Abstract
BACKGROUND
Bedside rationing by physicians is controversial. The debate, however, is clouded by lack of information regarding the extent and character of bedside rationing.
DESIGN, SETTING, AND PARTICIPANTS
We developed a survey instrument to examine the frequency, criteria, and strategies used for bedside rationing. Content validity was assessed through expert assessment and scales were tested for internal consistency. The questionnaire was translated and administered to General Internists in Norway, Switzerland, Italy, and the United Kingdom. Logistic regression was used to identify the variables associated with reported rationing.
RESULTS
Survey respondents (N =656, response rate 43%) ranged in age from 28 to 82, and averaged 25 years in practice. Most respondents (82.3%) showed some degree of agreement with rationing, and 56.3% reported that they did ration interventions. The most frequently mentioned criteria for rationing were a small expected benefit (82.3%), low chances of success (79.8%), an intervention intended to prolong life when quality of life is low (70.6%), and a patient over 85 years of age (70%). The frequency of rationing by clinicians was positively correlated with perceived scarcity of resources (odds ratio [OR]=1.11, 95% confidence interval [CI] 1.06 to 1.16), perceived pressure to ration (OR=2.14, 95% CI 1.52 to 3.01), and agreement with rationing (OR=1.13, 95% CI 1.05 to 1.23).
CONCLUSION
Bedside rationing is prevalent in all surveyed European countries and varies with physician attitudes and resource availability. The prevalence of physician bedside rationing, which presents physicians with difficult moral dilemmas, highlights the importance of discussions regarding how to ration care in the most ethically justifiable manner.
Keywords: health care rationing, health resources, attitude of health personnel, ethics, clinical, Europe
Health care rationing, or withholding interventions that could be of benefit on the grounds of scarcity or excessive cost, is controversial.1–4 A specific debate has surrounded the appropriateness of physician bedside rationing. The obligation to advocate for patients,5–11 and lack of trust that physicians will make the right kind of rationing decisions,12 have prompted reservations about physician involvement in health care rationing. Their involvement, however, has also been defended on the grounds that physicians are entrusted with the stewardship of scarce resources,13 could make cost control compatible with patient advocacy,14 and indeed may be in the best position to ration care in an appropriate and justifiable manner.14–16
This debate is hindered by insufficient data regarding whether, and how, rationing takes place in clinical practice.1,15 Descriptive data about what physicians withhold, from whom, and how they make these decisions, can be crucial to make normative judgments about the ethical acceptability of bedside rationing. If one adopts the normative perspective, as we do, that rationing ought to maximize fairness, data can eventually be used to examine whether physicians withhold in a discriminatory or even-handed manner and hence whether or not bedside rationing is morally problematic. If physician reasoning is consistent with practice guidelines, and cognizant of issues of fairness, then bedside rationing might be an ethically acceptable component of the processes dictating the distribution of medical resources.
Studies have explored physicians' opinions regarding rationing,17–20 their choices in hypothetical cases,21–24 as well as specific instances of rationing behavior.25–27 However, 3 key aspects have not been explored: (1) the frequency of rationing decisions made by physicians in clinical practice, (2) the type of interventions to which these decisions are applied, and (3) the criteria used in making these decisions.
To address these 3 aspects, we conducted an international survey of general physicians in Italy, Norway, Switzerland, and the United Kingdom, 4 European countries offering universal access to health care through very different systems, with per capita expenditure on health care ranging from $3,322 in Switzerland to $1,989 in the United Kingdom.28
PARTICIPANTS AND METHODS
Participants
General physicians were identified through the 2002 official list of the Norwegian Medical Association, the Swiss Medical Association, published listings of UK general practitioners and general physicians, and regional listings of Italian general practitioners and members of the Italian Society of Internal Medicine. A random sample of 400 individuals was drawn in each country in proportions of general practitioners and General Internists reflecting that of each national physician population. This sample was chosen to capture similar physician populations, who do the same kind of work in general internal medicine, in both in patient and outpatient care.
Survey Methods
Because of the controversial nature of rationing and the lack of clarity about its definition, we did not use the word “rationing” in the questionnaire. Although some regard rationing restrictively as dependent on following set rules and criteria, our definition of rationing was based on the more comprehensive definition proposed by Ubel and Goold,29 who define rationing as “any implicit or explicit mechanisms that allow people to go without beneficial services.” Based on this definition, we asked respondents exclusively about those decisions they had made that led to patients going “without beneficial services.” We specified that we meant decisions based on costs, in order to avoid confusion with situations where beneficial services were withheld because patients did not want them.
To develop the survey instrument, we started with a literature review using PubMed's database of Medical Subjects Headings and combining the following search terms: “resource allocation,” “health care rationing,” “attitudes of health personnel,” “professional practice,” and “physician's practice patterns.” Where existing survey items were found in the literature, they were included in our survey tool. Validated items were degree of agreement with the following statement: “Physicians should adhere to clinical guidelines that discourage the use of interventions that have a small proven advantage over standard interventions but cost much more,” and the following question: “On balance do the financial incentives in your main practice: favour reducing services to patients, favor expanding services to patients, favour neither?,”30 as well as a number of listed criteria for rationing.31
Two new items were developed based on a previously published questionnaire.27 These items were “cost to society is important in my decision to use or not to use an intervention,” and “I should sometimes deny beneficial but costly services to certain patients because resources should go to other patients that need them more.” Other new items grew out of a prior study in which we performed qualitative analysis of ethical dilemmas related to justice and scarcity reported by Internists in the U.S.32,33 In this prior study, we categorized comments made by physicians regarding their response to scarcity-related ethical difficulties. New items were independently rated for content validity by 2 ethicists with expertise in the ethics of rationing. The questionnaire was refined following these comments, and piloted on a convenience sample of 96 physicians in the United States, United Kingdom, and Switzerland. A cognitive questionnaire was appended to the pilot, asking respondents whether they had found any of the questions unclear, or awkward, and whether any questions had made them uncomfortable. Each scale was tested for internal consistency following the pilot, again on the entire sample, and for each national sample. Scale consistency was similar among the national samples. The questionnaire was translated into Norwegian, French, German, and Italian, back translated for accuracy, and checked by bilingual physicians for equivalence. The survey instrument is available online.
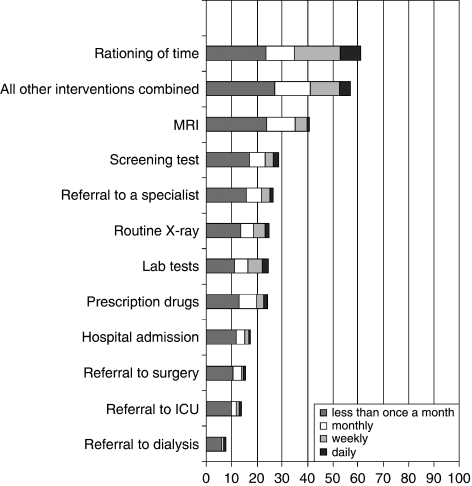
The Rationing scale, developed to explore physician reported rationing, was worded as follows: “During the last 6 months, how often did you personally refrain, because of cost to the health care system, from using the following interventions when they would have been the best intervention for your patient?” Ten listed interventions were chosen to represent the range of interventions across the spectrum of care from prevention to life-sustaining treatment (see Fig. 1). A separate item asked respondents about rationing of time in the prior 6 months. Response options were as follows: never or not applicable (0), less than once a month (1), monthly (2), weekly (3), and daily (4). The summed scale scores range was 0 to 40.
FIGURE 1.
Percentage of physicians reporting rationing in the prior 6 months. Percentages shown exclusive of missing data.
An Agreement with Rationing scale was composed of the following items “Cost to society is important in my decisions to use or not to use an intervention,” “Physicians should adhere to clinical guidelines that discourage the use of interventions that have a small proven advantage over standard interventions but cost much more,” and “I should sometimes deny beneficial but costly services to certain patients because resources should go to other patients that need them more.” Responses were on a 5-point Likert scale ranging from “strongly agree” (5) to “strongly disagree” (1). The summed scale scores range was 3 to 15.
A Perceived Scarcity scale was based on items worded as follows: “During the last 6 months, how often were you unable to obtain the following services for your patients when you thought they were necessary (this includes unacceptable waiting times)?” Listed items included surgery, referral to a specialist, admission to a hospital, access to mental health services, admission to a nursing home, endoscopy for colon cancer screening, rehabilitation for stroke, prescription drugs, referral to ICU, referral to dialysis, and services for patients at the end of life. These items used the same response options as the rationing scale. Scale range was 0 to 44.
Perceived pressure to ration was assessed using the following item: “In the last 6 months, how often have you felt under pressure to deny an expensive intervention that you thought was indicated?” These items used the same response options as the Rationing scale.
Participants were contacted by mail, and told about the aims of the study in a cover letter. Questionnaires were self-administered by the respondents. To maximize response rate, cover letters were addressed by local researchers and a repeat mailing was sent, including an incentive of €10, or the closest equivalent in local currency.34 Questionnaires were mailed to 1,600 physicians. Data collection was open from February 2003 to June 2004.
Human Subjects Protection
Participation was voluntary and responses were made anonymous before analysis to ensure confidentiality. Approval was given by the IRB of the National Institute of Child Health and Development at the U.S. National Institutes of Health, and by the Trent Multi-Centre Research Ethics Committee in the United Kingdom. This study was designated exempt from ethics committee review by IRBs in Norway, Italy, and Switzerland.
Statistical Analysis
Data were analyzed using descriptive statistics, and bivariate correlations were analyzed using Pearson's χ2 or Kruskall-Wallis tests as appropriate. We selected a significance level of .01 (2-tailed). Logistic regression was used to identify variables independently associated with reported rationing on the Rationing scale, and with rationing of time. The models were built using the variables that were found to be associated with reported rationing in bivariate analysis.
RESULTS
Respondents
Respondents (N = 656, 43% of eligible sample) ranged in age from 28 to 82, they had been in practice for an average of 25 years, and 38.4% were at least partly hospital based (Table 1). Respondents were predominantly male (85%), with the proportion of women ranging from 42.1% under the age of 30 to 7.8% from 61 to 70 years of age.
Table 1.
Respondent Characteristics
| Physicians (N = 656) | |
|---|---|
| Characteristics | |
| Age (y) | 28 to 82 (mean 51) |
| Years in practice | 1 to 62 (mean 25) |
| Male | 546 (85%) |
| Specialty | |
| Family medicine | 195 (30%) |
| General medicine | 188 (29%) |
| Internal medicine | 179 (28%) |
| Country of practice | |
| Italy | 139 (21%) |
| Norway | 222 (34%) |
| Switzerland | 183 (28%) |
| UK | 112 (17%) |
| Primary practice site | |
| Hospital | 258 (38%) |
| Solo practice | 182 (28%) |
| Primary care group practice | 164 (25%) |
| Multispecialty group | 23 (4%) |
| Other | 28 (4%) |
| Admitting hospital | |
| Public | 572 (94%) |
| Private | 21 (3%) |
| For-profit | 81 (17%) |
| Not-for–profit | 406 (82%) |
| Teaching hospital | 264 (46%) |
Percentages shown exclusive of missing data, and rounded to the nearest whole number.
Reported Rationing
Rationing of interventions was reported by 56.3% of respondents for the prior 6 months (Fig. 1). The most frequently rationed interventions were MRI (40.9%) and screening tests (28.6%), and the least frequently rationed referral to ICU (13.7%) and dialysis (15.4%). The mean score on the Rationing scale was 3.4 out of a maximum of 40 for the total sample, with a mean score of 6.4 for those physicians who reported rationing (Cronbach's α=0.90). A score of 6 could signify rationing each of 6 interventions less than once a month, or rationing 1 intervention daily and 1 intervention monthly. Among physicians who reported rationing, the median was once a month for lab tests and less than once a month for all other interventions. However, rationing was reported as often as daily for all interventions. Rationing of time was reported by 61.3% of respondents.
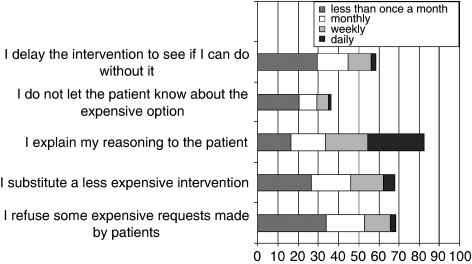
When asked about strategies for rationing, a majority of respondents (82.4%) reported that they explained their reasoning to their patients at least sometimes when avoiding an expensive intervention. However, 36.5% also reported that they sometimes did not let their patient know about the expensive alternative (Fig. 2).
FIGURE 2.
Strategies used to limit expensive interventions. Percentages shown exclusive of missing data.
The most frequently reported criteria for rationing decisions were a small expected benefit (82.3%), low chances of success (79.8%), intention to prolong life when quality of life is low (70.6%), and age over 85 years (70%) (Table 2).
Table 2.
Criteria Influencing the Use of Expensive Interventions
| Criterion* | Percentage of Respondents | ||
|---|---|---|---|
| Less Likely | No Change | More Likely | |
| Intent | |||
| The aim is to prolong the life of a patient whose quality of life you judge to be low | 71 | 17 | 12 |
| The aim is to improve quality of life in a patient whose life expectancy is short | 35 | 30 | 35 |
| Intervention | |||
| The benefit to the patient is small | 82 | 1 | 7 |
| Chances of success for the intervention are low | 80 | 14 | 6 |
| While you think the patient would benefit, the evidence base for the intervention is lacking | 58 | 29 | 14 |
| The intervention is primary prevention | 26 | 33 | 41 |
| Condition | |||
| The condition is attributable to smoking | 18 | 77 | 5 |
| The condition is attributable to a dangerous sport | 15 | 79 | 6 |
| The condition is attributable to pregnancy | 7 | 67 | 26 |
| The condition requires chronic care | 30 | 51 | 19 |
| Patient | |||
| The patient is over 85 | 70 | 24 | 6 |
| The patient is frail | 63 | 26 | 10 |
| The patient is cognitively impaired | 50 | 45 | 5 |
| The patient holds an important position in society | 7 | 81 | 12 |
| The patient asks for the intervention | 12 | 45 | 42 |
| The patient is poor | 8 | 82 | 10 |
| The patient will not work again | 15 | 78 | 7 |
A patient you are treating would benefit from an intervention. This intervention is very expensive. It is paid for by public money, or by a private insurer, or both. Under these circumstances, do the following factors make you more or less likely to use this intervention?
Percentages shown exclusive of missing data, and rounded to the nearest whole number.
Personal Attitudes Toward Rationing
On the Agreement with Rationing scale (Cronbach's α=0.60), 82.3% of respondents showed some degree of agreement, with a median score of 10 (range=3 to 15). Over a third of respondents (36.6%) agreed that they should sometimes deny beneficial but costly services. Half (51.2%) agreed that cost to society was important in their decision to use or not to use an intervention. Two-thirds (68.7%) agreed that physicians should adhere to clinical guidelines that discourage the use of interventions that have a small proven advantage over standard interventions but cost much more.
Perceptions of System-wide Rationing
Perceived Scarcity (Cronbach's α=0.84) was reported by 87.6% of respondents. Perceived pressure to ration was reported to have occurred in the prior 6 months by 46.2% of respondents. In addition, 44% agreed that their job or financial situation was threatened by current pressures to contain costs in health care. Despite this, 73.3% felt free to utilize resources in their patients' best interest.
Determinants of Reported Rationing
In bivariate analysis, physicians' age, gender, specialty, site of practice (in patient or outpatient, public or private admitting hospital, teaching admitting hospital), appointment with a university department, and years in practice since graduation were not associated with the degree of reported rationing, based on the Rationing scale. Degree of rationing was positively associated with number of hours a week in patient care, perceived scarcity, perceived pressure to ration, and agreement with rationing. There was a negative association between the degree of rationing and length of waiting time for an appointment, perceived freedom, and working in Norway or the United Kingdom.
A logistic regression model of factors associated with reported rationing included both personal attitudes toward rationing as well as perceptions of rationing at the system-wide level. Physicians were more likely to report rationing if they perceived more scarcity (odds ratio [OR] = 1.11, 95% confidence interval [CI] 1.06 to 1.16), or more pressure to ration (OR = 2.14, 95% CI 1.52 to 3.01), and if they agreed more strongly with rationing (OR = 1.13, 95% CI 1.05 to 1.23). Physicians from Norway (OR = 2.61, 95% CI 1.34 to 5.06), Italy (OR = 3.62, 95% CI 1.65 to 7.91), and Switzerland (OR=5.1, 95% CI 2.28 to 11.68) were more likely to report rationing than those in the United Kingdom.
Reported rationing of time was not associated with physicians' age, gender, years in practice since graduation, type of admitting hospital, number of patients cared for, or hours a week in inpatient care in bivariate analysis. It was positively associated with working in a rural area, in an outpatient setting, number of hours in outpatient care, being under pressure to ration interventions, reporting less freedom to utilize resources in patients' best interest, and reporting scarcity, rationing of interventions, and agreement with rationing. There was a negative association between the degree of reported rationing of time and working in Italy, being specialized in internal medicine, and fearing that denying care could jeopardize the doctor-patient relationship.
In a logistic regression model of factors associated with rationing of time, physicians were more likely to report rationing of time if they reported more scarcity (OR = 1.1, 95% CI 1.02 to 1.18), and less likely to do so if they practiced in Italy (OR = 0.13, 95% CI 0.04 to 0.43).
DISCUSSION
Bedside rationing is reported by physicians in all European countries studied. Physicians who personally agree with rationing, perceive more pressure to ration, and perceive more scarcity are more likely to report rationing. The interventions reported as being rationed the most frequently are personal time spent with patients, MRI, screening tests, lab tests, and prescription drugs. Although the most frequently mentioned criteria were a small expected benefit, and low chances of success, a majority of respondents also reported being more likely to refrain from using an intervention if the patient was over age 85.
Our study has several limitations. Using self-reports may have led to an underestimation of actual bedside rationing given its controversial nature. Additionally, self-reports will only capture instances of rationing of which practitioners are aware. Moreover, information gathered in the survey about withheld services did not include details regarding the particular circumstances. Cases where physicians may have reassessed medical indications so they are better aligned to match available resources are thus excluded. As we only surveyed general physicians, generalizations to other medical specialties, or to other health care systems should be cautious. Finally, the response rate was modest, as is often the case for physicians35 and questionnaires addressing sensitive topics.34 Nonrespondent bias is most likely to be associated either with lack of time, which we would expect yields an underestimation of the rationing of time, or with lack of interest in the topic, which we would expect to yield an overestimation of reported rationing of interventions. Reluctance to report a controversial practice could also have led to underreporting of bedside rationing. However, extrapolating our results to a response rate of 100%, and considering all nonrespondents to report no rationing results in a percentage of physicians reporting rationing of interventions of 23%. One concern could be that the associations between variables could be affected by nonresponse bias. Variables independently associated with reported rationing were perceived scarcity, pressure to ration, agreement with rationing, and country of practice. If nonresponse were due primarily to lack of interest in the topic, then we could expect overestimation of pressure to ration. As this would also likely be associated with overestimation of reported rationing, however, the association between these 2 variables may not be affected.
Our results complement studies that have examined clinical rationing such as nonreferral to dialysis.25,26 While it has been suggested that physicians often deny scarcity,36 our findings indicate that physicians are aware of personally denying some modicum of benefit to their patients. These findings will need to be supplemented with additional data gathered from sources such as medical records and administrative data sets. However, despite the exploratory nature of this study, our results raise a number of intriguing points.
We found significant differences between countries regarding the frequency of reported rationing. While one might expect that physicians in countries that spend more money per capita would report rationing less, this does not appear to be the case. Physicians in Switzerland, where the most is spent, report the most rationing. One plausible explanation is that, when more leeway is left to physicians by the structure of their health care system, a larger share of the responsibility for rationing falls to them. Thus, they may indeed more often “personally refrain from using interventions,” which a more rule-bound system would simply not have given them the discretion to use. Whether more leeway for clinical decisions regarding rationing is a favorable arrangement depends upon judgments about where rationing decisions ought to take place and upon clinical outcomes that we did not measure here. Moreover, we cannot know precisely all the factors that dictate the reported frequency of rationing. In addition to scarcity, or to agreement with rationing, it could also be a function of how often the clinical need arises.
This study has several implications. First, our results suggest an interaction between resource allocation at the levels of health care systems and individual provivders. This interaction may occur at various levels of health care organization including national and more local levels. The literature on practice variation shows that the availability of resources such as hospital and ICU beds varies geographically within a country and that utilization rates parallel this availability.37 Our finding that physicians's self-reports of rationing correlate with their perception of scarcity helps to provide an insight into this relationship. At a national level, we found that Italy, the country with the highest number of physicians per 1,000 population,38 is also where our respondents reported the least rationing of time. This suggests that manpower allocation decisions at the system level, whether intentionally or otherwise, impact reported bedside rationing.
Second, it seems that both health care systems that are more centralized, as exemplified by the United Kingdom, and those that are more market based, as exemplified by Switzerland,39 include clinical rationing behavior, as judged by physician self-reports. Of what interest might the findings in this study be to practitioners and patients in the United States where rationing is often thought to be driven by inability to pay due to uninsurance40 or by insurance coverage rules?41 While expansion of insurance may reduce inequities in access to care, it will not eliminate rationing. One can only hope that the pattern of rationing might be fairer. In this regard, this study is aimed at providing initial insights that may yield fair rationing strategies.
Overall, our study indicates that bedside rationing is ubiquitous but its extent and patterns vary with system-wide factors. Those who consider bedside rationing by physicians to be ethically unacceptable can glean from our findings that it would be prudent to promote aspects of any health care delivery systems that reduce pressure for physicians to take responsibility personally for the cost of care. But they might also be reassured by the finding that those interventions that are reportedly rationed involve nonvital benefits and interventions for which there are clinical alternatives.
While it is reassuring to see so few physicians report rationing based on poverty, criteria such as a patient's work status may suggest worrisome practices. While rationing criteria such as cognitive impairement may be viewed as discriminatory, they may, alternatively, reflect concerns for quality of life that are shared by patients and their families. In sum, physicians report a range of criteria for forgoing medical interventions that appear to be more and less equitable. These findings highlight the need for a more detailed attention both to the factors that do and to those that should influence rationing decisions. Given the prevalence of rationing, the public may be well served by more explicit discussion of how best to ration care at the bedside in an ethically justifiable manner. The concepts and skills required for fair rationing would also need to be included in medical curricula, which typically do not currently include such training.
Acknowledgments
The authors wish to thank Ole Norheim and Rein Vos for their review of the survey tool, Bruce Brinkley, Timothy Carey, Marie Neeser, Marc-Andre Raetzo, and Dan Sulmasy for their help in the pilot, the NIH Clinical Center Library for their outstanding translation service, MEDTAP international for their excellent data collection work, and Ezekiel Emanuel and the anonymous reviewers for invaluable criticism of the manuscript. We also wish to thank all the physicians who took the time to complete the questionnaire.
This work was funded by the Department of Clinical Bioethics at the National Institutes of Health, and was conducted while S.A.H. was a fellow at this Department. S.A.H. was funded in part by the University Hospitals of Geneva, by the Oltramare Foundation, and by the Centre Lémanique d'Ethique. The views expressed here are the authors' own, and not necessarily those of the University Hospitals of Geneva, the Oltramare Foundation, or the Centre Lémanique d'Ethique.
The funding sources were not involved in the study design, the collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
S.A.H. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supplementary Material
The following supplementary material is available for this article online at http://www.blackwell-synergy.com
Values at the Bedside. A Survey of Physicians Regarding Ethical Dilemmas in Clinical Practice.
REFERENCES
- 1.Asch DA, Ubel PA. Rationing by any other name. N Engl J Med. 1997;336:1668–71. doi: 10.1056/NEJM199706053362309. [DOI] [PubMed] [Google Scholar]
- 2.Relman A. Use of medical resources—overview. Prev Med. 1990;19:688–92. doi: 10.1016/0091-7435(90)90066-s. [DOI] [PubMed] [Google Scholar]
- 3.Bloche MG, Jungman ER. The “R” word. J Contemp Health Law Policy. 2002;18:633–9. [PubMed] [Google Scholar]
- 4.Coulter A, Ham C. The Global Challenge of Health Care Rationing. Buckingham: Open University Press; 2000. [Google Scholar]
- 5.Sulmasy DP. Physicians, cost control, and ethics. Ann Intern Med. 1992;116:920–6. doi: 10.7326/0003-4819-116-11-920. [DOI] [PubMed] [Google Scholar]
- 6.Hiatt HH. Protecting the medical commons: who is responsible? N Engl J Med. 1975;293:235–41. doi: 10.1056/NEJM197507312930506. [DOI] [PubMed] [Google Scholar]
- 7.Loewy EH. Cost should not be a factor in medical care. N Engl J Med. 1980;302:697. doi: 10.1056/NEJM198003203021226. [DOI] [PubMed] [Google Scholar]
- 8.Levinski N. The doctor's master. N Engl J Med. 1983;311:1573–5. doi: 10.1056/NEJM198412133112412. [DOI] [PubMed] [Google Scholar]
- 9.Pellegrino ED. Managed care at the bedside: how do we look in the moral mirror? Kennedy Inst Ethics J. 1997;7:321–30. doi: 10.1353/ken.1997.0036. [DOI] [PubMed] [Google Scholar]
- 10.Askin WJ. Bedside rationing. CMAJ. 2002;166:711. [PMC free article] [PubMed] [Google Scholar]
- 11.Weinstein MC. Should physicians be gatekeepers of medical resources? J Med Ethics. 2001;27:268–74. doi: 10.1136/jme.27.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veatch RM. Who should manage care? The case for patients. Kennedy Inst Ethics J. 1997;7:391–401. doi: 10.1353/ken.1997.0041. [DOI] [PubMed] [Google Scholar]
- 13.Morreim E. Balancing Act; The New Medical Ethics of Medicine's New Economics. Dordrecht: Kluwer Academic Publishers; 1991. [Google Scholar]
- 14.Pearson SD. Caring and cost: the challenge for physician advocacy. Ann Intern Med. 2000;133:148–53. doi: 10.7326/0003-4819-133-2-200007180-00014. [DOI] [PubMed] [Google Scholar]
- 15.Ubel P. Pricing Life: Why It's Time for Health Care Rationing. In: McGee G, Caplan A, editors. Basic Bioethics. Cambridge, MA: The MIT Press; 2001. [Google Scholar]
- 16.Daniels N. What is the obligation of the medical profession in the distribution of health care? Soc Sci Med [F] 1981;15F:129–33. [PubMed] [Google Scholar]
- 17.Baines DL, Tolley KH, Whynes DK. The ethics of resource allocation: the views of general practitioners in Lincolnshire, U.K. Soc Sci Med. 1998;47:1555–64. doi: 10.1016/s0277-9536(98)00256-1. [DOI] [PubMed] [Google Scholar]
- 18.Cooke L, Hutchinson M. Doctors' professional values: results from a cohort study of United Kingdom medical graduates. Med Educ. 2001;35:735–42. doi: 10.1046/j.1365-2923.2001.01011.x. [DOI] [PubMed] [Google Scholar]
- 19.Rosen P, Karlberg I. Opinions of Swedish citizens, health-care politicians, administrators and doctors on rationing and health-care financing. Health Expect. 2002;5:148–55. doi: 10.1046/j.1369-6513.2002.00169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Delden JJ, Vrakking AM, van der Heide A, van der Maas PJ. Medical decision making in scarcity situations. J Med Ethics. 2004;30:207–11. doi: 10.1136/jme.2003.003681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ubel PA, Baron J, Nash B, Asch DA. Are preferences for equity over efficiency in health care allocation “all or nothing”? Med Care. 2000;38:366–73. doi: 10.1097/00005650-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Perneger TV, Martin DP, Bovier PA. Physicians' attitudes toward health care rationing. Med Decis Making. 2002;22:65–70. doi: 10.1177/0272989X0202200106. [DOI] [PubMed] [Google Scholar]
- 23.Ryynanen OP, Myllykangas M, Kinnunen J, Takala J. Doctors' willingness to refer elderly patients for elective surgery. Fam Pract. 1997;14:216–9. doi: 10.1093/fampra/14.3.216. [DOI] [PubMed] [Google Scholar]
- 24.Escher M, Perneger TV, Chevrolet JC. National questionnaire survey on what influences doctors' decisions about admission to intensive care. BMJ. 2004;329:425. doi: 10.1136/bmj.329.7463.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendelssohn DC, Kua BT, Singer PA. Referral for dialysis in Ontario. Arch Intern Med. 1995;155:2473–8. [PubMed] [Google Scholar]
- 26.Wilson R, Godwin M, Seguin R, et al. End-stage renal disease: factors affecting referral decisions by family physicians in Canada, the United States, and Britain. Am J Kidney Dis. 2001;38:42–8. doi: 10.1053/ajkd.2001.25180. [DOI] [PubMed] [Google Scholar]
- 27.Arnesen T, Fredriksen S. Coping with obligations towards patient and society: an empirical study of attitudes and practice among Norwegian physicians. J Med Ethics. 1995;21:158–61. doi: 10.1136/jme.21.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. Countries: selected indicators. Vol. 2005; 2003. Available at http://www.who.int/countries/en/
- 29.Ubel PA, Goold SD. ‘Rationing’ health care. Not all definitions are created equal. Arch Intern Med. 1998;158:209–14. doi: 10.1001/archinte.158.3.209. [DOI] [PubMed] [Google Scholar]
- 30.Sulmasy DP, Bloche MG, Mitchell JM, Hadley J. Physicians' ethical beliefs about cost-control arrangements. Arch Intern Med. 2000;160:649–57. doi: 10.1001/archinte.160.5.649. [DOI] [PubMed] [Google Scholar]
- 31.Ryynanen OP, Myllykangas M, Kinnunen J, Takala J. Attitudes to health care prioritisation methods and criteria among nurses, doctors, politicians and the general public. Soc Sci Med. 1999;49:1529–39. doi: 10.1016/s0277-9536(99)00222-1. [DOI] [PubMed] [Google Scholar]
- 32.DuVal G, Clarridge B, Gensler G, Danis M. A national survey of U.S. internists' experiences with ethical dilemmas and ethics consultation. J Gen Intern Med. 2004;19:251–8. doi: 10.1111/j.1525-1497.2004.21238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hurst SA, Hull SC, DuVal G, Danis M. Physicians' responses to resource constraints. Arch Intern Med. 2005;165:639–44. doi: 10.1001/archinte.165.6.639. [DOI] [PubMed] [Google Scholar]
- 34.Edwards P, Roberts I, Clarke M, et al. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002;324:1183. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–36. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 36.Alexander GC, Werner RM, Ubel PA. The costs of denying scarcity. Arch Intern Med. 2004;164:593–6. doi: 10.1001/archinte.164.6.593. [DOI] [PubMed] [Google Scholar]
- 37.Wennberg JE, MacAndrew Cooper M. The Quality of Medical Care in the United States: a Report on the Medicare Program; the Dartmouth Atlas of Health Care 1999. Chicago, IL: AHA Press; 1999. [PubMed] [Google Scholar]
- 38.OECD. Health Data 2005. 2005.
- 39.Herzlinger RE, Parsa-Parsi R. Consumer-driven health care: lessons from Switzerland. JAMA. 2004;292:1213–20. doi: 10.1001/jama.292.10.1213. [DOI] [PubMed] [Google Scholar]
- 40.Committee on Consequences of Uninsurance. Insuring Health: Care Without Coverage: Too Little Too Late. Washington, DC: National Academy Press; 2002. (Institute of Medicine, ed) [Google Scholar]
- 41.Wynia MK, VanGeest JB, Cummins DS, Wilson IB. Do physicians not offer useful services because of coverage restrictions? Health Aff (Millwood) 2003;22:190–7. doi: 10.1377/hlthaff.22.4.190. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Values at the Bedside. A Survey of Physicians Regarding Ethical Dilemmas in Clinical Practice.