Abstract
A woman developed a prolonged QT interval and torsade de pointes while on methadone treatment for heroin addiction. We think methadone, or its impaired metabolism, was the major cause for her prolonged QT interval and progression to torsade. However, torsade is often multifactorial, as was likely so in this case. We advise physicians treating patients taking methadone to obtain careful medication and drug-use histories, screen for risk factors associated with long QT syndrome, counsel patients about potential drug interactions, and measure the QT interval before and during methadone treatment in high-risk patients.
Keywords: prolonged QT interval, torsade de pointes, QT-prolonging drugs, methadone
Methadone is a synthetic opioid used both for the treatment of heroin addiction and for chronic pain. In the United States, over 180,000 patients are enrolled in methadone maintenance treatment programs for heroin addiction and receive daily methadone.1 Federal regulations have shifted the responsibility for methadone treatment from the U.S. Food and Drug Administration to the Center for Substance Abuse Treatment, which has, in turn, given physicians greater independence and flexibility in prescribing methadone.2 While methadone has proven efficacy in reducing the use of nonprescription opioids and in alleviating pain, it has the potential for serious adverse effects.
Methadone is independently associated with a prolonged QT interval and progression to torsade de pointes. Experimental evidence has shown that methadone has multiple effects on cardiac function.3 In isolated guinea-pig heart preparations, methadone potentiates the inotropic response to sympathetic nerve stimulation and increases the functional refractory period. Methadone also decreases the maximum rate of depolarization and increases the action potential duration in Purkinje fibers. All of these effects may serve to prolong the QT or QTc interval [QTc interval=QT interval divided by the square root of the preceding R-R interval (in seconds)].
Clinically, several reports have linked high dose methadone to a prolonged QT interval and torsade. In a retrospective case series of 17 methadone-treated patients who developed torsade, investigators found that a daily dose of methadone (mean, 397±283 mg) correlated positively with a prolonged QTc interval (615±77 ms) after the analysis controlled for variables such as age, presence of structural heart disease, and presence of hypokalemia.4 Additionally, several case reports have described the development of torsade in patients on high dose methadone therapy and a shortening of the QT interval with a parallel decrease in methadone dose.5,6 However, while methadone alone may prolong the QT interval, most reported cases of methadone-associated torsade have involved other risk factors as well.
We describe a case in which a woman on methadone maintenance developed a long QT interval and torsade de pointes. Although this patient had multiple risk factors that likely contributed to the development of torsade, we believe that methadone or its impaired metabolism was the major cause of her arrhythmia. This case report is intended to help clinicians recognize the risk factors associated with an acquired long QT interval. We believe this report is particularly timely in light of a recent article that was published in the Journal of General Internal Medicine that revealed that a significant number of health care practitioners cannot correctly measure the QT interval or identify factors and medications that may prolong the QT interval.7
CASE REPORT
A 50-year-old woman with a history of intravenous drug use and HIV infection presented to the emergency department after experiencing several recent episodes of sudden shaking and sweating followed by lapses in consciousness. She reported that she had recently been using heroin and cocaine. Her medications included methadone, 145 mg daily, for heroin addiction; tenofovir plus a combined preparation of abacavir, lamivudine, and zidovudine for HIV infection; alprazolam for anxiety; and trazodone for sleep.
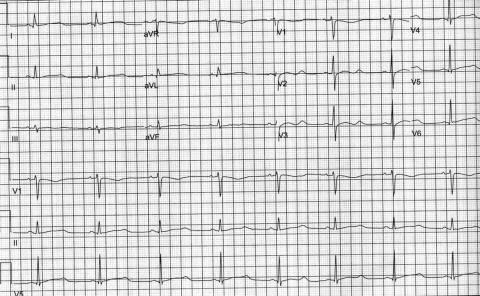
Physical exam was remarkable for normal mental status, blood pressure of 142/72 mm Hg, pulse of 86 beats/min and regular, no cardiac murmurs, and no signs of heart failure. Laboratory studies included potassium of 3.2 mmol/L and magnesium of 1.3 mmol/L. Her electrocardiogram demonstrated sinus rhythm, a rate of 54 beats/min, and a QTc of 618 ms (Fig. 1).
FIGURE 1.
Electrocardiogram obtained during initial evaluation. Note the prolonged QTc interval of 618 ms (normal QTc is <460 ms).
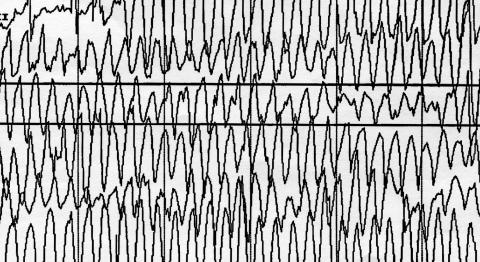
During evaluation in the emergency department, the patient suddenly lost consciousness and her cardiac rhythm revealed a polymorphic tachycardia identified as torsade de pointes (Fig. 2). She was treated with intravenous lidocaine and magnesium with subsequent conversion to sinus rhythm.
FIGURE 2.
Rhythm strip demonstrating torsade de pointes.
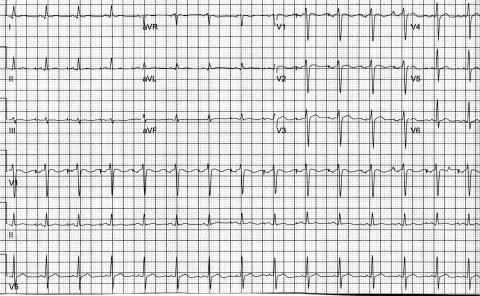
Upon admission to the cardiac care unit, potassium and magnesium were replaced, alprazolam and trazodone discontinued, and the methadone dosage tapered by 10% daily. Despite temporary pacing, electrolyte correction, and labetalol infusion, the patient experienced several more episodes of torsade throughout her hospitalization, several of which required cardioversion. Because of methadone's long half life, which can extend up to 190 hours, and the patient's recurrent hemodynamic instability, a dual chamber implantable cardioverter-defibrillator was placed.8 At the time of the patient's discharge, she was receiving methadone at a daily dosage of 30 mg, and her QTc interval had shortened to 365 ms (Fig. 3).
FIGURE 3.
Electrocardiogram after a dose reduction in methadone. Note the normal QTc of 365 ms (normal QTc is <460 ms).
DISCUSSION
Torsade de pointes is a polymorphic ventricular tachycardia characterized by QRS complexes that vary in axis and amplitude over an isometric line. It is distinguished from other polymorphic ventricular tachycardias by the presence of a prolonged QT interval. The genesis of torsade is postulated to result from derangements in ion flow, which lead to prolonged action potentials and the generation of spontaneous upstrokes, resulting in premature ventricular depolarizations.9 Propagation of these premature ventricular depolarizations may initiate torsade in susceptible patients. Torsade should be considered in patients presenting with palpitations or a history of syncope who are found to have a prolonged QT interval on electrocardiogram.
Methadone, like most drugs that prolong the QT interval, delays cardiac repolarization by blocking the flow of potassium ions through human ether-a-go-go-related gene channels (HERG channels).10 In vitro data have demonstrated that methadone is a very effective inhibitor of the HERG channel in human cells transfected with the HERG potassium channel gene.11 This has been corroborated clinically in a prospective study measuring serial electrocardiograms on 160 patients before and after starting methadone. At 6 and 12 months after drug initiation, the mean QTc increased by 12.4 ± 23 ms (P <.001) at 6 months and by 10.7 ± 30 ms (P <0.001) at 12 months.12
The case presented here supports previous literature associating methadone treatment with a prolonged QT interval and progression to torsade de pointes. We believe that methadone was the main cause for her torsade, as evidenced by a normalization in her QT interval with a parallel dose reduction in methadone. However, in addition to methadone, our patient was taking a variety of drugs that may have impaired the metabolism of methadone and resulted in increased serum levels. Methadone is metabolized by isoforms 2B6 and 3A4 of the cytochrome P450 system. Alprazolam, trazodone, and cocaine are also substrates of the 3A4 isoform.13 It is possible that as all 4 drugs are substrates of this isoform, the 3A4 isoform may have become saturated resulting in increased serum methadone levels.
As in this case, the etiology of torsade is most often multifactorial. A multiplicity of risk factors have been identified.14,15 These include female gender, hypokalemia, hypomagnesemia, structural heart disease, stroke, brain injury, bradyarrhythmias, and a wide variety of prescribed drugs and drug interactions. In 2003, when Zeltser et al.16 analyzed the records of 249 patients who developed torsade while receiving a QT-prolonging medication, they found that all patients had at least 1 additional risk factor in addition to the medication of concern, and that 71% of patients had 2 or more risk factors. The most common risk factors for torsade are drugs and drug interactions. The major classes of QT-prolonging drugs are antiarrhythmics, nonsedating antihistamines, macrolide antibiotics, antidepressants, and antipsychotics.17,18 However, any drug that either delays cardiac repolarization or inhibits the metabolism of another drug that delays cardiac repolarization can increase the risk for torsade. In a retrospective cohort study of drugs prescribed to about 5 million outpatients, Curtis et al.19 found that nearly 10% of patients who filled prescriptions for QT-prolonging medications filled them in conjunction with another medication of concern, defined as either another QT-prolonging drug or a medication that inhibits the clearance of a QT-prolonging drug.
Our patient admitted to using cocaine, which has been associated with QT prolongation and progression to torsade in a patient on methadone.20 Cocaine, in conjunction with methadone, may have contributed to the development of her arrhythmia. However, it is unlikely that cocaine alone was the major cause given its short half life (1 hour) and the patient's persistent QT prolongation several days after stopping cocaine.21
Another component of the patient's history that did not contribute directly to the prolonged QT interval was her HIV infection. Although HIV infection may lead to cardiovascular pathology such as myocarditis, cardiomyopathy, or autonomic neuropathy, HIV infection itself does not prolong the QT interval. And although several protease inhibitors used in highly active antiretroviral therapy may result in QT prolongation,22 the patient was not taking any of these drugs.
This case highlights the importance of using caution when treating patients with methadone or any other drug that has the potential of prolonging the QT interval. Physicians should obtain a careful medication history, screen for risk factors associated with long QT syndrome, and counsel the patient about drug interactions. Additionally, it is wise to consider performing an electrocardiogram on patients maintained on methadone who are at high risk for QT prolongation. This includes patients with a personal or family history of long QT syndrome, a history of bradyarrythmias or structural heart disease, or patients taking other drugs that interact with the CYP3A4 isoenzyme system. Finally, physicians who prescribe methadone may consider referring their patients to the patient-education handout from the Annals of Internal Medicine, which explains torsade de pointes and its association with methadone.23
Acknowledgments
We would like to thank Rosanne Granieri, MD, and Edward I. Curtiss, MD. We acknowledge Sharon Maddox for her editing expertise.
REFERENCES
- 1.McCaffrey BR. Methadone treatment: our vision for the future. J Addict Dis. 2001;20:93–101. doi: 10.1300/J069v20n01_09. [DOI] [PubMed] [Google Scholar]
- 2.Vastag B. Methadone regulations overhauled. JAMA. 2001;285:1435. [Google Scholar]
- 3.Mantelli L, Corti V, Bini R, Cerbai E, Ledda F. Effects of dl-methadone on the response to physiological transmitters and on several functional parameters of the isolated guinea-pig heart. Arch Int Pharmacodyn Ther. 1986;282:298–313. [PubMed] [Google Scholar]
- 4.Krantz MJ, Lewkowiez L, Hays H, Woodroffe MA, Robertson AD, Mehler PS. Torsade de pointes associated with very-high-dose methadone. Ann Intern Med. 2002;137:501–4. doi: 10.7326/0003-4819-137-6-200209170-00010. [DOI] [PubMed] [Google Scholar]
- 5.Walker PW, Klein D, Kasza L. High dose methadone and ventricular arrhythmias: a report of three cases. Pain. 2003;103:321–4. doi: 10.1016/S0304-3959(02)00461-X. [DOI] [PubMed] [Google Scholar]
- 6.Gil M, Sala M, Anguera I, et al. QT prolongation and torsades de pointes in patients infected with human immunodeficiency virus and treated with methadone. Am J Cardiol. 2003;92:995–7. doi: 10.1016/s0002-9149(03)00906-8. [DOI] [PubMed] [Google Scholar]
- 7.Al-Khatib SM, Allen LaPointe NM, Kramer JM, et al. A survey of health care practitioners' knowledge of the QT interval. J Gen Intern Med. 2005;20:392–6. doi: 10.1111/j.1525-1497.2005.0101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gazelle G, Fine PG. Fast Facts and Concepts #75: Methadone for the treatment of pain. End-of-Life Physician Education Resource Center, September 2002. http://www.eperc.mcw.edu.
- 9.El-Sherif N, Turritto G. Torsade de pointes. Curr Opin Cardiol. 2003;18:6. doi: 10.1097/00001573-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: hERG encodes the Ikr potassium channel. Cell. 1995;81:299–307. doi: 10.1016/0092-8674(95)90340-2. [DOI] [PubMed] [Google Scholar]
- 11.Katchman AN, McGroary KA, Kilborn MJ. Influence of opioid agonists on cardiac human ether-a-go-go-related gene K(+) currents. J Pharmacol Exp Ther. 2002;303:688–94. doi: 10.1124/jpet.102.038240. [DOI] [PubMed] [Google Scholar]
- 12.Martell BA, Arnsten JH, Krantz MJ. Impact of methadone treatment on cardiac repolarization and conduction in opioid users. Am J Cardiol. 2005;95:915–18. doi: 10.1016/j.amjcard.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 13.Indianapolis, Indiana: Department of Medicine, Indiana University School of Medicine; [May 18, 2006]. Table of cytochrome p450 drug interactions. updated May 12, 2006. Available at: http://medicine.iupui.edu/flockhart/table.htm. [Google Scholar]
- 14.Roden DM. Taking the “idio” out of “idiosyncratic”: predicting torsades de pointes. Pacing Clin Electrophysiol. 1998;21:1029–34. doi: 10.1111/j.1540-8159.1998.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 15.Viskin S. Long QT syndromes and torsade de pointes. Lancet. 1999;354:1625–33. doi: 10.1016/S0140-6736(99)02107-8. [DOI] [PubMed] [Google Scholar]
- 16.Zeltser D, Justo D, Halkin A, Prokhorov V, Heller K, Viskin S. Torsade de pointes due to noncardiac drugs: most patients have easily identifiable risk factors. Medicine (Baltimore) 2003;82:282–90. doi: 10.1097/01.md.0000085057.63483.9b. [DOI] [PubMed] [Google Scholar]
- 17.Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004;350:1013–22. doi: 10.1056/NEJMra032426. [DOI] [PubMed] [Google Scholar]
- 18.Viskin S, Justo D, Halkin A, Zeltser D. Long QT syndrome caused by noncardiac drugs. Prog Cardiovasc Dis. 2003;45:415–27. doi: 10.1053/pcad.2003.00101. [DOI] [PubMed] [Google Scholar]
- 19.Curtis LH, Ostbye T, Sendersky V, et al. Prescription of QT-prolonging drugs in a cohort of about 5 million outpatients. Am J Med. 2003;114:135–41. doi: 10.1016/s0002-9343(02)01455-9. [DOI] [PubMed] [Google Scholar]
- 20.Krantz MJ, Rowan SB, Mehler PS. Cocaine-related torsade de pointes in a methadone maintenance patient. J Addict Dis. 2005;24:53–60. doi: 10.1300/J069v24n01_05. [DOI] [PubMed] [Google Scholar]
- 21.Zickler P. Methamphetamine, cocaine abusers have different patterns of drug use, suffer different cognitive impairments. [May 16, 2006]. National Institute on Drug Abuse, December 2001. Available at: http://www.drugabuse.gov/NIDA_Notes/NNVol16N5/Meth_coc.html.
- 22.Anson BD, Weaver JG, Ackerman MJ, et al. Blockade of HERG channels by HIV protease inhibitors. Lancet. 2005;365:682–6. doi: 10.1016/S0140-6736(05)17950-1. [DOI] [PubMed] [Google Scholar]
- 23.Summary for patients. Ann Intern Med. 2002;137:I42. doi: 10.7326/0003-4819-136-8-200204160-00004. [DOI] [PubMed] [Google Scholar]