Abstract
Autoimmune responses to vimentin occur after solid organ transplantation, but their pathogenic effects are unclear. The aim of these studies was to investigate the effects of vimentin preimmunization on allogeneic and isografted hearts in a murine transplant model. Immunization of C57BL/6 mice with murine vimentin in complete Freund’s adjuvant resulted in anti-vimentin antibodies and vimentin-reactive Th-1 cells. Transplantation of 129/sv hearts into vimentin-immunized C57BL/6 recipients resulted in accelerated rejection (8.4 ± 1.5 days; n = 18), compared with hen egg lysozyme-immunized C57BL/6 (13.3 ± 2.2 days; n = 10; P < 0.0001, log-rank test). In contrast, isografts continued to beat beyond 90 days. Immunohistochemical analysis of allografts from vimentin/complete Freund’s adjuvant mice demonstrated increased numbers of T cells and enhanced microvascular deposition of C3d, CD41, and P-selectin compared with controls. Antibodies were necessary for accelerated rejection, shown by the fact that vimentin-immunized B-cell-deficient IgH6 mice did not show accelerated rejection of 129/sv allografts, but rejection was restored by adoptive transfer of serum containing anti-vimentin antibodies. Eluates from donor hearts placed in vimentin/complete Freund’s adjuvant recipients contained anti-vimentin antibodies, shown by Western blotting. Confocal imaging of rejected hearts demonstrated presence of vimentin and C3d on apoptosed leukocytes, endothelial cells, and platelet/leukocyte conjugates. These results demonstrate that autoantibodies to vimentin, in conjunction with the alloimmune response, have a pathogenic role in allograft rejection.
Cardiac transplantation is a successful operation for patients with end-stage heart disease that is refractory to more conventional therapy. As with other organ transplants, 1-year survival has increased over the years; however, long-term survival has not been impacted to the same degree and remains at 43% at 7 years.1 Cardiac graft vasculopathy characterized by obliterative arteriosclerosis with chronic inflammation, medial necrosis, and intimal thickening is a leading obstacle to long-term graft survival after heart transplantation.2 A similar vascular pathology limits long-term survival of renal allografts.3 Whereas rejection episodes occurring early after transplantation are sensitive to augmented immunosuppression or anti-T-cell therapy, these therapies do not necessarily prevent development of cardiac graft vasculopathy. Often called chronic rejection, this disease has antigen-dependent and antigen-independent components.
An important advance in recent years has been that alloreactive T cells can be activated via two distinct pathways. The first, known as direct recognition, consists of T-cell recognition of intact foreign major histocompatibility complex (MHC) molecules on donor allophycocyanin (APC); the second, known as indirect recognition, occurs when host T cells recognize peptides from the graft that have been processed and presented by host APC.4,5,6 There is good evidence that the indirect pathway is the predominant pathway driving chronic rejection.7,8,9 Although most clinical studies have followed T-cell response to allopeptides derived from donor MHCs, it is clear that the indirect response to minor polymorphic antigens can also cause tissue destruction.10,11 Autoantigens can be added to the list of antigens recognized as part of the alloimmune response. Two lines of evidence demonstrate this to be the case. First, clinical studies show patients make antibodies to tissue-specific antigens such as cardiac myosin,12,13,14 phospholipids,15 ribosomal antigens,16 intercellular adhesion molecule-1,17 and vimentin18 after heart transplantation. Second, experimental studies have demonstrated that allotransplantation breaks tolerance to self-antigens,19 heart transplantation in mice induces cardiac myosin-specific T- and B-cell responses,20 and collagen V is involved in regulating the alloimmune response to lung allografts.21,22,23 Although T-cell responses are initially epitope-specific, determinant spreading is a common feature of a prolonged immune responses, including chronic rejection after heart transplantation24; in this case, determinant spreading included different regions of donor MHC class II peptides. It is clear that in the inflammatory environment of a prolonged immune response to the allograft, which probably includes exposure of neoantigens, autoimmune responses are activated. Experimental studies have demonstrated that autoimmune responses following allotransplantation are not merely bystander effects, but they contribute to tissue destruction processes.20,21,22,23,25 These studies focused on the destructive effects of autoimmune T cells, whether to cardiac myosin,20 collagen V,21,22,23 or skin peptide25; they did not investigate the possible role of tissue-specific autoantibodies in graft destruction.
Vimentin is an intermediate filament characteristic of leukocytes, endothelial cells, and proliferating smooth muscle cells. After cardiac and renal transplantation, patients make an autoimmune response to vimentin, demonstrated by autoantibodies18,26,27 and self-restricted vimentin-specific CD8+ T cells.28 The autoantibody response is associated with development of cardiac graft vasculopathy18 in humans and non-human primates.29 Nonhuman primates with renal allograft also make anti-vimentin antibodies (AVA), but the response is not significantly associated with development of renal graft vasculopathy.30 This is the first study to design experiments to discover whether the autoimmune response to vimentin, and in particular anti-vimentin antibodies, actively contributes to graft rejection. The first part of the study investigated whether it was possible to break self-tolerance to vimentin in mice and, the second part, whether the autoimmune response to vimentin contributed to the pathogenesis of cardiac allograft rejection.
Materials and Methods
Mice
Male C57BL/6 and 129/sv mice, aged 7 to 9 weeks, were purchased from B&K Universal Ltd., Hull, UK. B-cell-knockout mice (IgH6; μMT), generated by targeted disruption of the transmembranous portion of immunoglobulin heavy chain on the C57BL/6 background, were bred at our facility and were used aged 7 to 9 weeks. Mice were housed under optimal conditions and procedures performed under license by the Animals and Scientific Procedures Act (1986).
Recombinant Murine Vimentin
The cDNA for mouse vimentin was isolated from an immortalized mouse endothelial cell line MCEC-131 expression library by polymerase chain reaction, introducing a 5′ NdeI restriction site and a BamHI site at the 3′ end of the cDNA (primers: forward 5′-GAATTCCATATGTCTACCAGGTCTGTG-3′; reverse 5′-AAGCTTGGATCCGTCGACTTTTTATTCAAGGTCATC-3′). The polymerase chain reaction product was subcloned into NdeI/BamHI of pET15b (Novagen, Merck Biosciences, Nottingham, UK), a bacterial expression vector, and transformed into BL21(DE3) Escherichia coli (Novagen). Crude preparations of recombinant mouse vimentin were prepared and extracted according to the pET system manual (Novagen) and purified on a His-Bind resin column under denaturing conditions, using a His-Bind purification kit (Novagen). The purified product was confirmed as being mouse vimentin by both sodium dodecyl sulfate-polyacrylamide gel electrophoresis (a single band at 58 kd was observed) and mass spectrometry.
Immunization Protocol
Recombinant murine vimentin (vim; 400 μg) was emulsified in 100 μl of complete or incomplete Freund’s adjuvant (CFA or IFA) and administered subcutaneously. Seven days later, mice received a booster consisting of 400 μg of vimentin alone. Controls received hen egg lysozyme (hel; 200 μg) in adjuvant, followed by protein alone without adjuvant according to the vimentin protocol. In some mice 100 μl of 6 mol/L urea (vehicle) was substituted for vimentin.
Heterotopic Heart Transplantation
Transplantation was performed according to standard techniques.32 In brief, the donor heart was harvested after heparinization and preserved in saline at 4°C. In the recipient, a midline laparotomy was performed, and the inferior vena cava and aorta were cross-clamped proximal and distal to the anastomotic site after adequate preparation. Donor aorta was anastomosed end-to-side to an aortotomy in the recipient aorta, and donor pulmonary artery was anastomosed to the abdominal inferior vena cava. Release of cross clamps re-established circulation. Postoperatively, the mice were nursed in a warm environment. Survival of recipients after 48 hours was >90%. Grafts were examined by daily palpation; the day of cessation of palpable heartbeat was taken as day of rejection.
Adoptive Transfer of Anti-Vimentin Antibodies
AVA were generated in rabbits (New-Zealand White; Sigma-Aldrich, Poole, Dorset, UK) by immunization with 200 μg of vimentin in CFA (vim/CFA) subcutaneously. Ten days later, the rabbits were bled, and serum was obtained. Serum was filtered through a sterile 0.22-μm filter to remove bacteria (AVA-serum). This was confirmed by enzyme-linked immunosorbent assay (ELISA) to have high titers of AVA [optical density (OD) 1.3 at 1/800 dilution; control preimmune serum OD 0.2]. This was adoptively transferred into IgH6 recipients by injection into the tail vein. Adoptive transfer of 0.5 ml of serum was performed 1 day before transplant, on day of transplant, and 6 days following transplantation. Control IgH6 recipients received equal volumes of filtered preimmunization rabbit serum.
Sample Preparation
Acute rejection was defined as cessation of palpable graft impulse. Animals were sacrificed, serum was obtained, and the heart allograft/isograft was harvested. One-half of this graft was embedded in Optimum-Cutting Tissue Compound (Tissue-Tek; Raymond Lamb, Eastbourne, UK) and frozen, and the other half was placed in 10% formalin. Spleens were collected for ELISPOT assays when required.
ELISA for AVA
Mouse vimentin was plated at 1 μg/well onto 96-well ELISA plates and incubated overnight at 4°C. Nonspecific binding sites on the plates were blocked with phosphate-buffered saline (PBS) with 0.1% Tween 20 and 5% milk (PBSTM) for 2 hours. For each ELISA, standard curves were plotted using doubling dilutions of murine monoclonal IgG anti-vimentin antibodies (clone RV202, 500 μg/ml; BD Biosciences, Oxford, UK) beginning at 1:4000 dilution in PBSTM, and murine monoclonal anti-vimentin IgM antibody (clone Vim13.2, 1.5 mg/ml; Sigma-Aldrich), beginning at 1:40,000 dilution in PBSTM. Both monoclonal antibodies cross-react with murine vimentin. Standards and samples (100 μl, diluted 1/200 for vim/CFA and 1/100 for vim/IFA and controls) were incubated for 1 hour, followed by the appropriate secondary antibody 1 hour (goat anti-mouse IgM or IgG/horseradish peroxidase; Serotec Ltd., Oxford, UK). For determination of Ig subclasses, bovine anti-mouse IgG1 and IgG2a and goat anti-mouse IgG2b and IgG3 were used, all conjugated to horseradish peroxidase (Serotec). Substrate (3,3′,5,5′-tetramethylbenzidene in citrate buffer with 20 μl of hydrogen peroxide) was added, color was developed, and optical densities were read using a dual-wavelength spectrophotometer at 450 nm and 620 nm. Standards were used to determine the titer of the samples. For each ELISA a standard curve was plotted, and the OD readings were read off the standard curves to obtain equivalent titers or units.
ELISPOT Assays
These cytokine assays were performed to determine interferon-γ (IFN-γ), interleukin (IL)-2, IL-4, and IL-5 production by splenocytes when restimulated with vimentin. Splenocytes were suspended in 0.83% ammonium chloride to lyse red blood cells and were washed, counted, and resuspended in medium (RPMI 1640; Sigma-Aldrich) enriched with antibiotics and 10% fetal calf serum to achieve a concentration of 10 × 106 cells/ml. Polyvinylidene difluoride 96-well plates were coated with monoclonal rat anti-mouse (m-RAM) capture antibodies to IFN-γ, IL-2, IL-4, and IL-5 (BD Biosciences, Oxford, UK), and incubated overnight at 4°C. One million splenocytes in 100 μl of RPMI medium were incubated in triplicate with either vimentin at 20 μg/ml, 100 μl of 6 mol/L urea (negative control, vehicle), or concanavalin-A (8 μg/ml, positive control), for 48 hours at 37°C with 5% CO2. Following this, the cells were lysed with distilled water, and plates were incubated with biotinylated m-RAM detection antibodies to IFN-γ, IL-2, IL-4, and IL-5 (BD Biosciences) in 1% BSA for 2 hours. Plates were then incubated with streptavidin-horseradish peroxidase (Vector Laboratories, Peterborough, UK) for 2 hours and developed with 3-amino-9-ethyl-carbazole/N,N-dimethylformamide substrate supplemented with hydrogen peroxide. Spots were developed and counted using an ELISPOT reader and software (AID ELISPOT Reader, AID Software; Autoimmun Diagnostika GmbH, Strassberg, Germany).
Eluting AVA from Heart Grafts
Elution was performed by low-pH treatment as previously described.29 In brief, allografts, isografts and recipient hearts were harvested, snap-frozen in liquid nitrogen, and pulverized. The tissue pellet was washed three times in ice-cold saline, incubated in glycine-HCl buffer, pH 2.7, for 20 minutes at 4°C, centrifuged, and the pH of the supernatant adjusted to 7.5 to obtain eluted antibody. Eluates were stored at −80°C in the presence of protease inhibitors. Eluates from four hearts from each group were pooled for these studies.
Western Blotting
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis provided the separation of proteins according to mass. Murine vimentin (3 μg) and rainbow marker, 5 μl (Amersham Biosciences, Buckinghamshire, UK), were diluted in buffer, heated at 100°C for 5 minutes, and loaded onto the gels. Proteins were separated on 7-cm 10% acrylamide sodium dodecyl sulfate-polyacrylamide gel electrophoresis gels, with 5% acrylamide stacking gel. Proteins were separated at 40 to 50 mA/250 V, until the bromphenol blue tracking dye reached the end of the gel. Proteins were then transferred by Western blotting onto polyvinylidene difluoride membranes (Amersham Biosciences) 200 mA/200 V at 4°C. The polyvinylidene difluoride strips with vimentin and marker were incubated for 12 hours in PBSTM at 4°C to block nonspecific binding sites, then with the eluates or mouse serum (1:10 in PBSTM) for 2.5 hours,29 and finally with the secondary antibody (goat anti-mouse Ig, IgM, or IgG:HRP; Serotec) at 1:2000 in PBSTM for 2 hours. The membranes were developed using enhanced chemiluminescence substrate (Amersham Biosciences) and exposed to X-ray film. The bands were quantified using Quantity One software (Bio-Rad Laboratories, Inc., Hercules, CA) and expressed in OD units. The amount of AVA in hearts was expressed as percentage of the AVA in serum taken at the same time as the hearts (OD % serum). The calculation was OD % serum = (OD pooled hearts/OD pooled serum) × 100.
Immunohistochemistry
Cryostat sections (6 μm) of frozen hearts were prepared and fixed in acetone. Endogenous peroxidase activity was blocked with 0.3% hydrogen peroxide. Sections were incubated with 2% BSA in 0.05% Tween PBS (PBST-BSA) for 30 minutes to block nonspecific binding sites, followed by the primary antibody in PBST-BSA for 1 hour (rat anti-mouse mAb to CD3, CD4, CD8, CD41, and CD62P, 1:25 to 1:50; BD Biosciences). After washing, sections were incubated with secondary antibody in PBS for 1 hour (biotinylated rabbit anti-rat Ig, 1:250; DakoCytomation, Cambridge, UK) and then with avidin-biotin-peroxidase complex (Vector Laboratories, Peterborough, UK) for 1 hour. Sections were visualized with diaminobenzidine substrate supplemented with hydrogen peroxide (Sigma-Aldrich) and counterstained with hematoxylin. When staining for complement C3d, polyclonal rabbit anti-human C3d conjugated with fluorescein isothiocyanate (FITC) was used (DakoCytomation). This antibody cross-reacts with mouse C3d.33 Intensity of FITC staining (for C3d) was quantitated using Lucia-G software (Laboratory Imaging Ltd., Prague, Czech Republic). Ten high power fields/graft and four hearts/group were analyzed, and results were expressed as pixel units. Likewise, for quantification of peroxidase-labeled cells, except in this case, numbers of positive cells/high power fields were counted by two investigators (B.M. and P.S.) blinded to the codes of the experimental groups.
Confocal Image Acquisition
Six-micrometer cryopreserved sections of murine hearts were stained with a combination of monoclonal antibodies (mAbs) and directly conjugated secondary antibodies as follows. To detect endothelial cells, rat anti-mouse CD31 (DakoCytomation) and goat anti-rat Alexa 546 (Invitrogen, Paisley, UK) was used; for vimentin, sheep anti-human vimentin (Affinity Biologicals, Cambridge, UK) and FITC-goat anti-sheep was used; and for C3d, unconjugated rabbit anti-human C3d was used followed by Cascade-Blue goat anti-rabbit (Molecular Probes, Inc, Eugene, OR). To detect activated platelets co-expressing vimentin and C3d, sheep anti-human vimentin (Affinity Biologicals) with goat anti-sheep Alexa 594, rat anti-mouse CD41-FITC (BD Biosciences), and directly conjugated Cascade Blue rabbit anti-human C3d (DakoCytomation) antibody combinations were used. To stain for apoptosing leukocytes co-expressing vimentin and C3d, sheep anti-human vimentin (Affinity Biologicals) with goat anti-sheep Alexa 594, rabbit anti-human C3d (DakoCytomation) and Cascade Blue goat anti-rabbit (Molecular Probes), and directly conjugated rat anti-mouse CD45-APC antibody combinations were used. This was followed by a terminal deoxynucleotidyl transferase dUTP nick-end labeling FITC stain after antibody staining to detect nuclei of apoptosed cells.
Confocal laser scanning image acquisition was performed with a Leica upright SM2 confocal laser scanning microscope (Wetzlar, Germany). Sequential channel scans of each stained section were optimized for maximum signal to noise ratio and minimal laser power output. Consistent pinhole effect (one airy) was maintained for each channel, and each channel consisted of an average of three images. Image analysis and processing was performed with NIH ImageJ software (Bethesda, MD), and only a median matrix filter was used for image processing.
Detection of Donor Reactive Antibody by Flow Cytometry
This was performed to assess presence of donor reactive antibodies in C57BL/6 mice that had been preimmunized with vim/CFA and given 129/sv allografts. Serum was obtained at cessation of palpable allograft impulse. B-cell-depleted splenocytes were incubated with sera at 1:10, 1:20, and 1:50 dilutions for 30 minutes, followed by goat anti-mouse Ig:FITC for 30 minutes. Washed cells were fixed in 0.5% formaldehyde, and 10,000 events examined using flow cytometry (Cytomics FC500). Normal C57BL/6 serum and serum from CBA (H2k) mice immunized with C57BL/6 (H2b) splenocytes were used as negative and positive controls, respectively.
Statistical Analysis
Data were analyzed using independent sample t-tests, and P < 0.05 was considered to represent a significant difference between the two samples/groups. Graft survival data were plotted by the Kaplan-Meier method, using the log-rank test to analyze differences in graft survival between groups, and P < 0.05 was considered to represent a significant difference between the groups.
Results
Breaking Tolerance to Vimentin
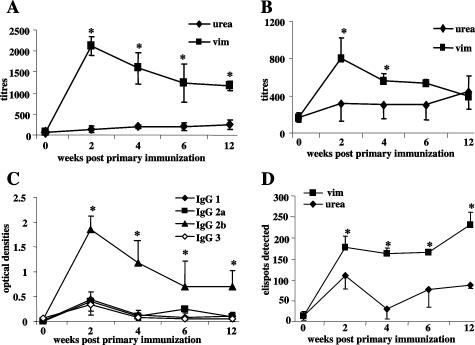
Vimentin-immunized mice had significantly higher IgG AVA titers 2 to 12 weeks after immunization, compared with controls, and the predominant subclass was IgG2b (Figure 1, A–C). Splenocytes from vim/CFA mice produced significantly higher numbers of cells making Th1 cytokines, IFN-γ, IL-2, and IL-4, compared with urea/CFA-immunized controls (Figure 1D, IFN-γ; other cytokines similar to IFN-γ and hence not shown). In contrast, when IFA was used as the adjuvant, vimentin-immunized C57BL/6 produced IgG titers at 2 weeks comparable with vim/CFA mice, but the titers dropped subsequently and were not higher than controls at 4 to 12 weeks (not shown). Cytokine production by splenocytes was no higher in vim/IFA-immunized mice than controls (not shown). Thus, the mycobacterial components in CFA are necessary to break tolerance to mouse vimentin, resulting in a sustained IgG2b and Th1 response.
Figure 1.
Antibody and cytokine production in vimentin-immunized mice. C57BL/6 mice were immunized with 400 μg of vimentin emulsified in CFA followed by a booster of 400 μg of vimentin alone 1 week later. Controls received 100 μl of 6 mol/L urea (vehicle) in CFA. ELISA was used to determine titers of IgG (A) and IgM (B) AVA at 2 to 12 weeks after the first injection. IgG subclasses of AVA were determined in C. Points represent means and standard deviations of four mice per group. *P < 0.05 for differences between vimentin-immunized mice and controls in A and B and for differences between IgG2b titers and other subclasses in C. D: Cytokine production by splenocytes from vimentin-immunized mice assessed by ELISPOT. Spleens from mice immunized with vim/CFA (vim) or urea/CFA (urea) were removed at time 0 and 2 to 12 weeks after the first injection, and splenocytes were prepared and cultured with murine vimentin to determine production of IFN-γ (see Materials and Methods). In brief, 106 splenocytes were cultured with vimentin, urea, or concanalavin-A (not shown) in vitro, in wells coated with mAb to IFN-γ (D). After 48 hours, the cells were lysed with distilled water and ELISPOTs developed using antibodies to appropriate biotinylated mAb. Points represent means and standard deviations of four mice per group. *P < 0.05 for differences between vimentin- or urea-immunized mice.
C57BL/6 Mice Immunized with vim/CFA Show Accelerated Rejection of MHC-Matched 129/sv Allografts
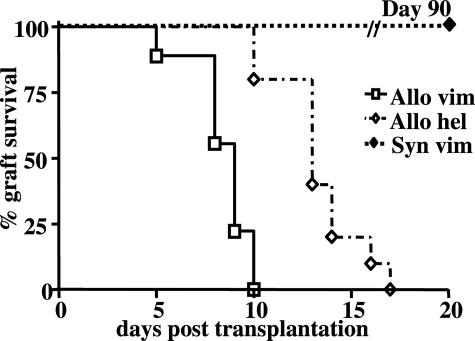
The effect of transplanting allogeneic hearts into mice with an ongoing autoimmune response to vimentin was examined. Hearts from 129/sv donors were transplanted into C57BL/6 recipients. Both belong to the same MHC haplotype H2b, differing in multiple mH alleles. This strain combination was chosen because recipients do not make alloantibodies to donor MHC,34,35 and rejection is slower than a complete MHC mismatch combination (not shown). Recipients were immunized with vim/CFA and received 129 allografts 7 days after the booster injection of vimentin alone. Allografts placed in vim/CFA recipients demonstrated accelerated rejection (8.4 ± 1.5 days; n = 18), compared with controls immunized with hel/CFA (13.3 ± 2.2 days; n = 10; P < 0.0001, log-rank test) (Figure 2). In contrast, isografts placed in vim/CFA-immunized C57BL/6 recipients continued to beat beyond 90 days (n = 11). Unimmunized mice rejected their grafts at day 11.8 ± 1.2 days (n = 9), not significantly different from hel/CFA (not shown).
Figure 2.
Accelerated rejection of cardiac allografts in vimentin-immunized mice. Kaplan-Meier survival graft shows accelerated rejection of 129/sv allografts placed in vim/CFA (Allo vim, n = 18) recipients compared with allografts placed in hel/CFA-immunized (Allo hel, n = 10) recipients (P < 0.0001, log-rank test). Isografts placed in vimentin-immunized C57BL/6 recipients (Syn vim) continued to beat at day 90. Vim/CFA mice were immunized with 400 μg of vimentin in 100 μl of CFA followed by a booster of 400 μg of vimentin alone without adjuvant. The hel/CFA controls received 200 μg of hel in 100 μl of CFA, followed by a booster of 200 μg of hel alone at 1 week. Recipients were transplanted 1 week after administration of booster antigen.
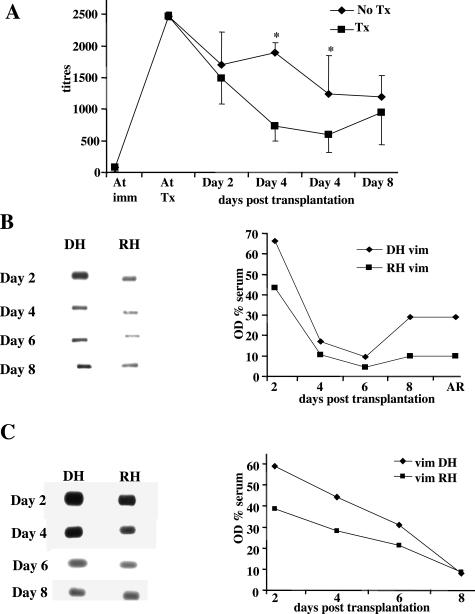
Absence of Alloantibodies and Presence of Anti-Vimentin Antibodies Binding to the Allograft
To ensure that vimentin-immunized recipients were only making AVA and were not making antibodies to other non-HLA cell surface molecules on donor cells, we analyzed binding of sera from vimentin and hel-immunized recipients of 129/sv allografts to 129/sv splenocytes. Serum was taken from recipients at cessation of graft impulse. Flow cytometry revealed complete absence of antibodies binding to 129/sv splenocytes (data not shown). There was a serial decline in serum AVA titers following transplantation compared with vimentin-immunized but nontransplanted controls, possibly reflecting binding of AVA to the allografts (Figure 3A). Experiments were performed to determine the presence of AVA bound within allografts and isografts at days 2 to 8 after transplantation into vim/CFA recipients. Eluates were taken from 129/sv allografts or C57BL/6 isografts and added to polyvinylidene difluoride membranes containing vimentin; binding of AVA to these gels was visualized by probing with horseradish peroxidase-labeled anti-mouse Ig antibodies. The amount of AVA eluted from these hearts was compared with AVA eluted from the recipients’ own (nontransplanted hearts). There was more AVA in both allografts and isografts placed in vim/CFA recipients compared with the recipients’ own hearts at 2 days after transplantation (Figure 3, B and C). Thereafter, the amount of AVA declined in both allogeneic and recipient hearts, but at days 6 to 8, there were increased levels of AVA in the allogeneic compared with recipients’ own hearts. In contrast, in the isografts, there was a steady decline in AVA, which reached the same levels as own hearts at day 8. These results suggest early accumulation of AVA in the newly transplanted heart, whether allografts or isografts, but there was a threefold retention of AVA in the allografts at day 8 and at the time of rejection.
Figure 3.
Levels of AVA in serum, transplanted hearts, and own hearts of vim/CFA-immunized mice. Time course of IgG AVA in serum of C57BL/6 mice immunized with vim/CFA and either receiving a 129/sv cardiac allograft (Tx) or not transplanted (No Tx), mean ± SD from five sera/group (A) (*P < 0.05). Western blot showing the presence of AVA in allografted 129/sv hearts (DH, B) or isografted C57BL/6 hearts (DH, C) placed in C57BL/6 mice immunized with vim/CFA (vim), and recipients’ own hearts (RH), removed at days 2, 4, 6, 8, and time of rejection. The OD % serum on the y axis represents the OD reading of the eluate from pooled hearts (either DH or RH) as a percentage of OD reading from pooled serum taken at the same time as hearts.
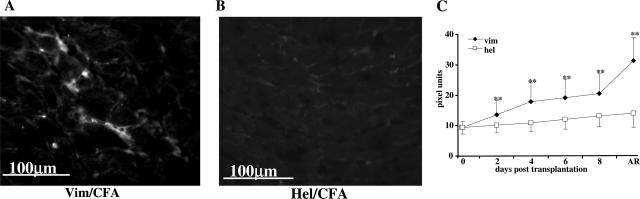
Presence of Increased Complement Deposition in Allografts Placed in vim/CFA-Immunized Recipients
Allografts and isografts were examined for evidence of antibody-mediated damage by examining deposition of complement. Allografts placed in vim/CFA recipients demonstrated significantly greater microvascular deposition of C3d at days 2 to 8 and time of rejection, compared with allografts placed in hel/CFA recipients (Figure 4). Isografts placed in vim/CFA recipients expressed no more C3d than isografts in hel/CFA recipients (not shown). In the absence of alloantibodies and other antibodies to donor splenocytes, this suggests complement fixation by anti-vimentin antibodies. C3d has been validated in animal models as indirect evidence of antibody-mediated damage.33,36
Figure 4.
Deposition of C3d in cardiac allografts. Photomicrograph of frozen section of 129/sv cardiac allograft placed in vim/CFA- (A) or hel/CFA- (B) immunized recipients taken at time of rejection, stained with FITC-conjugated rabbit anti-human C3d. Quantification of C3d deposits at days 2 to 8 and time of acute rejection (AR) revealed more C3d deposition in allografts placed in vimentin-immunized C57BL/6 recipients compared with allografts placed in hel-immunized recipients (C). Quantification is expressed as pixel units on the y axis. **P < 0.05 compared with the preceding time point and compared with hel/CFA recipient.
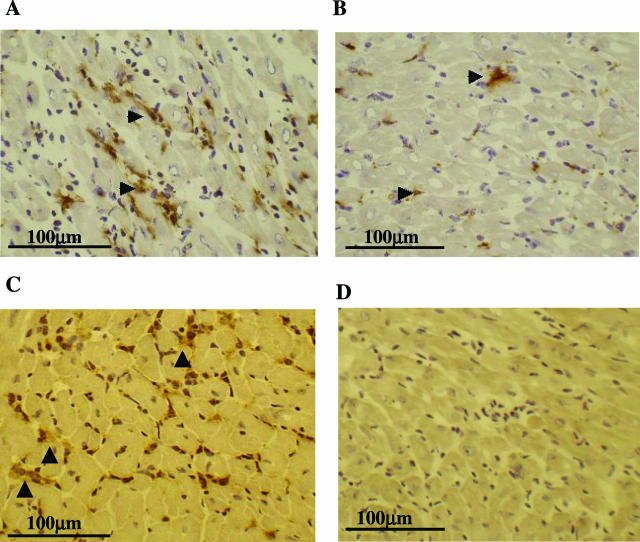
Presence of Infiltrating Cells and Vascular Damage in Allografts Placed in vim/CFA-Immunized Recipients
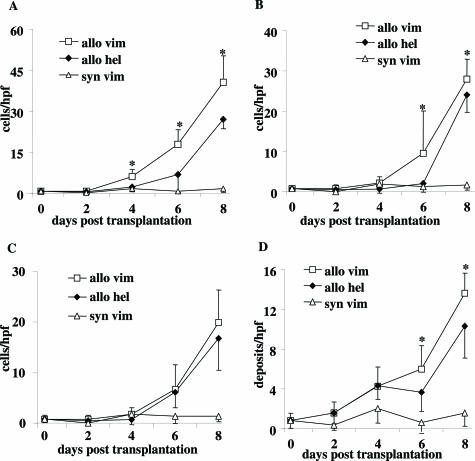
Allografts placed in vim/CFA recipients revealed significantly greater numbers of infiltrating CD3+ and CD4+ T cells, beginning early after implantation, until acute rejection (Figure 5, A and B). There was no difference in CD8+ T cells at day 8 (Figure 5C). There were significantly more CD41+ platelets in hearts from vim/CFA mice than hel/CFA (Figure 5D); immunohistochemistry demonstrated them to be occluding the microvessels of hearts from vim/CFA recipients (Figure 6A). Widespread and strong expression of P-selectin on the microvessels of hearts taken from vimentin-immunized recipients at days 4 and 6, compared with virtually no expression in control hearts (Figure 6, C and D), suggests early activation of endothelial cells of cardiac allografts in vimentin-immunized recipients compared with controls. Thereafter, expression of P-selectin appeared weak and diffuse in both groups (not shown). There was no evidence for an immune response to isografts placed in vim/CFA recipients (Figure 5, A–D). There was no expression of P-selectin in these hearts (not shown).
Figure 5.
Quantification of T cells and CD41 platelets. Quantification of CD3+ (A), CD4+ (B), and CD8+ (C) T cells and CD41+ platelets (D) infiltrating 129/sv allografts in C57BL/6 recipients immunized with vim/CFA (allo vim), hel/CFA (allo hel), or C57BL/6 isografts placed in vim/CFA (syn vim)-immunized mice at various times after transplantation. Results expressed as cells/hpf, mean ± SD (n = 4 mice/group). *P < 0.05 for differences between vim/CFA and hel/CFA controls.
Figure 6.
Demonstration of endothelial cell activation and microvascular damage in cardiac allografts from vim/CFA recipients. Photomicrographs of frozen sections of cardiac allografts from vim/CFA (A and C) or hel/CFA (B and D) recipients stained with mAb to CD41 (A and B) or CD62P (P-selectin, C and D) 6 days after transplantation. Hearts from vim/CFA recipients (C) show extensive microvascular expression of P-selectin compared with hearts from hel/CFA recipients (D). Hearts from mice at day 4 show similar results to day 6 (not shown).
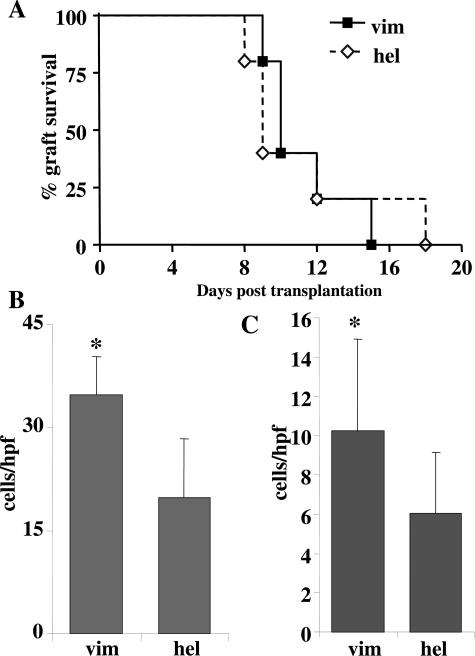
Allografts Placed in Vimentin-Immunized IgH6 Recipients Do Not Undergo Accelerated Allorejection
We next investigated whether vimentin-reactive T cells in the absence of antibodies would be able to mediate accelerated acute rejection of minor mismatched allografts. To this effect, 129/sv cardiac allografts were placed in vim/CFA-immunized B-cell-deficient IgH6 mice. Rejection occurred at 11.2 ± 2.4 days, no different from allografts placed in hel/CFA IgH6 controls (11.2 ± 4.1 days; n = 5; P = 0.99, log-rank test, Figure 7A). At the same time, allografts placed in vim/CFA wild-type C57BL/6 recipients were rejected by 8.8 ± 1.3 days (n = 8; P = 0.0164; log-rank test). As expected, IgH6 recipients did not produce antibodies nor was there any C3d deposited in rejected grafts (not shown). Comparison of numbers of T cells between allografts of vim/CFA and hel/CFA-immunized IgH6 recipients showed that the B-cell-deficient mice had mounted a significant T-cell response to vimentin (Figure 7, B and C), there being significantly more CD3, CD4 (not shown), and CD8+ T cells in grafts of vim/CFA IgH6 mice compared with hel/CFA IgH6 controls. Thus, despite the presence of significantly greater numbers of infiltrating vimentin-reactive T cells in allografts placed in vim/CFA IgH6 recipients, allograft survival was not different from hel/CFA controls. Thus, the absence of accelerated allorejection in allografts placed in vimentin-immunized IgH6 recipients could be due to absence of AVA.
Figure 7.
Rejection of allografts in vim/CFA IgH6 mice. Kaplan-Meier graft survival of 129/sv allografts placed in IgH6 immunized with vim/CFA (vim) or hel/CFA (hel) (A) demonstrates no difference in survival. Quantification of CD3 (B) and CD8 (C) T cells in cardiac allografts from immunized (vim) and hel mice (hel) showed increased CD3 and CD8 T cells in hearts of vim/CFA recipients at time of rejection. Cells expressed as numbers/hpf, mean ±SD (n = 4/group). *P < 0.05 for comparison of vim-immunized and hel-immunized groups.
Adoptive Transfer of AVA Leads to Accelerated Allograft Rejection in IgH6 Recipients
IgH6 mice received 0.5 ml of rabbit anti-mouse vimentin serum at day − 1, day 0, and 6 days after transplantation of 129/sv hearts; control mice received preimmune serum from the same rabbit. Allografts placed in IgH6 mice receiving AVA-serum were rejected at 8.5 ± 2.4 days (n = 4) compared with 12.3 ± 1.3 for those receiving preimmune serum (n = 4; P = 0.009, log-rank test, Figure 8). Allografts from IgH6 recipients of rabbit AVA expressed significantly more C3d than allografts placed in mice receiving preimmune rabbit serum (Figure 8B). Thus, adoptive transfer of anti-vimentin antibodies into IgH6 recipients restored the accelerated rejection of 129/sv allografts seen in vimentin-immunized C57BL/6 recipients.
Figure 8.
Passive transfer (PT) of immunized serum restores accelerated rejection. Kaplan-Meier survival curve of 129/sv allografts placed in IgH6 mice, which received serum from immunized (Vim PT) or unimmunized rabbits (Us PT) (A). Quantification of C3d in hearts at times of rejection is shown in the histogram (B), and the photomicrograph shows immunocytochemical localization of C3d in frozen section of heart placed in vim/CFA recipient at the time of rejection. **P < 0.05 for differences between Vim PT and Us PT.
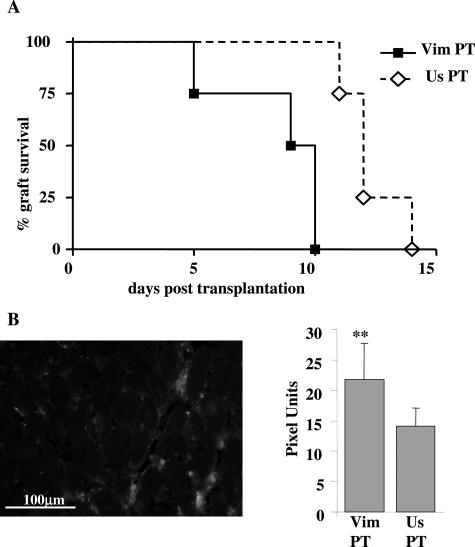
Localization of Vimentin and AVA in Rejected Allografts
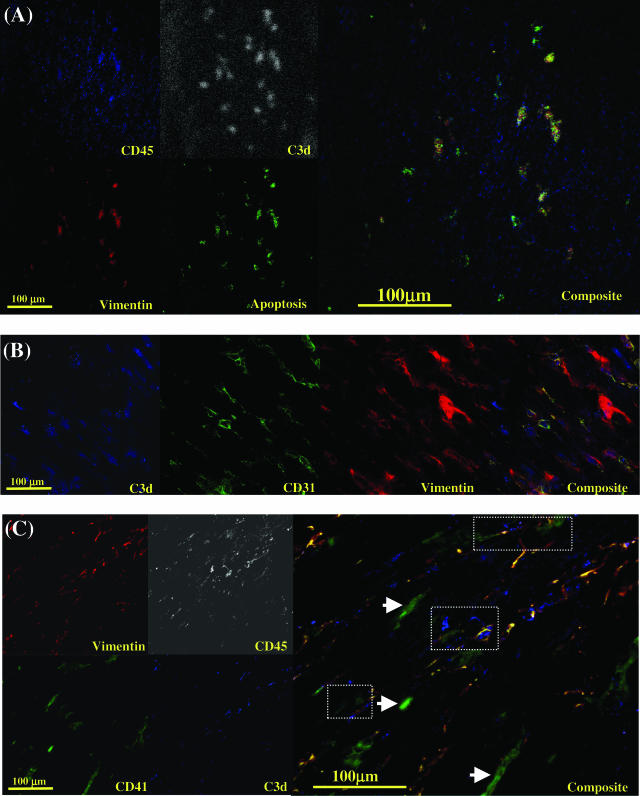
Confocal microscopy of allografts taken at the time of rejection from vim/CFA mice demonstrated extensive expression of vimentin on apoptosing infiltrating leukocytes, which in turn co-localized with C3d deposition (Figure 9A). Vimentin was also shown to be on the surface of CD31-positive endothelial cells not undergoing apoptosis (Figure 9B), and these cells coexpressed C3d. In view of the demonstration that activated platelets express vimentin,37 the presence of vimentin on isolated CD41-positive cells and platelet leukocyte conjugates was examined. As expected, isolated platelets did not express vimentin or C3d (Figure 9C, arrowhead), but platelet-leukocyte conjugates (defined as conjugates of cells expressing both CD41 and CD45) co-localized vimentin and C3d (Figure 9C, circled areas). Z-stacking revealed vimentin expression to be localized to the surface of apoptosing leukocytes, activated endothelial cells, and platelet-leukocyte conjugates (not shown). Confocal microscopy of isografts at day 2 showed a sparse leukocyte infiltrate, some of which were vimentin positive, as well as some vimentin-positive endothelial cells. Isografts at day 90 showed only vimentin-positive endothelial cells; there were no infiltrating leukocytes or platelets in isografts (not shown).
Figure 9.
Confocal laser scanning microscopy of cryostat sections of allografted heart from vimentin-immunized recipient at time of rejection. Antibody combinations are described in Materials and Methods. In A, sections stained for leukocytes (CD45-APC), C3d (Cascade Blue, pseudostained for white to represent the C3d signal), vimentin (Alexa 594), and apoptosis (terminal deoxynucleotidyl transferase dUTP nick-end labeling-FITC). The composite shows co-localization of vimentin and C3d expression on apoptosing infiltrating recipient leukocytes. In B, sections were stained for C3d (Cascade Blue), endothelial cells, CD31 (Alexa 546), and vimentin (Alexa 594). The composite shows co-localization of vimentin and C3d on endothelial cells. In C, sections were stained for vimentin (Alexa 594), leukocytes (CD45-APC, pseudostained for white to represent the CD45 signal), platelets (CD41-FITC), and C3d (Cascade Blue). The composite shows co-localization of vimentin and C3d expression on platelet (CD41+)-leukocyte (CD45+) conjugates (dotted areas). Isolated deposits of vimentin-negative unactivated platelets did not demonstrate C3d staining on their surfaces (arrowheads). Apoptosis was demonstrated by terminal deoxynucleotidyl transferase dUTP nick-end labeling staining.
Discussion
Anti-vimentin antibodies are not only found after heart and renal transplantation18,27,29,30 but are also associated with recognized autoimmune diseases such as rheumatoid arthritis38 and systemic lupus erythematosus.39 It is important to know whether the autoimmune response to vimentin contributes to cardiac allograft rejection. The minor mismatch model, 129/sv into C57BL/6, was chosen because no alloantibodies are produced in this model34,35 and rejection is relatively slow (13.3 ± 2.2 days in irrelevant-protein-immunized recipients) compared with rejection occurring in the presence of a complete MHC mismatch. We first demonstrated that it was possible to break tolerance to mouse vimentin by subcutaneous injection in the presence of complete Freund’s adjuvant. This resulted in a sustained IgG antibody response, predominately IgG2a, and splenocytes producing IFN-γ and IL-2. The IL-4 response was modestly elevated compared with controls, but this is not surprising given what is known about this cytokine being common to both Th1 and Th2 pathways.40 In contrast, immunization of mice with vimentin in incomplete Freund’s adjuvant resulted in a transient antibody response but insignificant production of either Th1 or Th2 cytokines compared with vehicle-immunized controls. Others have also demonstrated that CFA is necessary to generate Th1 cytokines (IFN-γ and IL-2) to autoantigens41,42; unlike these authors, we did not find that vimentin in IFA elicited production of Th2 cytokines.
Transplantation of heart grafts into C57BL/6 mice with a pre-existing autoimmune response to vimentin resulted in accelerated rejection of allografts and no effect on isografts (Figure 2). Although differing only in minor histocompatibility alleles, placement of 129/sv into unimmunized C57BL/6 recipients resulted in a vigorous T-cell response leading to acute rejection. Quantification of T cells showed that the immune response to vimentin resulted in significantly more CD3+ and CD4+ T cells in the allograft at days 4 to 8 after transplantation. Although it is possible that the T-cell response has contributed to accelerated rejection, the more important effector mechanism is likely to be antibodies. Three lines of evidence suggest the importance of anti-vimentin antibodies: presence of C3d in the heart, presence of persistent higher titers of AVA in transplanted hearts, and ability of adoptively transferred serum to restore accelerated rejection in B-cell-deficient mice.
The ability to elute greater amounts of AVA from donor hearts than the recipients’ own hearts, as well as the presence of C3d in allografts placed in vimentin-immunized recipients, suggest that anti-vimentin antibody has bound to the graft and that this antibody has fixed complement. C3a and C5a are highly chemotactic and proinflammatory43,44,45 and are likely to increase adhesion and extravasation of leukocytes into the graft. Restoration of accelerated rejection in IgH6 mice by adoptive transfer of AVA was achieved using rabbit polyclonal immune sera taken at 10 days; at this time the immunoglobulin consists of both IgM and IgG, and it is not possible to say at this stage which antibody subclass causes the damage. IgM is more effective than IgG at fixing complement. We have shown that high titers of IgM AVA in postcardiac transplant patients lead to increased platelet-leukocyte conjugate formation and fragmentation of platelets and leukocytes (H.-S. Leong, B.M. Mahesh, A.D. McCormack, T.J. Podor, M.L. Rose, unpublished data), suggesting that IgM may be the more important immunoglobulin. This is the first direct demonstration that autoantibodies cause accelerated graft rejection; other studies have shown associations between autoantibody production and cardiac allograft rejection,46 but adoptive transfer experiments were not performed.
AVA alone are not sufficient to cause graft rejection. They act in concert with the alloimmune response. In the current study, isografts continued to beat for 90 days in the presence of high titers of IgG AVA brought about by repeated immunization of the recipients with vimentin following transplantation; isografted hearts at the end of this period did not show any evidence of myocyte damage or graft vasculopathy (not shown). In this respect, the autoimmune response to vimentin is different from the responses to myosin and collagen, both of which cause damage to isografted organs.20,21,22,23 This reflects either different effector mechanisms (autoantibody for vimentin versus T cells for myosin and collagen) or different levels of exposure of the autoantigens in allografts and isografts. Immunocytochemical examinations of isografts from days 2 to 8 showed no infiltration or evidence of C3d deposition. Although there was evidence for retention of AVA in isografts at early times after transplantation (Figure 3B), this declined by 8 days. This is unlike AVA retention in allografts, which initially declined but started to rise again after day 6 (Figure 3), reflecting the influx of leukocytes (Figure 5).
Confocal microscopy demonstrated that expression of vimentin differed between isografts and allografts. Vimentin is an intermediate filament found in leukocytes, fibroblasts, endothelial cells, and proliferating smooth muscle cells. Although usually thought of as being a cytosolic protein, it is found on the surface of activated platelets,37 apoptosing neutrophils,47 apoptosing T cells,48 and activated macrophages.49 Caspase-dependent cleavage of vimentin is an essential requirement for apoptosis in many cell types.50 During apoptosis, there is reorganization of intracellular filaments and cytosolic proteins resulting in exposure of neoantigens on the cell surface, many of which have been described as autoantigens.51,52 We hypothesize that transient retention of AVA in isografts, compared with the recipients’ own hearts, may reflect exposure of vimentin on apoptosed cells, presumably caused by reperfusion injury, and this then declines reflecting clearance of apoptosed cells. This hypothesis is supported by confocal examination of isografts at day 2, which showed patchy expression of vimentin-positive leukocytes and endothelial cells. In contrast, confocal microscopy of allografts at time of rejection revealed the presence of large numbers of vimentin-positive apoptotic leukocytes and platelet-leukocyte conjugates co-localizing with areas of C3d deposition. Others have also demonstrated apoptosing leukocytes within the graft during rejection.53,54 At this time, apoptotic endothelial cells were not found in allografts. We propose that apoptotic leukocytes within the graft are the major target for anti-vimentin antibodies; deposition of C3d and other components of complement activation will enhance the inflammatory infiltrate. In addition, the possibility that AVA interact with activated vimentin-expressing platelets, causing them to aggregate in the microcirculation of the graft, is suggested by the confocal images of vimentin-positive, C3d-positive platelet/leukocyte conjugates in the grafts. It is proposed that isografts are not damaged by the anti-vimentin antibodies because they lack large numbers of infiltrating leukocytes and activated platelets, although endothelial cells expressing vimentin were present. In allografts, confocal microscopy revealed extensive expression of vimentin on nonapoptotic endothelial cells, which co-localized with areas of C3d deposition. At this time the role of endothelial cells as targets for AVA and their contribution to accelerated rejection is not clear; more work needs to be done to quantify the numbers of vimentin expressing CD31-positive endothelial cells in allografts and isografts. Experiments are in progress to investigate the effect of chronic production of AVA in a model where acute rejection is attenuated, to see whether they contribute to chronic graft vasculopathy.
In conclusion, it is likely that early non-antigen-dependent damage to the graft, such as ischemia-reperfusion injury, in conjunction with the alloimmune response, sets the scene for an autoimmune response. Although high-affinity autoreactive T cells are eliminated in the thymus, T cells expressing an autoimmune repertoire still escape to the periphery55,56; various mechanisms including peripheral deletion,57 anergy,58 and regulation59 inhibit their activation. These mechanisms fail in an appropriate proinflammatory environment, where the natural process of epitope spreading may allow recognition of neo or cryptic epitopes (eg, on apoptosed cells) derived from the graft. The fact that AVA are characteristic of patients with rheumatoid arthritis and are also found in a mouse model of systemic lupus erythematosus, suggests that vimentin is an abundant or common autoantigen that is exposed as a result of tissue damage and apoptosis. It is likely that dendritic cells, which have receptors for apoptotic cells60 will present vimentin to potentially autoreactive recipient T cells; whether this results in tolerance or T-cell priming depends on a number of factors including the abundance of apoptotic and dying cells as well as the local cytokine milieu.61 Understanding how to limit exposure of vimentin or control activation of vimentin-specific T and B cells may lead to better therapeutic strategies to limit tissue damage in diseases of autoimmunity and transplant rejection.
Acknowledgments
We acknowledge Mihalis Jacovides and Dr. John Smith for technical assistance and advice.
Footnotes
Address reprint requests to Marlene L. Rose, Imperial College, Heart Science Centre, Harefield Hospital, Harefield, UB9 6JH, UK. E-mail: marlene.rose@imperial.ac.uk.
Supported by British Heart Foundation grant RG/2001/005 (to B.M., A.H., and A.M.) and by a British Heart Foundation Traveling Fellowship FS/05/124/19972 (to H.-S.L.).
M.L.R. is employed by Imperial College, which has intellectual property rights regarding “anti-vimentin antibodies” and has a patent on their use as a “marker of rejection.”
References
- Taylor DO, Edwards LB, Boucek MM, Trulock EP, Keck BM, Hertz MI. The Registry of the International Society for Heart and Lung Transplantation: twenty-first official adult heart transplant report–2004. J Heart Lung Transplant. 2004;23:796–803. doi: 10.1016/j.healun.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Ramzy D, Rao V, Brahm J, Miriuka S, Delgado D, Ross HJ. Cardiac allograft vasculopathy: a review. Can J Surg. 2005;48:319–327. [PMC free article] [PubMed] [Google Scholar]
- Chapman JR, O’Connell PJ, Nankivell BJ. Chronic renal allograft dysfunction. J Am Soc Nephrol. 2005;16:3015–3026. doi: 10.1681/ASN.2005050463. [DOI] [PubMed] [Google Scholar]
- Benichou G, Takizawa PA, Olson CA, McMillan M, Sercarz EE. Donor major histocompatibility complex (MHC) peptides are presented by recipient MHC molecules during graft rejection. J Exp Med. 1992;175:305–308. doi: 10.1084/jem.175.1.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornick P, Lechler R. Direct and indirect pathways of alloantigen recognition: relevance to acute and chronic allograft rejection. Nephrol Dial Transplant. 1997;12:1806–1810. doi: 10.1093/ndt/12.9.1806. [DOI] [PubMed] [Google Scholar]
- Watschinger B, Gallon L, Carpenter CB, Sayegh MH. Mechanisms of allo-recognition: recognition by in vivo-primed T cells of specific major histocompatibility complex polymorphisms presented as peptides by responder antigen-presenting cells. Transplantation. 1994;57:572–576. [PubMed] [Google Scholar]
- Baker RJ, Hernandez-Fuentes MP, Brookes PA, Chaudhry AN, Cook HT, Lechler RI. Loss of direct and maintenance of indirect alloresponses in renal allograft recipients: implications for the pathogenesis of chronic allograft nephropathy. J Immunol. 2001;167:7199–7206. doi: 10.4049/jimmunol.167.12.7199. [DOI] [PubMed] [Google Scholar]
- Hornick PI, Mason PD, Yacoub MH, Rose ML, Batchelor R, Lechler RI. Assessment of the contribution that direct allorecognition makes to the progression of chronic cardiac transplant rejection in humans. Circulation. 1998;97:1257–1263. doi: 10.1161/01.cir.97.13.1257. [DOI] [PubMed] [Google Scholar]
- Hornick PI, Mason PD, Baker RJ, Hernandez-Fuentes M, Frasca L, Lombardi G, Taylor K, Weng L, Rose ML, Yacoub MH, Batchelor R, Lechler RI. Significant frequencies of T cells with indirect anti-donor specificity in heart graft recipients with chronic rejection. Circulation. 2000;101:2405–2410. doi: 10.1161/01.cir.101.20.2405. [DOI] [PubMed] [Google Scholar]
- Simpson E, Roopenian D, Goulmy E. Much ado about minor histocompatibility antigens. Immunol Today. 1998;19:108–112. doi: 10.1016/s0167-5699(97)01213-9. [DOI] [PubMed] [Google Scholar]
- Chen Y, Demir Y, Valujskikh A, Heeger PS. The male minor transplantation antigen preferentially activates recipient CD4+ T cells through the indirect presentation pathway in vivo. J Immunol. 2003;171:6510–6518. doi: 10.4049/jimmunol.171.12.6510. [DOI] [PubMed] [Google Scholar]
- Dunn MJ, Rose ML, Latif N, Bradd S, Lovegrove C, Seymour C, Pomerance A, Yacoub MH. Demonstration by western blotting of antiheart antibodies before and after cardiac transplantation. Transplantation. 1991;51:806–812. doi: 10.1097/00007890-199104000-00014. [DOI] [PubMed] [Google Scholar]
- Warraich RS, Pomerance A, Stanley A, Banner NR, Dunn MJ, Yacoub MH. Cardiac myosin autoantibodies and acute rejection after heart transplantation in patients with dilated cardiomyopathy. Transplantation. 2000;69:1609–1617. doi: 10.1097/00007890-200004270-00015. [DOI] [PubMed] [Google Scholar]
- Morgun A, Shulzhenko N, Unterkircher CS, Diniz RV, Pereira AB, Silva MS, Nishida SK, Almeida DR, Carvalho AC, Franco M, Souza MM, Gerbase-DeLima M. Pre- and post-transplant anti-myosin and anti-heat shock protein antibodies and cardiac transplant outcome. J Heart Lung Transplant. 2004;23:204–209. doi: 10.1016/S1053-2498(03)00114-1. [DOI] [PubMed] [Google Scholar]
- Laguens RP, Argel MI, Chambo JG, Vigliano CA, San Martino JA, Perrone SV, Favaloro RR. Anti-skeletal muscle glycolipid antibodies in human heart transplantation as markers of acute rejection. Correlation with endomyocardial biopsy. Transplantation. 1996;62:211–216. doi: 10.1097/00007890-199607270-00011. [DOI] [PubMed] [Google Scholar]
- Linke AT, Marchant B, Marsh P, Frampton G, Murphy J, Rose ML. Screening of a HUVEC cDNA library with transplant-associated coronary artery disease sera identifies RPL7 as a candidate autoantigen associated with this disease. Clin Exp Immunol. 2001;126:173–179. doi: 10.1046/j.1365-2249.2001.01654.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson C, Holder AL, Stanford RE, Smith J, Rose ML. Anti-intercellular adhesion molecule-1 antibodies in sera of heart transplant recipients: a role in endothelial cell activation. Transplantation. 2005;80:264–271. doi: 10.1097/01.tp.0000165433.88295.4c. [DOI] [PubMed] [Google Scholar]
- Jurcevic S, Ainsworth ME, Pomerance A, Smith JD, Robinson DR, Dunn MJ, Yacoub MH, Rose ML. Antivimentin antibodies are an independent predictor of transplant-associated coronary artery disease after cardiac transplantation. Transplantation. 2001;71:886–892. doi: 10.1097/00007890-200104150-00011. [DOI] [PubMed] [Google Scholar]
- Fedoseyeva EV, Tam RC, Popov IA, Orr PL, Garovoy MR, Benichou G. Induction of T cell responses to a self-antigen following allotransplantation. Transplantation. 1996;61:679–683. doi: 10.1097/00007890-199603150-00001. [DOI] [PubMed] [Google Scholar]
- Fedoseyeva EV, Zhang F, Orr PL, Levin D, Buncke HJ, Benichou G. De novo autoimmunity to cardiac myosin after heart transplantation and its contribution to the rejection process. J Immunol. 1999;162:6836–6842. [PubMed] [Google Scholar]
- Haque MA, Mizobuchi T, Yasufuku K, Fujisawa T, Brutkiewicz RR, Zheng Y, Woods K, Smith GN, Cummings OW, Heidler KM, Blum JS, Wilkes DS. Evidence for immune responses to a self-antigen in lung transplantation: role of type V collagen-specific T cells in the pathogenesis of lung allograft rejection. J Immunol. 2002;169:1542–1549. doi: 10.4049/jimmunol.169.3.1542. [DOI] [PubMed] [Google Scholar]
- Yasufuku K, Heidler KM, O’Donnell PW, Smith Jr GN, Cummings OW, Foresman BH, Fujisawa T, Wilkes DS. Oral tolerance induction by type V collagen downregulates lung allograft rejection. Am J Respir Cell Mol Biol. 2001;25:26–34. doi: 10.1165/ajrcmb.25.1.4431. [DOI] [PubMed] [Google Scholar]
- Yasufuku K, Heidler KM, Woods KA, Smith GN, Jr, Cummings OW, Fujisawa T, Wilkes DS. Prevention of bronchiolitis obliterans in rat lung allografts by type V collagen-induced oral tolerance. Transplantation. 2002;73:500–505. doi: 10.1097/00007890-200202270-00002. [DOI] [PubMed] [Google Scholar]
- Liu Z, Colovai AI, Tugulea S, Reed EF, Fisher PE, Mancini D, Rose EA, Cortesini R, Michler RE, Suciu-Foca N. Indirect recognition of donor HLA-DR peptides in organ allograft rejection. J Clin Invest. 1996;98:1150–1157. doi: 10.1172/JCI118898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valujskikh A, Fedoseyeva E, Benichou G, Heeger PS. Development of autoimmunity after skin graft rejection via an indirect alloresponse. Transplantation. 2002;73:1130–1137. doi: 10.1097/00007890-200204150-00021. [DOI] [PubMed] [Google Scholar]
- Wheeler CH, Collins A, Dunn MJ, Crisp SJ, Yacoub MH, Rose ML. Characterization of endothelial antigens associated with transplant-associated coronary artery disease. J Heart Lung Transplant. 1995;14:S188–S197. [PubMed] [Google Scholar]
- Carter V, Shenton BK, Jaques B, Turner D, Talbot D, Gupta A, Chapman CE, Matthews CJ, Cavanagh G. Vimentin antibodies: a non-HLA antibody as a potential risk factor in renal transplantation. Transplant Proc. 2005;37:654–657. doi: 10.1016/j.transproceed.2004.12.043. [DOI] [PubMed] [Google Scholar]
- Barber LD, Whitelegg A, Madrigal JA, Banner NR, Rose ML. Detection of vimentin-specific autoreactive CD8+ T cells in cardiac transplant patients. Transplantation. 2004;77:1604–1609. doi: 10.1097/01.tp.0000129068.03900.25. [DOI] [PubMed] [Google Scholar]
- Azimzadeh AM, Pfeiffer S, Wu GS, Schroder C, Zhou H, Zorn GL, 3rd, Kehry M, Miller GG, Rose ML, Pierson RN., 3rd humoral immunity to vimentin is associated with cardiac allograft injury in nonhuman primates. Am J Transplant. 2005;5:2349–2359. doi: 10.1111/j.1600-6143.2005.01022.x. [DOI] [PubMed] [Google Scholar]
- Jonker M, Danskine A, Haanstra K, Wubben J, Kondova I, Kuhn EM, Rose M. The autoimmune response to vimentin after renal transplantation in nonhuman primates is immunosuppression dependent. Transplantation. 2005;80:385–393. doi: 10.1097/01.tp.0000166920.18998.15. [DOI] [PubMed] [Google Scholar]
- Lidington EA, Rao RM, Marelli-Berg FM, Jat PS, Haskard DO, Mason JC. Conditional immortalization of growth factor-responsive cardiac endothelial cells from H-2K(b)-tsA58 mice. Am J Physiol Cell Physiol. 2002;282:C67–C74. doi: 10.1152/ajpcell.2002.282.1.C67. [DOI] [PubMed] [Google Scholar]
- Corry RJ, Winn HJ, Russell PS. Primarily vascularized allografts of hearts in mice: the role of H-2D, H-2K, and non-H-2 antigens in rejection. Transplantation. 1973;16:343–350. doi: 10.1097/00007890-197310000-00010. [DOI] [PubMed] [Google Scholar]
- Rahimi S, Qian Z, Layton J, Fox-Talbot K, Baldwin WM, Wasowska BA. Non-complement- and complement-activating antibodies synergize to cause rejection of cardiac allografts. Am J Transplant. 2004;4:326–334. doi: 10.1111/j.1600-6143.2004.00334.x. [DOI] [PubMed] [Google Scholar]
- Russell PS, Chase CM, Winn HJ, Colvin RB. Coronary atherosclerosis in transplanted mouse hearts. II. Importance of humoral immunity. J Immunol. 1994;152:5135–5141. [PubMed] [Google Scholar]
- Russell PS, Chase CM, Colvin RB. Alloantibody- and T cell-mediated immunity in the pathogenesis of transplant arteriosclerosis: lack of progression to sclerotic lesions in B cell-deficient mice. Transplantation. 1997;64:1531–1536. doi: 10.1097/00007890-199712150-00005. [DOI] [PubMed] [Google Scholar]
- Wasowska BA, Qian Z, Cangello DL, Behrens E, Van Tran K, Layton J, Sanfilippo F, Baldwin WM., III Passive transfer of alloantibodies restores acute cardiac rejection in IgKO mice. Transplantation. 2001;71:727–736. doi: 10.1097/00007890-200103270-00007. [DOI] [PubMed] [Google Scholar]
- Podor TJ, Singh D, Chindemi P, Foulon DM, McKelvie R, Weitz JI, Austin R, Boudreau G, Davies R. Vimentin exposed on activated platelets and platelet microparticles localizes vitronectin and plasminogen activator inhibitor complexes on their surface. J Biol Chem. 2002;277:7529–7539. doi: 10.1074/jbc.M109675200. [DOI] [PubMed] [Google Scholar]
- Vossenaar ER, Despres N, Lapointe E, van der Heijden A, Lora M, Senshu T, van Venrooij WJ, Menard HA. Rheumatoid arthritis specific anti-Sa antibodies target citrullinated vimentin. Arthritis Res Ther. 2004;6:R142–R150. doi: 10.1186/ar1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thébault S, Gilbert D, Hubert M, Drouot L, Machour N, Lange C, Charlionet R, Tron F. Orderly pattern of development of the autoantibody response in (New Zealand White x BXSB)F1 lupus mice: characterization of target antigens and antigen spreading by two-dimensional gel electrophoresis and mass spectrometry. J Immunol. 2002;169:4046–4053. doi: 10.4049/jimmunol.169.7.4046. [DOI] [PubMed] [Google Scholar]
- Yip HC, Karulin AY, Tary-Lehmann M, Hesse MD, Radeke H, Heeger PS, Trezza RP, Heinzel FP, Forsthuber T, Lehmann PV. Adjuvant-guided type-1 and type-2 immunity: infectious/noninfectious dichotomy defines the class of response. J Immunol. 1999;162:3942–3949. [PubMed] [Google Scholar]
- Fedoseyeva EV, Kishimoto K, Rolls HK, Illigens BM, Dong VM, Valujskikh A, Heeger PS, Sayegh MH, Benichou G. Modulation of tissue-specific immune response to cardiac myosin can prolong survival of allogeneic heart transplants. J Immunol. 2002;169:1168–1174. doi: 10.4049/jimmunol.169.3.1168. [DOI] [PubMed] [Google Scholar]
- Heeger PS, Forsthuber T, Shive C, Biekert E, Genain C, Hofstetter HH, Karulin A, Lehmann PV. Revisiting tolerance induced by autoantigen in incomplete Freund’s adjuvant. J Immunol. 2000;164:5771–5781. doi: 10.4049/jimmunol.164.11.5771. [DOI] [PubMed] [Google Scholar]
- Baldwin WM, Kasper EK, Zachary AA, Wasowska BA, Rodriguez ER. Beyond c4d: other complement-related diagnostic approaches to antibody-mediated rejection. Am J Transplant. 2004;4:311–318. doi: 10.1111/j.1600-6143.2004.00348.x. [DOI] [PubMed] [Google Scholar]
- Baldwin WM, III, Qian Z, Wasowska B, Sanfilippo F. Complement causes allograft injury by cell activation rather than lysis. Transplantation. 1999;67:1498–1499. doi: 10.1097/00007890-199906150-00023. [DOI] [PubMed] [Google Scholar]
- Baldwin WM, III, Qian Z, Ota H, Samaniego M, Wasowska B, Sanfilippo F, Hruban RH. Complement as a mediator of vascular inflammation and activation in allografts. J Heart Lung Transplant. 2000;19:723–730. doi: 10.1016/s1053-2498(00)00137-6. [DOI] [PubMed] [Google Scholar]
- Tanaka M. Progression of alloresponse and tissue-specific immunity during graft coronary artery disease. Am J Transplant. 2005;5:1286–1296. doi: 10.1111/j.1600-6143.2005.00880.x. [DOI] [PubMed] [Google Scholar]
- Moisan E, Girard D. Cell surface expression of intermediate filament proteins vimentin and lamin B1 in human neutrophil spontaneous apoptosis. J Leukoc Biol. 2006;79:489–498. doi: 10.1189/jlb.0405190. [DOI] [PubMed] [Google Scholar]
- Boilard E, Bourgoin SG, Bernatchez C, Surette ME. Identification of an autoantigen on the surface of apoptotic human T cells as a new protein interacting with inflammatory group IIA phospholipase A2. Blood. 2003;102:2901–2909. doi: 10.1182/blood-2002-12-3702. [DOI] [PubMed] [Google Scholar]
- Mor-Vaknin N, Punturieri A, Sitwala K, Markovitz DM. Vimentin is secreted by activated macrophages. Nat Cell Biol. 2003;5:59–63. doi: 10.1038/ncb898. [DOI] [PubMed] [Google Scholar]
- Nakanishi K, Maruyama M, Shibata T, Morishima N. Identification of a caspase-9 substrate and detection of its cleavage in programmed cell death during mouse development. J Biol Chem. 2001;276:41237–41244. doi: 10.1074/jbc.M105648200. [DOI] [PubMed] [Google Scholar]
- Casciola-Rosen LA, Anhalt G, Rosen A. Autoantigens targeted in systemic lupus erythematosus are clustered in two populations of surface structures on apoptotic keratinocytes. J Exp Med. 1994;179:1317–1330. doi: 10.1084/jem.179.4.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney JA, Rosen A. Apoptosis and autoimmunity. Curr Opin Immunol. 2005;17:583–588. doi: 10.1016/j.coi.2005.09.018. [DOI] [PubMed] [Google Scholar]
- Oh SI, Kim IW, Jung HC, Seo JW, Chae IH, Kim HS, Oh BH. Correlation of Fas and Fas ligand expression with rejection status of transplanted heart in human. Transplantation. 2001;71:906–909. doi: 10.1097/00007890-200104150-00015. [DOI] [PubMed] [Google Scholar]
- Shulzhenko N, Morgun A, Zheng XX, Diniz RV, Almeida DR, Ma N, Strom TB, Gerbase-DeLima M. Intragraft activation of genes encoding cytotoxic T lymphocyte effector molecules precedes the histological evidence of rejection in human cardiac transplantation. Transplantation. 2001;72:1705–1708. doi: 10.1097/00007890-200111270-00025. [DOI] [PubMed] [Google Scholar]
- Lehmann PV, Targoni OS, Forsthuber TG. Shifting T-cell activation thresholds in autoimmunity and determinant spreading. Immunol Rev. 1998;164:53–61. doi: 10.1111/j.1600-065x.1998.tb01207.x. [DOI] [PubMed] [Google Scholar]
- Targoni OS, Lehmann PV. Endogenous myelin basic protein inactivates the high avidity T cell repertoire. J Exp Med. 1998;187:2055–2063. doi: 10.1084/jem.187.12.2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JF, Morahan G. Peripheral T cell tolerance. Annu Rev Immunol. 1992;10:51–69. doi: 10.1146/annurev.iy.10.040192.000411. [DOI] [PubMed] [Google Scholar]
- Rocha B, Grandien A, Freitas AA. Anergy and exhaustion are independent mechanisms of peripheral T cell tolerance. J Exp Med. 1995;181:993–1003. doi: 10.1084/jem.181.3.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevach EM. Regulatory T cells in autoimmmunity. Annu Rev Immunol. 2000;18:423–449. doi: 10.1146/annurev.immunol.18.1.423. [DOI] [PubMed] [Google Scholar]
- Albert ML, Sauter B, Bhardwaj N. Dendritic cells acquire antigen from apoptotic cells and induce class I-restricted CTLs. Nature. 1998;392:86–89. doi: 10.1038/32183. [DOI] [PubMed] [Google Scholar]
- Viorritto IC, Nikolov NP, Siegel RM. Autoimmunity versus tolerance: can dying cells tip the balance? Clin Immunol. 2007;122:125–134. doi: 10.1016/j.clim.2006.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]