Abstract
BACKGROUND
Despite uncertain benefit, many women over age 80 (oldest-old) receive screening mammography.
OBJECTIVE
To explore decision-making and physician counseling of oldest-old women around mammography screening.
DESIGN
Qualitative research using in-depth semi-structured interviews.
PARTICIPANTS
Twenty-three women aged 80 or older who received care at a large academic primary care practice (13 had undergone mammography screening in the past 2 years) and 16 physicians at the same center.
APPROACH
We asked patients and physicians to describe factors influencing mammography screening decisions of oldest-old women. We asked physicians to describe their counseling about screening to the oldest-old.
RESULTS
Patients and/or physicians identified the importance of physician influence, patient preferences, system factors, and social influences on screening decisions. Although physicians felt that patient's health affected screening decisions, few patients felt that health mattered. Three types of elderly patients were identified: (1) women enthusiastic about screening mammography; (2) women opposed to screening mammography; and (3) women without a preference who followed their physician's recommendation. However, physician counseling about mammography screening to elderly women varies; some individualize discussions; others encourage screening; few discourage screening. Physicians report that discussions about stopping screening can be uncomfortable and time consuming. Physicians suggest that more data could facilitate these discussions.
CONCLUSIONS
Some oldest-old women have strong opinions about screening mammography while others are influenced by physicians. Discussions about stopping screening are challenging for physicians. More data about the benefits and risks of mammography screening for women aged 80 or older could inform patients and improve provider counseling to lead to more rational use of mammography.
Keywords: mammography, elderly, women, screening, decision-making
In 2000, 51% of the estimated 3.8 million community-dwelling women aged 80 and older residing in the United States had received breast cancer screening with mammography in the previous 2 years. Even among the 1.3 million oldest-old women with probable life expectancies of less than 5 years, 39% received screening mammograms despite little chance of benefit. Screening mammography has increased among elderly women since Medicare first began paying for them in 1991.1,2 As the randomized mammography trials did not include women over age 743–7 it remains unknown whether there is any survival benefit associated with mammography screening for many elderly women. Two observational studies suggested a potential survival benefit for women aged 80 or older. However, neither could adequately adjust for lead-time bias.8,9 Most cost-effective analyses have found that the positive effects of screening balance with the negative effects of screening around 80 years of age.10–13
The uncertainty of benefit of mammography screening for women aged 80 or older is reflected in guidelines, which vary among the major professional organizations.14–16 Most guidelines do not give an absolute age to stop screening older women with mammography but do encourage physicians to consider a patient's life expectancy.14–18 The benefits of screening women aged 80 or older may include increased longevity and decreased morbidity caused by metastases from advanced breast cancers.9,17 However, risks include: anxiety related to “false-positive” mammograms; complications from follow-up procedures; finding breast cancers that might never have become clinically significant during a patient's lifetime; and morbidity associated with treating breast cancer among frail elderly women.19 In the absence of clear clinical evidence and uncertain ratio of risks to benefits, physicians are faced with the difficult decision of whether to recommend mammography screening to women aged 80 and older (oldest-old) and these patients are faced with the decision whether or not to undergo mammography screening. This dilemma will become even more important over the coming decades, as women aged 80 or older are the fastest growing segment of the U.S. population.20
Despite the complexities involved in decision making around mammography screening for the oldest-old, little is known about how these women decide on screening, what risks and benefits they consider in their decisions and what role their physicians play. The purpose of this study was to explore women aged 80 and older's decision-making regarding mammography screening and physician counseling about mammography screening to oldest-old women. Given limited existing information in this area we used qualitative methods to identify and describe aspects of the decision-making process.
METHODS
Study Design
We used individual interviews to obtain in-depth information about women aged 80 and older's decision-making around mammography screening from both patients and physicians. From physicians, we additionally collected detailed information about their counseling about mammography screening to women aged 80 and older.
Participants
Patients
We identified patients for this study using the electronic medical record at one large academic primary care clinic in Boston. Our electronic search identified 196 women aged 80 and older scheduled to see their primary care physicians (PCPs) between September and November 2004. We then e-mailed each physician for permission to contact women, asking physicians to exclude women who had a history of breast cancer and those who were unable to communicate verbally in English. We asked physicians to note if they thought a patient would be particularly thoughtful on their decision making around mammography screening and whether the patient was a racial minority. PCPs deemed 113 women eligible for the study. After using the electronic medical record to determine whether or not a woman was recently screened with mammography, we contacted eligible women by phone to see if they would be willing to meet with a study investigator after their next scheduled visit with their PCP. We met those who agreed to be interviewed at their next clinic visit and obtained written informed consent. Participants were offered $15 for completing the interview.
Since we sought to obtain a broad range of information and perspectives about mammography screening decisions among women aged 80 and older, we purposefully selected to interview both patients who had been screened with mammography within the past 2 years (recent screening) as well as women who not been recently screened. We also aimed to interview both white and African-American women. This sampling technique is known as “maximum variation sampling” and is used in qualitative research to capture diverse perspectives.21 We did not aim to sample women of other ethnic groups because few women from other backgrounds in this age group are in our practice.
Physicians
To recruit physicians for this study, we e-mailed physicians who cared for the most women aged 80 and older in their department as determined by reviewing patient panels. We met physicians who agreed to participate in their offices and obtained written informed consent. We initially planned on interviewing a small number of Internists and geriatricians to insure that our semi-structured interview guide for the patient interviews was complete. However, from early analysis of these interviews, it was clear that physicians offered rich insight about women aged 80 and older's decision-making and we chose to include the physician perspective in our analyses. From initial interviews with patients, Internists, and geriatricians, we learned that both gynecologists and mammographers can influence oldest-old women's decision-making around mammography screening and we decided to interview several gynecologists and mammographers to insure that our understanding of women aged 80 and older's decision-making was complete.
Interview Structure
All in-depth, semi-structured interviews were conducted in person by one investigator (M.S.) who had received graduate training in qualitative research. In-depth interviews are particularly useful in gaining insight into participants' beliefs, knowledge, and experiences.19 Questions were open-ended and probes were used to clarify and to further explore particular responses. To understand oldest-old women's decisions whether or not to undergo mammography screening, we adapted questions from previous qualitative studies involving younger women. The patient interview guide started by asking all women to “tell me what you know about mammograms.”22 We then asked women: “Please tell me about your decision to have a mammogram/not to have a mammogram in the past 2 years? What did you consider as you made this decision?”23 From studies of younger women, we knew that physicians, family, friends, as well as family history of breast cancer, perceived risk of breast cancer, the media, and health can influence mammography screening decisions and we probed about the influence of these factors among oldest-old women. At the conclusion of the interview, participants were asked about demographics, health status, and functional capacity. Patient interviews took approximately 20 minutes each.
At the beginning of each physician interview, we asked physicians to describe factors they thought influenced oldest-old women's mammography screening decisions. Physicians were then asked to comment on the influence of physicians, the doctor-patient relationship, patient's family and friends, the media, and patient's health and functional status. We then asked physicians (excluding mammographers) to describe their counseling about mammography screening to women aged 80 and older. We asked these physicians to describe any difficulties they encounter when counseling women aged 80 or older about mammography screening and to share any ideas they may have about improving counseling. We collected information on physician gender and years since graduating medical school. Physician interviews took approximately 30 minutes each.
Data Analysis
All interviews were audio-taped and transcribed verbatim using an external professional transcription service. Copies of all transcripts were distributed to each member of the analysis team (M.A.S., R.A.R., and E.R.M.). Qualitative analyses were conducted using an iterative process and following standard techniques. For analysis, we used an “editing” style.21 Each investigator began by systematically reading all of the interview notes in their entirety while making observations. Investigators independently then organized their observations into categories or codes. Coded sections were re-read for further interpretation. Coding discrepancies were resolved by consensus. One investigator (M.A.S.) used word processing software to separate the interview text by codes to insure complete identifications of themes within codes. When interpretation of interviews revealed no new significant insights (thematic saturation), interviewing was stopped. In qualitative research, sampling until the point of redundancy or thematic saturation provides evidence of the credibility of developed theory and is an accepted point to stop sampling subjects.21 Descriptive characteristics of the sample were determined using SAS statistical software version 8.1 (Cary, NC). Some quotes have been edited for grammar.
This study was approved by the Committee on Clinical Investigations.
RESULTS
We interviewed 23 women aged 80 and older until we achieved thematic saturation. The mean age of the 23 participants was 86 years, 13 had undergone recent mammography screening and 6 were African American (Table 1). We contacted 11 additional women who declined participation. None of the women who declined participation had received screening mammography within the past 2 years (this is significantly different from those who agreed to participate, P < .01), 3 were African American, and their mean age was 88 years. For the physician interviews, we interviewed 16 physicians until we achieved thematic saturation. Only 1 physician who was contacted (an Internist) chose not to participate. Our final physician sample included 6 Internists, 5 geriatricians, 3 gynecologists, and 2 mammographers (Table 1).
Table 1.
Patient and Physician Sample Characteristics
| Characteristics | n |
|---|---|
| Patient Characteristics | 23 |
| Mean age (86 ± 4 y; range 80 to 97 y) | |
| Race | |
| White | 17 |
| African American | 6 |
| Insurance | |
| Medicare+(Private/Medigap/Medex) | 17 |
| Medicare+(FreeCare/Medicaid) | 6 |
| Education | |
| College | 12 |
| Less than college | 11 |
| Functional dependence | |
| None | 9 |
| IADL dependence only | 7 |
| ADL and IADL dependence | 7 |
| Marital status | |
| Widowed | 14 |
| Married | 5 |
| Other | 4 |
| Health status | |
| Excellent/very good | 6 |
| Good | 7 |
| Fair/poor | 10 |
| Mammogram in the past 2 y | |
| Yes | 13 |
| No | 10 |
| Physician Characteristics | |
| Gender | |
| Male | 7 |
| Female | 9 |
| Mean years since medical school graduation (27 ± 12.0 y) | |
| Specialty | |
| Internal Medicine | 6 |
| Geriatrics | 5 |
| Gynecology | 3 |
| Mammography | 2 |
ADL, activity of daily living; IADL, instrumental activity of daily living
Factors Influencing Screening Decisions
Patients and physicians noted several factors in common that influenced mammography screening decisions among women aged 80 or older (Table 2). Such factors included: the importance of physician influence; patient factors including patient preferences (which we will discuss in greater detail below), habit of screening, personal/family history of breast disease, previous experience with mammography, and perceived risk of breast cancer; system factors including mailed reminder cards and access, specifically the ease of actually getting a mammogram; and social influences including the influence of patients' daughters or a family/friend's experience with breast cancer. Many factors influenced some women to choose screening and others not to choose screening. For instance, women who perceive their risk of breast cancer to be low because “no one in my family has ever had breast cancer” may choose not to be screened. However, women who perceive their risk of breast cancer to be high, possibly due to a history of benign breast disease or family history, may choose to continue with screening. Similarly, women who are in the habit of undergoing screening may not want to stop at age 80 and those who were never screened before age 80 are unlikely to want to start now. Several factors appeared to influence women solely in the direction of choosing screening such as a daughter's recommendation or mailed reminder cards. Table 2 demonstrates each theme, the frequency each theme was discussed, and gives example quotes. Figure 1 illustrates the relationship of these content areas within a conceptual framework.
Table 2.
Content Areas and Themes in Women Aged 80 or Older's Decision-making Regarding Mammography Screening
| Content Area | Themes | Frequency* | Example Quotes | ||
|---|---|---|---|---|---|
| Pts | MDs | ||||
| Physician influence | MD recommendations | 10 | 10 | Pt: “No doctor has told me to have a mammogram lately, so I have not been bothered with that.”MD: “Older patients are more likely to go with what the doctor tells them.” | |
| Patient factors | Taking care of oneself | 6 | 6 | Pt: “I think [mammography screening] is good for everybody. All women should find out about their bodies.”MD: “Patients feel that [getting a mammogram] is part of being a healthy woman.” | |
| Rather not know | 5 | 5 | Pt: “Maybe the less I know the better.”MD: “Some patients do not get [mammograms], because they do not want to know.” | ||
| Habit | 4 | 8 | Pt: “I have become used to it, I have been having it for quite a few years now.”MD: “If it becomes a habit in your earlier years why would you not continue?” | ||
| Family history | 5 | 8 | Pt: “I feel that because of my family history it is a good idea.”MD: “If [patients] have family members who have had breast cancer often that will influence them to want to be screened.” | ||
| Personal history of breast disease | 8 | 3 | Pt: “I did have one biopsy…It was nothing…I just come back automatically once a year to be sure.”MD: “Personal experience with breast abnormalities [influence elderly women's screening decisions].” | ||
| Previous experience | 8 | 5 | Pt: When I went for a mammogram, around me everybody was nervous and I decided that this is the time to stop.”MD: “Some patients who have had an unpleasant experience, physically, once they get to be over age 80 do not want to do [mammography] again.” | ||
| Perception of risk | 6 | 7 | Pt: “Once you reach 80, you do not have to worry.”MD: “A patient might ask, what is the risk at this point in my life of actually getting breast cancer.” | ||
| Age | 6 | 9 | Pt: “I am old and it is not very important to me.” | ||
| MD: “There is a perception among some elderly that they do not need [mammography] anymore, that as you get older it is less important.” | |||||
| Health | 2 | 16 | Pt: “If I was dying from something else then I probably would not worry too much about breast cancer.”MD: “On some level they incorporate whether they are going to live long enough to make it worth their while without actually saying so.” | ||
| Functional status | 3 | 7 | Pt: “As long as I can get there.”MD: “If their functional status is very good they will proceed with testing; even if they have a lot of medical problems, because they can.” | ||
| System factors | Mailed reminder cards | 3 | 4 | Pt: “The hospital sends me a notice when it is time [for my mammogram] and that is about it.”MD: “It really happens without my knowledge. They get a card from the radiology department that it is time.” | |
| Ease of getting a mammogram | 9 | 4 | Pt: “It is easy. I just come in and have it done and go home.”MD: “I do not think that most people find getting a mammogram particularly onerous.” | ||
| Social influences | Family/friend's experience | 5 | 7 | Pt: “The reason why I really started having mammograms [was] because my sister she died of cancer and I do not think she ever went for a mammogram.”MD: “One patient saw a niece die from breast cancer, that was the deciding factor in her continuing to get mammograms.” | |
| Daughter's recommendation | 2 | 8 | Pt: “My daughter makes sure I get to all of my scheduled appointments.”MD: “I have seen patients change their minds because the daughter has encouraged them to continue.” | ||
As this study used qualitative methods, the frequencies presented cannot be used to determine prevalence of ideas
FIGURE 1.
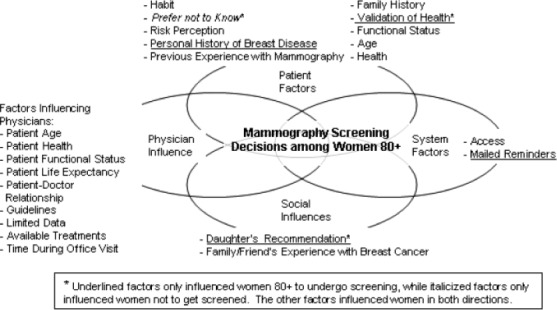
Conceptual framework of mammography screening decisions among women aged 80 and older. The other factors influenced women in both directions
Physicians more than patients commented about the influence of patient's health and functional status on mammography screening decisions. Most physicians commented that patient's health influenced patient's screening decisions but few patients felt that their health influenced their decision. Patients frequently commented that mammography screening was associated with no risks, was available, and easy to undergo. Nine women believed that there were no risks to getting screening mammograms and another 9 women commented that although mammography screening could be uncomfortable the pain was tolerable. One patient commented, “I feel that it is very important whether you are 30 or you are 80 [that] you have any tests that you can.” Although we asked both patients and physicians about the role of media on mammography screening decisions, none of the patients thought it influenced their screening decisions and 10 physicians felt that the media influenced screening decisions of women of all ages but were less influential for women aged 80 or older.
Patient Screening Preferences
We identified 3 types of elderly women's screening preferences: (1) women enthusiastic about screening mammography; (2) women opposed to screening mammography; and (3) women without a strong preference who followed their physician's recommendation. We found that 10 women were very enthusiastic about screening mammography, including 1 woman who had not been screened in the past 2 years. One woman commented: “Mammograms are as important to me as visiting Dr. X. I just feel that it is a very important, very important procedure.” Another woman commented: “I should have it [mammography] every year as long as I am living, so if any tumors are growing then I will know about them before they get too advanced.” These women described feeling a sense of reassurance after a negative mammogram, “when they tell you on the same day that everything [is] all right it is a relief.” The 1 women who had not been screened with mammography in the past 2 years but still felt that she needed to be screened commented, “I know I have to do this, I have not felt so good so I have not done it. I will.”
Six women were opposed to getting screened mammography; 3 mainly due to age. “I decided [not to go for mammography] because I am an old woman and nobody lives forever.” One woman decided not to go for mammography because “I have other problems with my health;” 1 women “because if they found something, I would not go through an operation anyway;” and 1 women because “I just cannot get there…on account of my legs.”
Seven women based their screening decisions mainly on their physician's recommendations (4 who were screened in the past 2 years and 3 who were not). “I go along with what they say. If they say you do not need a mammogram at your age, I will settle for that. If they say you need a mammogram then I will just get one.”
Physician Counseling About Screening
Physician counseling about mammography screening to oldest-old women varied. Many individualized their discussions to each patient. Eight physicians described recommending screening to patients they perceived to have adequate life expectancy and discussing stopping screening or not discussing screening with patients who they perceived to have very limited life expectancy. If patients had a preference about screening they followed the patient's preference. Five physicians generally encouraged screening to most patients, “until I am told that the data shows that there's no use to it or worse that it's harmful, I will encourage them [women aged 80 or older] to do it on an annual basis.” Two physicians generally discouraged screening for women in this age group. Patient's age, health, functional status, and life expectancy, influenced physicians' screening recommendations. “If I think that someone has 1 to 3 years to live it is preposterous to start screening. If someone at the other end is incredibly healthy and may have 15 to 20 years ahead of them, then at least theoretically it makes more sense.” Three physicians commented that they were less likely to recommend screening to patients as they aged into their late 80s or 90s. Eight physicians noted that the availability of acceptable treatments for elderly women with breast cancer influenced their screening recommendations.
Nine physicians described difficulties when discussing stopping screening with women aged 80 or older. Six of these physicians commented that discussing stopping screening can be uncomfortable, “it is very hard for me to say you do not need a mammogram, you are not going to benefit…so sometimes even though I know that it does not make sense, I will still do it.” Six physicians also described how difficult it was for patients to understand the risks associated with mammography and 3 physicians talked about the fact that this discussion can take a great deal of time during an already busy clinic. One physician commented, “there is a magical thinking that goes on about cancer screening with people. They feel that if they do it, it protects them. I do not disavow people of that just because it is too time consuming.” Six physicians described that a long-standing doctor-patient relationship and patient trust can facilitate these discussions. “It has a lot to do with trust, especially if someone is accustomed to having regular mammograms done and you are recommending not [to] do it anymore.” Six physicians requested more data about the risks and benefits of mammography screening for women aged 80 or older, “it would be nice if we had better studies, better guidelines…that might make it a little easier.”
DISCUSSION
Our study explored the complex nature of decision making about mammography screening for women aged 80 or older. We identified several content areas and consistent emerging themes that influenced women aged 80 or older's screening decisions including physician's influence, patient preferences, system factors, and social influences. We found that some women aged 80 or older have strong opinions about whether or not to get screening mammography, while others appear to follow their doctor's or daughter's recommendations. Some physicians individualize their discussions about screening to oldest-old women, others generally encourage screening unless a patient has a very short life expectancy; and few discourage screening. Physicians feel that discussing stopping screening with women aged 80 or older is difficult because the discussions can be uncomfortable and time consuming. Many requested more data about the benefits and risks of mammography screening for women aged 80 or older to facilitate these discussions.
To date no studies have explored factors influencing mammography screening decisions among women aged 80 and older. Several studies have examined factors that influence screening decisions among younger women.23–25 Nekhlyudov et al.24 explored decision-making around screening among 16 women aged 38 to 45 without prior screening mammograms and found that decisions for screening were motivated by the media, medical providers, other women with breast cancer, and psychosocial factors. Salazar and Moor25 explored decision making around mammography screening among 87 working women aged 39 to 75 and found that challenges arranging mammography screening, fear of breast cancer or breast cancer treatment, the cost of screening, and the influence of a health care provider, among other factors, influenced screening decisions. We found that some of the factors that influenced younger women's screening decisions also influenced women aged 80 or older's screening decisions (e.g., doctor's recommendation, perceived risk of breast cancer); however, we also found that other factors were important to women aged 80 or older (e.g., habit, functional status, personal history of breast disease, or daughter's recommendation). We also found that some factors that appeared to influence younger women's decisions may be less important to older women (e.g., media, cost of mammography).
Since prior studies have generally found that elderly women more than younger women defer medical decisions to their physicians,26–28 we were interested to learn that many women aged 80 or older had their own opinions about whether or not they should be screened with mammography. In the future, we will determine which factors are most important to women aged 80 or older when considering mammography screening and how the importance of these factors differs for women aged 80 or older compared with younger women. Our goal is to help patients make decisions about mammography screening in accordance with their values and preferences and to insure that screening is targeted to those most likely to benefit.
We were somewhat surprised to find how enthusiastic some women aged 80 or older were about mammography screening, especially when there is no clinical trial data demonstrating a mortality benefit for these women. Our results may have been biased toward enthusiasm for screening, since women who agreed to participate in our study were more likely to have been screened with mammography in the past 2 years than those who refused to participate. The enthusiasm expressed by many oldest-old women in our study may be a result of years of messages from public health officials, physicians, and advocacy groups, persuading women about the importance of mammography screening. Schwartz et al.29 recently sampled a random sample of U.S. adults and found that 87% believed routine cancer screening is almost always a good idea and 41% of women felt it was irresponsible of an 80-year-old woman to choose not to be screened with mammography. Public health messages about mammography screening in the future may need to present a more balanced picture of the benefits and risks to insure informed decision-making, particularly for the oldest-old.
Interestingly, daughters of the oldest-old appear to play an important role in their mother's decisions around mammography screening. Experts have described that medical decision making in geriatrics often occurs in collaboration between older patients, their physicians, and their family members.30–32 Daughters may encourage their oldest-old mothers to undergo mammography screening since they know that mammography screening is important for their own health and assume that it must be equally important to their mother's health. Daughters may see themselves as advocates of their older mother's health and may view physicians who do not offer their mothers mammography screening as ageist, especially since there is some evidence to suggest that there are some age-related disparities in cancer screening.33 It is important to explore the role of daughters in elderly women's decision-making to ensure that screening and other medical decisions reflect the preferences of patients and not only of their daughters.
Since experts encourage physicians to discuss both the benefits and harms of screening to elderly patients,19 we were interested in learning more about physician counseling about mammography screening to women aged 80 or older. Prior studies have found that physicians generally highlight the benefits of screening because it is difficult to explain population statistics to an individual patient during short clinic visits.34,35 In addition to these difficulties, we found that physicians are particularly uncomfortable discussing stopping screening with oldest-old women as it requires discussing patient's life expectancy. This discomfort may be similar to the discomfort physicians feel when discussing end-of-life care with patients.36,37 To improve end-of-life discussions, experts recommend that physicians initiate and re-initiate these discussions, clarify prognosis, identify goals, and develop a treatment plan.38,39 These same principles may help physicians when discussing stopping mammography screening. Physicians may need to initiate and re-initiate screening discussions, discuss patient's life expectancy, determine patients' preferences for work-up and treatment of abnormal mammograms, and focus on health promotion measures that can benefit oldest-old women in a shorter time frame. As it is important to learn how to encourage patients to undergo screening it is also important to learn how to discuss stopping screening with patients who have little chance to benefit. More data on the risks and benefits of screening may help physicians with these discussions.
In addition, physicians understanding which factors are influencing oldest-old women's screening preferences may help physicians individualize their discussions about mammography screening. For instance, a woman with limited life expectancy who prefers to undergo mammography screening because it gives her a sense that she is doing all she can for her health may benefit from her physician discussing other ways besides mammography that she can maintain her health, perhaps through physical activity. Similarly, a woman in her early 80s without significant illness but who prefers not to get screened because “she is too old” may benefit from a more thoughtful discussion about the risks and benefits of screening. Physicians should work to become more comfortable discussing stopping screening with those patients who defer their screening decisions to their physicians. Finally, physicians may want to question whether annual reminder cards about mammography screening are appropriate for oldest-old women who may not benefit. Ideally, mammography screening should be targeted to oldest-old women most likely to benefit.
Our study has several limitations that must be acknowledged. All of the in-depth interviews took place at one academic medical center in Boston, limiting generalizability. Participants were more likely to have received a recent mammogram than nonresponders which may bias our results to more favorable views of mammography screening, however, nearly half of the women in our sample had not been screened with mammography in the past 2 years. Since we used qualitative methods we cannot use our data to estimate the prevalence of ideas. Additionally, although we had 3 independent coders, coding of interviews is subjective. Finally, due to small sample size we were unable to look at differences within patient groups (e.g., recent use of mammography) or physician groups (e.g., specialty).
In this qualitative study, we identified factors that influenced oldest-old women's mammography screening decisions and explored physician counseling around mammography screening to oldest-old women. We were interested to learn how enthusiastic some women aged 80 or older were about mammography screening and that physicians find discussing stopping screening with patients difficult and uncomfortable. Understanding which factors influence a patient's decision-making may aid with discussions about screening as would more data about the benefits and risks of mammography screening for women aged 80 and older. Ideally, women aged 80 and older should understand the benefits and risks associated with each possible course of action that they might choose when deciding on mammography screening.
Acknowledgments
We would like to thank Lisa I. Iezzoni, MD, MSc, from the Division of General Medicine and Primary Care, Beth Israel Deaconess Medical Center for her help in reviewing this manuscript. Grant support was obtained from the National Research Service Award from the National Cancer Institute (1 F32 CA110424-01).
REFERENCES
- 1. Medicare laws: PL 105-33; section 410 and 42 U.S.C. section 1395m.
- 2.Walter LC, Lindquist K, Covinsky KE. Relationship between health status and use of screening mammography and Papanicolaou smears among women older than 70 years of age. Ann Intern Med. 2004;140:681–8. doi: 10.7326/0003-4819-140-9-200405040-00007. [DOI] [PubMed] [Google Scholar]
- 3.Alexander FE, Anderson TJ, Brown HK, et al. 14 years of follow-up from the Edinburgh randomised trial of breast-cancer screening. Lancet. 1999;353:1903–8. doi: 10.1016/s0140-6736(98)07413-3. [DOI] [PubMed] [Google Scholar]
- 4.Andersson I, Aspegren K, Janzon L, et al. Mammographic screening and mortality from breast cancer: the Malmo mammographic screening trial. BMJ. 1988;297:943–8. doi: 10.1136/bmj.297.6654.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu KC, Smart CR, Tarone RE. Analysis of breast cancer mortality and stage distribution by age for the Health Insurance Plan clinical trial. J Natl Cancer Inst. 1988;80:1125–32. doi: 10.1093/jnci/80.14.1125. [DOI] [PubMed] [Google Scholar]
- 6.Frisell J, Lidbrink E, Hellstrom L, Rutqvist LE. Followup after 11 years—update of mortality results in the Stockholm mammographic screening trial. Breast Cancer Res Treat. 1997;45:263–70. doi: 10.1023/a:1005872617944. [DOI] [PubMed] [Google Scholar]
- 7.Tabar L, Fagerberg G, Chen HH, et al. Efficacy of breast cancer screening by age. New results from the Swedish Two-County Trial. Cancer. 1995;75:2507–17. doi: 10.1002/1097-0142(19950515)75:10<2507::aid-cncr2820751017>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy EP, Burns RB, Freund KM, et al. Mammography use, breast cancer stage at diagnosis, and survival among older women. J Am Geriatr Soc. 2000;48:1226–33. doi: 10.1111/j.1532-5415.2000.tb02595.x. [DOI] [PubMed] [Google Scholar]
- 9.McPherson CP, Swenson KK, Lee MW. The effects of mammographic detection and comorbidity on the survival of older women with breast cancer. J Am Geriatr Soc. 2002;50:1061–8. doi: 10.1046/j.1532-5415.2002.50261.x. [DOI] [PubMed] [Google Scholar]
- 10.Boer R, de Koning HJ, van Oortmarssen GJ, van der Maas PJ. In search of the best upper age limit for breast cancer screening. Eur J Cancer. 1995;31A:2040–3. doi: 10.1016/0959-8049(95)00457-2. [DOI] [PubMed] [Google Scholar]
- 11.Mandelblatt J, Saha S, Teutsch S, et al. The cost-effectiveness of screening mammography beyond age 65 years: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139:835–42. doi: 10.7326/0003-4819-139-10-200311180-00011. [DOI] [PubMed] [Google Scholar]
- 12.Mandelblatt JS, Wheat ME, Monane M, Moshief RD, Hollenberg JP, Tang J. Breast cancer screening for elderly women with and without comorbid conditions. A decision analysis model. Ann Intern Med. 1992;116:722–30. doi: 10.7326/0003-4819-116-9-722. [DOI] [PubMed] [Google Scholar]
- 13.Mandelblatt JS, Schechter CB, Yabroff KR, et al. Toward optimal screening strategies for older women. J Gen Intern Med. 2005;20:487–96. doi: 10.1111/j.1525-1497.2005.0116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Geriatrics Society Clinical Practice Committee. Breast cancer screening in older women. J Am Geriatr Soc. 2000;48:842–4. [PubMed] [Google Scholar]
- 15.Screening for breast cancer: recommendations and rationale. Ann Intern Med. 2002;137(5 Part 1):344–6. doi: 10.7326/0003-4819-137-5_part_1-200209030-00011. [DOI] [PubMed] [Google Scholar]
- 16.Smith RA, Saslow D, Sawyer KA, et al. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53:141–69. doi: 10.3322/canjclin.53.3.141. [DOI] [PubMed] [Google Scholar]
- 17.Taplin SH, Ichikawa L, Yood MU, et al. Reason for late-stage breast cancer: absence of screening or detection, or breakdown in follow-up? J Natl Cancer Inst. 2004;96:1518–27. doi: 10.1093/jnci/djh284. [DOI] [PubMed] [Google Scholar]
- 18.Walter LC, Lewis CL, Barton MB. Screening for colorectal, breast, and cervical cancer in the elderly: a review of the evidence. Am J Med. 2005;118:1078–86. doi: 10.1016/j.amjmed.2005.01.063. [DOI] [PubMed] [Google Scholar]
- 19.Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285:2750–6. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau. Washington, DC: US Census Bureau; 2002. [July 15, 2005]. Current Population Survey, July 2002. Available at: http://www.census.gov. [Google Scholar]
- 21.Doing Qualitative Research. Vol. 12. Newbury Park, CA: Sage Publications; 1992. pp. 1–2. [Google Scholar]
- 22.Silverman E, Woloshin S, Schwartz LM, Byram SJ, Welch HG, Fischhoff B. Women's views on breast cancer risk and screening mammography: a qualitative interview study. Med Decis Making. 2001;21:231–40. doi: 10.1177/0272989X0102100308. [DOI] [PubMed] [Google Scholar]
- 23.Lewis ML, Corcoran-Perry SA, Narayan SM, Lally RM. Women's approaches to decision making about mammography. Cancer Nurs. 1999;22:380–8. doi: 10.1097/00002820-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Nekhlyudov LD, Ross-Degnan D, Fletcher SW. Beliefs and expectations of women under 50 years old regarding screening mammography: a qualitative study. J Gen Intern Med. 2003;18:182–9. doi: 10.1046/j.1525-1497.2003.20112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salazar MK, de Moor C. An evaluation of mammography beliefs using a decision model. Health Educ Q. 1995;22:110–26. doi: 10.1177/109019819502200110. [DOI] [PubMed] [Google Scholar]
- 26.Degner LF, Kristjanson LJ, Bowman D. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277:1485–92. [PubMed] [Google Scholar]
- 27.Sox HC. Screening for disease in older people. J Gen Intern Med. 1998;13:424–5. doi: 10.1046/j.1525-1497.1998.00126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benbassat J, Pilpel D, Tidhar M. Patients' preferences for participation in clinical decision making: a review of published surveys. Behav Med. 1998;24:81–8. doi: 10.1080/08964289809596384. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz LM, Woloshin S, Fowler FJ, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291:71–8. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- 30.Adelman RD, Greene MG, Charon R. The physician-elderly patient-companion triad in the medical encounter: the development of a conceptual framework and research agenda. Gerontologist. 1987;27:729–34. doi: 10.1093/geront/27.6.729. [DOI] [PubMed] [Google Scholar]
- 31.Greene MG, Majerovitz SD, Adelman RD, Rizzo C. The effects of the presence of a third person on the physician-older patient medical interview. J Am Geriatr Soc. 1994;42:413–9. doi: 10.1111/j.1532-5415.1994.tb07490.x. [DOI] [PubMed] [Google Scholar]
- 32.Dalton JM. Development and testing of the theory of collaborative decision-making in nursing practice for triads. J Adv Nurs. 2003;41:22–33. doi: 10.1046/j.1365-2648.2003.02502.x. [DOI] [PubMed] [Google Scholar]
- 33.Jerant AF, Franks P, Jackson JE, Doescher MP. Age-related disparities in cancer screening: analysis of 2001 Behavioral Risk Factor Surveillance System data. Ann Fam Med. 2004;2:481–7. doi: 10.1370/afm.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dunn AS, Shridharani KV, Lou W, Bernstein J, Horowitz CR. Physician-patient discussions of controversial cancer screening tests. Am J Prev Med. 2001;20:130–4. doi: 10.1016/s0749-3797(00)00288-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolf AM, Becker DM. Cancer screening and informed patient discussions. Truth and consequences. Arch Intern Med. 1996;156:1069–72. [PubMed] [Google Scholar]
- 36.Mermann AC, Gunn DB, Dickinson GE. Learning to care for the dying: a survey of medical schools and a model course. Acad Med. 1991;66:35–8. doi: 10.1097/00001888-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Tulsky JA, Chesney MA, Lo B. See one, do one, teach one? House staff experience discussing do-not-resuscitate orders. Arch Intern Med. 1996;156:1285–9. doi: 10.1001/archinte.156.12.1285. [DOI] [PubMed] [Google Scholar]
- 38.Balaban RB. A physician's guide to talking about end-of-life care. J Gen Intern Med. 2000;15:195–200. doi: 10.1046/j.1525-1497.2000.07228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.von Gunten CF, Ferris FD, Emanuel LL. The patient-physician relationship. Ensuring competency in end-of-life care: communication and relational skills. JAMA. 2000;284:3051–7. doi: 10.1001/jama.284.23.3051. [DOI] [PubMed] [Google Scholar]


