Abstract
OBJECTIVES
Temperature is universally measured in the hospitalized patient, but the literature on hospital-acquired fever has not been systematically reviewed. This systematic review is intended to provide clinicians with an overview of the incidence, etiology, and outcome of hospital-acquired fever.
DATA SOURCES
We searched MEDLINE (1970 to 2005), EMBASE (1988 to 2004), and Web of Knowledge. References of all included articles were reviewed. Articles that focused on children, fever in the developing world, classic fever of unknown origin, or specialized patient populations were excluded.
REVIEW METHODS
Articles were reviewed independently by 2 authors before inclusion; a third author acted as arbiter.
RESULTS
Of over 1,000 studies reviewed, 7 met the criteria for inclusion. The incidence of hospital-acquired fever ranged from 2% to 17%. The etiology of fever was infection in 37% to 74%. Rates of antibiotic use for patients with a noninfectious cause of fever ranged from 29% to 55% for a mean duration of 6.6 to 9.6 days. Studies varied widely in their methodology and the patient population studied.
CONCLUSIONS
Limited information is available to guide an evidence-based approach to hospital-acquired fever. We propose criteria to help standardize future studies of this important clinical situation.
Keywords: fever, hospital units, hospitalization, inpatients
Antimicrobial resistance has emerged as a major problem in the hospitalized patient. The National Nosocomial Infections Surveillance System found up to a 30% increase in resistant isolates from 1998 to 2003.1 Antimicrobial resistance has been associated with poorer patient outcomes and increased hospital expenditures.2 Unfortunately, significant numbers of new antimicrobials with activity against resistant isolates are not expected in the near future.3
Hospital-acquired fever—fever occurring at least 24 to 48 hours after admission of a previously afebrile patient—is common, and clinicians are faced with the decision of whether or not to begin empiric antimicrobial therapy. As empiric use of broad-spectrum antibiotics contributes to antibiotic resistance in the hospital setting,2 one practical approach to decrease antibiotic resistance entails a better understanding of the need for empiric antibiotics when hospitalized patients become febrile. Accordingly, we undertook a systematic review of the literature focused on adult general medical patients with hospital-acquired fever in order to estimate the incidence, etiology, risk factors, and outcome of hospital-acquired fever and to assist in decisions regarding institution of empiric antibiotic therapy.
METHODS
Literature Search
We sought to identify all published studies of hospital-acquired fever in adult general medicine patients. The MEDLINE database was searched by the investigators, and a reference librarian independently searched MEDLINE and EMBASE. The MEDLINE search utilized the following Medical Subject Heading (MeSH) terms: hospital units; hospitalization; hospitals; critical care; and inpatients. These terms were exploded and combined with fever and limited by year 1970 to 2005. This search produced 877 references. An EMBASE search using a similar strategy (but limited to fever/epidemiology and references from 1988 to 2004) produced 78 references. A Web of Knowledge search was conducted searching for references citing the 7 most prominent articles. This search resulted in 98 references. Finally, the references of all included articles were searched for additional studies.
Selection Criteria
We reviewed titles, abstracts, and articles to identify relevant publications for inclusion. Articles were included if they prospectively or retrospectively reported the incidence, etiology, risk factors or effect on length of stay, antibiotic usage, or mortality of fever acquired during hospitalization. Articles that included subjects with both hospital-acquired and community-acquired fever were included if data were reported in a manner that distinguished hospital-acquired from community-acquired fever. Studies that focused on pediatric patients, fever in the developing world, classic fever of unknown origin or specialized patient populations (e.g., neutropenic patients, patients with neurological injury, critically ill patients, postoperative patients) were excluded.
Data Assessment
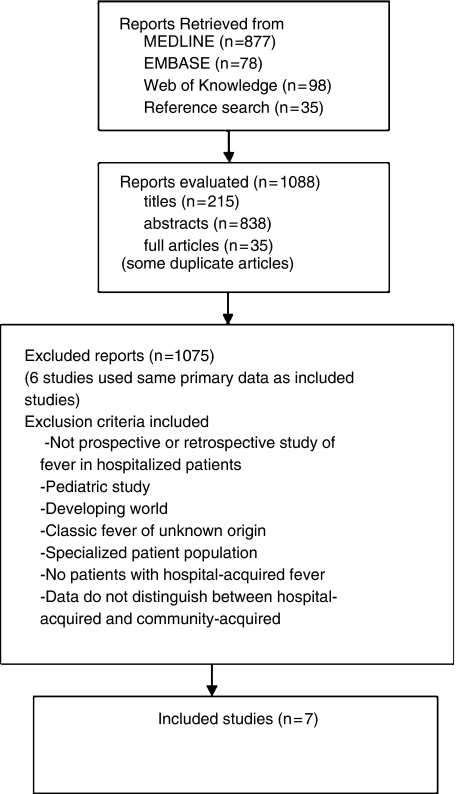
One author (D.R.K.) evaluated all abstracts, articles, or titles. Articles that clearly did not meet inclusion criteria were excluded; all other articles were then independently reviewed in detail by 2 authors (D.R.K., S.A.F.). In the case of disagreement, a third reviewer (S.S.) acted as arbiter. Figure 1 illustrates the process used to select articles.
FIGURE 1.
Method literature review and flow of articles.
Data Synthesis
Assessment of Study Characteristics and Design
A total of 7 studies were included4–10 (Table 1). Six other published reports used the same primary data as included studies. These studies were not included as separate studies, but were reviewed and any relevant data were analyzed.11–16
Table 1.
Summary of Strengths and Weaknesses for Each Included Study
| Study | Design | Comments | Incidence/Etiology of Hospital-acquired Fever | Selected Risk Factors for Infectious Etiology | Antibiotic Use at Onset of Fever |
|---|---|---|---|---|---|
| Arbo et al.4 | Prospective case-control, university hospital 1989 to 1991 | Included only hospital-acquired fever | Incidence 100%* Infectious 56%Noninfectious 25%Unknown 19% | Diabetes mellitusTemperature>38.7°CWBC >10 × 109 | Infectious 67%Noninfectious 31% |
| Bor et al.5 | Prospective cohort, university hospital | Included community-acquired fever | Incidence 17%Infectious 37%Noninfectious 52%Unknown 11% | Higher maximum temperature(38.9° vs 38.3°C) | Not reported |
| Bossink et al.6 | Prospective cohort, Dutch university hospital 1994 to 1995 | Designed to examine risk factors for bacterial etiology of fever | Incidence 100%* Infectious 65% | Higher peak temperature and WBC count | Not reported |
| Filice et al.7 | Prospective case-control, referral VA 1983 to 1984 | Unmatched controls used | Incidence 2%Infectious 67%Noninfectious 40%Unknown 2% | Not done | Infectious 82%Noninfectious 55% |
| McGowan† et al.8 | Retrospective review, county hospital 1975 | Review of data collected in 1975 for other purposes | Incidence 17%Infectious 45%Noninfectious 35%Unknown 21% | Not done | Not reported |
| Trivalle et al.9 | Prospective cohort, French geriatric unit 1995 | Included only hospital-acquired fever | Incidence 11%Infectious 74%Noninfectious 14%Unknown 12% | Number of invasive procedures | Infectious 92%Noninfectious 29% |
| Ueno et al.10 | Prospective cohort, Japanese geriatric unit 1994 to 1995 | Included only hospital-acquired fever | Incidence 100%* Infectious 70%Noninfectious 3%Unknown 27% | Not done | Not reported |
Study examined febrile patients only.
Included only fevers that occurred at least 48 hours after hospitalization.
While all studies included general medical patients, the populations studied differed. One study was conducted exclusively in a general medical ward,4 2 focused on hospitalized geriatric patients,9,10 and 4 included mixed populations but focused on the general medicine setting.5–8 Sites included university hospitals in the United States, Europe, and Japan, a VA hospital, and a county hospital.
Four studies were designed to investigate hospital-acquired fever exclusively4,7,9,10; 3 studies included patients with both hospital-acquired and community-acquired fever.5,6,8 Three studies enrolled only patients with fever4,6,10 and thus made no estimate of incidence of fever; 3 enrolled patients admitted to a unit or hospital over a defined period of time,5,8,9 and 1 study enrolled only patients with fever and calculated incidence of fever on the same ward at a later time.7 Two studies used a case-control design to calculate risk factors for hospital-acquired fever4,7; one of these studies selected unmatched controls randomly from patients on the same unit at the same time as the case subject.7 Two studies used a cohort design to estimate either risk factors for hospital-acquired fever or risk factors for infectious etiology of fever.6,9
Studies varied in the threshold temperature for defining fever and the definition of hospital-acquired fever. The threshold varied from an oral temperature >37.4°C,5 to a rectal temperature >38.3°C.6 Two studies required 2 elevated temperatures4,8; 5 studies required only a single fever.5–7,9,10 The definition of hospital-acquired fever ranged from 24 hours to 7 days after admission, and 4 studies required a 5- or 7-day fever-free interval prior to hospital admission.4,7,9,10
Incidence and Etiology of Hospital-acquired Fever
The incidence of hospital-acquired fever ranged from 2% to 17%5,7–9 (Table 1). Fever was attributed to infection in 37% to 74% of patients, whereas a noninfectious etiology was identified in 3% to 52%.4–10 The most common infectious causes included urinary tract infection, pneumonia, sinusitis, and bloodstream infection.4,7,9,10 The most common noninfectious causes were procedure related (e.g., blood transfusion), malignancies, and ischemic conditions (e.g., myocardial infarction, pulmonary embolism).4,7,9,10
Studies varied in the methodology used to determine the etiology of fever. Two studies used the 1988 Centers for Disease Control and Prevention (CDC) definitions for nosocomial infection, which defines 48 specific sites or types of infection occurring at 13 site categories based on a combination of clinical and laboratory findings.4,9,17 One earlier study used previously described criteria for nosocomial infection.5,18 The authors of 3 other studies used their own classification schemes that relied on the opinions of the authors and the treating physicians regarding the cause of fever.7,8,10 One study classified patients as having microbial infections if blood cultures were positive or local cultures were positive and the treating physicians felt that this required ongoing antimicrobial treatment. A separate classification was made for clinical infection based on physician opinion.6
Selected Risk Factors for Infectious Etiology of Hospital-acquired Fever
Risk factors for infectious etiology of hospital-acquired fever varied from study to study (Table 1). Higher maximum temperature or higher peak white blood cell count were associated with an infectious etiology of fever in more than 1 study.4–6
Antibiotic Usage and Hospital-acquired Fever
Three studies described the use of antibiotics in response to fever.4,7,9 In patients determined to have a bacterial cause of fever, antibiotics were prescribed at onset of fever in 66% to 92% of febrile episodes. Rates of antibiotic use for patients with a noninfectious cause of fever ranged from 29% to 55% for a mean duration of 6.6 to 9.6 days.4,7,9
DISCUSSION
Our review demonstrates that only 7 studies of hospital-acquired fever in the general medical population have been conducted. Moreover, only 4 studies were intended to investigate hospital-acquired fever specifically.4,7,9,10 Drawing clinically relevant conclusions from these studies is limited by heterogeneity in patient population studied, definition of hospital-acquired fever, and determination of etiology of fever.
Our review has several strengths. Several databases were systematically searched and multiple authors independently reviewed papers for inclusion. Furthermore, a separate search was conducted by a research librarian. Explicit criteria were applied to exclude studies of specialized populations that would not be applicable to our questions of interest.
In order to conduct further studies in this important inpatient area, standardization of several methodological issues is necessary. The threshold for fever that should prompt evaluation is arbitrary and depends on the patient setting and condition. For example, an otherwise healthy patient with a single fever to 38.3°C immediately after routine uncomplicated abdominal surgery would rarely require significant evaluation. In contrast, an elderly patient with unexplained delirium and temperature to 38.0°C requires a more thorough evaluation. Elderly patients are known to have lower temperatures at baseline,19 and in one study of hospitalized patients with pneumonia for each decade increase in age the average temperature was decreased by 0.15°C.20 In an attempt to establish a standard for critically ill adults, Infectious Disease Society of America (IDSA) guidelines have suggested that those with temperatures ≥38.3° should be considered febrile.21 IDSA guidelines for neutropenic patients with cancer define fever as “a single oral temperature of ≥38.3°C (101°F) or a temperature of ≥38.0°C (100.4°F) for ≥1 hour.”22 We think that a threshold temperature similar to that used for neutropenic fever would be reasonable to guide further studies of hospital-acquired fever.
The optimal site for measuring temperature needs to be standardized. In one study comparing core temperature with readings obtained with a tympanic thermometer, erroneous readings were common.23 IDSA guidelines for critically ill patients recommend that “axillary measurements should not be used.”21 Thus, we think an oral temperature should be used when possible.
The fever-free interval and duration of hospitalization before fever require definition. We think it is important to study hospital-acquired fever as a distinct population separate from patients admitted with infectious diagnosis who are febrile early in their hospital course. A 5-day afebrile period before admission and at least 48 hours of hospitalization before occurrence of fever should exclude most of these patients.
Finally, classification of the etiology of fever (e.g., infectious, noninfectious, unknown) is a difficult task. Ideally, studies should be conducted prospectively with standardized investigations based on a patient's clinical findings (e.g., chest radiography if new cough or sputum production is present) if the etiology of fever is not obvious on initial evaluation. The best tool available for defining infectious etiology of fever is the CDC definition for nosocomial infection.17
Hospital-acquired fever in the general medicine population appears to be a relatively common but poorly studied subject. Clinicians require further information regarding the etiology, incidence, and outcomes associated with hospital-acquired fever to better optimize empiric antibiotic usage.
Acknowledgments
We are indebted to Patricia M. Redmond, Reference Librarian, Taubman Medical Library, University of Michigan, for her literature search.
Financial support: Dr. Saint is supported by a Career Development Award from the Health Services Research & Development Program of the Department of Veterans Affairs and a Patient Safety Developmental Center Grant from the Agency for Healthcare Research and Quality (P20-HS11540).
REFERENCES
- 1.Cardo D, Horan T, Andrus M, Dembinski M, Edwards J, Peavy G, Tolson J, Wagner D. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32:470–85. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- 2.Shales DM, Gerding DN, John JF, et al. Society for Healthcare Epidemiology of America and Infectious Disease Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25:584–99. doi: 10.1086/513766. [DOI] [PubMed] [Google Scholar]
- 3.Wenzel R. The antibiotic pipeline—challenges, costs, and values. N Engl J Med. 2004;351:523–6. doi: 10.1056/NEJMp048093. [DOI] [PubMed] [Google Scholar]
- 4.Arbo M, Fine MJ, Hanusa BH, Sefcik T, Kapoor WN. Fever of nosocomial origin: etiology, risk factors, and outcomes. Am J Med. 1992;95:505–12. doi: 10.1016/0002-9343(93)90333-k. [DOI] [PubMed] [Google Scholar]
- 5.Bor DH, Makadon HJ, Friedland G, Dasse P, Komaroff AL, Aronson MD. Fever in hospitalized medical patients: characteristics and significance. J Gen Intern Med. 1988;3:119–25. doi: 10.1007/BF02596115. [DOI] [PubMed] [Google Scholar]
- 6.Bossink AW, Groeneveld AB, Hack CE, Thijs LG. The clinical host response to microbial infection in medical patients with fever. Chest. 1999;116:380–90. doi: 10.1378/chest.116.2.380. [DOI] [PubMed] [Google Scholar]
- 7.Filice GA, Weiler MD, Hughes RA, Gerding DN. Nosocomial febrile illnesses in patients on an internal medicine service. Arch Intern Med. 1989;149:319–24. [PubMed] [Google Scholar]
- 8.McGowan JE, Rose RC, Jacobs NF, Schaberg DR, Haley RW. Fever in hospitalized patients with special reference to the medical service. Am J Med. 1987;82:580–6. doi: 10.1016/0002-9343(87)90103-3. [DOI] [PubMed] [Google Scholar]
- 9.Trivalle C, Chassagne P, Bouaniche M, et al. Nosocomial febrile illness in the elderly: frequency, causes, and risk factors. Arch Intern Med. 1998;158:1560–5. doi: 10.1001/archinte.158.14.1560. [DOI] [PubMed] [Google Scholar]
- 10.Ueno K, Hayashi J, Yamaga S, et al. Febrile episodes in elderly inpatients—a one year survey to determine the causes of fever in the hospital. Kansenshogaku Zasshi (J Jpn Assoc Infect Dis) 1998;72:493–8. doi: 10.11150/kansenshogakuzasshi1970.72.493. [DOI] [PubMed] [Google Scholar]
- 11.Bossink AW, Groeneveld AB, Hack CE, Thijs LG. Prediction of mortality in febrile medical patients. How useful are systemic inflammatory response syndrome and sepsis criteria? Chest. 1998;113:1533–41. doi: 10.1378/chest.113.6.1533. [DOI] [PubMed] [Google Scholar]
- 12.Bossink AW, Groeneveld AB, Koffeman GI, Becker A. Prediction of shock in medical patients with clinical infection. Crit Care Med. 2001;29:25–31. doi: 10.1097/00003246-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Bossink AW, Groeneveld AB, Thijs LG. Prediction of microbial infection and mortality in medical patients with fever: plasma procalcitonin, neutrophilic elastase—alpha1-antitrypsin, and lactoferrin compared with clinical variables. Clin Infect Dis. 1999;29:398–407. doi: 10.1086/520222. [DOI] [PubMed] [Google Scholar]
- 14.Groeneveld AB, Bossink AW, Van Mierlo GJ, Hack CE. Circulating inflammatory mediators in patients with fever: predicting bloodstream infection. Clin Diagn Lab Immun. 2001;8:1189–95. doi: 10.1128/CDLI.8.6.1189-1195.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makadon HJ, Bor DH, Friedland G, et al. Febrile inpatients: house officers' use of blood cultures. J Gen Intern Med. 1987;2:293–7. doi: 10.1007/BF02596161. [DOI] [PubMed] [Google Scholar]
- 16.Ueno K. A relationship between febrile illness, serum albumin level and mortality in elderly hospitalized patients. Fukuoka Acta Med. 2003;94:9–19. [PubMed] [Google Scholar]
- 17.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infect Control. 1988;12:128–40. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 18.Spengler RF, Greenough WB. Hospital costs and mortality attributed to nosocomial bacteremias. JAMA. 1978;240:2455–8. [PubMed] [Google Scholar]
- 19.Norman DC. Fever in the elderly. Clin Infect Dis. 2000;31:148–51. doi: 10.1086/313896. [DOI] [PubMed] [Google Scholar]
- 20.Roghmann M, Warner J, Mackowiak PA. The relationship between age and fever magnitude. Am J Med Sci. 2001;322:68–70. doi: 10.1097/00000441-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 21.O'Grady NP, Barie PS, Bartlett JG, et al. Practice guidelines for evaluating new fever in critically ill adult patients. Clin Infect Dis. 1998;26:1042–59. doi: 10.1086/520308. [DOI] [PubMed] [Google Scholar]
- 22.Hughes WT, Armstrong D, Bodey GP, et al. Guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002;34:730–51. doi: 10.1086/339215. [DOI] [PubMed] [Google Scholar]
- 23.Farnell S, Maxwell L, Tan S, Rhodes A, Philips B. Temperature measurement: comparison of non-invasive methods used in adult critical care. J Clin Nurs. 2005;14:632–9. doi: 10.1111/j.1365-2702.2004.00916.x. [DOI] [PubMed] [Google Scholar]