [Google Scholar]
- 11.Masaoka, T., H. Suzuki, K. Kurabayashi, A. G. Kamiya, and H. Ishii. 2004. Second-line treatment of Helicobacter pylori infection after dilution agar methods and PCR-RFLP analysis. Aliment. Pharmacol. Ther. 20(Suppl. 1):68-73. [DOI] [PubMed] [Google Scholar]
- 12.Moore, R. A., B. Beckthold, S. Wong, A. Kureishi, and L. E. Bryan. 1995. Nucleotide sequence of the gyrA gene and characterization of ciprofloxacin-resistant mutants of Helicobacter pylori. Antimicrob. Agents Chemother. 39:107-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NCCLS. 2004. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard-6th ed., M7-A6. National Committee for Clinical Laboratory Standards, Wayne, PA.
- 14.NCCLS. 2004. Performance standard for antimicrobial susceptibility testing; 14th informational supplement (aerobic dilution) M100-S14. NCCLS, Wayne, PA.
- 15.Nevilie, M., R. Selzer, B. Aizenstein, M. Maguire, K. Hogan, R. Walton, K. Welsh, B. Neri, and M. de Arruda. 2002. Characterization of cytochrome P450 2D6 alleles using the Invader system. BioTechniques 2002(Suppl.):34-38, 40-43. [PubMed] [Google Scholar]
- 16.Newton, C. R., A. Graham, L. E. Heptinstall, S. J. Powell, C. Summers, N. Kalsheker, J. C. Smith, and A. F. Markham. 1989. Analysis of any point mutation in DNA. The amplification refractory mutation system (ARMS). Nucleic Acids Res. 17:2503-2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishizawa, T., H. Suzuki, K. Kurabayashi, T. Masaoka, H. Muraoka, M. Mori, E. Iwasaki, I. Kobayashi, and T. Hibi. 2006. Gatifloxacin resistance and mutations in gyra after unsuccessful Helicobacter pylori eradication in Japan. Antimicrob. Agents Chemother. 50:1538-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orita, M., Y. Suzuki, T. Sekiya, and K. Hayashi. 1989. Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics 5:874-879. [DOI] [PubMed] [Google Scholar]
- 19.Reece, R. J., and A. Maxwell. 1991. DNA gyrase: structure and function. Crit. Rev. Biochem. Mol. Biol. 26:335-375. [DOI] [PubMed] [Google Scholar]
- 20.Sharara, A. I., H. F. Chaar, E. Aoun, H. Abdul-Baki, G. F. Araj, and S. S. Kanj. 2006. Efficacy and safety of rabeprazole, amoxicillin, and gatifloxacin after treatment failure of initial Helicobacter pylori eradication. Helicobacter 11:231-236. [DOI] [PubMed] [Google Scholar]
- 21.Suerbaum, S. 2000. Genetic variability within Helicobacter pylori. Int. J. Med. Microbiol. 290:175-181. [DOI] [PubMed] [Google Scholar]
- 22.Tankovic, J., C. Lascols, Q. Sculo, J. C. Petit, and C. J. Soussy. 2003. Single and double mutations in gyrA but not in gyrB are associated with low- and high-level fluoroquinolone resistance in Helicobacter pylori. Antimicrob. Agents Chemother. 47:3942-3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang, Y., W. M. Huang, and D. E. Taylor. 1993. Cloning and nucleotide sequence of the Campylobacter jejuni gyrA gene and characterization of quinolone resistance mutations. Antimicrob. Agents Chemother. 37:457-463. [DOI] [PMC free article] [PubMed] [Google Scholar]