Abstract
Active caspase-6 (Csp6) and Tau cleaved by Csp6 (TauΔCsp6) are abundant in neuritic plaques (NPs), neuropil threads (NPTs), and neurofibrillary tangles (NFTs) in end-stage Alzheimer’s disease (AD) (Guo H, Albrecht S, Bourdeau M, Petzke T, Bergeron C, LeBlanc AC: Active caspase-6 and caspase-6 cleaved Tau in neuropil threads, neuritic plaques and neurofibrillary tangles of Alzheimer’s disease. Am J Pathol 2004, 165:523–531). The goal of this study was to determine whether active Csp6 is present in young and aged noncognitively impaired (NCI); aged mild cognitively impaired (MCI); and aged mild, moderate, severe, and very severe AD individuals. Csp6 activity was assessed with anti-p20Csp6 and TauΔCsp6 immunoreactivity. Active Csp6 is present in NFTs, NPTs, and NPs at all stages of AD. Active Csp6 is present in NFTs of all MCI cases and present in NPTs and NPs of some MCI cases. Active Csp6 is present in NFTs and NPTs of all NCI cases but is absent in younger cases. The level of TauΔCsp6-positive NFTs and NPTs correlates inversely with global cognitive scores in NCI individuals. Therefore, Csp6 activity can occur with aging in the absence of AD and is always associated with clinical and pathological features of confirmed AD cases. Given the ability of active Csp6 to increase amyloid-β peptide production and cleave Tau and several synaptic proteins (LeBlanc AC, Liu H, Goodyer C, Bergeron C, Hammond J: Caspase-6 role in apoptosis of human neurons, amyloidogenesis and Alzheimer’s disease. J Biol Chem 1999, 274:23426–23436; Petzke TL, Rousselet E, Goodyer C, LeBlanc AC: Substrates of caspase-6 in human primary neurons: a proteomic study. Program No. 80.9. 2005 Abstract Viewer/Itinerary Planner. Washington, DC: Society for Neuroscience. Online), we suggest that active Csp6 could be an early instigator of neuronal dysfunction.
Identification of the early events of Alzheimer’s disease (AD) is essential for effective treatment. Although neuritic plaques (NPs) and neurofibrillary tangles (NFTs) have been the main focus of fundamental research efforts to quell the progressive dementia associated with AD, few investigations have been dedicated to elucidating events that lead to the formation of plaques and tangles in the sporadic form of the disease. Our research has focused on identifying key molecular components that initiate neuronal dysfunction and degeneration and subsequent NP and NFT formation in AD. We have identified caspase-6 (Csp6) as a strong candidate for such a role. Csp6 is activated in human neurons on an apoptotic insult, indirectly increases the levels of amyloid-β peptide (Aβ) production, and directly induces a protracted type of cell death in the absence of any other insult.1,2,3,4 The active Csp6 and Tau cleaved by Csp6 (TauΔCsp6) are highly abundant in the neuropil threads (NPTs), NFTs, and NPs of severe AD brains.5 In AD brains, Csp6 remains neuritic and is not nuclear, in contrast to human ischemia, in which Csp6 translocates to the nuclei, a mechanism known to be important for lamin A cleavage and subsequent condensation of the chromatin in apoptotic cells.6 These results indicate that Csp6 may be involved in neuritic remodeling rather than cell death in AD. A proteomic approach revealed that several cytoskeleton or associated proteins involved in learning and memory are substrates of Csp6.7 Therefore, the activation of Csp6 may play an important role in the early phases of AD when cognitive problems are first observed and in the progressive dementia associated with AD. To determine whether Csp6 is activated during the prodromal stages of AD, we immunostained hippocampi from young and old individuals with no cognitive impairment (NCI); mild cognitive impairment (MCI); or mild, moderate, severe, and very severe AD. In many instances, people with a clinical diagnosis of NCI or MCI progress to AD.8,9,10,11,12,13,14 The anti-active p20Csp6 or TauΔCsp6 antisera strongly immunostain the hippocampi at all stages of AD and MCI. Interestingly, anti-p20Csp6 immunostains neurons in some NCI cases, and TauΔCsp6 also immunostains NFTs and NPTs in NCI aged control hippocampi. In contrast, there is no anti-p20Csp6 or TauΔCsp6 immunoreactivity in any of the young hippocampi. We observe an inverse relationship between the level of TauΔCsp6 immunoreactivity and the global cognitive score of aged NCI individuals. We conclude that Csp6 activity precedes the clinical diagnosis of AD and could be an early instigator of neuronal dysfunction in aged individuals.
Materials and Methods
Antibodies and Reagents
The antibody to active Csp6 (p20Csp6) is the 1277 antiserum developed against the p20 subunit C-terminal PLDVVD sequence of human Csp6.5 The TauΔCsp6 antiserum is the 10635 antiserum developed against the C-terminal KSPVVSED epitope generated by cleavage with Csp6.5 The anti-amyloid-β peptide antiserum was generated from rabbits using amyloid-β peptide 1-40 as antigen.2 The PHF-1 antibody was generously provided by Dr. Peter Davies (Department of Neuroscience, Albert Einstein College of Medicine, New York, NY).15 The neuropathologist (S.A.) has extensively used these antibodies for routine diagnosis of AD in autopsied brains, and there is no decrease in antigen recognition for fixation durations of up to 1 year.
Collection of Brain Tissues, Fixation, and Preparation of Slides
Brain tissue was obtained from subjects who participated in the Religious Orders Study (ROS). Details of the clinical evaluation, brain autopsy, and Braak staging have been previously reported.16,17 The Braak staging scores were done by the ROS and were unveiled only after this study was completed. Briefly, more than 1000 older nuns, priests, and brothers agreed to annual detailed clinical evaluation and brain donation at death. The evaluation included a medical history, neuropsychological performance tests, and a clinical evaluation.16 The diagnosis of AD followed the National Institute for Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorder Association criteria. MCI referred to those persons impaired on cognitive testing who did not meet criteria for dementia. NCI referred to persons without cognitive impairment. Each member of the ROS was cognitively assessed using a global cognitive score. In brief, 19 cognitive test scores are converted to z-scores based on the mean and SD of all ROS participants at baseline. The 19 z-scores are averaged to yield a composite measure of global cognition.16 Brains were removed in a standard and uniform fashion at predetermined sites across the country. Tissue blocks from one hemisphere were fixed for 3 to 14 days in 4% paraformaldehyde and paraffin-embedded before sectioning at 4-μm thickness. In addition, hippocampal tissue was harvested from seven young cases, ranging in age from 12 to 22 years, obtained from Baylor College of Medicine (Houston, TX). The mean age of these cases, composed of three females and four males, was 17.28 years. None of these subjects had central nervous system involvement except for one case with Rothia mucilaginosa meningitis. In addition, six male hippocampal tissues aged 20 to 39 years and with no history of neurological diseases were obtained from the Brain and Tissue Bank for Developmental Disorders (University of Maryland, College Park, MD).
Immunostaining of Tissue Sections with TauΔCsp6, PHF-1, and Anti-Aβ
The immunohistochemistry was performed using the Ventana Benchmark Automated Immunostainer (Ventana Medical Systems, Tucson, AZ) as described previously.5 The dilutions for the neoepitope p20Csp6 (1277 antisera), TauΔCsp6 (10635 antisera), PHF-1, and F25276 anti-Aβ antisera2 were 1/2000, 1/16,000, 1/100, and 1/100, respectively. The p20Csp6 antiserum was adsorbed on purified recombinant active Csp6, and TauΔCsp6 antiserum was adsorbed on purified recombinant Tau, generously provided by Dr. Hemant Paudel (Department of Neurology and Neurosurgery, McGill University), cleaved by active Csp6 as described.5 The automated immunostaining allows constant conditions and eliminates the uneven staining that can occur with manual staining.
Assessment of the Immunohistochemical Staining
Scoring was done by the neuropathologist (S.A.) in a blinded manner and as is customary for the diagnosis of AD. The densities of NFTs, NPs, NPTs, and β-amyloid deposits were scored semiquantitatively as absent (0), low/mild (1), moderate (2), or high/severe (3). Scoring diagrams developed by The Consortium to Establish a Registry for Alzheimer’s Disease for assessing AD pathology in autopsy brains were used as guides.18 Alzheimer-type tau pathology (neurofibrillary tangles, neuropil threads, and neuritic plaques) was assessed using conventional well-established neuropathological diagnostic criteria. Flame- or skein-shaped filamentous, tau-immunoreactive inclusions in neuronal cell bodies were considered to represent NFTs, whereas neurons with diffuse or finely granular or diffuse homogeneous perikaryal tau-immunoreactivity were considered to contain pre-tangles. Thin linear tau-immunoreactive profiles in the neuropil were considered to represent NPTs. NPs had an amyloid core surrounded by a halo of radially arranged thickened, beaded tau-immunoreactive neurites. We considered a structure to be tau-immunoreactive if it was decorated with either monoclonal PHF-1 antibody or the 10635 (Csp6-cleaved tau) antiserum. The structures that were decorated only by the 10635 antiserum had the exact same morphology as those that were decorated only by monoclonal PHF-1 antibody or both.
Results
Characterization of the AD, MCI, and NCI Cases Used in This Study
The demographic information of the aged cases is shown in Table 1. The NCI cases were slightly younger but not significantly different from the MCI cases. There was no difference in age between the MCI and AD cases. The mini-mental state examination (MMSE) score was not significantly different between NCI and MCI cases but was much lower in AD cases. Each group had equal numbers of males and females and equivalent levels of education. The AD clinical diagnoses were supported by the Braak staging scores of IV or V, except for one case with an MMSE score of 20 that had a Braak staging score of I (Table 2). The Braak staging scores, measured independently by the ROS, were consistent with the semiquantitative assessment of PHF-1 immunostaining scores in NFTs and NPTs assessed blindly by SA, even in the AD case that had a Braak stage of I. Only 1 of 18 AD cases with a Braak stage of V had lower PHF-1-immunopositive NFTs and NPTs. Anti-Aβ-positive NPs were present at varying levels in all of the AD cases, and the level did not seem to correlate with the severity of AD. However, there was clearly more anti-Aβ immunoreactivity in AD than in MCI and NCI cases, as expected.
Table 1.
Demographics Based on Cognition Status
| NCI | MCI | AD | |
|---|---|---|---|
| N | 6 | 6 | 18 |
| Age at death (years) | 79.50 ± 5.5 | 87.17 ± 7.0 | 88.89 ± 4.2* |
| Education (years) | 19.50 ± 3.1 | 19.83 ± 2.7 | 17.78 ± 4.0 |
| Gender | Three males, three females | Three males, three females | Nine males, nine females |
| MMSE | 28.50 ± 1.1 | 27.20 ± 1.7 | 12.6 ± 8.1* |
| Interval since last exam (days) | 238.80 ± 192.9 | 463.5 ± 539.1 | 246.5 ± 108.4 |
Data represent mean ± SD. Statistically significant differences evaluated by paired t-test of NCI versus MCI or AD.
P < 0.05.
Table 2.
Immunostaining for TauΔCsp6, PHF-1, or Aβ in NCI, MCI, and AD Cases
| Individual | Age at death (years) | Education (years) | Gender | MMSE score | Days since last MMSE at death | Clinical diagnosis | Braak stage score | NFT
|
NPT
|
NP
|
Global cognitive score | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TauΔ-Csp6 | PHF-1 | TauΔ-Csp6 | PHF-1 | Aβ | TauΔ-Csp6 | PHF-1 | |||||||||
| MMSE 0 to 5 AD | |||||||||||||||
| 1 | 89 | 18 | M | 2 | 61 | 4 | V | 3 | 3 | 3 | 3 | 1 | 3 | 1 | −3.66753 |
| 2 | 90 | 11 | F | 0 | 323 | 4 | V | 3 | 3 | 3 | 3 | 1 | 3 | 3 | −3.44916 |
| 3 | 84 | 16 | M | 3 | 29 | 4 | V | 3 | 3 | 3 | 3 | 1 | 3 | 1 | −3.86259 |
| 4 | 90 | 22 | M | 1 | 349 | 4 | IV | 3 | 3 | 3 | 3 | 1 | 3 | 1 to 2 | −4.24437 |
| MMSE 6 to 10 AD | |||||||||||||||
| 1 | 90 | 20 | F | 10 | 331 | 4 | V | 3 | 3 | 3 | 3 | 2 | 3 | 1 | −2.53453 |
| 2 | 95 | 16 | F | 7 | 323 | 4 | V | 3 | 1 | 3 | 1 | 1 | 3 | .5 | −2.38578 |
| 3 | 97 | 16 | F | 9 | 339 | 4 | V | 3 | 3 | 3 | 3 | 1 to 2 | 3 | 3 | −1.49416 |
| 4 | 94 | 16 | F | 7 | 243 | 4 | V | 3 | 4 | 3 | 4 | 4 | 3 | 4 | −2.69227 |
| MMSE 11 to 15 AD | |||||||||||||||
| 1 | 92 | 19 | M | 15 | 202 | 4 | V | 3 | 3 | 3 | 3 | 2 | 3 | 2 | * |
| 2 | 86 | 20 | M | 12 | 145 | 4 | V | 3 | 3 | 3 | 3 | 1 to 2 | 3 | 3 | −2.53204 |
| 3 | 94 | 22 | M | 15 | 265 | 4 | IV | 2 | 3 | 1 to 2 | 3 | 1 | 2 | 1 | −2.95918 |
| MMSE 16 to 20 AD | |||||||||||||||
| 1 | 83 | 16 | F | 16 | 86 | 4 | V | 3 | 3 | 3 | 3 | 1 | 3 | 1 | −1.83198 |
| 2 | 88 | 24 | F | 19 | 211 | 4 | IV | 3 | 3 | 1 to 2 | 3 | 2 | 2 | 1 | −1.19181 |
| 3 | 87 | 8 | M | 20 | 350 | 4 | I | 1 | .5 | 0 to 1 | 0 | 1 | 0 to 1 | 0 | −1.44703 |
| MMSE 21 to 25 AD | |||||||||||||||
| 1 | 84 | 16 | F | 22 | 190 | 4 | V | 3 | 3 | 3 | 3 | 2 | 3 | 3 | −1.53034 |
| 2 | 84 | 22 | F | 24 | 276 | 4 | IV | 3 | 3 | 3 | 3 | 2 | 3 | 2 | −0.97412 |
| 3 | 86 | 20 | M | 21 | 381 | 4 | IV | 3 | 2 to 3 | 3 | 2 to 3 | 1 | 2 | 2 to 3 | −1.26995 |
| 4 | 87 | 18 | M | 24 | 333 | 4 | V | 3 | 3 | 3 | 3 | 1 | 3 | 1 | −1.23048 |
| MMSE 26 to 30 MCI | |||||||||||||||
| 1 | 90 | 20 | F | 26 | 350 | 2 | III | 3 | 3 | 3 | 3 | 0 | 1 to 2 | 1 | −0.8602 |
| 2 | 92 | 19 | F | 29 | 98 | 2 | IV | 3 | 3 | 2 | 3 | 3 | 3 | 3 | −0.43836 |
| 3 | 95 | 25 | F | 28 | 1442 | 2 | II | 2 | 3 | 3 | 3 | 2 | 2 | 1 | −0.39552 |
| 4 | 82 | 18 | M | 29 | 282 | 2 | III | 2 | 3 | 2 | 3 | 0 to 1 | 0 | 1 | −0.45539 |
| 5 | 76 | 16 | M | 26 | 318 | 2 | II | 0 to 1 | 0 | 0 | 0 | 0 | 0 | 0 | −0.62942 |
| 6 | 88 | 21 | M | 25 | 291 | 2 | I | 0 to 1 | 1 | 0 to 1 | 1 | 0 | 0 | 0 | −0.21812 |
| MMSE 26 to 30 NCI | |||||||||||||||
| 1 | 77 | 18 | F | 29 | 186 | 1 | III | 2 to 3 | 1 | 2 to 3 | 1 | 1 | 1 | 0 | −0.07983 |
| 2 | 78 | 18 | F | 29 | 584 | 1 | II | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 0.61261 |
| 3 | 89 | 21 | F | 30 | 289 | 1 | III | 1 | 1 to 2 | 1 | 1 to 2 | 0 | 0 | 0 | 0.5143 |
| 4 | 83 | 16 | M | 28 | 59 | 1 | III | 2 to 3 | 1 | 3 | 1 | 0 | 1 | 0 | −0.61081 |
| 5 | 76 | 25 | M | 28 | 68 | 1 | III | 1 to 2 | 1 to 2 | 2 | 1 to 2 | 0.5 | 1 | 0 | 0.26269 |
| 6 | 74 | 19 | M | 27 | 247 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0.59916 |
A clinical diagnosis of 1 represents NCI, of 2 represents MCI, and of 4 represents AD. AD cases are divided based on MMSE scores as a measure of the severity of the disease. The global cognitive score was assessed as described.17 M, male; F, female.
The global cognitive score of this case was not taken at the time that the MMSE score was 15. Scores taken 3 to 7 years before death indicate declining function.
The MCI cases had more variable Braak staging scores of I to IV, and NCI cases varied from 0 to III. The one Braak stage IV MCI case had high PHF-1 immunoreactivity in NFTs, NPTs, and NPs. There was no correlation between Braak stage levels 0 to III and the level of PFH-1 immunoreactivity in NCI and MCI cases. There was also no correlation with the global cognitive score, as expected because the Braak stage III correlates poorly with cognitive status.17,19 However, there was generally more NFT and NPT PHF-1 immunoreactivity in MCI cases than in NCI cases. Likewise, when present, higher levels of anti-Aβ-immunoreactive NPs were seen in MCI cases than in the NCI cases.
The global cognitive scores were the lowest in AD cases and the highest in NCI cases. Therefore, the clinico-pathological assessment of these AD, MCI, and NCI cases allowed us to determine whether Csp6 activity precedes the clinical and pathological diagnosis of AD.
Tau Cleaved by Csp6 (TauΔCsp6) Immunostaining Is Present in the Hippocampus of Mild, Moderate, Severe, and Very Severe AD
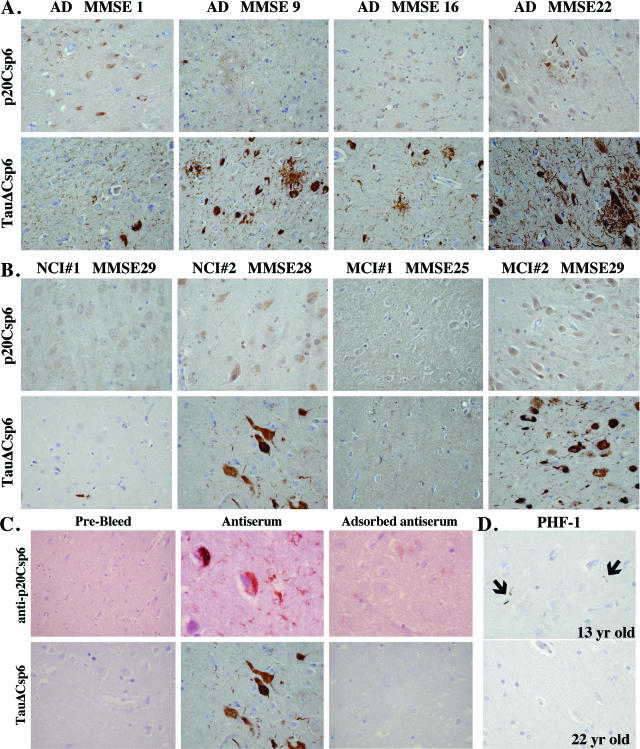
Previously, we have shown active Csp6 in the NPTs, NPs, and NFTs of very severe AD cases.5 Also, we have shown that the Csp6 p20 subunit and TauΔCsp6 are present in pre-tangles, indicating that Csp6 is activated at a very early stage of tangle formation. To determine whether Csp6 is activated in the brains of persons without clinical AD, we immunostained hippocampal formations from young and older individuals with NCI and aged individuals with MCI, in addition to mild, moderate, severe, and very severe AD, with antisera to the p20 subunit of active Csp6 (p20Csp6) or TauΔCsp6. Active Csp6 and TauΔCsp6 both immunostained all AD cases, regardless of the stage of severity (Figure 1A; Table 2). The specificity of both antisera was confirmed by the fact that the pre-bleed antiserum was not immunoreactive to brain tissue, and the immunoreactivity of both antisera was immunoadsorbed on recombinant epitopes (Figure 1C). Active Csp6 immunoreactivity was localized in NFTs, NPTs, and NPs as described previously,5 but it was also present in the cytoplasmic compartment of neurons. TauΔCsp6 was stronger than p20Csp6 immunostaining because Tau protein is both more abundant and more stable than Csp6. Therefore, we conducted our investigations with the TauΔCsp6 antiserum. A semiquantitative assessment of TauΔCsp6 showed strong immunoreactivity in NFTs, NPTs, and NPs of all AD cases regardless of the MMSE, global cognitive, or Braak staging scores with one exception. The AD case with a MMSE score of 20, a global cognitive score of −1.44703, and a Braak stage of I showed low levels of PHF-1, anti-amyloid β peptide (Aβ), and TauΔCsp6 immunoreactivity that was most consistent with the Braak stage of I. Overall, the immunoreactivity of TauΔCsp6 in AD cases was gender independent and did not depend on the levels of education. Together, these data show the presence of Csp6 activity at the very onset of clinically diagnosed AD.
Figure 1.
Active Csp6 and TauΔCsp6 immunostaining in NCI, MCI, and AD hippocampus. Representative micrographs of active Csp6 (p20Csp6) and TauΔCsp6 immunostaining in the hippocampi of NCI, MCI, and AD individuals with varying MMSE scores. A: AD cases at various stages of the disease as indicated by the MMSE score. B: Two NCI and two MCI cases with and without immunoreactivity to the p20Csp6 or TauΔCsp6 antisera. C: Immunohistochemistry of the rabbit pre-bleed and the p20Csp6 and TauΔCsp6 antisera without and with adsorption of the neoepitope. D: PHF-1 immunostaining of 13- and 22-year-old hippocampi. Arrows indicate rare PHF-1 immunoreactive neuropil threads. There was no immunoreactivity with the p20Csp6, anti-Aβ, or TauΔCsp6 antisera.
TauΔCsp6-Immunopositive NFTs Are Present in the Hippocampus of MCI Cases
TauΔCsp6-positive NFTs were present in all MCI cases, TauΔCsp6-positive NPTs were present in five of six MCI cases, and TauΔCsp6-positive NPs were present in three of six cases (Figure 1B; Table 2). Although there was less or no TauΔCsp6 immunoreactivity in two cases with Braak stage I and II, there was one MCI case with a Braak stage of II that had relatively strong TauΔCsp6-immunoreactive NTs, NPTs, and NPs. There was no correlation between Braak staging or the global cognitive scores and the level of TauΔCsp6 in the MCI cases. However, the presence of TauΔCsp6-positive NFTs in all MCI cases showed that Csp6 activity precedes a clinical and pathological diagnosis of AD.
TauΔCsp6-Immunopositive NFTs and NPTs Are Present in the Hippocampus of NCI Cases, and the Level Correlates Inversely with the Global Cognitive Score
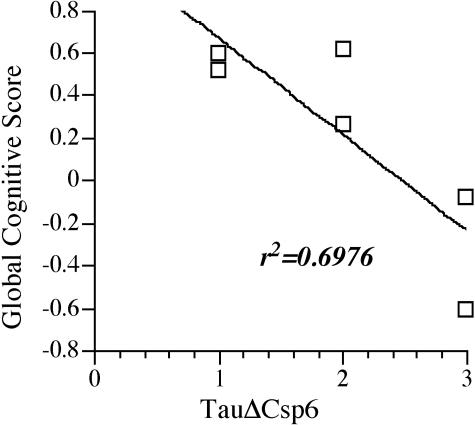
Unexpectedly, TauΔCsp6-immunopositive NFTs and NPTs were present in all NCI cases, and TauΔCsp6-immunopositive NPs were present in three of six cases (Figure 1B; Table 2). As with MCI cases, the level of TauΔCsp6 immunoreactivity in NCI cases did not correlate with the Braak stage score. Interestingly, in these NCI cases, the two cases with the highest levels of TauΔCsp6 (2 to 3) have the most negative global cognitive scores, despite the absence or very low levels (0 or 1) of PHF-1-positive NFTs and NPTs and anti-Aβ-immunopositive NPs. The lowest levels of TauΔCsp6 (0 to 1) occurred in two cases with high global cognitive scores despite one of these cases having level 1 to 2 PHF-1-positive NFTs and NPTs. One case with intermediate levels of TauΔCsp6 (1 to 2) had a lower but positive global cognitive score of 0.26269. The remaining case had also an intermediate level of TauΔCsp6 (2 in NFTs and NPTs) but had a high global cognitive score. This case was unfortunately only examined 584 days before death (1 year and 7 months), so it is unclear whether this person remained cognitively intact at the time of death. The Braak stage of II indicates that the individual did not progress to AD. There was a good correlation (r2 = 0.70) between the level of TauΔCsp6 and the global cognitive score of these individuals (Figure 2).
Figure 2.
TauΔCsp6 levels correlate inversely with global cognitive scores of NCI individuals. The highest level of Tau-positive NFTs and NPTs were plotted against the cognitive score and submitted to linear curve fitting with Delta Graph software (RockWare, Golden, CO). f(x) = −4.510225E−1*x + 1.118400E+0; R2 = 6.976118E−1.
TauΔCsp6 Immunoreactivity Is Absent in 13 Younger Control Cases
Immunostaining of the hippocampi of 13 young individuals failed to reveal any immunoreactivity for TauΔCsp6 or active Csp6 in seven cases of 12 to 22 years of age and six additional cases of 20 to 40 years of age, except for one 33-year-old case, which showed one TauΔCsp6-positive tangle. One 13-year-old hippocampus had three short PHF-1-positive neuropil threads (Figure 1D), and none immunostained with the anti-Aβ antisera.
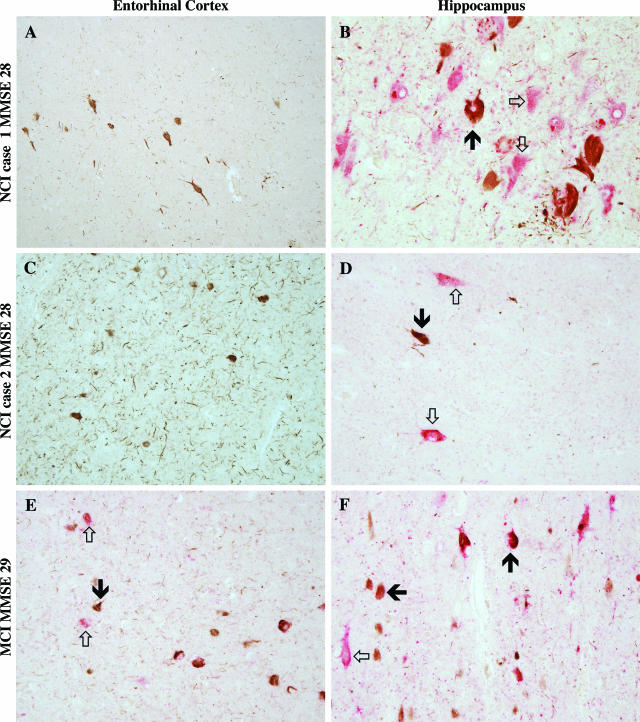
TauΔCsp6 Greatly Exceeds PHF-1 Immunoreactivity in the Entorhinal Cortex
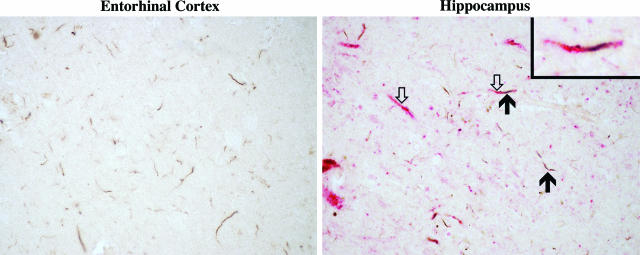
To determine whether active Csp6 is present in the absence of PHF-1 pathology, we performed co-immunostaining of TauΔCsp6 and PHF-1. Of the 12 cases that were clinically either NCI or MCI, nine had only minimal to mild AD pathology essentially restricted to the entorhinal cortex, the transentorhinal cortex, and the hippocampus (especially the CA1). In the three other cases (all categorized as MCI), AD pathology was either moderate or marked, with diffuse hippocampal involvement and involvement of the temporal neocortex. In all cases, pre-tangles (ie, rounded areas of diffuse or finely granular perikaryal tau immunoreactivity) were mostly immunoreactive with PHF-1 or with both PHF-1 and TauΔCsp6 (Figure 3, A–D). There was a strikingly different regional distribution of immunoreactivity of NFTs in the entorhinal cortex on the one hand (Figure 3, A, C, and E) and the hippocampus and transentorhinal cortex on the other hand (Figure 3, B, D, and F). In seven of the nine cases with mild pathology, TauΔCsp6 immunoreactivity in the entorhinal cortex far exceeded that for PHF-1, with four of these seven being completely negative for PHF-1 (Figure 3, A and C). The TauΔCsp6 immunoreactivity was localized in tangle-like structures that appeared to be similar to PHF-1-positive NFTs of AD or in the hippocampus of the NCI and MCI cases. In contrast, all of these cases showed immunoreactivity for both antibodies, with NFTs being decorated by either or both antibodies in the hippocampus and transentorhinal cortex (Figure 3, B and D). In the three cases with moderate to marked AD pathology, one had the same pattern (Figure 3, E and F), whereas the other two had extensive staining with both antibodies in all regions. NPTs had a similar pattern, with predominant or exclusive staining with TauΔCsp6 in the entorhinal cortex and a “mixed” pattern in the other regions (Figure 4). However, there was no correlation between TauΔCsp6 immunoreactivity in absence of PHF-1 immunoreactivity in the entorhinal cortex and either the Braak or global cognitive scores. These results show that the TauΔCsp6 precedes or is present in the absence of PHF-1 Tau in the entorhinal cortex. Overall, the results of these experiments show that Csp6 activity occurs with aging and precedes the clinical diagnosis of AD.
Figure 3.
TauΔCsp6 and PHF-1 co-immunostaining in NCI and MCI cases. Co-immunostaining of TauΔCsp6 (brown) and PHF-1 (red) is shown in entorhinal cortex (A, C, and E) and hippocampus (B, D, and F) of two mild pathological cases labeled NCI (MMSE, 28 in both) (A–D) and one more affected pathological case labeled MCI (MMSE, 29). Solid arrows indicate NFT; open arrows indicate pre-tangles. Original magnification, ×400.
Figure 4.
TauΔCsp6 and PHF-1 co-immunostaining of neuropil threads. Co-immunostaining of TauΔCsp6 (brown) and PHF-1 (red) in neuropil threads in entorhinal cortex and hippocampus (same case as Figure 3, A and B). Solid arrows indicate TauΔCsp6 immunostaining; open arrows indicate PHF-1 immunostaining. Original magnification, ×600. Inset shows a higher magnification of the double-arrowed neuropil thread, which is decorated by both antibodies.
Discussion
In this study, we investigated whether Csp6 is activated in aged individuals with NCI; MCI; or mild, moderate, severe, and very severe AD. We find that active Csp6 is intimately linked to the pathological hallmarks of AD in the hippocampus of persons with all stages of AD. In addition, we find that active Csp6 is associated with AD pathology in several aged cognitively normal (NCI) or mildly affected (MCI) individuals. Interestingly, the active Csp6 is present in the entorhinal cortex of several of the NCI and MCI individuals despite the virtual absence of PHF-1 tau immunopositivity. Furthermore, in NCI individuals, the level of TauΔCsp6 in the hippocampus inversely correlates with the level of cognition. Together, the present results indicate that the active Csp6 occurs before clinical dementia but may influence cognition in the elderly.
We show here that the active Csp6 is present in the hippocampus of very severe, severe, moderate, and mild forms of AD and that it is intimately associated with NPs, NFTs, and NPTs. The level of TauΔCsp6 is similar in the very severe and the milder cases as defined by the MMSE and the global cognitive scores. Therefore, Csp6 activity is not the result of end-point neurodegeneration that arises with time in brains but is present at the very onset of AD. Of the 18 AD cases studied, two cases stand out from the others. One case with an MMSE of 20 and a low global cognitive score indicative of dementia has a Braak staging score of only I and also displays weak immunoreactivity to PHF-1, Aβ, and TauΔCsp6 antisera. This case is likely a non-AD dementia. The other case has a MMSE of 7, a low global cognitive score, a Braak staging score of V, and strong TauΔCsp6-immunopositive NFTs, NPTs, and NPs but low PHF-1-positive pathology. Because the immunostaining was performed on all AD cases together, low levels of PHF-1-positive immunoreactivity are nevertheless detected, and the TauΔCsp6 antiserum strongly immunostains these sections, we can probably exclude antibody or fixation technical problems with these sections. Therefore, in this case, the PHF-1 epitope is much lower compared with the other AD cases. The reason for this is unclear, but sometimes phospho-epitopes of Tau disappear in ghost tangles, which appear with time of disease.21
The MCI and NCI cases have Braak staging scores of I to IV. A Braak stage of I indicates AD pathology in the transentorhinal cortex, which in stage II extends to the entorhinal cortex and the hippocampus.20 At stage III, neocortical association areas are additionally affected, and at stage IV, there is also involvement of the frontal and occipital cortex. The MCI and NCI cases used in this study were classified according to the clinical diagnosis because the Braak staging score does not correlate well with cognitive status in MCI.17,19 It is expected that some MCI and some NCI cases will progress to AD, so it is difficult to draw correlative conclusions from these studies. Nevertheless, TauΔCsp6 is present in NFTs of all MCI and NCI cases investigated but not in normal young and younger adult control brains. These results indicate that active Csp6 precedes AD and remains associated with pathological features of AD. At this time, it is not possible to say whether Csp6 activity leads to AD. In MCI cases, there is no correlation between the level of active Csp6 and the global cognitive score of these individuals. This result indicates that the levels of Csp6 activity do not predict MCI progression to AD. However, it is not possible to exclude the possibility that MCI cases have already advanced to a stage of cognitive deficit due to the activity of Csp6. In NCI cases, which have normal but more variable cognitive scores, the level of TauΔCsp6 is inversely proportional to the global cognitive score (r2 = 0.70). Therefore, it is possible that Csp6 activity is a harbinger of more serious cognitive deficit.
Interestingly, although TauΔCsp6 immunoreactivity overlaps that of PHF-1 Tau in the hippocampus and transentorhinal cortex, it far exceeds PHF-1 Tau pathology in the entorhinal cortex of 7 of 12 of the NCI and MCI cases. Braak staging scores indicate that all of these seven cases have Gallyas-positive pathology in the transentorhinal cortex (appears at stage I), entorhinal cortex, hippocampus (appears at stage II), and neocortex (appears at stage III). PHF-1 antibodies detect hyperphosphorylated Tau at amino acids 396 and 404, and this occurs relatively late compared with the AT8 antiserum against hyperphosphorylated Tau 199 and 202.20,21,22 Therefore, the presence of TauΔCsp6 before PHF-1 immunoreactivity does not exclude the possibility that Tau is hyperphosphorylated at other sites. However, because PHF-1 and TauΔCsp6 immunostaining appear in the entorhinal cortex at all stages of AD, these results indicate that the TauΔCsp6 immunoreactivity in the absence of PHF-1 immunoreactivity is an early event in AD pathology. Braak and Braak23 have noted the first neurofibrillary changes in the layer II of the entorhinal cortex in AD. The entorhinal cortex is affected at a very early stage of AD and even in preclinical AD. In cases evaluated from the ROS cohort, there is a 26% reduction in entorhinal cortex volume in MCI similar to that reported for early (CDR 1) AD that increases to 40% in severe AD.24,25 The reduction of volume is proportional to the severity of the disease as measured by MMSE scores.24 There is a 32% loss of neurons in the entorhinal cortex of individuals with MCI (CDR 0.5) compared with normal controls with as much as a 60% loss in the layer II of the entorhinal cortex of these and the ROS study individuals.26 This loss increases significantly to 90% in AD (CDR 3). There is a reduction of synaptic densities in the molecular layer of the dentate gyrus that is likely a consequence of the reduction of neurons in the entorhinal cortex.27 The presence of active Csp6 in this area before clinical manifestation of disease indicates either that the active Csp6 is involved in the degeneration process or that it is involved in some physiological function. Because active Csp6 is neuritic and not nuclear, we know that in AD, it is not associated with classical neuronal apoptosis.5 However, active Csp6 cleaves many cytoplasmic cytoskeleton and cytoskeleton-associated proteins in neurons.7 Our results show a good correlation between levels of TauΔCsp6 immunoreactivity in NFTs and NPTs and the lowest global cognitive scores in NCI individuals, indicating that the active Csp6 may promote cognitive decline. It is therefore possible that the active Csp6 could be initiated to repair some local damage in the neurites, but without a down-regulation of this activity, active Csp6 would contribute to the demise of the synapses and neuritic cytoskeleton.
Recently, two studies have shown that elimination of the caspase-6 cleavage sites in disease-associated mutant amyloid precursor protein and huntingtin protein abrogates cognitive deficits and synaptic loss, despite normal production of the Aβ in the AD model.28,29 These data indicate that Csp6 cleavage of proteins in AD and Huntington’s disease promotes neurodegeneration by producing small toxic fragments of proteins. Because active Csp6 has a considerable number of protein substrates in neurons,7 it is unlikely that only one of these proteins is the trigger for neurodegeneration when Csp6 is activated. However, these results combined with our findings of active Csp6 at very early stages of AD highlight the importance of finding Csp6 inhibitors as a potential treatment for neurodegeneration.
We conclude from these experiments that the activity of Csp6 precedes the clinical and pathological diagnosis of AD. This raises the possibility that the active Csp6 contributes to the generation of AD pathology because we know that active Csp6 in primary cultures of human neurons increases the production of Aβ1,2 and cleaves Tau protein5 and several cytoskeleton and cytoskeleton-associated proteins involved in maintaining the structure and function of synapses.7 Active Csp6 may contribute significantly to the cognitive impairment of aged, MCI, and AD individuals depending on its level of activation and its location in the brain. Therefore, inhibition of Csp6 may be an early target that could prevent or delay neurodegeneration in AD.
Acknowledgments
We gratefully acknowledge the gift of PHF-1 antibody from Dr. Peter Davies (Albert Einstein College of Medicine).
Footnotes
Address reprint requests to Andréa LeBlanc, Ph.D., The Bloomfield Center for Research in Aging, Lady Davis Institute for Medical Research, The Sir Mortimer B Davis Jewish, General Hospital, 3755 Ch. Côte Ste-Catherine, Montréal, QC, Canada, H3T 1E2. E-mail: andrea.leblanc@mcgill.ca.
Supported by National Institutes of Health grant NS/MH40965, Canadian Institutes of Health Research grant MOP15118, Valorisation-Recherche Québec, and Fonds de Recherche en Santé du Québec (to A.L.B.); National Institute on Aging grants P30-AG10161 and R01-AG15819 (to D.A.B.); and National Institutes of Health grant PO1-AG14449 (to E.J.M.).
References
- LeBlanc AC, Liu H, Goodyer C, Bergeron C, Hammond J. Caspase-6 role in apoptosis of human neurons, amyloidogenesis and Alzheimer’s disease. J Biol Chem. 1999;274:23426–23436. doi: 10.1074/jbc.274.33.23426. [DOI] [PubMed] [Google Scholar]
- LeBlanc A. Increased production of 4 kDa amyloid beta peptide in serum deprived human primary neuron cultures: possible involvement of apoptosis. J Neurosci. 1995;15:7837–7846. doi: 10.1523/JNEUROSCI.15-12-07837.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tesco G, Koh YH, Tanzi RE. Caspase activation increases beta-amyloid generation independently of caspase cleavage of the beta-amyloid precursor protein (APP). J Biol Chem. 2003;278:46074–46080. doi: 10.1074/jbc.M307809200. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Goodyer C, LeBlanc A. Selective and protracted apoptosis in human primary neurons microinjected with active caspase-3, -6, -7, and -8. J Neurosci. 2000;20:8384–8389. doi: 10.1523/JNEUROSCI.20-22-08384.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Albrecht S, Bourdeau M, Petzke T, Bergeron C, LeBlanc AC. Active caspase-6 and caspase-6 cleaved Tau in neuropil threads, neuritic plaques and neurofibrillary tangles of Alzheimer’s disease. Am J Pathol. 2004;165:523–531. doi: 10.1016/S0002-9440(10)63317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruchaud S, Korfali N, Villa P, Kottke TJ, Dingwall C, Kaufmann SH, Earnshaw WC. Caspase-6 gene disruption reveals a requirement for lamin A cleavage in apoptotic chromatin condensation. EMBO J. 2002;21:1967–1977. doi: 10.1093/emboj/21.8.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzke TL, Rousselet E, Goodyer C, LeBlanc AC: Substrates of caspase-6 in human primary neurons: a proteomic study. Program No. 80.9. 2005 Abstract Viewer/Itinerary Planner. Washington, DC: Society for Neuroscience. Online [Google Scholar]
- Hulette CM, Welsh-Bohmer KA, Murray MG, Saunders AM, Mash DC, McIntyre LM. Neuropathological and neuropsychological changes in “normal” aging: evidence for preclinical Alzheimer disease in cognitively normal individuals. J Neuropathol Exp Neurol. 1998;57:1168–1174. doi: 10.1097/00005072-199812000-00009. [DOI] [PubMed] [Google Scholar]
- Davis DG, Schmitt FA, Wekstein DR, Markesbery WR. Alzheimer neuropathologic alterations in aged cognitively normal subjects. J Neuropathol Exp Neurol. 1999;58:376–388. doi: 10.1097/00005072-199904000-00008. [DOI] [PubMed] [Google Scholar]
- Morris JC, Storandt M, Miller JP, McKeel DW, Price JL, Rubin EH, Berg L. Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol. 2001;58:397–405. doi: 10.1001/archneur.58.3.397. [DOI] [PubMed] [Google Scholar]
- Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Lancet. 2001;357:169–175. doi: 10.1016/s0140-6736(00)03589-3. [DOI] [PubMed] [Google Scholar]
- Markesbery WR, Schmitt FA, Kryscio RJ, Davis DG, Smith CD, Wekstein DR. Neuropathologic substrate of mild cognitive impairment. Arch Neurol. 2006;63:38–46. doi: 10.1001/archneur.63.1.38. [DOI] [PubMed] [Google Scholar]
- Morris JC, Storandt M, McKeel DW, Jr, Rubin EH, Price JL, Grant EA, Berg L. Cerebral amyloid deposition and diffuse plaques in “normal” aging: evidence for presymptomatic and very mild Alzheimer’s disease. Neurology. 1996;46:707–719. doi: 10.1212/wnl.46.3.707. [DOI] [PubMed] [Google Scholar]
- Knopman DS, Parisi JE, Salviati A, Floriach-Robert M, Boeve BF, Ivnik RJ, Smith GE, Dickson DW, Johnson KA, Petersen LE, McDonald WC, Braak H, Petersen RC. Neuropathology of cognitively normal elderly. J Neuropathol Exp Neurol. 2003;62:1087–1095. doi: 10.1093/jnen/62.11.1087. [DOI] [PubMed] [Google Scholar]
- Greenberg SG, Davies P, Schein JD, Binder LI. Hydrofluoric acid-treated tau PHF proteins display the same biochemical properties as normal tau. J Biol Chem. 1992;267:564–569. [PubMed] [Google Scholar]
- Bennett DA, Wilson RS, Schneider JA, Evans DA, Beckett LA, Aggarwal NT, Barnes LL, Fox JH, Bach J. Natural history of mild cognitive impairment in older persons. Neurology. 2002;59:198–205. doi: 10.1212/wnl.59.2.198. [DOI] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Bienias JL, Evans DA, Wilson RS. Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology. 2005;64:834–841. doi: 10.1212/01.WNL.0000152982.47274.9E. [DOI] [PubMed] [Google Scholar]
- Mirra SS, Hart MN, Terry RD. Making the diagnosis of Alzheimer’s disease: a primer for practicing pathologists. Arch Pathol Lab Med. 1993;117:132–144. [PubMed] [Google Scholar]
- Gold G, Bouras C, Kovari E, Canuto A, Glaria BG, Malky A, Hof PR, Michel JP, Giannakopoulos P. Clinical validity of Braak neuropathological staging in the oldest-old. Acta Neuropathol (Berl) 2000;99:579–582. doi: 10.1007/s004010051163. discussion 583–574. [DOI] [PubMed] [Google Scholar]
- Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Del Tredici K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol (Berl) 2006;112:389–404. doi: 10.1007/s00401-006-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otvos L, Jr, Feiner L, Lang E, Szendrei GI, Goedert M, Lee VM. Monoclonal antibody PHF-1 recognizes tau protein phosphorylated at serine residues 396 and 404. J Neurosci Res. 1994;39:669–673. doi: 10.1002/jnr.490390607. [DOI] [PubMed] [Google Scholar]
- Su JH, Cummings BJ, Cotman CW. Early phosphorylation of tau in Alzheimer’s disease occurs at Ser-202 and is preferentially located within neurites. Neuroreport. 1994;5:2358–2362. doi: 10.1097/00001756-199411000-00037. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E. Neuropathological staging of Alzheimer-related changes. Acta Neuropathol (Berl) 1991;82:239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- Juottonen K, Laakso MP, Insausti R, Lehtovirta M, Pitkanen A, Partanen K, Soininen H. Volumes of the entorhinal and perirhinal cortices in Alzheimer’s disease. Neurobiol Aging. 1998;19:15–22. doi: 10.1016/s0197-4580(98)00007-4. [DOI] [PubMed] [Google Scholar]
- Kordower JH, Chu Y, Stebbins GT, DeKosky ST, Cochran EJ, Bennett D, Mufson EJ. Loss and atrophy of layer II entorhinal cortex neurons in elderly people with mild cognitive impairment. Ann Neurol. 2001;49:202–213. [PubMed] [Google Scholar]
- Gómez-Isla T, Hollister R, West H, Mui S, Growdon J, Petersen R, Parisi J, Hyman B. Neuronal loss correlated with but exceeds neurofibrillary tangles in Alzheimer’s disease. Ann Neurol. 1997;41:17–24. doi: 10.1002/ana.410410106. [DOI] [PubMed] [Google Scholar]
- Coleman P, Federoff H, Kurlan R. A focus on the synapse for neuroprotection in Alzheimer disease and other dementias. Neurology. 2004;63:1155–1162. doi: 10.1212/01.wnl.0000140626.48118.0a. [DOI] [PubMed] [Google Scholar]
- Galvan V, Gorostiza OF, Banwait S, Ataie M, Logvinova AV, Sitaraman S, Carlson E, Sagi SA, Chevallier N, Jin K, Greenberg DA, Bredesen DE. Reversal of Alzheimer’s-like pathology and behavior in human APP transgenic mice by mutation of Asp664. Proc Natl Acad Sci USA. 2006;103:7130–7135. doi: 10.1073/pnas.0509695103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham RK, Deng Y, Slow EJ, Haigh B, Bissada N, Lu G, Pearson J, Shehadeh J, Bertram L, Murphy Z, Warby SC, Doty CN, Roy S, Wellington CL, Leavitt BR, Raymond LA, Nicholson DW, Hayden MR. Cleavage at the caspase-6 site is required for neuronal dysfunction and degeneration due to mutant huntingtin. Cell. 2006;125:1179–1191. doi: 10.1016/j.cell.2006.04.026. [DOI] [PubMed] [Google Scholar]