Abstract
BACKGROUND
Providing antidepressant information to patients may foster greater adherence to therapy.
OBJECTIVE
To assess physician information-giving while prescribing antidepressants, and to identify factors that influence the provision of information.
DESIGN
Randomized experiment using standardized patients (SPs). Standardized patients roles were generated by crossing 2 clinical conditions (major depression or adjustment disorder) with 3 medication request types (brand-specific, general, or none).
PARTICIPANTS
One hundred and fifty-two general internists and family physicians recruited from solo and group practices and health maintenance organizations; cooperation rates ranged from 53% to 61%.
MEASUREMENTS
We assessed physician information-giving by analyzing audio-recordings of interactions between physicians and SPs, and collected physician background information by survey. Generalized estimating equations were used to examine the influence of patient and physician factors on physicians' provision of information.
RESULTS
One hundred and one physicians prescribed antidepressants, accounting for 131 interactions. The mean age of physicians was 46.3 years; 69% were males. Physicians mentioned an average of 5.7 specific topics of anti-depressant–related information (of a possible maximum of 11). The most frequently mentioned topic was purpose (96.1%). Physicians infrequently provided information about the duration of therapy (34.9%) and costs (21.4%). Standardized patients who presented with major depression received less information than those with adjustment disorder, and older and solo/private practice physicians provided significantly less information to SPs.
CONCLUSIONS
Physicians provide limited information to patients while prescribing antidepressants, often omitting critical information that may promote adherence. Mechanisms are needed to ensure that patients receive pertinent antidepressant information.
Keywords: physician, communication, drug information
Researchers estimate that the lifetime prevalence rate of depression is 16%, affecting about 5% of the U.S. adult population in a given year.1,2 Patients experiencing their first episode of major depression need to continue antidepressant therapy for 4 to 9 months for maximum efficacy.3 However, nonadherence to medications is a significant barrier to the effective treatment of depression.4–6 Discontinuation rates of antidepressants within 3 months of treatment initiation can reach 68%.7 Therefore, it is important to develop strategies to encourage patients to adhere to antidepressant treatment.
Primary care physicians can play an essential role in increasing adherence to antidepressants by educating patients about treatment.8 In several studies, when physicians provided information to patients regarding antidepressant treatment, patients were more knowledgeable and had more positive initial beliefs about their medication, and were more likely to adhere to antidepressant therapy.4,7,9 These findings suggest a causal relationship between greater physician information-giving and better antidepressant adherence.
Despite the manifest importance of providing appropriate information to patients initiating antidepressants, current practice may be suboptimal.4,10 Variations in depression severity, antidepressant history (new vs refill), medical comorbidities, and visit types (new vs follow-up) within and between previous studies make it difficult to draw firm conclusions about the current state of practice.10–13
In this study, we examined physicians' information giving on antidepressants and assessed whether patient level of depression and physician characteristics influenced such behavior. We addressed the following research questions: (1) what types of drug information do physicians provide at the time of prescribing antidepressants; (2) what are the relationships between patients' level of depression (major depression and adjustment disorder with depressed mood) and physicians' provision of drug information; and (3) what are the relationships between physician-level characteristics (age, gender, ethnicity, practice setting, and number of patients seen during a typical half-day) and physicians' provision of drug information? We used an experimental study design to control for patient variability, a level of control absent in past research.
METHODS
Procedures
This study was a part of a larger randomized experiment in which primary care physicians in 3 U.S. cities saw 2 unannounced standardized patients (SP) from May 2003 to 2004. The SPs were trained to portray 6 roles, generated by crossing 2 clinical conditions (major depression or adjustment disorder with depressed mood) with 3 prescription drug request types (brand-specific, general, or none).
Standardized patients were white, middle-aged, nonobese women, most with professional acting experience. Standardized patient role outlines were developed and reviewed by national experts in psychology, psychiatry, primary care, and SP methodology. Role outlines were revised iteratively until they were judged by a consensus of primary investigators and advisors to be clinically credible and manageable within the context of 15 to 20 minute new primary care, acute consultation. Training focused on depicting the historical and emotional features of depression and adjustment disorder, and mastering biographical details of the roles. Standardized patients were not scripted to ask for any specific information about a prescribed antidepressant. Each SP was assigned 1 of the 6 roles for the entire study and was required to portray role details with 95% accuracy and maintain affective fidelity. In addition, SPs were monitored throughout training and data collection. Detailed information about SP roles and training is available elsewhere.14 The study protocol was approved by the institutional review boards at all participating institutions.
In order to assess SP detection, physicians were sent a letter by facsimile (within 2 weeks of an SP visit) asking them to indicate whether “during the past 2 weeks” they were at any time “suspicious” that a patient visiting their office was actually an SP. Clinicians responded that they had been “definitely” or “probably” suspicious before or during at least 1 patient encounter during the previous 2 weeks in 12.8% of visits.
Internal and family medicine physicians (N = 152) were recruited by working with 4 physician groups: the UC Davis Primary Care Network (UCD) and Kaiser-Permanente in Sacramento, California; Brown and Toland Medical Group in San Francisco, California; and Excellus-Blue Cross in Rochester, New York. Recruiting was conducted by mail with telephone follow-up at all sites. Physicians were told that the purpose of the study was to “assess social influences on practice and the competing demands of primary care.” Physicians were also told that the study would involve seeing 2 SPs several months apart, and that each SP would present with a combination of common symptoms. Full debriefing was supplied afterwards. Physicians and their practices were offered monetary incentives of up to $375 for participation and visit reimbursement. Participation rates ranged from 53% (Kaiser) to 61% (UCD). The age and gender distributions of participating physicians were similar to those of the practices as a whole.
All visits were covertly audio-taped with prior physician consent. Information about physician characteristics (i.e., age, gender, ethnicity, practice setting, and number of patients seen during a typical half-day) was obtained by surveying participating physicians. For the purposes of this analysis, we selected all cases from the overall sample in which antidepressant medications (including a newer generation antidepressant in any dose or a heterocyclic antidepressant in a final (target) dose equivalent to at least 75 mg of amitriptyline) were prescribed (n = 131). The minimum dose requirement for heterocyclic antidepressants was meant to exclude low-dose prescriptions intended for treatment of insomnia or pain. Prescribing decisions were based on the review of actual prescription forms or in some cases, drug samples.
Coding
Two coders assessed the information physicians provided to the SPs directly from the audiotapes. The coding system used for this study was based upon tools used in previous research that were found to be reliable.4,10,15 The coding system allowed research assistants to take an inventory of the prescription drug information physicians provided to the SPs.15 The coding system was composed of (a) specific topics of information (Provision of Drug Information) and (b) Instructional Messages.
Provision of Drug Information
First, coders recorded whether physicians mentioned: name of the medication; purpose; dose/strength; timing/schedule; what to do if patient misses a dose; duration of therapy (e.g., 3, 6, 9 months); how well the medication works (expected benefits); side effects; problems or barriers to use; costs; and technical information (e.g., mechanism of action, drug interactions). The specific topics of information items were summated to indicate how many topic areas physicians discussed during the consultation (Provision of Drug Information). The Provision of Drug Information scores could range from 0 to 11. We selected a random sample of 20% of the audiotapes to assess reliability between the 2 coders. Interrater reliability coefficients (κ values) ranged from K =0.82 to 1.00 for agreement on specific drug information items, and intraclass correlation of 0.97 for the Provision of Drug Information score.
Individual antidepressant information elements also were sorted into 3 categories: basic (physician stated the name and purpose), drug administration (dose and timing), and effectiveness and safety (how well the medication works and side effects). The depth and quality of discussion about particular topics of drug information was not assessed in this study. However, interactions were randomly selected to provide illustrative examples of physicians' communication regarding specific antidepressant information.
Instructional Messages
Next, the coders assessed whether physicians provided the following specific instructions: take the medication daily; antidepressants must be taken for 2 to 4 weeks for a noticeable effect; continue to take the medicine even if feeling better; do not stop taking antidepressant without checking with the physician; and specific instructions regarding what to do to resolve questions regarding antidepressants. We examined these specific messages because they previously have been found to be positively associated with adherence to antidepressants.4 Specific instruction items were summated to indicate how many instructional messages physicians discussed during the consultation. The Instructional Message scores could range from 0 to 5. Inter-rater reliability coefficients for these items ranged from K =0.82 to 1.00; intraclass correlation of 0.93.
Analysis
We calculated descriptive statistics to examine specific information obtained in the inventory. We used generalized estimating equations (GEE) specifying the Poisson distribution to examine the relationships between physicians' provision of antidepressant drug information and (1) patient's level of depression, and (2) physician characteristics (age, gender, ethnicity, primary clinical practice, and number of patients seen during a typical half-day). We used GEE to adjust the standard errors of the regression coefficients because patients were nested within physicians. We included the experimental factor (prescription drug request types), office visit duration (in minutes), follow-up schedule (within 2 weeks of the office visit vs other), and SPs (we created dummy variables for each SP) in the GEE models in order to control for their potential effects. We specified a Poisson distribution to deal with the count data. Alternative models using a normal distribution produced results that were not materially different, so only the primary results are reported. The Statistical Analysis System (SAS for Windows, version 8.0, SAS Institute, Cary, NC) was used to analyze the data.
RESULTS
One hundred and one physicians prescribed antidepressant medications during at least 1 SP visit, accounting for 131 interactions (30 physicians prescribed antidepressants to 2 SPs). However, analyses were conducted on data from 129 interactions because 2 audio recordings failed. The average age of physicians was 46.3 years, range 30 to 81 (SD=10.4 years). The majority of the physicians were male (69%) and Caucasian (75%). Forty-six percent of prescribing physicians described their main clinical practice setting as single-specialty or multispecialty group practice, 23% reported solo private practice, 19% reported group or staff model health maintenance organization, and 12% reported practicing in an academic medical center.
On average, physicians provided information about 5.7 (SD=1.6) specific topics concerning prescribed antidepressants (of a possible maximum of 11). As shown in Table 1, the most frequently provided pieces of drug information were purpose (96.1%), name (90.7%), side effects (85.3%), and timing/schedule (76.0%). The areas of drug information that were mentioned the least were addressing problems or barriers to use (1.6%) and what to do if you missed a dose (0.8%).
Table 1.
Antidepressant Information Provided by Physicians
| Drug Topic | Percentage of Visits |
|---|---|
| Purpose | 96.1 |
| Name | 90.7 |
| Side effects | 85.3 |
| Timing | 76.0 |
| Technical information | 68.2 |
| Dose/strength | 59.7 |
| How well drug works | 38.0 |
| Duration | 34.9 |
| Costs | 21.4 |
| Problems or barriers to use | 1.6 |
| What to do if you miss a dose | 0.8 |
| Instructional messages | |
| Medication takes 2 to 4 wk for noticeable effect | 69.8 |
| Take medication daily | 68.2 |
| What to do to resolve concerns/questions | 25.6 |
| Continue medication even if feeling better | 5.4 |
| Do not stop taking medication without consulting with doctor | 3.9 |
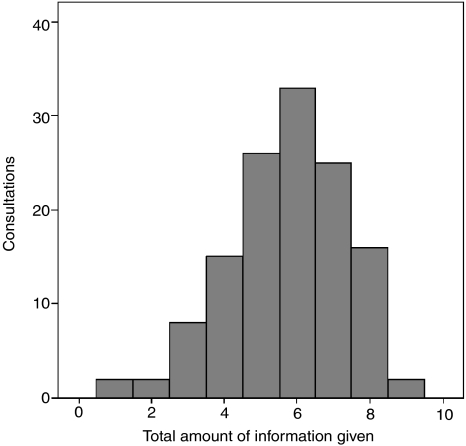
There were no consultations in which a physician informed a SP about every item of information contained in the Provision of Drug Information scale. Physicians failed to provide SPs with the name of the prescribed antidepressant in 12 consultations. However, there were no cases in which an SP left a consultation without at least 1 piece of information about the prescribed antidepressant, and there were only 2 cases in which physicians provided information about just 1 topic area. The purpose of the drug was mentioned in both cases. Figure 1 presents a histogram of the proportion of consultations in which various amounts of information were provided.
FIGURE 1.
Histogram of consultations and the amount of information provided.
Physicians mentioned basic, administration, and effectiveness and safety information in 87.6%, 47.3%, and 34.1% of visits, respectively. Table 2 provides qualitative illustrations of physician communication about specific antidepressant information. There seems to be some evidence of physicians using technical jargon only to describe technical information about prescribed drugs (e.g., mechanism of action).
Table 2.
Qualitative Illustrations of Physician Communication about Prescribed Antidepressants
| Drug Topics | Examples |
|---|---|
| Purpose | “… there's all kinds of medicines we give for depression … I'll give you some samples of an antidepressant.” |
| Name | “There is a specific medicine that I would think might be helpful for you. Its called Remeron.” |
| Side effects | “Basically, there are no real side effects of taking this medication, especially for women. In men there is some sexual dysfunction and to women usually there isn't. You may gain a little bit of weight. You may lose a little bit of weight. It's unpredictable.” |
| Timing | “So we usually start off, a standard starting dose is one tablet daily.” |
| Technical information | “Actually, what it does is it binds the receptors, some receptors in your brain and so it blocks that serotonin from being taken out of your system so it boosts it up, the serotonin that is already in the brain up. So it is not like we're giving you serotonin. It is basically giving you a medicine that helps your body naturally increase the serotonin in your brain. Do you understand what I am saying?” |
| Dose/strength | “Paxil you usually start out with a lower dose on it, although some people start out on 25 mg, start out on 12.5 mg.” |
| How well drug works | “… So that is how the medicines work and they work very well.” |
| Duration | “Now if you said to me, ‘How long do I need to do this?’ we'll talk about that, but given what you've talking about and all, I'd probably be saying probably about a year is how long we would keep you on antidepressant [1 s], but let's see how you do first. Okay?” |
| Costs | “Prozac is a medication that's been around for a long time and has recently gone generic. And the importance of that for you is it's cheap, okay?” |
| Problems or barriers to use | “The other thing is, if you get insomnia, which is a side effect with this medication then, more insomnia, what you would be sure to do is not take the second pill just before you go to bed. You want to take one in the morning and one in the afternoon, eight hours later, so you're … you're not taking it just before you would lie down to go to bed.” |
| What to do if you miss a dose | “… on the fourth day take one in the morning and one eight hours later … If you miss a dose, let it go … Don't double up, okay?” |
Among the instructional messages previously demonstrating an association with adherence, physicians stated that antidepressants must be taken for 2 to 4 weeks for a noticeable effect in 69.8% of visits, and that patients must take medication daily in 68.2%. Physicians gave specific instructions about what to do to resolve questions/concerns regarding antidepressants in 25.6% of visits. Physicians rarely advised SPs to continue to take the medicine even if they were feeling better (5.4%), or to continue to take the medication until further review (i.e., do not stop taking antidepressant without checking with the physician) (3.9%). Physicians gave an average of 1.7 instructional messages (SD=0.9) during consultations.
As shown in Table 3, SPs who presented with major depression symptoms received less information about antidepressant medications (P =.01) and fewer instructional messages (P =.004) than those who presented with adjustment disorder. In addition, older (P =.01) and solo/private practice (P =.02) physicians provided significantly less information to patients.
Table 3.
Generalized Estimating Equations Predicting Physician Provision of Drug Information and Instructional Messages
| Variables* | Provision of Drug Information | Instructional Messages | ||
|---|---|---|---|---|
| β | P | β | P | |
| Medical condition (depression) | −0.41 | .01 | −0.51 | .004 |
| Physician age | −0.01 | .002 | −0.01 | .25 |
| Physician gender (male) | 0.07 | .19 | 0.04 | .69 |
| Physician ethnicity (Caucasian) | 0.06 | .31 | 0.03 | .79 |
| HMO | 0.00 | .97 | 0.12 | .60 |
| Group | −0.01 | .92 | −0.02 | .87 |
| Solo/Private | −0.20 | .02 | −0.16 | .22 |
| Number of patients seen | 0.01 | .73 | 0.02 | .24 |
| Brand-specific drug request | 0.25 | .34 | 0.74 | .21 |
| General drug request | 0.40 | .07 | 1.28 | .02 |
| Office visit duration (minutes) | 0.01 | .11 | 0.01 | .02 |
| Follow-up (within 2 wk) | −0.06 | .46 | 0.36 | .007 |
Results for each SP are not displayed in the table.
DISCUSSION
In this study of physician-SP encounters in which antidepressants were prescribed, physicians typically mentioned information about the drug's name, purpose, and side effects. While these elements are important, depressed patients also need information about the duration of pharmacotherapy and onset of clinical effect.3,16 Physicians failed to provide information about the anticipated duration of antidepressant therapy and expected delay in onset of action in 65% and 30% of the consultations, respectively. In addition, few SPs were told how to resolve concerns, to continue medicine even if feeling better, and not to skip medication without talking to the doctor: information that might be provided during follow up visits. As good adherence for 6 to 9 months is critical to achieving optimal depression outcomes, messages such as these are key.
This study shows that patients who are prescribed antidepressants for the first time may leave their physician offices without important drug information. Although it may not be beneficial for patients to be inundated with all types of drug information during brief initial visits (which could lead to information overload), patients should arguably receive certain basic elements of information, particularly those that have been associated with improved adherence to therapy.4,17,18 Mechanisms need to be in place to ensure that patients: (1) are informed about these critical elements during the initial visit and (2) have access to other important but less crucial information, if desired. For example, patients could receive pamphlets or brochures, or be directed to websites detailing antidepressant information at the end of their office visit. Physicians' office staff could review new prescriptions and answer questions patients may have concerning their medications. Alternatively, pharmacists could be encouraged to provide education and counseling to patients prescribed antidepressants. In fact, current thinking in pharmacy supports such a role for pharmacists.19
Regarding depression symptom severity, we found that physicians provided less information to SPs presenting with major depression than to those with adjustment disorder and depressed mood. This result seems counter-intuitive because the absolute benefit of a therapy usually increases with disease severity; one would expect physicians to encourage their more depressed patients to take medicine and therefore provide them with more information.20 However, this result is similar to Meredith and Mazel's11 finding that encounters with major depression patients contained significantly less psychotherapeutic depression counseling (compared with encounters with subthreshold depression patients). During initial encounters with seriously depressed patients, physicians may appropriately focus more on history-taking, assessing patients' symptoms and lifestyle issues, and making a diagnosis.11,21 In addition, physicians may assume that the more depressed patients are more limited cognitively in what they can absorb, and thus deliver less information at least initially.22,23 Physicians may plan to discuss additional issues with the more depressed patients during follow-up visits. Alternatively, physicians may be proactive about giving lots of information (including cost information) to patients when the medicine is not really indicated.
This study also sheds light on reported discrepancies between physician and patient reports about the amount and kinds of drug information discussed in primary care visits. Bull et al.7 found that 72% of physicians reported that they usually told patients to take antidepressants for at least 6 months, and 29% reported that they initially do not specify treatment duration. In contrast, 34% of patients reported that they were told by their prescribing physicians to take the antidepressants for at least 6 months, and 56% reported receiving no instructions about expected therapy duration. Our results (in which physicians provided information about antidepressant treatment duration in 35% of interactions) comport more closely with the recollections of patients (rather than doctors) in the study by Bull et al.7
Previous literature shows that patients want to discuss certain topics of information about drugs. For example, in 1 study 63% of patients reported a desire to talk with their physicians about their out-of-pocket costs, but only 15% reported ever having this discussion with their physicians.24 Our findings suggest that patients' reports about discussions pertaining to costs are accurate: physicians only mentioned cost information in 21% of visits. Patients' out-of-pocket costs may be a pertinent factor that influences the use of antidepressants. Donohue et al.25 found that patients who were facing a copayment of more than $15 for an antidepressant were much less likely to initiate medication therapy than those facing a copay of $5 or less. Physician-patient communication about out-of-pocket drug costs at the time of prescribing may help patients find means to pay for the medication, or lead the physician to prescribe a less expensive drug. However, given the present system it may be difficult for physicians to stay knowledgeable of drug costs associated with various pharmaceutical benefit structures.26
This study has several limitations
First, although we provided illustrative examples of physician communication, we did not assess the quality of information physicians provided to SPs. Physicians may have provided various degrees of information or may have provided the information using technical jargon that might be difficult for a patient to understand. Second, physicians who agreed to participate in this study may have greater than average confidence in their clinical communication skills. Thus, study physicians may perform patient education and other communicative behaviors better than average physicians. Third, while SPs offer many advantages, they may not reflect typical patients seen in an average practice. Next, the study examines efforts to educate that accompany prescribing and does not address antidepressant discussions in any other context. Finally, we analyzed first visits with no opportunity for follow-up. The usual practice is for clinicians to follow-up patients being initiated on antidepressants within 2 weeks. It is possible that other domains of information giving would occur during these follow-up visits. It could also be argued that it would not be appropriate for clinicians to discuss all 11 domains of medication prescribing during a single visit. Since depression care occurs over time, information-giving may appropriately occur over time. Conversely, it is possible that even less information will be provided during follow-up visits. Future studies should explore the continuum of communication over the entire course of treatment.
CONCLUSION
Patient education begins in the doctor's office, but should not end there. This study indicates that physicians may regularly fail to provide important information to patients starting antidepressants. Encounters in which patients are not told that antidepressants do not work immediately and that long-term treatment is required may represent missed opportunities for enhancing medication adherence and promoting safe use. Further research is needed to identify effective interventions for assuring that patients starting antidepressants are armed with the critical information needed to maximize the likelihood of a favorable outcome.
Acknowledgments
This work was supported by a research supplement for underrepresented minorities, and grant 5 R01 MH064683-03 from the National Institute of Mental Health. We are grateful for the individuals who assisted with this project: Sheila Krishnan and Jason Mudrock.
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Rush AJ, Golden WE, Hall GW, et al. Depression in Primary Care: Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services; 1993. [Google Scholar]
- 3.Stimmel GL. How to counsel patients about depression and its treatment. Pharmacotherapy. 1995;15:100S–4S. [PubMed] [Google Scholar]
- 4.Lin EH, Von Korff M, Katon W, et al. The role of the primary care physician in patients' adherence to antidepressant therapy. Med Care. 1995;33:67–74. doi: 10.1097/00005650-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Nemeroff CB. Improving antidepressant adherence. J Clin Psychiatry. 2003;64:25–30. [PubMed] [Google Scholar]
- 6.Vergouwen AC, Bakker A, Katon WJ, Verheij TJ, Koerselman F. Improving adherence to antidepressants: a systematic review of interventions. J Clin Psychiatry. 2003;64:1415–20. doi: 10.4088/jcp.v64n1203. [DOI] [PubMed] [Google Scholar]
- 7.Bull SA, Hu XH, Hunkeler EM, et al. Discontinuation of use and switching of antidepressants: influence of patient-physician communication. JAMA. 2002;288:1403–9. doi: 10.1001/jama.288.11.1403. [DOI] [PubMed] [Google Scholar]
- 8.Brody DS, Thompson TL, Larson DB, Ford DE, Katon WJ, Magruder KM. Recognizing and managing depression in primary care. Gen Hosp Psychiatry. 1995;17:93–107. doi: 10.1016/0163-8343(94)00093-s. [DOI] [PubMed] [Google Scholar]
- 9.Bultman DC, Svarstad BL. Effects of physician communication style on client medication beliefs and adherence with antidepressant treatment. Patient Educ Couns. 2000;40:173–85. doi: 10.1016/s0738-3991(99)00083-x. [DOI] [PubMed] [Google Scholar]
- 10.Sleath B, Rubin RH, Huston SA. Hispanic ethnicity, physician-patient communication, and antidepressant adherence. Compr Psychiatry. 2003;44:198–204. doi: 10.1016/S0010-440X(03)00007-5. [DOI] [PubMed] [Google Scholar]
- 11.Meredith LS, Mazel RM. Counseling for depression by primary care providers. Int J Psychiatry Med. 2000;30:343–65. doi: 10.2190/T0YP-U28Q-52Q4-G28M. [DOI] [PubMed] [Google Scholar]
- 12.Sleath BL, Williams JW. Hispanic ethnicity, language, and depression: physician-patient communication and patient use of alternative treatments. Int J Psychiatry Med. 2004;34:235–46. doi: 10.2190/VQU1-QYWT-XW6Y-4M14. [DOI] [PubMed] [Google Scholar]
- 13.Sleath B, Rubin RH. Gender, ethnicity, and physician-patient communication about depression and anxiety in primary care. Patient Educ Couns. 2002;48:243–52. doi: 10.1016/s0738-3991(02)00177-5. [DOI] [PubMed] [Google Scholar]
- 14.Kravitz RL, Epstein RM, Feldman MD, et al. Influence of patients' requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA. 2005;293:1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med. 1995;41:1241–54. doi: 10.1016/0277-9536(95)00061-b. [DOI] [PubMed] [Google Scholar]
- 16.Bucci KK, Possidente CJ, Talbot KA. Strategies to improve medication adherence in patients with depression. Am J Health Syst Pharm. 2003;60:2601–5. doi: 10.1093/ajhp/60.24.2601. [DOI] [PubMed] [Google Scholar]
- 17.Ley P. Memory for medical information. Br J Soc Clin Psychol. 1979;18:245–55. doi: 10.1111/j.2044-8260.1979.tb00333.x. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan EM. Antidepressant noncompliance as a factor in the discontinuation syndrome. J Clin Psychiatry. 1997;58(suppl. 7):31–6. [PubMed] [Google Scholar]
- 19.Hepler CD, Strand LM, Tromp D, Sakolchai S. Critically examining pharmaceutical care. J Am Pharm Assoc. 2002;42(suppl. 1):S18–S19. doi: 10.1331/108658002764653648. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell PM, Warlow CP. Prediction of benefit from carotid endarterectomy in individual patients: a risk-modelling study. European carotid surgery trialists' collaborative group. Lancet. 1999;353:2105–10. doi: 10.1016/s0140-6736(98)11415-0. [DOI] [PubMed] [Google Scholar]
- 21.Callahan EJ, Jaen CR, Crabtree BF, Zyzanski SJ, Goodwin MA, Stange KC. The impact of recent emotional distress and diagnosis of depression or anxiety on the physician-patient encounter in family practice. J Fam Pract. 1998;46:410–18. [PubMed] [Google Scholar]
- 22.Harvey PO, Le Bastard G, Pochon JB, et al. Executive functions and updating of the contents of working memory in unipolar depression. J Psychiatr Res. 2004;38:567–76. doi: 10.1016/j.jpsychires.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 23.Palmer BW, Boone KB, Lesser IM, Wohl MA, Berman N, Miller BL. Neuropsychological deficits among older depressed patients with predominantly psychological or vegetative symptoms. J Affect Disord. 1996;41:17–24. doi: 10.1016/0165-0327(96)00059-6. [DOI] [PubMed] [Google Scholar]
- 24.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290:953–8. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 25.Donohue JM, Berndt ER, Rosenthal M, Epstein AM, Frank RG. Effects of pharmaceutical promotion on adherence to the treatment guidelines for depression. Med Care. 2004;42:1176–85. doi: 10.1097/00005650-200412000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Shrank WH, Young HN, Ettner SL, Glassman P, Asch SM, Kravitz RL. Do the incentives in 3-tier pharmaceutical benefit plans operate as intended? Results from a Physician Leadership Survey. Am J Manage Care. 2005;11:16–22. [PubMed] [Google Scholar]