Abstract
Objectives. We examined barriers to influenza vaccination among long-term care facility (LTCF) health care workers in Southern California and developed simple, effective interventions to improve influenza vaccine coverage of these workers.
Methods. In 2002, health care workers at LTCFs were surveyed regarding their knowledge and attitudes about influenza and the influenza vaccine. Results were used to develop 2 interventions, an educational campaign and Vaccine Day (a well-publicized day for free influenza vaccination of all employees at the worksite). Seventy facilities were recruited to participate in an intervention trial and randomly assigned to 4 study groups.
Results. The combination of Vaccine Day and an educational campaign was most effective in increasing vaccine coverage (53% coverage; prevalence ratio [PR]=1.45; 95% confidence interval [CI]=1.24, 1.71, compared with 27% coverage in the control group). Vaccine Day alone was also effective (46% coverage; PR= 1.41; 95% CI=1.17, 1.71). The educational campaign alone was not effective in improving coverage levels (34% coverage; PR=1.18; 95% CI=0.93, 1.50).
Conclusion. Influenza vaccine coverage of LTCF health care workers can be improved by providing free vaccinations at the worksite with a well-publicized Vaccine Day.
During annual influenza epidemics, persons aged 65 years and older are most likely to suffer severe influenza-related complications and death.1 Residents of long-term care facilities (LTCFs) are at particularly high risk of influenza infection because they often have multiple underlying medical problems, reside in proximity to each other, and are in contact with a wide range of caregivers in a closed setting.2–5 Outbreaks of influenza in LTCFs can result in considerable resident morbidity and mortality.6–8 Because of their susceptibility to influenza-related complications, LTCF residents are considered by the Advisory Committee on Immunization Practices to be a high-priority group for annual vaccination.1
LTCF residents should receive the influenza vaccination annually; however, in contrast to healthy adults, the elderly have suboptimal immunologic response to the influenza vaccine.9,10 Although the vaccine efficacy is estimated to be 80% in preventing death and 50% to 60% in preventing hospitalizations and pneumonia among LTCF residents, the vaccine is only 30% to 40% effective in preventing influenza infection.11–15 Thus, despite generally high vaccination rates among residents, influenza outbreaks still occur in LTCFs, sometimes triggered by illness among unvaccinated health care workers.16–19
Health care worker vaccination has been shown to reduce morbidity and mortality among the elderly in long-term care settings.20,21 Preventing influenza among LTCF residents through vaccination of health care workers is therefore critical in protecting this vulnerable population. Vaccination of these LTCF personnel also lowers costs for LTCFs because it prevents worker illness and reduces absenteeism.22–24 National organizations, including the Advisory Committee on Immunization Practices, American Medical Association, and Association for Professionals in Infection Control and Epidemiology, Inc, strongly promote influenza vaccination of health care workers as an important public health goal.25,26 Nonetheless, health care worker vaccination rates are estimated to be less than 40% in LTCFs in the United States, far below the national health objective for 2010 to achieve health care worker coverage of 60%.1,27
We conducted a 2-year study in community-based LTCFs to ascertain the reasons for the low influenza vaccine coverage of health care workers and used this information to design and test interventions to improve their vaccination rates.
METHODS
Survey and Intervention Design
In May 2002, 30 LTCFs were randomly selected from 4 Southern California local health department jurisdictions to participate in a knowledge, attitudes, and behaviors survey. The administrator of each LTCF was asked to complete a questionnaire regarding number of employees (total and by job category) and employee influenza vaccination policies and practices. A self-administered questionnaire in English and Spanish was distributed to all employees with direct resident contact (nurses, nursing assistants, rehabilitation therapists, and housekeeping staff). Questions included demographic information, knowledge and attitudes about influenza and influenza vaccine, and vaccination behaviors for the 2000 to 2001 and the 2001 to 2002 influenza seasons.
The reasons health care workers cited in the survey for not receiving the influenza vaccine belonged to 2 main categories: misconceptions regarding influenza and the vaccine and vaccine accessibility. Accordingly, we developed interventions to specifically address each category: (1) an educational campaign that clarified misconceptions about influenza and the vaccine and emphasized the seriousness of influenza, and (2) a “Vaccine Day,” which addressed vaccine accessibility issues by providing free vaccinations at the LTCF work site. The educational campaign included the following components: in-service training at which employees were shown a 10-minute educational video and given a detailed question-and-answer brochure, a 1-page educational flyer distributed with paychecks, and informational posters displayed in common areas. The Vaccine Day intervention consisted of 1 or more well-publicized days when all health care workers could receive the influenza vaccine for free at the facility. Vaccine Day reminder posters were displayed in common areas, and employees received reminder notices with their paychecks. LTCFs were provided with inactivated influenza vaccine for staff vaccination; LTCFs designated nurses for vaccine administration. Influenza vaccine was available during the remainder of the season for employees who were not vaccinated on Vaccine Day. All intervention materials were available in English and Spanish. (Materials used in this study, including educational flyers and posters, are available for free at http://www.immunizecaadults.org.)
The intervention trial used a 2 × 2 factorial design, with 4 groups of LTCFs: group A was the control group and did not conduct either intervention, group B conducted the educational campaign, group C conducted the Vaccine Day intervention, and group D conducted both interventions. The protocol and questionnaires were approved by the committee for the protection of human subjects at the California Department of Health Services.
Seventy LTCFs from the 4 local health department jurisdictions involved in the knowledge, attitudes, and behaviors survey were recruited to participate in the intervention trial. To avoid potential bias, 131 LTCFs that had participated in the knowledge, attitudes, and behaviors survey or in an LTCF influenza vaccine survey conducted the previous year were excluded from consideration, leaving 376 LTCFs eligible for recruitment (Figure 1 ▶). Three local health departments were unable to provide influenza vaccine for the study LTCFs within their jurisdictions; therefore, the 92 LTCFs within these jurisdictions were randomly assigned to recruitment lists for the control group and the educational campaign group. The remaining 284 LTCFs within the other local health department jurisdiction were randomly assigned to recruitment lists for the Vaccine Day group and the group conducting both interventions (the combined intervention group). The LTCFs were recruited by telephone; if appropriate personnel were not reached in 4 attempts, the next LTCF on the list was contacted. Recruitment continued until there were 25 LTCFs for the control group and 15 LTCFs each for the educational campaign group, the Vaccine Day group, and the combined intervention group.
FIGURE 1—
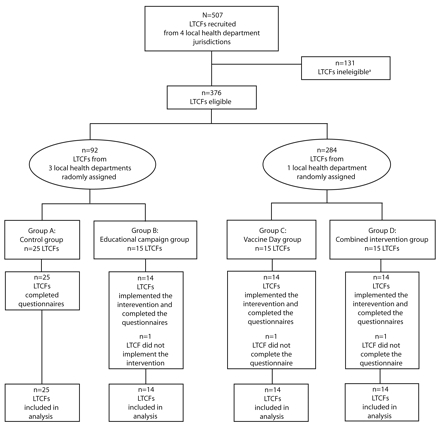
Assignment of long-term care facilities (LTCFs) to intervention groups: Southern California, 2002–2003
Note. Three local health departments were unable to provide the influenza vaccine to health care workers; LTCFs in these jurisdictions were randomly assigned to the control group and the educational campaign group only. LTCFs in the fourth local health department jurisdiction were randomly assigned to the Vaccine Day group and the combined intervention (conducting both the educational campaign and the Vaccine Day interventions) group.
aLTCFs were not eligible if they participated in the knowledge, attitudes, and behaviors survey or in an LTCF influenza vaccine survey conducted in 2001 or if they were not exclusively classified as a skilled nursing facility.
The educational campaign and Vaccine Day interventions were implemented in October and November 2002. Study personnel delivered the intervention materials to LTCFs in the educational campaign group, the Vaccine Day group, and combined intervention group and reviewed the intervention protocol with the LTCF administrator, director of nursing, or director of staff development. LTCFs were responsible for conducting the assigned interventions.
In January 2003, all employees in participating LTCFs were asked to complete a self-administered questionnaire (in English or Spanish) regarding their job category and vaccination status for the baseline (2001–2002) and postintervention (2002–2003) influenza seasons. The primary contact at each LTCF in the educational campaign group, Vaccine Day group, and combined intervention group also completed a questionnaire regarding his or her facility’s implementation of the interventions.
Statistical Analysis
Statistical analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC). The significance level selected for all analyses was P ≤ .05. We used the χ2 test to perform univariate analyses and bivariate analyses to examine data distributions and associations between variables. To account for correlated observations within each LTCF, the GENMOD procedure was used to fit a log-binomial regression model with generalized estimating equations. Factors previously shown to be associated with influenza vaccination were included in the model.28–33 Facility size (number of licensed beds) was modeled as a continuous variable, and employee baseline vaccination status was modeled as a categorical variable. Employee baseline and postintervention influenza vaccination rates were calculated by dividing the number of employees who responded “yes” to receiving the influenza vaccine from September through December 2001 and from September through December 2002, respectively, by the total number of employees responding to the survey, excluding those who answered “don’t remember.”
The estimated material cost of each intervention was based on an average LTCF with 100 employees and included the provision of English and Spanish materials. The vaccine cost was calculated using the 2002 to 2003 influenza season wholesale vaccine price of $10.50 per dose.
RESULTS
Knowledge, Attitudes, and Behaviors Survey
The 30 LTCFs in the survey had a mean of 94 employees (SD = 31; range = 48–184). None of the LTCFs had written policies requiring employees to receive the influenza vaccine annually. For the health care worker questionnaire, 1020 (45%) of 2271 questionnaires were returned. The majority of respondents were nursing assistants (55%), women (79%), and younger than 50 years (81%); 50% were Hispanic. Only 54% of the health care workers received paid sick leave, and 30% reported having no health insurance coverage. Thirty percent of respondents reported vaccination for the 2000 to 2001 influenza season and 34% for the 2001 to 2002 influenza season (Table 1 ▶).
TABLE 1—
Characteristics and Beliefs Associated With Influenza Vaccination Among Health Care Workers (N = 1020) at Long-Term Care Facilities: Southern California, 2002
| Received Influenza Vaccine for 2001–2002a | |||
| Characteristic or Belief | Total No. (%)b | No. (%) | Pc |
| Job Classification | |||
| Nurse | 275 (27) | 92 (35) | .85 |
| Nursing assistant | 564 (55) | 177 (35) | |
| Housekeeping staff | 127 (12) | 37 (33) | |
| Rehabilitation therapist | 54 (5) | 16 (30) | |
| Gender | |||
| Women | 799 (79) | 250 (33) | .26 |
| Men | 208 (21) | 69 (38) | |
| Race/Ethnicity | |||
| Hispanic | 507 (50) | 144 (31) | .07 |
| Asian/Pacific Islander | 349 (35) | 129 (40) | |
| White | 80 (8) | 26 (34) | |
| Black | 73 (7) | 19 (28) | |
| Age, y | |||
| < 30 | 221 (23) | 50 (26) | <.001 |
| 30–39 | 276 (28) | 86 (33) | |
| 40–49 | 293 (30) | 94 (35) | |
| ≥ 50 | 191 (19) | 81 (46) | |
| Receives paid sick leave | |||
| Yes | 522 (54) | 177 (36) | .14 |
| No | 436 (46) | 125 (32) | |
| Health insurance | |||
| Insured | 709 (70) | 237 (36) | .09 |
| Uninsured | 298 (30) | 81 (30) | |
| Received influenza vaccine for the 2000–2001 influenza season | |||
| Yes | 274 (30) | 205 (78) | <.001 |
| No | 637 (70) | 82 (13) | |
| Received influenza vaccine for the 2001–2002 influenza season | |||
| Yes | 322 (34) | . . . | . . . |
| No | 615 (66) | . . . | . . . |
| Facility offered influenza vaccine in 2001 | |||
| Yes | 473 (48) | 221 (48) | <.001 |
| No | 308 (31) | 49 (17) | |
| Do not know | 205 (21) | 47 (27) | |
| Vaccine can cause influenza | |||
| Yes | 379 (39) | 96 (26) | <.001 |
| No | 351 (36) | 159 (48) | |
| Do not know | 246 (25) | 57 (26) | |
| Effectiveness of vaccine | |||
| Very effective | 320 (32) | 157 (53) | <.001 |
| Somewhat effective | 397 (40) | 121 (32) | |
| Not effective | 83 (8) | 17 (22) | |
| Do not know | 200 (20) | 21 (12) | |
Note. Ellipses indicate that data was not applicable.
aHealth care workers who responded “don’t remember” to receiving influenza vaccine for 2001–2002 season were excluded.
bHealth care workers who did not respond regarding a characteristic or belief were excluded.
cSignificance determined using the χ2 test.
Factors significantly associated with health care workers not being vaccinated for the 2001 to 2002 influenza season included younger age, perception that the vaccine was risky or ineffective, and unavailability of free vaccine for employees at their workplace (Table 1 ▶). Many health care workers (39%) believed that the vaccine could cause influenza. A strong predictor for influenza vaccination was receipt of the vaccine in the previous season (P<.001).
Among those who did not receive the influenza vaccine for the 2001 to 2002 season, common reasons for not receiving the vaccine included concern about side effects (17%) and the belief that they never got influenza (18%) or that the vaccine was ineffective (17%). Other reasons included forgetting to get vaccinated (16%), being too busy (15%), and concern about getting influenza from the vaccine (14%).
Intervention Implementation and Effectiveness
Sixty-seven (95%) LTCFs completed the intervention trial. One educational campaign group LTCF did not implement the specified intervention and 2 LTCFs (1 each from the Vaccine Day and combined intervention groups) did not return health care worker questionnaires (Figure 1 ▶). These 3 LTCFs were excluded from further analyses.
The facility characteristics are presented in Table 2 ▶. The majority (92%) of LTCFs were for-profit facilities. The LTCFs had a mean of 105 licensed beds (SD=49; range=28–299) and 103 employees (SD=51; range=30–381). Facility characteristics were similar across all groups.
TABLE 2—
Characteristics of Long-Term Care Facilities, by Intervention Group: Southern California, 2002–2003
| Characteristic | Control Group (n = 25) | Educational Campaign Group (n = 14) | Vaccine Day Group (n = 14) | Combined Intervention Groupa (n = 14) | Total (N = 67) | P |
| For-profit ownership, no. (%) | 23 (92) | 12 (86) | 13 (93) | 11 (79) | 59 (88) | .64 |
| No. licensed beds, mean (SD; range) | 107 (42; 45–199) | 117 (55; 45–255) | 103 (67; 28–299) | 92 (31; 43–156) | 105 (49; 28–299) | .60 |
| No. employees, mean (SD; range) | 107 (41; 39–194) | 110 (30; 52–161) | 98 (86; 30–381) | 93 (39; 40–196) | 103 (51; 30–381) | .79 |
aThe combined intervention group conducted both the educational campaign intervention and the Vaccine Day intervention.
Of the 7039 questionnaires distributed to employees postintervention, 4338 (62%) were returned. The response rates for the control group, educational campaign group, Vaccine Day group, and combined intervention group were 64%, 59%, 67%, and 65%, respectively; the differences in response rates were not statistically significant. Response rates by job category also did not differ across groups. Nurses and nursing assistants accounted for the largest proportion of respondents, approximately 60%; 20% of respondents were housekeeping and food service personnel.
Table 3 ▶ shows the baseline (2001–2002 season) and postintervention (2002–2003 season) influenza vaccination rates for health care workers. Baseline vaccination rates for the 4 groups ranged from 29% to 39%; after adjusting for correlated observations, baseline vaccination rates differed only between the educational campaign group and the combined intervention group (P= .03). Postintervention vaccination rates ranged from 28% to 53%. With the exception of the control group, which had a decrease in the vaccination rate from baseline to post-intervention (31% baseline vs 28% post-intervention), all other groups had increases in vaccination rates. In the educational campaign group, the rate increased only slightly, from 29% to 34%, whereas the increases in vaccination rates were more marked in the Vaccine Day and combined intervention groups. In the Vaccine Day group, the rate increased 31%, from 35% to 46%, and in the combined intervention group, the rate increased from 39% to 53%, a 36% increase from baseline to postintervention.
TABLE 3—
Baseline (2001–2002 Influenza Season) and Postintervention (2002–2003 Influenza Season) Influenza Vaccine Coverage of Health Care Workers at Long-Term Care Facilities, by Intervention Group: Southern California, 2002–2003
| No. Vaccinated (%) | |||||
| Group | No. of Health Care Workersa | Baseline | Postintervention | Crude PR (95% CI) | Adjusted PR (95% CI)b |
| Control group | 1517 | 467 (31) | 450 (28) | 1.00 | 1.00 |
| Educational campaign group | 821 | 240 (29) | 298 (34) | 1.23 (0.87, 1.72) | 1.18 (0.93, 1.50) |
| Vaccine Day group | 832 | 292 (35) | 410 (46) | 1.66 (1.23, 2.23) | 1.41 (1.17, 1.71) |
| Combined intervention groupc | 754 | 295 (39) | 439 (53) | 1.93 (1.45, 2.58) | 1.45 (1.24, 1.71) |
Note. PR = prevalence ratio; CI = confidence interval.
aHealth care workers whose influenza vaccination status was unknown for the 2001–2002 or 2002–2003 influenza seasons were excluded from the analyses.
bAdjusted for health care worker baseline vaccination status, facility size (number of licensed beds), and correlated observations.
c The combined intervention group conducted both the educational campaign intervention and the Vaccine Day intervention.
Crude and adjusted prevalence ratios (PRs) for postintervention vaccination status are also shown in Table 3 ▶. The combination of Vaccine Day and educational campaign interventions conducted by LTCFs in the combined intervention group was the most effective in increasing employee vaccination when compared with the control group; employees from the combined intervention group were 45% more likely to be vaccinated than were employees from the control group (adjusted PR= 1.45; 95% confidence interval [CI]=1.24, 1.71). The Vaccine Day intervention was also effective; employees from the Vaccine Day group were 42% more likely to be vaccinated than were employees from the control group (PR=1.42; 95% CI=1.17, 1.71). Although the educational campaign group showed a slight increase in coverage, this was not significant in comparison with the control group (PR=1.18; 95% CI=0.93, 1.50).
Time and Cost of Implementing Interventions
LTCFs in the educational campaign group, Vaccine Day group, and combined intervention group reported that the interventions were easy to implement. On average, LTCFs reported spending less than 30 minutes on displaying posters and distributing flyers, less than 1 hour for planning in-service training, and less than 1 hour for organizing Vaccine Days.
The estimated cost of materials for the educational campaign in an LTCF with 100 employees was $70. The cost for the Vaccine Day intervention was estimated to be $1080 per LTCF, with 97% ($1050) of the cost for influenza vaccine. Hence, the estimated cost to conduct both the educational campaign and Vaccine Day interventions in a facility with 100 employees was $1150.
DISCUSSION
Influenza vaccine coverage of LTCF health care workers can be improved. LTCFs in this study significantly increased employee vaccination by conducting Vaccine Days, well-publicized days in which vaccine was provided free of charge to all employees. To our knowledge, this is the first US study to concurrently and prospectively assess different methods to improve health care worker influenza vaccination rates in a substantial number of community-based LTCFs. The few previously published intervention studies have been conducted either in single facilities or in facilities outside the United States.34–36
Our Vaccine Day intervention was designed to address vaccine accessibility issues identified through the knowledge, attitudes, and behaviors survey by providing free influenza vaccine at the worksite, thereby minimizing cost and time barriers. In addition, Vaccine Day was presented as an important facility-wide event at the LTCFs, with posters prominently displayed and reminder flyers distributed to each employee. We feel that offering the vaccine in such a well-publicized, institutionally supported manner was critical to the success of this intervention. Other vaccination programs that have also achieved success have strongly promoted health care worker influenza vaccination as organized events, such as in the setting of a Vaccine Fair or with the use of vaccination carts.36–40
In addition to underscoring vaccine accessibility issues, the knowledge, attitudes, and behaviors survey indicated that health care workers were not getting vaccinated because of misconceptions regarding influenza and the influenza vaccine, a finding consistent with other studies.28–31,41 Although our educational campaign addressed these misconceptions, it did not significantly affect employee vaccination when implemented independently of Vaccine Day. Therefore, although education should be part of any intervention to increase LTCF staff vaccination, improving access to the vaccine is crucial.
Although the Vaccine Day interventions had significant effects on employee vaccine coverage, the vaccination rates were still low. However, employees vaccinated against influenza in 1 season are more likely to get vaccinated the following season.28,30 If Vaccine Day becomes an established annual event at LTCFs, it is possible that more employees will be vaccinated each subsequent year as institutional support increases and vaccinated employees become role models to their coworkers, as has been demonstrated in other employee vaccination programs.37,39
Limitations
Our study has several limitations. Response rates for the knowledge, attitudes, and behaviors and postintervention employee surveys were suboptimal, which could have led to response bias if nonrespondents differed from respondents. We were unable to directly compare characteristics of respondents and non-respondents, because employees submitted questionnaires anonymously. However, when we examined respondents by job category, the proportions of respondents for the knowledge, attitudes, and behaviors survey and the post-intervention employee survey were similar to the staffing compositions reported by the participating LTCFs and the National Nursing Home Survey,42 respectively. Recall bias is also a potential study limitation, because employee vaccination status was self-reported; however, this should be minimal, because the vaccination rates for both the knowledge, attitudes, and behaviors survey and the postintervention employee survey (baseline influenza season) were consistent with published data.1,18 In addition, the intervention survey was part of a controlled study and we would expect staff recall of vaccination status to be similar across study groups.
For logistical reasons, LTCFs for the Vaccine Day and combined intervention groups were recruited from only 1 local health department jurisdiction, potentially creating a sampling bias because the amount of interaction that a local health department has with LTCFs may differ between jurisdictions. However, there were no significant differences in LTCF characteristics (ownership, number of licensed beds, and number of employees) or in baseline vaccination rates between each intervention group and the control group. Finally, we did not have the resources to ensure that the LTCFs implemented all the components of their respective interventions; it is possible that some LTCFs may not have adhered completely to their intervention protocol, diminishing the true effect of the interventions.
Conclusions
Our study confirmed that influenza vaccination rates among LTCF health care workers are dismally low, with fewer than 40% receiving the influenza vaccine during the 2001 to 2002 influenza season. Adding urgency to this finding is that these employees may work while infected with influenza,18,22,43 increasing the risk of disease transmission to residents. A substantial number of workers in our study did not receive paid sick leave, creating a financial disincentive for absenteeism. Furthermore, we found that 30% of LTCF health care workers do not have health insurance, suggesting that many of these employees lack access to routine medical services, including vaccinations. Vaccine must therefore be given at the place of employment to ensure full coverage.
Convincing LTCF management (e.g., owners, administrators, medical directors) that vaccinating their employees is as important as vaccinating their residents remains a formidable challenge because providing influenza vaccine to all their personnel is a significant expense for LTCFs. However, the primary responsibility of LTCFs is to act in the best interest of their residents. It is the LTCFs’ obligation to protect their residents’ health by improving employee vaccination rates. LTCF management must recognize that vaccinating their employees is a sound fiscal investment in addition to being the standard of care.1,26
Although we did not perform a cost–benefit analysis, model-based economic analyses have indicated that influenza vaccination of healthy working adults is generally cost effective.24,44,45 Costs from employee absenteeism during influenza outbreaks can be considerable; sick leave costs for a Canadian hospital during the 1980 to 1981 influenza epidemic reached $24,500.46 With increased employee absenteeism during an influenza epidemic, LTCFs may need to hire temporary workers or require workers who are not ill to work longer shifts, which may compromise care and lead to higher costs.47 Furthermore, when influenza outbreaks occur in LTCFs, standard guidelines dictate that all residents and any unvaccinated health care workers be placed on chemoprophylaxis, all unvaccinated residents and workers be vaccinated, and all ill residents be confined to the same area of the facility.1,48 Implementation of these measures can be much more costly to LTCFs than providing vaccine to their employees.
Legislative and regulatory efforts may need to be enacted to further improve vaccination rates. Federal and state agencies may consider subsidizing influenza vaccine purchased for health care workers. Health department licensing and certification programs can record vaccination rates for these employees, encourage vaccination efforts, and provide incentives for improvement. Health care worker vaccination rates can be included as a federal quality indicator for Medicare- and Medicaid-certified nursing homes. Legislative mandates to vaccinate eligible health care personnel against influenza have reportedly been enacted in some states, although the effect on vaccination coverage is unknown.26,49
The US population is aging. In 2000, persons aged 65 years and older accounted for 12% (35 million people) of the population; this figure is expected to increase to almost 20% (70 million people) by 2030.50 As the population ages, the number of persons living in LTCFs and other chronic care facilities will likewise increase. In 2000, there were 1.7 million residents in LTCFs in the United States; this is projected to increase to 3 million by 2030.51 Addressing preventive care in LTCFs to optimize the health and well-being of an expanding elderly population is of critical public health importance. A vital component of preventive care for LTCF residents is the vaccination of health care workers against influenza. LTCFs can improve vaccination coverage in their employees and thereby reduce influenza-related illness and death among their residents by making influenza vaccination of health care workers an important and accessible annual event.
Acknowledgments
This study was supported in part by the Epidemiology and Lab Capacity for Infectious Diseases Cooperative Agreement, Centers for Disease Control and Prevention, Atlanta, Ga (grant U50/CCU916805).
We gratefully acknowledge the participating long-term care facilities and the following public health programs for their contributions to this study: Centers for Disease Control and Prevention, National Immunization Program; California Department of Health Services, Infectious Diseases and Immunization Branches; Los Angeles County Department of Health Services, Immunization Program, and Public Health Training Unit; County of Orange Health Care Agency, Epidemiology and Assessment; Long Beach Department of Health and Human Services, Epidemiology and Communicable Disease; and Pasadena Health Department, Disease Prevention and Control Division. We especially appreciate the assistance of Howard Backer, MD; Davíd Betterton; Alvin Nelson El-Amin, MD; Maureen Flannery, MPH; David Gambill, MSc; Nisha Gandhi, MPH; Leticia Ibarra, MPH; Anna Invencion, MPH; Marcy Connel Jones; Hildy Meyers, MD, MPH; Denise Rogers, MPH; Amanda Roth, MPH; Blanca Sanchez; Cathy Schellhase, RN, PHN; Martha Stokes; and Joyanna Wendt, MD, MPH.
Human Participant Protection This study was approved by the California Health and Human Services Agency committee for the protection of human subjects.
Peer Reviewed
Contributors A. C. Kimura assisted in the origination and design of the study and interventions, supervised all aspects of the study’s implementation, and drafted the article. C.N. Nguyen developed the intervention materials, served as liaison for long-term care facilities, and collected and analyzed the data. J.I. Higa assisted with the study and intervention design and with data collection and analyses. E.L. Hurwitz assisted with data analyses and was integral in the interpretation of data. D.J. Vugia provided technical and scientific support and helped conceive the study design. All authors contributed substantially to the revision and approval of the article.
References
- 1.Harper SA, Fukuda K, Uyeki TM, Cox NJ, Bridges CB. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2005;54:1–40. [PubMed] [Google Scholar]
- 2.Gravenstein S, Davidson HE. Current strategies for management of influenza in the elderly population. Clin Infect Dis. 2002;35:729–737. [DOI] [PubMed] [Google Scholar]
- 3.Arden NH. Control of influenza in the long-term-care facility: a review of established approaches and newer options. Infect Control Hosp Epidemiol. 2000;21:59–64. [DOI] [PubMed] [Google Scholar]
- 4.Bridges CB, Kuehnert MJ, Hall CB. Transmission of influenza: implications for control in health care settings. Clin Infect Dis. 2003;37:1094–1101. [DOI] [PubMed] [Google Scholar]
- 5.Patriarca PA, Weber JA, Parker RA, et al. Risk factors for outbreaks of influenza in nursing homes. A case-control study. Am J Epidemiol. 1986;124:114–119. [DOI] [PubMed] [Google Scholar]
- 6.Morens DM, Rash VM. Lessons from a nursing home outbreak of influenza A. Infect Control Hosp Epidemiol. 1995;16:275–280. [DOI] [PubMed] [Google Scholar]
- 7.Meiklejohn G, Hall H. Unusual outbreak of influenza A in a Wyoming nursing home. J Am Geriatr Soc. 1987;35:742–746. [DOI] [PubMed] [Google Scholar]
- 8.Goodman RA, Orenstein WA, Munro TF, Smith SC, Sikes RK. Impact of influenza A in a nursing home. JAMA. 1982;247:1451–1453. [PubMed] [Google Scholar]
- 9.Potter JM, O’Donnel B, Carman WF, Roberts MA, Stott DJ. Serological response to influenza vaccination and nutritional and functional status of patients in geriatric medical long-term care. Age Ageing. 1999;28:141–145. [DOI] [PubMed] [Google Scholar]
- 10.Remarque EJ, Cools HJ, Boere TJ, van der Klis RJ, Masurel N, Ligthart GJ. Functional disability and antibody response to influenza vaccine in elderly patients in a Dutch nursing home. BMJ. 1996;312:1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Influenza vaccine efficacy in nursing home outbreaks reported during 1981–1982. MMWR Morb Mortal Wkly Rep. 1982;31:. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Outbreaks of influenza among nursing home residents–Connecticut, United States. MMWR Morb Mortal Wkly Rep. 1985;34:478–482. [PubMed] [Google Scholar]
- 13.Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med. 1995;123:518–527. [DOI] [PubMed] [Google Scholar]
- 14.Patriarca PA, Weber JA, Parker RA, et al. Efficacy of influenza vaccine in nursing homes. Reduction in illness and complications during an influenza A (H3N2) epidemic. JAMA. 1985;253:1136–1139. [PubMed] [Google Scholar]
- 15.Monto AS, Hornbuckle K, Ohmit SE. Influenza vaccine effectiveness among elderly nursing home residents: a cohort study. Am J Epidemiol. 2001;154:155–160. [DOI] [PubMed] [Google Scholar]
- 16.Zadeh MM, Buxton Bridges C, Thompson WW, Arden NH, Fukuda K. Influenza outbreak detection and control measures in nursing homes in the United States. J Am Geriatr Soc. 2000;48:1310–1315. [DOI] [PubMed] [Google Scholar]
- 17.Budnick LD, Stricof RL, Ellis F. An outbreak of influenza A in a nursing home, 1982. N Y State J Med. 1984;84:235–238. [PubMed] [Google Scholar]
- 18.Coles FB, Balzano GJ, Morse DL. An outbreak of influenza A (H3N2) in a well immunized nursing home population. J Am Geriatr Soc. 1992;40:589–592. [DOI] [PubMed] [Google Scholar]
- 19.Monto AS, Rotthoff J, Teich E, et al. Detection and control of influenza outbreaks in well-vaccinated nursing home populations. Clin Infect Dis. 2004;39:459–464. [DOI] [PubMed] [Google Scholar]
- 20.Carman WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–97. [DOI] [PubMed] [Google Scholar]
- 21.Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilde JA, McMillan JA, Serwint J, Butta J, O’Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999;281:908–913. [DOI] [PubMed] [Google Scholar]
- 23.Saxen H, Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18:779–783. [DOI] [PubMed] [Google Scholar]
- 24.Yassi A, Kettner J, Hammond G, Cheang M, McGill M. Effectiveness and cost benefit of an influenza vaccination program for health care workers. Can J Infect Control. 1991;2:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Foundation for Infectious Diseases. Call to action: influenza immunization among health-care personnel, 2003. Available at: http://www.nfid.org/publications/calltoaction.pdf. Accessed August 4, 2005.
- 26.Pearson ML, Bridges CB, Harper SA. Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006;55:1–16. [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services. Healthy People 2010 Midcourse Review. Available at: http://www.healthypeople.gov/data/midcourse/comments/faobjective.asp?id=14. Accessed March 17, 2006.
- 28.Heimberger T, Chang HG, Shaikh M, Crotty L, Morse D, Birkhead G. Knowledge and attitudes of healthcare workers about influenza: why are they not getting vaccinated? Infect Control Hosp Epidemiol. 1995;16:412–415. [DOI] [PubMed] [Google Scholar]
- 29.Nichol KL, Hauge M. Influenza vaccination of healthcare workers. Infect Control Hosp Epidemiol. 1997;18:189–194. [DOI] [PubMed] [Google Scholar]
- 30.Begue RE, Gee SQ. Improving influenza immunization among healthcare workers. Infect Control Hosp Epidemiol. 1998;19:518–520. [DOI] [PubMed] [Google Scholar]
- 31.Beguin C, Boland B, Ninane J. Health care workers: vectors of influenza virus? Low vaccination rate among hospital health care workers. Am J Med Qual. 1998;13:223–227. [DOI] [PubMed] [Google Scholar]
- 32.Stevenson CG, McArthur MA, Naus M, Abraham E, McGeer AJ. Prevention of influenza and pneumococcal pneumonia in Canadian long-term care facilities: how are we doing? CMAJ. 2001;164(10):1413–1419. [PMC free article] [PubMed] [Google Scholar]
- 33.Doebbeling BN, Edmond MB, Davis CS, Woodin JR, Zeitler RR. Influenza vaccination of health care workers: evaluation of factors that are important in acceptance. Prev Med. 1997;26(1):68–77. [DOI] [PubMed] [Google Scholar]
- 34.Tannenbaum TN, Thomas D, Baumgarten M, Saintonge F, Rohan I. Evaluation of an influenza vaccination program for nursing home staff. Can J Public Health. 1993;84:60–62. [PubMed] [Google Scholar]
- 35.Dey P, Halder S, Collins S, Benons L, Woodman C. Promoting uptake of influenza vaccination among health care workers: a randomized controlled trial. J Public Health Med. 2001;23:346–348. [DOI] [PubMed] [Google Scholar]
- 36.Thomas DR, Winsted B, Koontz C. Improving neglected influenza vaccination among healthcare workers in long-term care. J Am Geriatr Soc. 1993;41:928–930. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. Interventions to increase influenza vaccination of health-care workers—California and Minnesota. MMWR Morb Mortal Wkly Rep. 2005;54:196–199. [PubMed] [Google Scholar]
- 38.Hall KL, Holmes SS, Evans ME. Increasing hospital employee participation in an influenza vaccine program. Am J Infect Control. 1998;26:367–368. [DOI] [PubMed] [Google Scholar]
- 39.Boersma B, Rhames T, Keegan JM. Additional cost savings of an effective employee influenza program on prevention of nosocomial influenza. Am J Infect Control. 1999;27:177–178. [DOI] [PubMed] [Google Scholar]
- 40.Pachucki CT, Pappas SA, Fuller GF, Krause SL, Lentino JR, Schaaff DM. Influenza A among hospital personnel and patients. Implications for recognition, prevention, and control. Arch Intern Med. 1989;149:77–80. [PubMed] [Google Scholar]
- 41.Manuel DG, Henry B, Hockin J, Naus M. Health behavior associated with influenza vaccination among healthcare workers in long-term-care facilities. Infect Control Hosp Epidemiol. 2002;23:609–614. [DOI] [PubMed] [Google Scholar]
- 42.Jones A. The National Nursing Home Survey: 1999 summary. Vital and Health Statistics, series 13, no. 152. Hyattsville, Md: US Department of Health and Human Services; 2002. [PubMed]
- 43.Elder AG, O’Donnell B, McCruden EA, Symington IS, Carman WF. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993–4 epidemic: results of serum testing and questionnaire. BMJ. 1996;313:1241–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nichol KL. The efficacy, effectiveness and cost-effectiveness of inactivated influenza virus vaccines. Vaccine. 2003;21:1769–1775. [DOI] [PubMed] [Google Scholar]
- 45.Lee PY, Matchar DB, Clements DA, Huber J, Hamilton JD, Peterson ED. Economic analysis of influenza vaccination and antiviral treatment for healthy working adults. Ann Intern Med. 2002;137:225–231. [DOI] [PubMed] [Google Scholar]
- 46.Hammond GW, Cheang M. Absenteeism among hospital staff during an influenza epidemic: implications for immunoprophylaxis. Can Med Assoc J. 1984; 131:449–452. [PMC free article] [PubMed] [Google Scholar]
- 47.Todd C, Reid N, Robinson G. The quality of nursing care on wards working eight and twelve hour shifts: a repeated measures study using the MONITOR index of quality of care. Int J Nurs Stud. 1989;26:359–368. [DOI] [PubMed] [Google Scholar]
- 48.Bradley SF. Prevention of influenza in long-term-care facilities. Long-Term-Care Committee of the Society for Healthcare Epidemiology of America. Infect Control Hosp Epidemiol. 1999;20:629–637. [DOI] [PubMed] [Google Scholar]
- 49.Stewart A, Cox M, Rosenbaum S. The epidemiology of U.S. immunization law: immunization requirements for staff and residents of long-term care facilities under state laws/regulations. Available at: http://www.gwumc.edu/sphhs/healthpolicy/immunization/EUSIL-LTC-report.pdf. Accessed March 8, 2006.
- 50.US Census Bureau. U.S. interim projections by age, sex, race, and Hispanic origin. Available at: http://www.census.gov/ipc/www/usinterimproj. Accessed June 14, 2005.
- 51.Sahyoun NR, Pratt LA, Lentzner H, Dey A, Robinson KN. The changing profile of nursing home residents: 1985–1997. Available at: http://www.cdc.gov/nchs/data/agingtrends/04nursin.pdf. Accessed July 29, 2005. [DOI] [PubMed]


